Despite being documented for decades, racial and ethnic disparities in health and health care persist with some widening in recent years. The COVID-19 pandemic and the nationwide racial justice movement in 2020 increased attention and calls to address racial and ethnic disparities in health and recognition of their root causes, including the ongoing impacts of racism and discrimination. Addressing health disparities is not only important from an equity standpoint but also for improving the nation’s overall health and economic prosperity. This chapter provides an overview of racial and ethnic disparities in health and health care and the factors that drive them, examines the actions to address them, and outlines future considerations.
Race, Inequality, and Health
Published: May 28, 2024
Health Policy 101:
Table of Contents
Introduction
What are Health and Health Care Disparities?
Health and health care disparities refer to differences in health and health care between groups that stem from broader social and economic inequities. There are multiple definitions of health disparities. Healthy People 2030 defines a health disparity as “a particular type of health difference that is linked with social, economic, and/or environmental disadvantage” and that adversely affects groups of people who have systematically experienced greater obstacles to health. The Centers for Disease Control and Prevention (CDC) defines health disparities as “preventable differences in the burden, disease, injury, violence, or in opportunities to achieve optimal health experienced by socially disadvantaged racial, ethnic, and other population groups and communities.” A health care disparity typically refers to differences between groups in health insurance coverage, affordability, access to and use of care, and quality of care. The terms “health inequality” and “inequity” are also sometimes used to describe unjust differences. Racism, which the CDC defines as the structures, policies, practices, and norms that assign value and determine opportunities based on the way people look or the color of their skin, results in conditions that unfairly advantage some and disadvantage others, resulting in negative mental and physical health outcomes for marginalized groups.
Reflecting the intersectional nature of people’s identities, some individuals experience disparities across multiple dimensions such as race and ethnicity, gender, or sexual orientation. Beyond race and ethnicity, disparities occur across other factors, including socioeconomic status, age, geography, language, gender, disability status, citizenship status, and sexual identity and orientation. Federal efforts to reduce disparities focus on designated priority populations, including “members of underserved communities: Black, Latino, and Indigenous and Native American persons, Asian Americans and Pacific Islanders and other persons of color; members of religious minorities; lesbian, gay, bisexual, transgender, and queer (LGBTQ+) persons; persons with disabilities; persons who live in rural areas; and persons otherwise adversely affected by persistent poverty or inequality.” These groups are not mutually exclusive and often intersect in meaningful ways. Disparities also occur within subgroups of broader racial and ethnic groups, such as ethnic identity, immigration status, and English proficiency.
Health equity generally refers to individuals achieving their highest level of health through the elimination of disparities in health and health care. Healthy People 2030 defines health equity as the attainment of the highest level of health for all people and notes that it requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and health and health care disparities. The CDC describes health equity as when everyone has the opportunity to be as healthy as possible.
What Factors Drive Racial and Ethnic Health Disparities?
The U.S. has a long history of policies and events that have resulted in stark differences in access to resources, opportunities, and power that contribute to racial and ethnic disparities in health today. Dating back to slavery and colonization of the Americas, people of color have been subject to abuse and mistreatment, including medical exploitation and experimentation, family separation, and efforts to eliminate cultural practices and languages. Historic discriminatory policies, such as redlining, have lasting effects today, leading to residential segregation of Black and Hispanic people into urban neighborhoods with more limited resources and increased health risks, including climate-related risks. Anti-immigrant policies have excluded and discriminated against certain groups, contributing to “othering” and “perpetual foreigner” stereotypes, particularly among Asian immigrants, with a resurgence in anti-Asian rhetoric amid the COVID-19 pandemic. Within medicine, disproven beliefs about biological differences by race have led to race permeating clinical decision making and treatment in multiple ways, including through providers’ attitudes and implicit biases, disease stereotyping and clinical nomenclature, and its use in clinical algorithms, tools, and treatment guidelines.
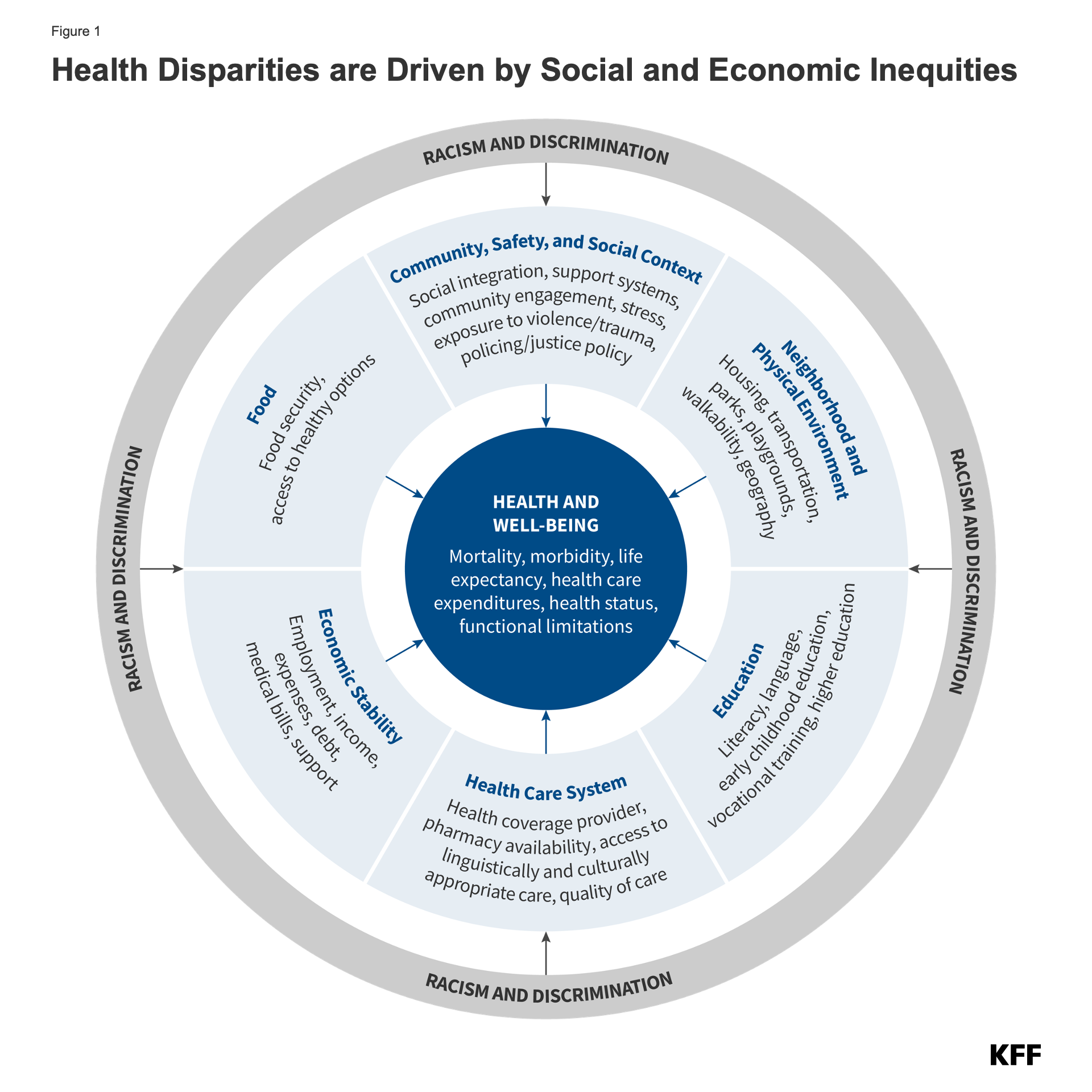
Underlying inequities in social and economic factors that reflect historic and contemporary policies drive racial and ethnic disparities in health (Figure 1). Though health care is essential to health, studies suggest that social and economic factors, often referred to as social determinants of health, are the primary drivers of health outcomes. These include factors such as access to housing and food and economic and educational opportunities. Hispanic, Black, American Indian or Alaska Native (AIAN), and Native Hawaiian or Pacific Islander (NHPI) people fare worse compared to White people across many social and economic factors. Experiences for Asian people are mixed, although some subgroups of Asian people fare worse compared to White people, and Asian immigrants face certain additional challenges.
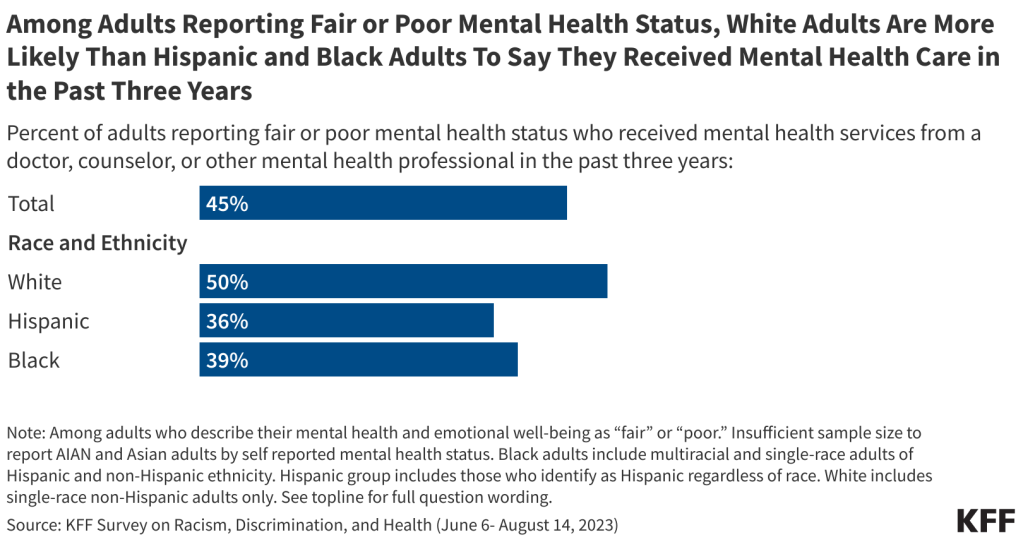
Experiences with unfair treatment and discrimination negatively impact health and well-being. Despite growing calls to address racism, many adults continue to experience unfair treatment and discrimination in their daily lives and in health care settings. A 2023 KFF survey shows that at least half of AIAN (58%), Black (54%), Hispanic adults (50%), and about 4 in 10 Asian adults (42%) say they experienced at least one type of discrimination in daily life in the past year. These experiences include receiving poorer service than others at restaurants or stores; people acting as if they are afraid of them or as if they aren’t smart; being threatened or harassed; or being criticized for speaking a language other than English. Consistent with other research, which shows that racism has negative effects on mental health and results in certain negative physical health outcomes, the KFF survey finds that adults who report experiences with discrimination in daily life are more likely than others to report adverse effects from worry or stress as well as regular feelings of loneliness, anxiety, and depression. Among those with discrimination experiences, 4 in 10 (40%) say they “always” or “often” felt anxious in the past year, compared to 14% of adults who rarely or never experience such discrimination (Figure 2). Similarly, those with discrimination experiences in their daily life are more than three times as likely as others to say they always or often felt lonely (26% vs. 7%) or depressed (25% vs. 7%) in the past year.
Racism and discrimination also negatively affect people’s health care experiences. Black, Hispanic, AIAN, and Asian adults report higher levels of unfair treatment when seeking health care than their White counterparts and are more likely to report having certain negative experiences with a health care provider because of their race and ethnicity (Figure 3). Reflecting these experiences, half or more of Hispanic, Black, and AIAN adults say they prepare for possible insults from providers or staff and/or feel they must be very careful about their appearance to be treated fairly during health care visits at least some of the time. About a quarter of adults who experienced unfair treatment, a negative experience with a provider, or a language access challenge say it led to worse health, being less likely to seek care, and/or switching providers.
Why Is It Important to Address Disparities?
Addressing disparities in health and health care is important not only from an equity standpoint but also for improving the nation’s overall health and economic prosperity. Racial and ethnic health and health care disparities result in higher rates of illness and death across a wide range of health conditions, limiting the overall health of the nation. Research further finds that health disparities are costly, resulting in excess medical care costs and lost productivity, as well as additional economic losses due to premature deaths each year.
It is increasingly important to address health disparities as the population becomes more diverse and stark income inequalities persist. The U.S. Census Bureau projects that people of color will account for over half (52%) of the population in 2050, with the largest growth occurring among people who identify as Asian or Hispanic (Figure 4). Over time, the population has become increasingly racially diverse, reflecting shifting immigration patterns, a growing multiracial population, as well as adjustments to how the Census Bureau measures race and ethnicity. Over time, income inequality within the U.S. has also widened. As of 2022, the top 10% of households in the U.S. had incomes above $216,000 compared with incomes at or below $17,100 among the lowest 10% of households.
What Is the Status of Racial and Ethnic Disparities in Health Today?
Major recognition of health disparities began nearly four decades ago. In 1985, the Report of the Secretary’s Task Force on Black and Minority Health (commonly known as the Heckler Report) documented persistent health disparities that accounted for 60,000 excess deaths each year and synthesized ways to advance health equity. The Heckler Report led to the creation of the U.S. Department of Health and Human Services Office of Minority Health and influenced federal recognition of and investment in many aspects of health equity. Federal recognition of disparities continued in 2003 with the Institute of Medicine’s Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care report, which identified systemic racism as a major cause of health disparities in the United States.
Despite the recognition and documentation of disparities for decades and overall improvements in population health over time, many disparities persist, and in some cases, have widened over time. Analysis across a broad range of measures of health finds that Black and AIAN people fare worse than their White counterparts across half or more of these measures. Data for Hispanic people are more mixed relative to White people, with them faring better on some measures but worse on others. In the aggregate, Asian people fare the same or better than White people on many measures of health, although this finding masks disparities among subgroups of the population. Data gaps limit the ability to examine disparities among NHPI people; where data are available, they point to disparities, particularly for certain subgroups of this population. Some examples of disparities in health outcomes include:
- Black infants were more than two times as likely to die as White infants, and AIAN and NHPI infants were roughly twice as likely to die as White infants as of 2022 (Figure 5). Black and AIAN women also had the highest rates of pregnancy-related mortality across groups between 2017 and 2019.
- In 2022, the age-adjusted mortality rates for diabetes for AIAN, NHPI, and Black people were about twice as high as the rate for White people; Hispanic people also had a higher diabetes death rate compared to White people.
- Although Black people did not have higher cancer incidence rates than White people overall and across most types of cancer, they were more likely to die from cancer in 2020.
- In 2021, the HIV diagnosis rate for Black people was roughly eight times higher than the rate for White people, and the rate for Hispanic people was about four times higher than the rate for White people. AIAN and NHPI people also had higher HIV diagnosis rates compared to White people.
There also are ongoing racial and ethnic disparities in health coverage and access to care. Overall, Black, Hispanic, and AIAN people fare worse compared to White people across many measures of health coverage and access to and use of care. Despite large gains in coverage across groups since the Affordable Care Act (ACA), as of 2022, nonelderly AIAN, Hispanic, Black, and NHPI people were more likely to be uninsured compared to their White counterparts (Figure 6), with even higher uninsured rates among noncitizen Hispanic adults. In addition, Hispanic, Black, Asian, AIAN, and NHPI adults are more likely than White adults to report not having a personal health care provider, and Hispanic, Black, AIAN, and NHPI adults are more likely than White adults to report not seeing a doctor in the past 12 months because of cost.
The COVID-19 pandemic widened some racial and ethnic health disparities, including in life expectancy and mortality. During the height of the COVID-19 pandemic, AIAN, Hispanic, and Black people experienced higher rates of death. Beyond these direct health impacts, the pandemic disproportionately negatively impacted the well-being and social and economic factors that drive health for these and other underserved groups. Largely reflecting the impacts of the pandemic, between 2019 and 2021, there was a sharp drop-off in life expectancy, with particularly large declines among some racial and ethnic groups. AIAN people experienced the largest decline in life expectancy of 6.2 years, followed by Hispanic and Black people (4.1 and 3.6 years, respectively) (Figure 7). Following these declines, provisional data for 2022 show a recent uptick in life expectancy, however, disparities persist across racial and ethnic groups. In 2022, life expectancy was lowest for AIAN people at 67.9 years, followed by Black people, whose expectancy was 72.8 years, both lower compared with the life expectancy of 77.5 years for White people.
What Are Recent Actions to Address Disparities?
Early in his presidency, President Biden issued a series of executive orders focused on advancing health equity. These included orders that outlined equity as a priority for the federal government broadly and as part of the pandemic response and recovery efforts. Federal agencies were directed to develop Equity Action Plans. In its Equity Action Plan, the Department of Health and Human Services (HHS) outlined a series of strategies, including addressing increased pregnancy and postpartum morbidity and mortality among Black and AIAN women; addressing barriers that individuals with limited English proficiency face in obtaining information, services, and benefits from HHS programs; leveraging grants to incorporate equity consideration into funding opportunities; implementing equity assessments; investing in resources to advance civil rights; and expanding contracting opportunities for small, disadvantaged businesses. The plan builds on earlier efforts that included increasing stakeholder engagement, establishing the Office of Climate Change and Health Equity, and establishing the National Institutes of Health UNITE Initiative to address structural racism and racial inequities in biomedical research. Since the release of its Equity Action Plan, HHS has taken actions to extend postpartum coverage through Medicaid and the Children’s Health Insurance Program (CHIP); issued rules to strengthen patient protections, including nondiscrimination protections; and issued guidance to ensure that telehealth services are accessible to people with disabilities and those with limited English proficiency.
The Centers for Medicare and Medicaid Services (CMS) released an updated framework to advance health equity for people covered by Medicare, Medicaid, CHIP, and the Health Insurance Marketplaces. The framework outlines five priorities, including expanding the collection, reporting, and analysis of standardized data on demographics and social determinants of health; assessing the causes of disparities within CMS programs and addressing inequities in policies and operations; building capacity of health care organizations and the workforce to reduce disparities; advancing language access, health literacy, and the provision of culturally tailored services; and increasing all forms of accessibility to health services and coverage. State Medicaid programs also are focused on addressing racial disparities in health outcomes. States have increasingly requested and/or received approval for waivers that aim to advance equity. Further, a growing number of states have approved or pending waivers with provisions related to addressing health-related social needs, such as food and housing, often focused on specific populations with high needs or risks.
The Administration and Congress took a range of actions to stabilize and increase access to health coverage amid the pandemic, with some extending beyond the Public Health Emergency but others ending. Early in the pandemic, Congress passed the Families First Coronavirus Response Act (FFCRA), which included a temporary requirement that Medicaid programs keep people continuously enrolled during the COVID-19 Public Health Emergency in exchange for enhanced federal funds. Primarily due to this provision, Medicaid enrollment grew substantially and the uninsured rate dropped, with AIAN and Hispanic people experiencing the largest decline. The American Rescue Plan Act (ARPA) of 2021 included an option, made permanent in the Consolidated Appropriations Act 2023, to allow states to extend Medicaid postpartum coverage from 60 days to 12 months, and the majority of states have taken steps to extend postpartum coverage. The Consolidated Appropriations Act also included a requirement for all states to implement 12 months of continuous coverage for children in Medicaid, supporting their coverage stability. However, the broader Medicaid continuous enrollment provision adopted during the Public Health Emergency ended on March 31, 2023, and millions of Medicaid enrollees have been disenrolled since then.
There has been a growing focus on addressing disparities in maternal health. The Biden Administration launched several initiatives focused on addressing inequities in maternal health, including releasing a Blueprint for Addressing the Maternal Health Crisis. Federal agencies also have announced plans and actions to support the Blueprint, including CMS, which released a maternity care action plan; the Health Resources and Services Administration, which committed $90 million to various efforts aimed at improving maternal health, and the Office of the Assistant Secretary for Health, which invested $8.5 million in initiatives designed to reduce pregnancy-related deaths and complications that disproportionately impact people of color and those living in rural areas. Other recent actions have focused on enhancing data on maternal and infant health outcomes and disparities, increasing health care workforce diversity, and expanding access to doulas and other services. States, providers, and health systems; foundations; and communities also are engaged in a broad range of efforts to advance maternal and child health and reduce disparities. Moreover, organizations are advocating for more interventions and support to address maternal mental health and substance use issues, major causes of pregnancy-related mortality and morbidity.
There are efforts underway to increase data available to identify and address disparities. The exclusion of disaggregated data for smaller population groups, including AIAN and NHPI people from many datasets and analyses, limits the visibility and understanding of the health and health care disparities they face and inhibits efforts to address them. There are efforts underway to expand and improve the availability of disaggregated data, including a charge from the Biden Administration to address the systemic lack of disaggregated data. In March 2024, the Office of Management and Budget (OMB) announced revisions to update the minimum standards for collecting and presenting data on race and ethnicity for all federal reporting by adding a new racial category for people who identify as Middle Eastern and North African, moving to collect race and ethnicity through a combined single question instead of asking about Hispanic or Latino ethnicity in a separate question from race, and requiring the collection of detailed racial and ethnic categories. Efforts to disaggregate data may help identify health disparities among smaller racial and ethnic groups and subgroups of larger racial and ethnic groups. They also may inform more culturally attuned and community-informed responses to addressing disparities.
Future Outlook
Looking to the future, racial and ethnic disparities in health and health care remain a persistent problem despite their longstanding recognition and growing calls to address them. These disparities reflect the ongoing impacts of racism that lead to structural inequities in resources and opportunities as well as bias and discrimination in health care and daily life. Some key challenges ahead for eliminating racial and ethnic health and health care disparities include:
- How to address underlying social and economic inequities that drive disparities in health.
- How to close racial and ethnic gaps in health coverage and prevent further widening of disparities in health coverage.
- How to increase diversity of the health care workforce and expand access to culturally and linguistically competent care.
- How to ensure all communities are visible in data to identify and address disparities.
- How to protect communities from the uneven impacts of climate change and mitigate widening disparities due to climate-related health risks.
- How to mitigate the perpetuation of disparities amid the growing use of AI and clinical algorithms to guide clinical decision-making.
Addressing racial and ethnic health and health care disparities is of increasing significance as the diversity of the country grows. It is important not only from an equity standpoint but also for improving the overall health and economic prosperity of our nation.
Resources
- Survey on Racism, Discrimination and Health: Experiences and Impacts Across Racial and Ethnic Groups
- Health and Health Care Experiences of Immigrants: The 2023 KFF/LA Times Survey of Immigrants
- Disparities in Health and Health Care: 5 Key Questions and Answers
- Key Data on Health and Health Care by Race and Ethnicity
- Health Coverage by Race and Ethnicity, 2010-2021
- What is Driving Widening Racial Disparities in Life Expectancy?
- Racial Disparities in Maternal and Infant Health: Current Status and Efforts to Address Them
- Key Facts on Health Coverage of Immigrants
- Climate Change and Health Equity: Key Questions and Answers
- Medicaid and Racial Health Equity
- How History Has Shaped Racial and Ethnic Health Disparities: A Timeline of Policies and Events
Citation
Ndugga, N., Hill, L., Pillai, D., & Artiga, S., Race, Inequality, and Health. In Altman, Drew (Editor), Health Policy 101, (KFF, July 2024) https://staging-modern.kff.org/health-policy-101-race-inequality-and-health/ (date accessed).
 Nambi Ndugga
Nambi Ndugga  Latoya Hill
Latoya Hill  Drishti Pillai
Drishti Pillai  Samantha Artiga
Samantha Artiga 







 Emma Wager
Emma Wager  Cynthia Cox
Cynthia Cox 















 Stephanie Oum
Stephanie Oum  Kellie Moss
Kellie Moss  Jennifer Kates
Jennifer Kates 









 Larry Levitt
Larry Levitt 
 Julie Rovner
Julie Rovner