State Health Coverage for Immigrants and Implications for Health Coverage and Care
Note: This brief was updated on May 29, 2025 to update fully state-funded coverage programs for adults and children.
As of 2023, there were 22.4 million individuals who are noncitizen immigrants residing in the U.S., accounting for about 7% of the country’s total population. Among noncitizen immigrants, about six in ten are lawfully present immigrants while the remaining four in ten are undocumented immigrants. Noncitizen immigrants, particularly those who are undocumented, face significant barriers to accessing health coverage and care and are significantly more likely than citizens to be uninsured. These higher uninsured rates reflect more limited access to private coverage and eligibility restrictions for federally funded coverage options. Some states have taken up options in Medicaid and the Children’s Health Insurance Program (CHIP) to expand coverage for lawfully present immigrants and/or established fully state-funded programs to fill gaps in coverage for immigrants. This brief provides an overview of state take-up of these options and state health coverage programs for immigrants regardless of status. It also examines how health coverage and care for immigrants vary by state coverage policies using data from the 2023 KFF/LA Times Survey of Immigrants.
There has been increased state action to expand coverage to immigrants, including immigrant adults, in recent years although these efforts are limited by funding constraints. As of April 2025, 14 states plus D.C. provide fully state-funded coverage for income-eligible children regardless of immigration status, seven states plus D.C. provide fully state-funded coverage to some income-eligible adults regardless of status, and most states have taken up options in Medicaid and CHIP to expand coverage to lawfully present immigrant children and pregnant women. Data and research suggest that coverage expansions for immigrants are associated with lower uninsured rates and improved access to care. A provision in the budget reconciliation bill being considered by Congress would penalize states that have used their own funds to expand coverage to immigrants, including undocumented immigrants, by reducing the federal Medicaid match rates for their Affordable Care Act Medicaid expansion group. Under this provision, there would be cost shift to states if they maintain their coverage expansions or coverage losses among immigrant families if they eliminate them.
Health Coverage for Immigrants
Noncitizen immigrants have high uninsured rates because they have more limited access to private coverage due to working in jobs that are less likely to offer coverage and face eligibility restrictions for federally funded coverage options. Lawfully present immigrants may qualify for Medicaid and CHIP but are subject to eligibility restrictions that result in some, particularly recent immigrants, being ineligible to enroll even if they meet other eligibility criteria. For example, many must meet a five-year waiting period before qualifying for Medicaid or CHIP. Lawfully present immigrants can purchase coverage through the Affordable Care Act (ACA) Marketplaces and may receive tax credits for this coverage without a waiting period. Undocumented immigrants are ineligible to enroll in Medicaid or CHIP or to purchase coverage through the ACA Marketplaces. Medicaid payments for emergency services reimburse hospitals for emergency care they are obligated to provide to individuals who meet other Medicaid eligibility requirements (such as income) but who do not have an eligible immigration status, including undocumented immigrants. These payments help cover costs to hospitals for providing emergency care to immigrants who remain ineligible for Medicaid but are not coverage for individuals.
Medicaid and CHIP Options for Lawfully Present Immigrants
In general, lawfully present immigrants must have a “qualified” immigration status to be eligible for Medicaid or CHIP, and many, including most lawful permanent residents or “green card” holders, must wait five years after obtaining qualified status before they may enroll even if they meet other eligibility requirements. Some immigrants, such as those with Temporary Protected Status, are lawfully present but do not have a qualified status and are not eligible to enroll in Medicaid or CHIP regardless of their length of time in the country. For children and pregnant people, states can cover lawfully residing immigrants without a five-year wait, otherwise known as the Immigrant Children’s Health Improvement Act (ICHIA) option. As of April 2025, 37 states plus D.C. have taken up this option for children and 31 states plus D.C. have elected the option for pregnant people (Figure 1). Indiana plans to implement the option for children and pregnant people in 2025.
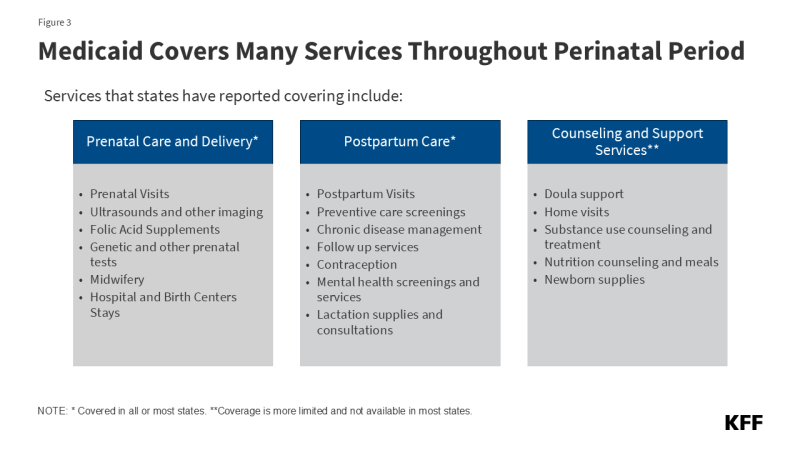
A total of 24 states plus D.C. have also extended coverage through the CHIP From-Conception-to-End-of-Pregnancy (FCEP) option, which provides prenatal care and pregnancy related benefits to targeted low-income children beginning from conception to end of pregnancy regardless of their parent’s citizenship or immigration status (Figure 2). While other pregnancy-related coverage in Medicaid and CHIP requires 60 days of postpartum coverage, the CHIP FCEP option does not include this coverage. However, some states that took up this option provide postpartum coverage through a CHIP health services initiative or using state-only funding. Twelve of the states that have implemented the FCEP option (California, Colorado, Connecticut, Illinois, Maine, Massachusetts, Minnesota, New York, Oregon, Rhode Island, Texas, and Washington) plus D.C. have used state funding or CHIP health services initiatives to extend postpartum coverage to 12 months to align with the Medicaid extension established by the American Rescue Plan Act. Maryland extends coverage for four months postpartum, and Alabama and Virigina extend coverage for 60 days postpartum using CHIP health services initiatives.
Fully State-Funded Coverage
Beyond state take-up of options in Medicaid and CHIP, some states provide fully state-funded coverage to fill gaps in coverage for immigrants. States vary in the eligibility and scope of benefits offered through these coverage programs. These programs extend coverage to lawfully present immigrants who are in the five-year waiting period for Medicaid or CHIP or do not have “qualified status” and are ineligible for federally funded coverage as well as undocumented immigrants. These programs also extended coverage to Deferred Action for Childhood Arrivals (DACA) recipients who previously were not considered lawfully present for purposes of eligibility for federally funded health coverage programs. Effective November 1, 2024, new regulations changed the definition of lawfully present to include DACA recipients for purposes of eligibility to purchase coverage through the ACA Marketplaces and to receive tax credits to help pay for premiums and cost sharing. However, as of April 2025, implementation of this coverage expansion is halted in 19 states due to pending litigation.
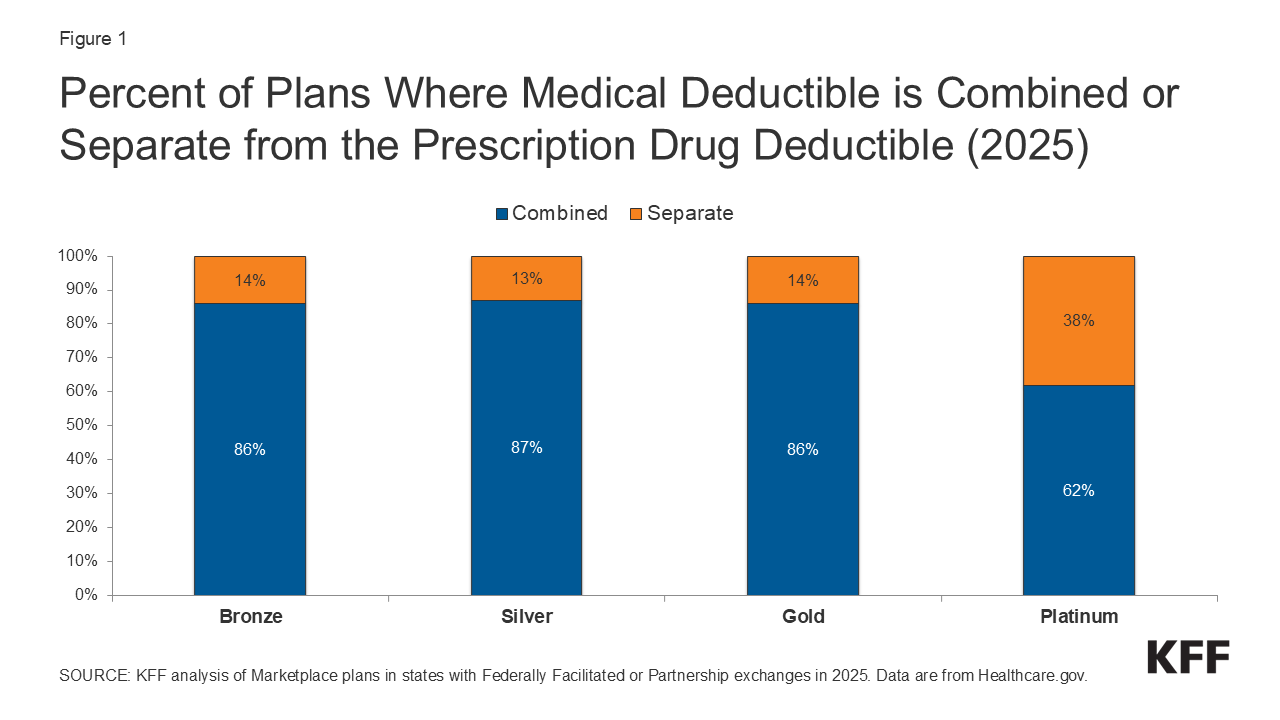
As of May 2025, 14 states plus D.C. provide comprehensive state-funded coverage for children regardless of immigration status (Figure 3). These states include California, Colorado, Connecticut, Illinois, Maine, Massachusetts, Minnesota, New Jersey, New York, Oregon, Rhode Island, Utah, Vermont, Washington, and D.C. Additionally, two of these states (New Jersey and Vermont) also provide state-funded coverage to income-eligible pregnant people regardless of immigration status, with Vermont extending this coverage for 12 months postpartum.
As of April 2025, seven states (California, Colorado, Illinois, Minnesota, New York, Oregon, Washington) plus D.C. have also expanded fully state-funded coverage to some income-eligible adults regardless of immigration status (Figure 4). Some additional states cover some income-eligible adults who are not otherwise eligible due to immigration status using state-only funds but limit coverage to specific groups, such as lawfully present immigrants who are in the five-year waiting period for Medicaid coverage, or provide more limited benefits.
- California extended state-funded health coverage to income-eligible young adults ages 19-25 in January 2020, adults ages 50 and older in May 2022 and adults ages 26 to 49 regardless of immigration status in January 2024, making all low-income immigrants in the state eligible for state-funded health coverage regardless of immigration status. California plans to pause enrollment for undocumented adults 19 and older in 2026.
- Colorado uses state funds to provide Marketplace coverage with premium subsidies to individuals with incomes at or below 300% of the federal poverty level (FPL) regardless of immigration status through OmniSalud using a section 1332 waiver. Colorado previously provided subsidized plans with $0 premiums through SilverEnhanced Savings, but the program is capped at 12,000 people and has paused enrollment for 2025 due to funding constraints.
- D.C. provides health coverage to low-income adults 21 and older regardless of immigration status through its longstanding locally funded Healthcare Alliance program.
- Illinois extended state-funded coverage to low-income individuals ages 65 and older regardless of immigration status through its Health Benefits for Immigrant Seniors (HBIS) program in December 2020 but has paused enrollment due to funding constraints as of April 2025. Illinois previously extended coverage to low-income immigrants ages 42 to 64 regardless of immigration status through the Health Benefits for Immigrant Adults (HBIA) program in 2022 but paused enrollment with plans to end HBIA coverage by July 2025 due to funding constraints.
- Minnesota extended state-funded health coverage to income-eligible individuals regardless of immigration status in January 2025. However, Minnesota plans to end coverage for undocumented adults by 2026.
- New York extended state-funded coverage to individuals ages 65 and older regardless of immigration status beginning in 2023.
- Oregon extended state-funded health coverage to all income-eligible adults regardless of immigration status in July 2023.
- Washington uses state funds to provide Marketplace coverage with premium subsidies to individuals with incomes up to 250% FPL regardless of immigration status through Cascade Care using a section 1332 waiver, but subsidies are no longer available for 2025 due to funding constraints. In July 2024, Washington extended state-funded health coverage to individuals with incomes up to 138% FPL regardless of immigration status, but the program is capped at 13,000 people and has paused enrollment for 2025 due to funding constraints.
In addition to these states, Maryland plans to allow income-eligible individuals to purchase Marketplace coverage without subsidies regardless of immigration status starting November 2025 through a section 1332 waiver.
Impact of State Coverage Expansions on Health Care Access and Use
Data suggest that state coverage options for immigrants make a difference in their health coverage and health care access and use. The 2023 KFF/LA Times Survey of Immigrants shows that immigrants residing in states with more expansive coverage policies for immigrants have higher rates of health coverage, are less likely to postpone or go without care, and are more likely to receive care and to have a trusted health care provider compared to their counterparts living in states with less expansive coverage policies, as described below. (See Box 1).
Box 1: Classifying States by Coverage Policies for Immigrants
The 2023 KFF/LA Times Survey of Immigrants is a nationally representative survey focused on understanding immigrants’ experiences that included questions related to health care access. The survey data were analyzed by expansiveness of health coverage for immigrants in the state in which they reside. States were classified as having less, moderate, and more expansive coverage policies based on whether states have taken up the ACA Medicaid expansion to low-income adults broadly, options in Medicaid and CHIP to cover immigrants, and/or provide state-funded coverage to at least some groups (such as children) regardless of immigration status as follows:
More expansive coverage. States were classified as having more expansive coverage if they have implemented the ACA Medicaid expansion to low-income adults, have taken up options in Medicaid and CHIP to cover immigrants, and provide state-funded coverage to at least some groups (such as children) regardless of immigration status. Even when state-funded coverage is limited to children, the availability of this coverage may reduce fears among immigrant adults about applying for coverage for themselves if they are eligible for other options.
Moderately expansive coverage. States were classified as having moderately expansive coverage if they implemented the ACA Medicaid expansion to low-income adults and have taken up at least two options available in Medicaid and CHIP to expand coverage for immigrants, including covering lawfully-residing immigrant children or pregnant people without a five year wait or adopting the CHIP From-Conception-to-End-of-Pregnancy option to cover income-eligible pregnant people regardless of immigration status.
Less expansive coverage. States were identified as having less expansive coverage if they have not implemented the ACA Medicaid expansion to low-income adults and/or have taken up fewer than two options in Medicaid or CHIP to expand coverage for immigrants and do not offer state-funded health coverage to immigrants.
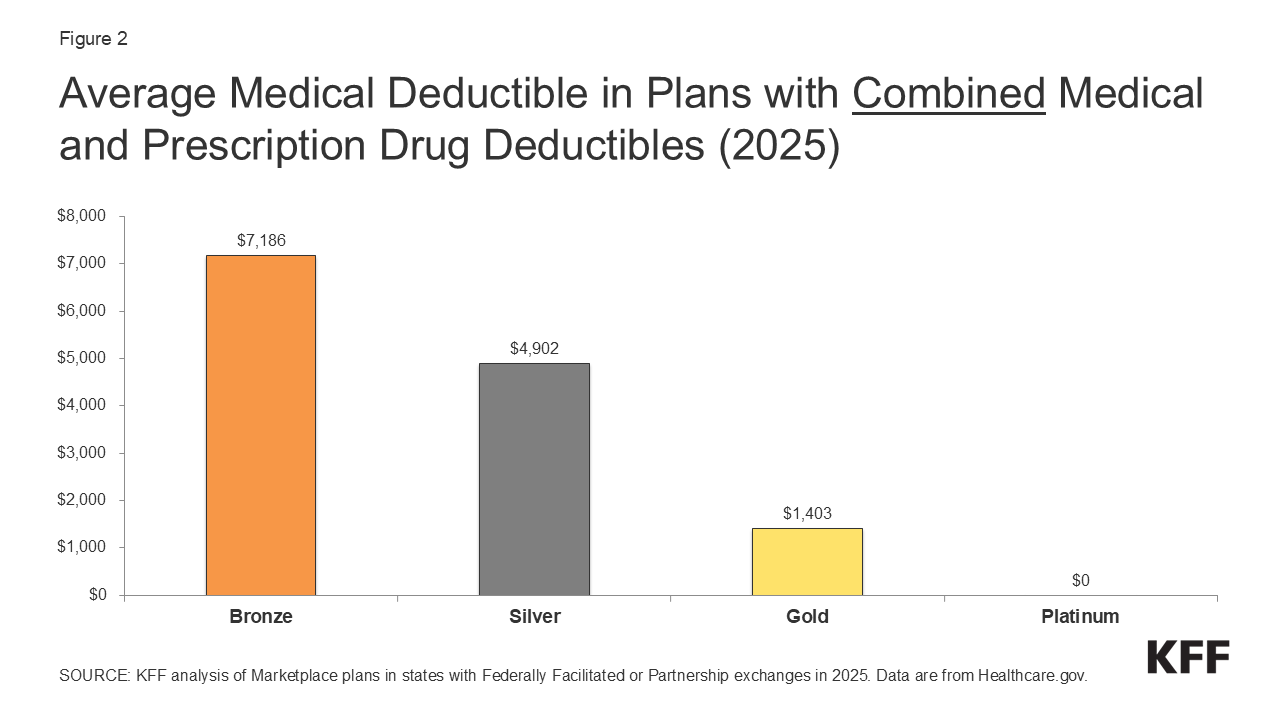
Immigrant adults in states that provide more expansive coverage, including the ACA Medicaid expansion for low-income adults and at least some state-funded coverage for immigrants, are half as likely to be uninsured as those in states with less expansive coverage (11% vs. 22%). This difference is driven by higher rates of Medicaid and other public coverage (including state-funded coverage) in states with more expansive coverage compared to those with less expansive policies (23% vs. 9%) while rates of private and Medicare coverage are similar (Figure 5).
Reflecting higher rates of health coverage, immigrant adults in states with more expansive policies are somewhat less likely to say they skipped or postponed care due to cost. Immigrants in states with more expansive policies are half as likely to report delaying or going without medical care (4% vs. 10%) or dental care (7% vs. 14%) due to cost than those in less expansive states (Figure 6).
Differences in use of care among immigrants by state coverage policies are smaller, which may reflect use of safety-net resources available to uninsured immigrants such as community health centers and emergency rooms. Most (77%) immigrant adults in the U.S. report seeking health care in the past year. The shares reporting seeking health care are slightly lower in states with less expansive coverage (74%) compared to those in states with more expansive coverage (79%), although the majority still report seeking care. This pattern may reflect use of safety-net resources available to uninsured immigrants such as community health centers or emergency rooms. Immigrant adults are more likely than U.S.-born adults to say they rely on community health centers (CHCs) as their usual source of care, reflecting CHCs’ in providing free or low-cost care to low-income and uninsured populations and their ability to provide culturally and linguistically appropriate care. Immigrants in states with less expansive policies are somewhat more likely to say they use a CHC (33% vs. 28%) and somewhat less likely to say they use a private doctor’s office (39% vs. 44%) (Figure 7). Immigrant adults in states with less expansive policies are also less likely to report having a medical provider they trust to answer questions about their health than those in more expansive states (68% vs. 78%).
Other research suggests that state coverage expansions for immigrants can reduce uninsured rates, increase health care use, lower costs, and improve health outcomes. Noncitizen children are more likely to be uninsured and experience more delays in health care due to cost than their citizen siblings. Citizen children with a noncitizen parent are also more likely to be uninsured than citizen children with U.S-born parents. California’s 2016 expansion to cover low-income children regardless of immigration status was associated with a 34% decline in uninsurance rates. Similarly, a study found that children who reside in states that have expanded coverage to all children regardless of immigration status were less likely to be uninsured, to forgo medical or dental care, and to go without a preventive health visit than children residing in states that have not expanded coverage. Other research has found that expanding Medicaid coverage to pregnant people regardless of immigration status was associated with higher rates of prenatal care and improved outcomes including increases in average gestation length and birth weight among newborns, while more restrictive state coverage policies were associated with reduced postpartum care utilization. The cost of providing insurance to immigrant adults through Medicaid expansion was also found to be less than half the per person cost of doing so for U.S-born adults. Recent estimates also suggest that the state-funded expansion to all immigrants regardless of status in California could reduce poverty among noncitizen immigrants and their families.