2012 Employer Health Benefits Survey
Section 9: Prescription Drug Benefits
Almost all covered workers have coverage for prescription drugs. More than three in four covered workers are in plans with three or more cost-sharing tiers for prescription drugs. Copayments rather than coinsurance continue to be the dominant form of cost sharing for prescription drugs.
- As in prior years, nearly all (99%) covered workers in employer-sponsored plans have a prescription drug benefit.
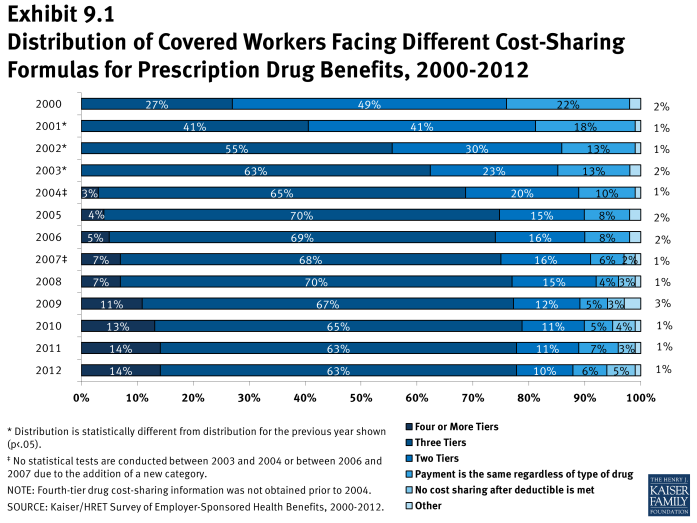
- A large majority of covered workers (87%) in 2012 have a tiered cost-sharing formula for prescription drugs (Exhibit 9.1). Cost-sharing tiers generally refer to a health plan placing a drug on a formulary or preferred drug list, which classifies drugs as generic, preferred, or nonpreferred. Over the past years, an increasing number of plans have created a fourth tier of drug cost sharing, which may be used for lifestyle drugs or expensive biologics.
- Seventy-eight percent of covered workers are enrolled in plans with three, four, or more tiers of cost sharing for prescription drugs, a similar percentage as the last two years (Exhibit 9.1).
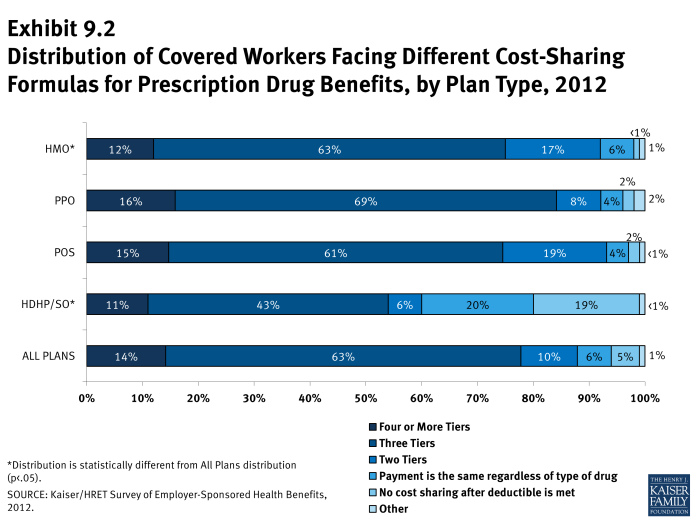
- HDHP/SOs have different cost-sharing patterns for prescription drugs than other plan types. Only 55% of covered workers in HDHP/SOs are in a plan with three or more tiers of cost sharing for prescription drugs; 19% are in plans that pay 100% of prescription costs once the plan deductible is met (Exhibit 9.2).
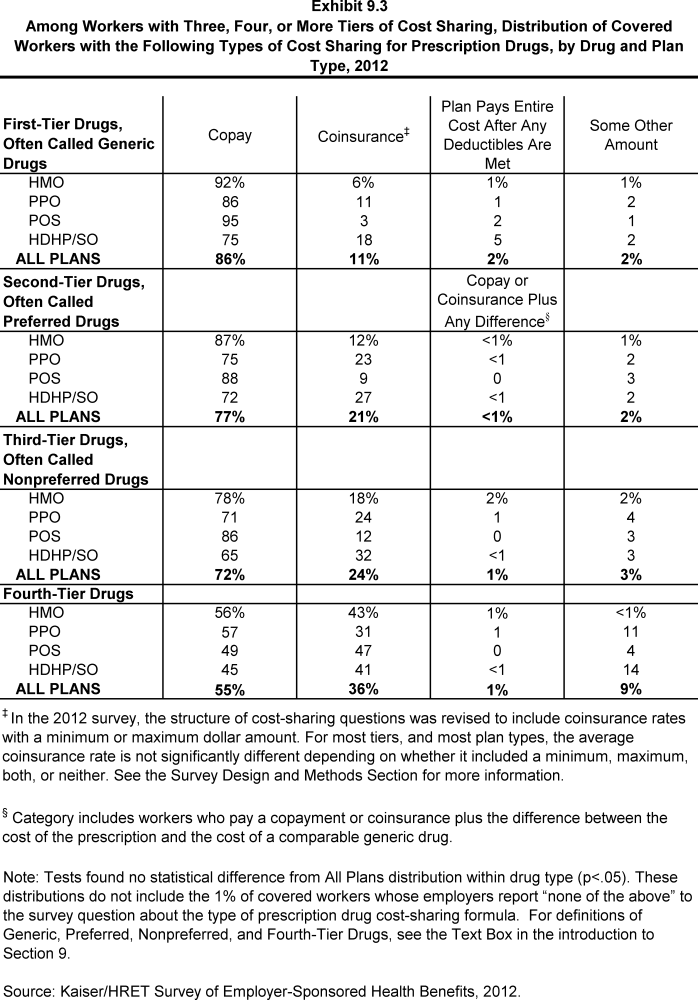
- Among workers covered by plans with three or more tiers of cost sharing for prescription drugs, a large majority face copayments rather than coinsurance (Exhibit 9.3). The percentages differ slightly across drug types because some plans have copayments for some drug tiers and coinsurance for other drug tiers.
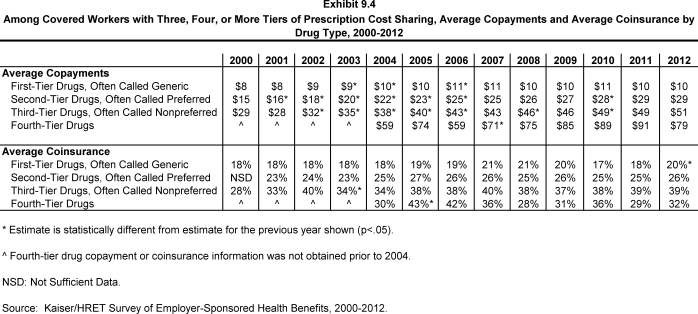
- For covered workers in plans with three, four, or more tiers of cost sharing for prescription drugs, the average drug copayments for first-tier drugs ($10) and second-tier drugs ($29), third-tier drugs ($51), and fourth-tier ($79) are comparable to the amounts reported in 2011 ($10, $29, $49, and $91, respectively) (Exhibit 9.4).
- For covered workers in plans with three, four, or more tiers of cost sharing for prescription drugs who face coinsurance rather than copayments, coinsurance levels average 20% for first-tier drugs, 26% for second-tier drugs, and 39% for third-tier drugs. All of the estimates are similar to last year except for the average coinsurance for first-tier drugs (20%) which is statistically different from 2011 (18%) (Exhibit 9.4).
- Fourteen percent of covered workers are in a plan that has four or more tiers of cost sharing for prescription drugs (Exhibit 9.1). For covered workers in plans with three or more cost-sharing tiers, 55% face a copayment for fourth-tier drugs and 36% face coinsurance (Exhibit 9.3).
- The average copayment for a fourth-tier drug is $79 and the average coinsurance is 32%. These amounts are not statistically different from the amounts reported in 2011 (Exhibit 9.4).
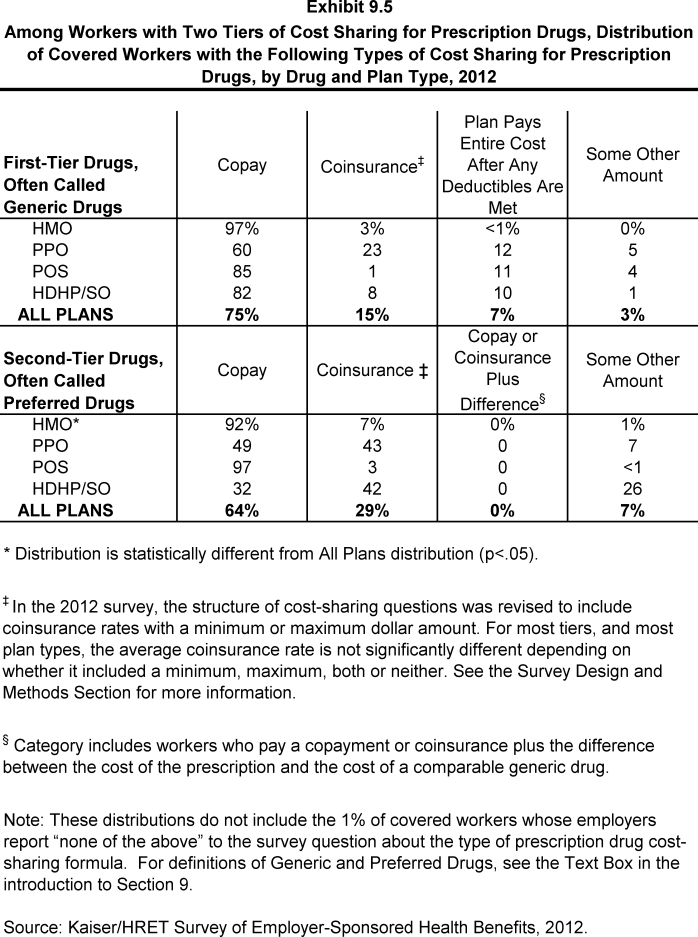
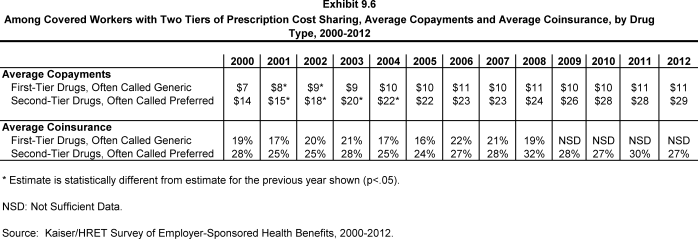
- Ten percent of covered workers are in a plan that has two tiers for prescription drug cost sharing (Exhibit 9.1). Similar to workers in plans with more cost-sharing tiers, copayments are more common than coinsurance for workers in plans with two tiers (Exhibit 9.5). The average copayment for the first tier is $11, and the average copayment for the second tier is $29. The average coinsurance rate for the second tier is 27% (Exhibit 9.6).
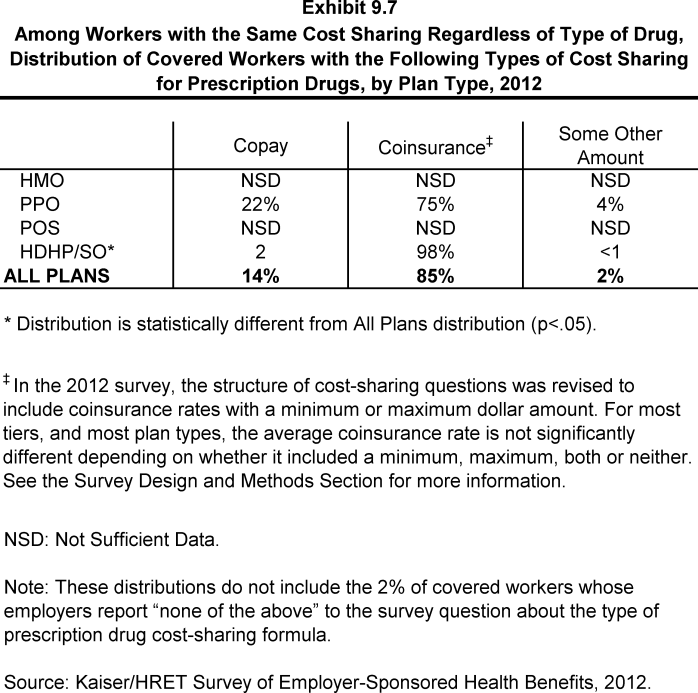
- Six percent of covered workers are covered by plans in which cost sharing is the same regardless of the type of drug chosen (Exhibit 9.1). Among these covered workers, 14% have copayments and 85% have coinsurance (Exhibit 9.7).
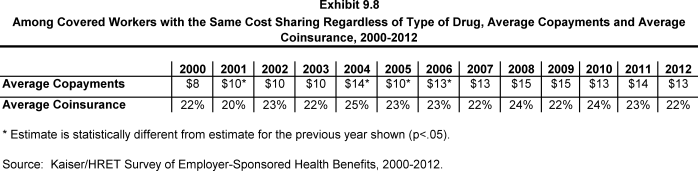
- For those workers with the same cost sharing regardless of the type of drug, the average copayment is $13 and the average coinsurance is 22% (Exhibit 9.8).
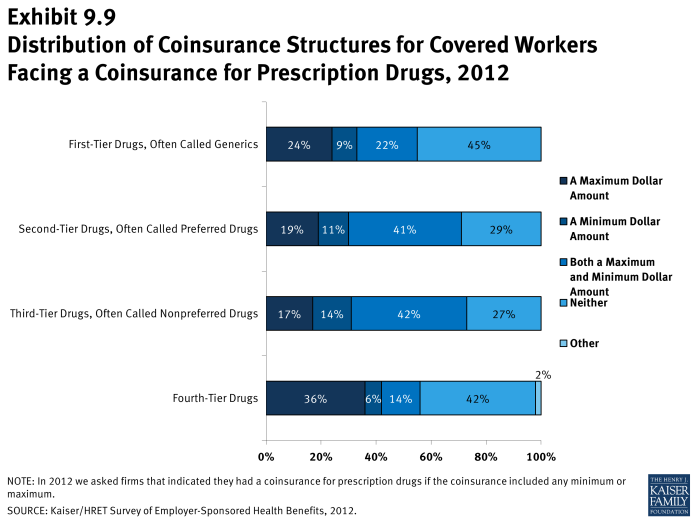
- Coinsurance rates for prescription drugs often have maximum or minimum dollar amounts associated with the coinsurance rate. Twenty-four percent of workers with a coinsurance rate have a maximum dollar amount attached to the coinsurance rate, 9% have a minimum, and 22% have both for first-tier drugs (Exhibit 9.9).
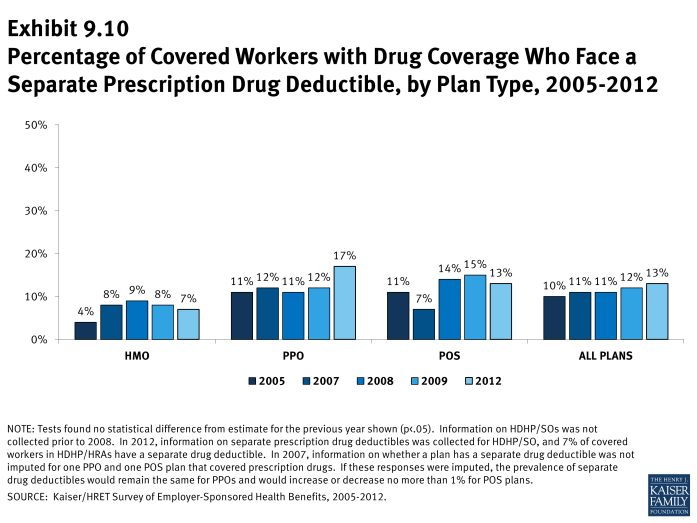
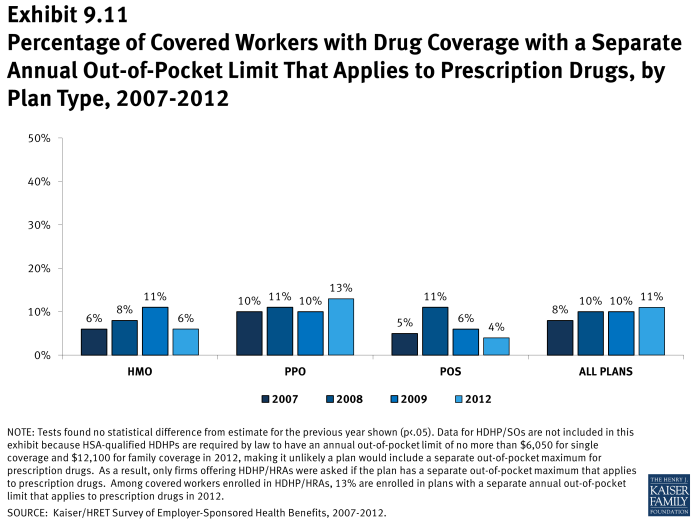
- Small percentages of covered workers are enrolled in plans in which they have a separate prescription drug deductible or annual out-of-pocket limit that applies to prescription drugs only.
- Thirteen percent of covered workers with prescription drug coverage are in plans with a separate prescription drug deductible that is in addition to any general annual deductible the plan might have, similar to the 12% in 2009 (Exhibit 9.10). Seventeen percent of covered workers in PPOs have a separate drug deductible (Exhibit 9.10).
- Of firms with an annual deductible for prescription drugs, 69% of covered workers are in plans where the deductible applies to every tier.
- For those with a separate drug deductible, the average annual deductible amount is $145.
- Similarly, 11% of covered workers with coverage for prescription drugs are in plans with a separate prescription drug annual out-of-pocket limit (Exhibit 9.11), statistically unchanged from 2009.
- For those with a separate prescription drug annual out of pocket limit, the average annual deductible amount is $1,722.
Generic drugs: A drug product that is no longer covered by patent protection and thus may be produced and/or distributed by multiple drug companies.
Preferred drugs: Drugs included on a formulary or preferred drug list; for example, a brand-name drug without a generic substitute.
Nonpreferred drugs: Drugs not included on a formulary or preferred drug list; for example, a brand-name drug with a generic substitute.
Fourth-tier drugs: New types of cost-sharing arrangements that typically build additional layers of higher copayments or coinsurance for specifically identified types of drugs, such as lifestyle drugs or biologics.
Brand-name drugs: Generally, a drug product that is covered by a patent and is thus manufactured and sold exclusively by one firm. Cross-licensing occasionally occurs, allowing an additional firm to market the drug. After the patent expires, multiple firms can produce the drug product, but the brand name or trademark remains with the original manufacturer’s product.