Patient and Consumer Protections
-
Final Prior Authorization Rules Look to Streamline the Process, but Issues Remain
This brief examines the final CMS regulations governing prior authorization in Medicare Advantage, Marketplace, Medicaid, and other plans, how they might address some current consumer concerns, and some issues that remain.
-
KFF Health News: States Target Health Insurers’ ‘Prior Authorization’ Red Tape

Doctors, patients, and hospitals have railed for years about the prior authorization processes that health insurers use to decide whether they’ll pay for patients’ drugs or medical procedures. The Biden administration announced a crackdown in January, but some state lawmakers are looking to go further.
-
The Health Wonk Shop: Prior Authorization in Health Insurance

Nearly 1 in 5 consumers with health insurance say their insurer delayed or denied care in the past year due to its requirements for prior authorization, a process through which insurers can require patients to obtain approval in advance before they will agree to cover specific services. Insurers point to prior authorization as…More
-
Consumer Problems with Prior Authorization: Evidence from KFF Survey

This Data Note highlights findings from the KFF Consumer Survey on problems consumers have experienced with prior authorization requirements. Overall, those with Medicaid, those who are higher utilizers of care encountered more problems with prior authorization over the past year.
-
This brief analyzes data from CMS to examine the number and outcome of Medicare Advantage prior authorization requests in 2021, overall and by firm.
-
Proposed Mental Health Parity Rule Signals New Focus on Outcome Data as Tool to Assess Compliance
Proposed updates to federal mental health parity rules would make wide ranging changes to current standards that apply to private insurance and coverage provided by most employers. This issue brief focuses on a requirement that plans perform an “outcome analysis.”
-
Health Care Debt In The U.S.: The Broad Consequences Of Medical And Dental Bills
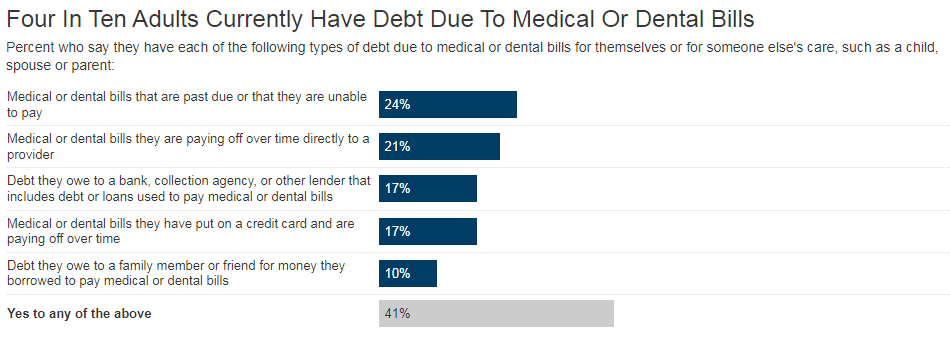
The KFF Health Care Debt Survey finds that four in ten adults have some form of health care debt, with most citing one-time or short-term medical expenses as the contributor. Many of those with health care debt report making personal sacrifices and enduring financial consequences as a result of their debt, while nearly one in five think they will never be able to pay off.
-
SCOTUS Decision on "Chevron Deference" Could Have Big Impacts on Health Policy
The Supreme Court decision overturning “Chevron deference” has profound implications for health care.
It ushers in an era in which courts will not have to accept agency expertise in their review of challenged federal regulations. -
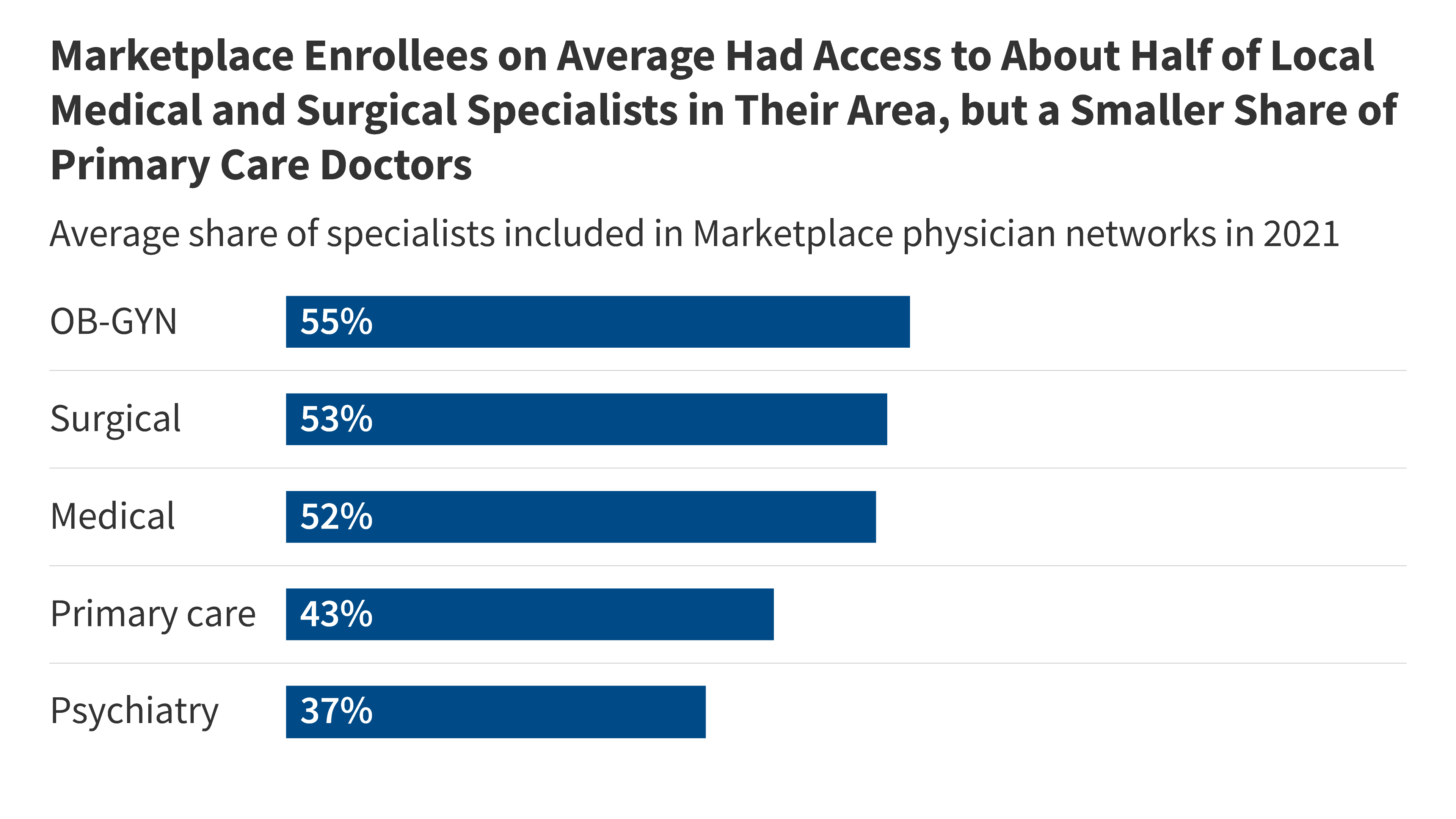
Claims Denials and Appeals in ACA Marketplace Plans in 2021
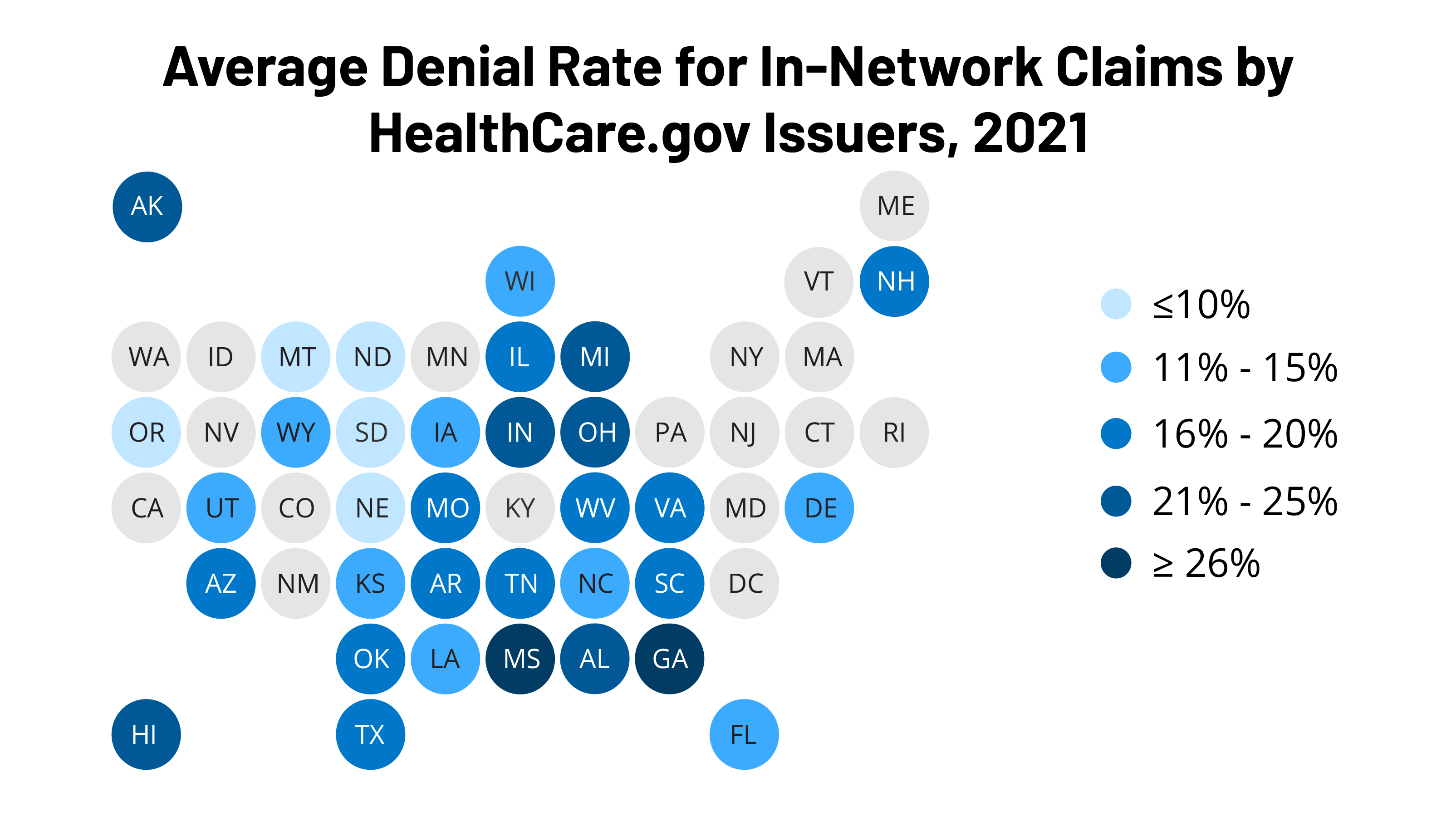
This analysis of HealthCare.gov Marketplace insurers’ transparency data finds that 17% of in-network claims were denied in 2021, with denial rates varying widely across insurers. Consumers appealed less than two-tenths of 1% of denied in-network claims.