States Focus on Quality and Outcomes Amid Waiver Changes: Results from a 50-State Medicaid Budget Survey for State Fiscal Years 2018 and 2019
Eligibility and Premiums
| Key Section Findings |
| Since 2014, most major Medicaid eligibility policy changes have been related to adoption of the ACA Medicaid expansion. Thirty-two states have implemented the expansion to date and two additional states adopted the expansion in FY 2018 and plan to implement the policy in FY 2019 (Maine and Virginia). Other Medicaid eligibility expansions for FY 2018 or FY 2019 were narrow and targeted to a limited number of beneficiaries. In contrast, eligibility restrictions implemented in FY 2018 (by six states) or planned for implementation in FY 2019 (in 11 states) generally target broader Medicaid populations including expansion adults and parents/caretakers. Policies that have or are likely to result in enrollment declines are counted as restrictions in this report. The vast majority of states implementing or planning eligibility policies that are counted as restrictions in FY 2018 or FY 2019 are doing so through Section 1115 waiver authority, whereas most states implementing or planning eligibility expansions are doing so through state plan amendment (SPA) authority.
What to watch:
Tables 1, 2, and 3 at the end of this section include additional details on eligibility, premium, and corrections-related policy changes in FY 2018 and FY 2019. |
Changes to Eligibility Standards
Eligibility Restrictions
A growing number of states are pursuing Section 1115 waivers that include policies that would result in eligibility restrictions in FY 2018 and FY 2019 (Exhibit 1). Some of these policies are in response to January 2018 CMS guidance1 indicating the agency’s support for Section 1115 waiver proposals that would require certain Medicaid enrollees to meet a work requirement in order to maintain coverage. Policies that have or are likely to result in enrollment declines are counted as restrictions in this report.
| Exhibit 1: Eligibility Restrictions by Policy Authority | ||||
| FY 2018 | FY 2019 | |||
| SPA | 2 States | CT, NM | 0 States | |
| Section 1115 Waiver | 4 States | AR, IA, IN, UT | 11 States | AL*, FL*, IN, KY*^, MA, ME*, MI*, NH, NM*, OH*, SD* |
|
*Indicates the Section 1115 Waiver has not yet been approved by CMS.
^CMS’ approval of Kentucky’s waiver authorizing FY 2019 restrictions was set aside by a court order in June 2018 that also remanded the waiver to CMS for reconsideration regarding how the waiver would meet the medical assistance objectives of the Medicaid statute.
|
||||
Six states reported implementing restrictions in FY 2018 and 11 states reported restrictions already implemented or planned for implementation in FY 2019 (Exhibit 1 and Table 1). This year’s survey reports changes that states plan to implement in FY 2019, even if the changes are in Section 1115 waiver proposals that are still pending approval2 at CMS. Waiver provisions that states plan to implement in FY 2020 or after are described later in the “Challenges and Priorities” section of this report.
Eight states reported implementing or plans to implement work requirements under Section 1115 waiver authority in FY 2018 or FY 2019 (Table 2).3 These policies generally require beneficiaries to verify their participation in approved activities, such as employment, job search, or job training programs, for a certain number of hours per week or month to receive health coverage or qualify for an exemption. Data show, however, that most Medicaid enrollees are already working or would qualify for exemptions from these requirements, yet these individuals would still need to navigate a reporting or exemption process to retain their Medicaid coverage. In this report, work requirement policies are counted based on the initial date of implementation rather than the date on which the first coverage terminations will occur.
- Three states have approved waivers to implement a work requirement, including one state (Arkansas) that implemented the policy in June of FY 2018 and two states (Indiana and New Hampshire) that plan to implement in FY 2019.
- Five additional states reported pending work requirement proposals that they plan to implement in FY 2019. Four of these states (Alabama, Maine, Ohio, and South Dakota) have proposals pending approval by CMS and one state (Kentucky) received approval for a work requirement waiver that was set aside by court order. That waiver is now back with CMS for reconsideration (see the Kentucky HEALTH waiver box below). Kentucky’s waiver is referred to as “pending” throughout the rest of this report.
Many of these states reported new administrative requirements or costs associated with implementation of work requirement policies, including those related to vendor contracts for call centers, systems modifications, increased state and local office staff, outreach to beneficiaries and providers, and increased MCO personnel costs.
| Kentucky HEALTH Waiver |
| In January 2018, Kentucky received initial CMS approval for the Kentucky HEALTH Section 1115 waiver. The waiver included several provisions approved for the first time in Medicaid — a work requirement, monthly premiums up to 4% of income, and coverage lock-outs for failure to timely renew eligibility or timely report changes affecting eligibility — as well as heightened cost-sharing for non-emergency ER use, elimination of retroactive eligibility, and elimination of non-emergency medical transportation. A court order issued in Stewart v. Azar on June 29, 2018, however, set aside the CMS approval and remanded the waiver to CMS for reconsideration regarding how the Kentucky waiver would meet the medical assistance objectives of the Medicaid statute. At the time of the survey, CMS had completed an additional federal public comment period and the state was preparing for FY 2019 implementation, but the waiver remained under consideration at CMS. |
Eight states indicated that they have eliminated or propose to eliminate or restrict retroactive eligibility for one or more groups in FY 2018 and FY 2019 (Table 2).4 In FY 2018, Arkansas limited retroactive eligibility from 90 to 30 days, Iowa eliminated retroactive eligibility for all groups other than children under age one and pregnant women (but restored retroactive eligibility for nursing facility residents in July 2018), and Utah eliminated retroactive eligibility for Primary Care Network (PCN) waiver adults. In FY 2019, five states (Florida, Kentucky, Maine, New Hampshire, and New Mexico) plan to eliminate retroactive eligibility or limit it to a single month for most enrollees.
Other examples of reported eligibility restrictions in FY 2018 or FY 2019 include:
- In FY 2018, as part of their HIP 2.0 waiver renewal (a waiver that already included other eligibility restrictions), Indiana5 imposed a three-month lock-out from coverage on expansion adults who fail to comply with redetermination. Enrollees who do not verify eligibility at renewal are disenrolled but can re-enroll without a new application if they provide necessary documentation within 90 days. After 90 days, individuals are subject to a three-month lock-out before they can re-enroll.6
- In FY 2019, New Mexico plans to implement proposals included in a pending waiver application to disenroll and lock-out expansion adults who do not pay required Medicaid premiums and a “reasonable promptness” waiver that would delay coverage until the first day of the first month following receipt of required premiums.
- In FY 2019, Maine7 plans to implement (if their pending waiver is approved) several restrictions on their traditional Medicaid populations in addition to their planned waiver of retroactive eligibility and the work requirement. These include applying a $5,000 asset test to all coverage groups that currently do not have an asset test and eliminating hospital presumptive eligibility for all coverage groups. The state’s pending waiver application proposes to implement these initiatives within six months of demonstration approval.
Eligibility expansions
Aside from planned implementation of the ACA Medicaid expansion in two states in FY 2019, most other eligibility expansions for FY 2018 and FY 2019 are narrow in scope. Overall, ten states implemented Medicaid eligibility expansions in FY 2018, and seven states plan to implement expansions in FY 2019.
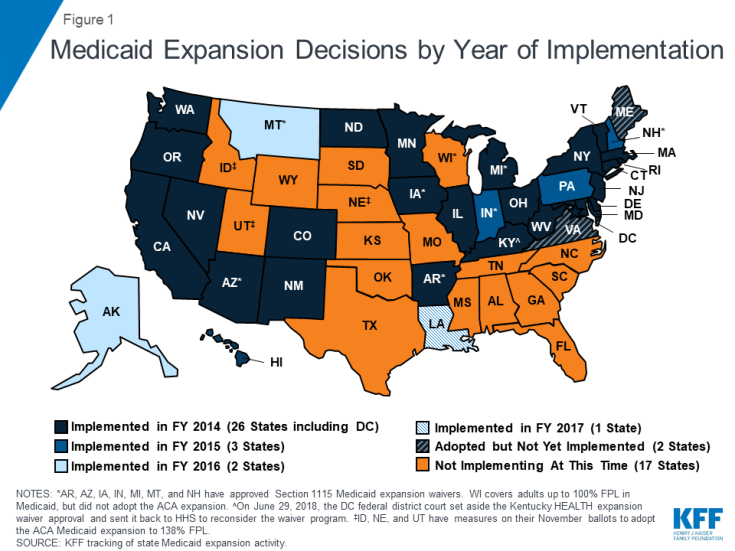
Two states (Maine and Virginia) plan to implement the ACA Medicaid expansion in FY 2019. These expansions will add to the 32 states that had already implemented the ACA Medicaid expansion as of July 2018 (Figure 1). In Virginia, the expansion was adopted as part of the FY 2019-2020 Medicaid budget, with implementation planned for January 1, 2019. Maine voters adopted the Medicaid expansion through a ballot initiative in November 2017 that required submission of a state plan amendment (SPA) within 90 days and implementation of expansion within 180 days of the measure’s effective date.8 After failing to meet the SPA submission deadline (April 3, 2018), Maine’s Governor complied with a Maine Supreme Judicial Court order to submit an expansion SPA on September 4, 2018 but also sent a letter to the federal government asking CMS to reject the SPA. The expansion had not yet been implemented at the time of the survey, and implementation will fall to the new governor after the November 2018 election.
Three additional states (Idaho, Nebraska, and Utah) will have referendum initiatives to adopt the Medicaid expansion on the November 2018 ballot. Montana also has an expansion-related initiative for voters on the November ballot that would eliminate the state’s June 2019 expansion program sunset date and raise tobacco taxes to fund the state’s share of expansion costs.
| Exhibit 2: Eligibility Expansions by Policy Authority | ||||
| FY 2018 | FY 2019* | |||
| SPA | 8 States | AR, CO, ID, MO, PA, SC, UT, VT | 6 States | CT, MD, ME, MO, NJ, VA |
| Section 1115 Waiver | 3 States | DE, UT, VA | 0 States | |
| *Iowa’s FY 2019 eligibility expansion that reinstated 3-month retroactive eligibility for Medicaid-eligible nursing facility residents did not require new Section 1115 or SPA authority. | ||||
Ten states implemented more narrow eligibility expansions in FY 2018 and five states plan to implement more limited expansions in FY 2019. In contrast to eligibility restrictions, which states are primarily implementing under Section 1115 authority, most states implementing or planning eligibility expansions in FY 2018 or FY 2019 are doing so through optional authority using a state plan amendment (SPA) (Exhibit 2). Some examples of these other expansions include the following:
- In FY 2018 under Section 1115 waiver authority, Utah implemented coverage for individuals with income below 5% of the federal poverty level (FPL) who are chronically homeless, justice-involved, or in need of substance use and/or mental health treatment. The state also has approval to implement 12 month continuous eligibility for this population.
- Missouri increased asset limits in both FY 2018 and FY 2019 for aged and disabled beneficiaries and Vermont increased asset limits in FY 2018 for their Working People with Disabilities Program.
- In FY 2018, Arkansas and South Carolina eliminated the five-year waiting period on Medicaid eligibility for lawfully-residing immigrant children and pregnant women.9
Premiums
The Medicaid statute generally does not allow states to charge premiums to most Medicaid beneficiaries. Historically, premiums were limited to special higher income categories of beneficiaries such as expanded Medicaid for the working disabled. However, some states have obtained waiver authority to charge higher premiums and/or copayments than otherwise allowed.
Only Indiana reported activity related to Medicaid premiums in FY 2018 (Table 2). Effective January 1, 2018, the state changed its monthly premiums (which are paid into a health account) for expansion adults from 2% of income to tiered amounts based on income ranges (expressed as a percentage of the FPL). The result is reduced fluctuation of premiums. This report considers the change neutral from the beneficiary’s perspective.
Seven states report proposed implementation of new premium programs or changes to existing premiums for FY 2019 (Table 2). Three of these states (Idaho, Indiana, and Iowa) have already received approval for these changes, while they are still pending as part of Section 1115 waiver requests in four states (Kentucky, Maine, Michigan, and New Mexico). Notable FY 2019 premium policy changes include an approved waiver provision in Indiana to implement a premium surcharge for tobacco users and a pending waiver request in Michigan to require premiums of up to 5% of income (a higher amount than CMS has ever approved for any state) for expansion adults after 48 cumulative months of expansion eligibility.
Coverage Initiatives for the Criminal Justice Population
In recent years, many states have implemented new policies to connect individuals involved with the criminal justice system to Medicaid, as the Medicaid expansion extended new coverage to these individuals in many states (especially childless adults who were not previously eligible in most states). Connecting these individuals to health coverage10 can facilitate their integration back into the community upon release. While individuals may be enrolled in Medicaid while they are incarcerated, Medicaid cannot cover the cost of their care during incarceration, except for inpatient services. Nearly all states have policies in place to cover inpatient care under Medicaid for eligible, incarcerated individuals (Exhibit 3 and Table 3). Most states are also working with corrections agencies and with local jails to facilitate Medicaid enrollment prior to release. The majority of states do not terminate Medicaid coverage for enrollees who become incarcerated: states either maintain the eligibility of the incarcerated individual with benefits limited to inpatient hospital care, or they suspend eligibility. When coverage is suspended, it can be reinstated more easily and quickly upon release from incarceration or when an inpatient hospital stay occurs.
As this report was being finalized, the Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities (SUPPORT) Act was expected to be signed into law. Beginning in October 2019, the Act would prohibit states from terminating Medicaid eligibility for an individual under age 21 or former foster care youth up to age 26 while incarcerated. States would also be required to redetermine eligibility prior to release without requiring a new application and restore coverage upon release.
While both Medicaid expansion and non-expansion states have adopted strategies to connect justice-involved individuals to Medicaid coverage, these initiatives affect many more people in expansion states compared to non-expansion states where Medicaid eligibility for adults remains restrictive.
| Exhibit 3: Coverage Initiatives for the Criminal Justice Population in FY 2018 and/or FY 2019 (# of States) | |||
| Select Medicaid Coverage Policies for the Criminal Justice Population | Jails | Prisons* | Parolees |
| Medicaid coverage for inpatient care provided to incarcerated individuals | 42 | 48 | N/A |
| Medicaid outreach/assistance strategies to facilitate enrollment prior to release from incarceration or for parolees | 34 | 39 | 26 |
| Eligibility maintained or suspended (rather than terminated) for Medicaid enrollees who become incarcerated^ | 36 | 38 | N/A |
| ^States that continue Medicaid eligibility for incarcerated individuals but limit covered benefits to inpatient hospitalization are also included in the count of states that suspend eligibility.
*The District of Columbia has jails but not a prison system. However, DC is counted under Medicaid outreach/assistance strategies because some individuals who serve prison terms outside of DC may be placed in residential re-entry centers upon returning to DC and may apply for Medicaid to access coverage for 24-hour inpatient care and to facilitate enrollment prior to release. |
|||
Table 1: Changes to Eligibility Standards in all 50 States and DC, FY 2018 and FY 2019
|
Eligibility Standard Changes
|
||||||
| States | FY 2018 | FY 2019 | ||||
| (+) | (-) | (#) | (+) | (-) | (#) | |
| Alabama | X | |||||
| Alaska | ||||||
| Arizona | ||||||
| Arkansas | X | X | X | |||
| California | ||||||
| Colorado | X | |||||
| Connecticut | X | X | ||||
| Delaware | X | |||||
| DC | X | |||||
| Florida | X | |||||
| Georgia | ||||||
| Hawaii | ||||||
| Idaho | X | |||||
| Illinois | ||||||
| Indiana | X | X | X | |||
| Iowa | X | X | ||||
| Kansas | ||||||
| Kentucky | X | |||||
| Louisiana | ||||||
| Maine | X | X | ||||
| Maryland | X | |||||
| Massachusetts | X | |||||
| Michigan | X | |||||
| Minnesota | ||||||
| Mississippi | ||||||
| Missouri | X | X | ||||
| Montana | ||||||
| Nebraska | ||||||
| Nevada | ||||||
| New Hampshire | X | |||||
| New Jersey | X | |||||
| New Mexico | X | X | ||||
| New York | X | |||||
| North Carolina | ||||||
| North Dakota | ||||||
| Ohio | X | |||||
| Oklahoma | ||||||
| Oregon | ||||||
| Pennsylvania | X | |||||
| Rhode Island | ||||||
| South Carolina | X | |||||
| South Dakota | X | |||||
| Tennessee | ||||||
| Texas | ||||||
| Utah | X | X | ||||
| Vermont | X | |||||
| Virginia | X | X | ||||
| Washington | ||||||
| West Virginia | ||||||
| Wisconsin | ||||||
| Wyoming | ||||||
| Totals | 10 | 6 | 3 | 7 | 11 | 1 |
|
NOTES: From the beneficiary’s perspective, eligibility expansions or policies likely to increase Medicaid enrollment are denoted with (+), eligibility restrictions or policies likely to decrease enrollment are denoted with (-), and neutral changes are denoted with (#). This table captures eligibility changes that states have implemented or plan to implement in FY 2018 or FY 2019, including changes that are part of pending Section 1115 waivers. For pending waivers, only provisions planned for implementation before the end of FY 2019 (according to waiver application documents and/or interviews with state Medicaid staff) are counted in this table. Waiver provisions in pending waivers that states plan to implement in FY 2020 or after are not counted here. SOURCE: Kaiser Family Foundation Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2018. |
||||||
| State | Fiscal Year | Eligibility Changes |
| Alabama | 2019 | Parents & Caretaker Relatives (-): Pending Section 1115 Waiver: Add a work/community engagement requirement for non-disabled, non-pregnant individuals under age 60 (75,000 individuals). |
| Arkansas | 2018 | Expansion Adults (-) Approved Sec. 1115 Waiver: Limit retroactive coverage from 90 to 30 days.
Expansion Adults (-) Approved Sec. 1115 Waiver: Work requirement for expansion adults (40,000 individuals) (first case closures occurred 9/1/2018). Expansion Adults (#) Approved Sec. 1115 Waiver: End premium assistance program for employer sponsored insurance and transition individuals to QHP coverage (40 individuals). Children and Pregnant Women (+): Implement the CHIPRA option to eliminate the 5-year waiting period on Medicaid eligibility for lawfully-residing immigrant children and pregnant women. |
| Colorado | 2018 | Aged & Disabled (+): Medicaid buy-in option for individuals in support living services, spinal cord injury, & brain injury waivers (40 individuals). |
| Connecticut | 2018 | Parents & Caretaker Relatives (-): Reduce the income threshold for Husky A from 155% FPL to 138% FPL (12,000 individuals). |
| 2019 | Parents & Caretaker Relatives (+): Increase the income threshold for Husky A from 138% FPL to 155% FPL (12,000 individuals). | |
| Delaware | 2018 | Former Foster Youth (+) Approved Sec. 1115 Waiver: Add coverage for individuals who were in foster care and on Medicaid in another state at the time they aged out of the foster care system (under age 26 and under 133% FPL) (3 individuals). |
| District of Columbia | 2019 | Medically Needy (#): Clarification of Medically Needy eligibility criteria (with regard to countable medical expenditures) (7,000 individuals). |
| Florida | 2019 | Non-Pregnant Adults (-): Pending Sec. 1115 Waiver:Discontinue retroactive eligibility beyond the current application month. |
| Idaho | 2018 | Children (+): Cover children with serious emotional disturbance (SED) in families with income between 185% and 300% FPL (SED YES program) (2,000 to 10,000 children). |
| 2019 | Premiums (New): Children enrolled in the 1915(i) SED YES program will be subject to a premium in early 2019. | |
| Indiana | 2018 | Expansion Adults (-) Approved Sec. 1115 Waiver: Three-month lock-out of coverage following a 90-day period of disenrollment for failure to comply with redetermination.
Expansion Adults (#) Approved Sec. 1115 Waiver: End HIP Link premium assistance program for employer-sponsored insurance (enrollees will be moved to other HIP 2.0 coverage). Parents & Caretaker Relatives (#) Approved Sec. 1115 Waiver: Transitional Medical Assistance (TMA) is now for families in which a qualified HIP low-income parent/caretaker would otherwise fail financial eligibility due to new or increased earned income from a job or from self-employment exceeding the 133% FPL MAGI income limit. Premiums (Neutral) for Expansion and Other Adults Approved Sec. 1115 Waiver: Monthly POWER Account contributions are now tiered based on income. The tiered amounts, effective January 1, 2018, are $1.00, $5.00, $10.00, $15.00, and $20.00. |
| 2019 | Expansion and Other Adults (-) Approved Sec. 1115 Waiver: Work/community engagement requirement, phased implementation beginning 1/1/2019.
Premiums (New) for Expansion Population Approved Sec. 1115 Waiver: Add a 50% premium surcharge for tobacco users beginning in the second year of enrollment. |
|
| Iowa | 2018 | All Groups but Pregnant Women and Children Under Age 1 (-) Approved Sec. 1115 Waiver: Eliminate retroactive eligibility. |
| 2019 | Nursing Facility Residents (+): Reinstate 3-month retroactive eligibility for Medicaid-eligible nursing facility residents, effective July 1, 2018.
Premiums (New) Approved Section 1115 Waiver: Adults must complete healthy behaviors (preventive dental visit and health risk assessment) or pay a $3 monthly premium for the Dental Wellness Plan. |
|
| Kentucky | 2019 | Expansion Adults and Parents/Caretakers (-) Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering:14 Work/community engagement requirement.
Expansion Adults and Parents/Caretakers (-) Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering: Eliminate retroactive eligibility. Expansion Adults and Parents/Caretakers (-) Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering: Reasonable promptness waiver to delay coverage until the first day of the first month following receipt of the required premium. Expansion Adults and Parents/Caretakers (-) Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering: Disenrollment and lock-out of coverage if renewal is not completed timely. Expansion Adults and Parents/Caretakers (-) Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering: Disenrollment and lock-out of coverage if changes affecting eligibility are not reported timely. Expansion Adults (-) Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering: Disenrollment and lock-out of coverage for non-payment of premiums. Premiums (New) for Expansion Adults and Parents/Caretakers Sec. 1115 Waiver Approval Set Aside by Court, CMS Reconsidering: Up to 4% of income but at least $1. |
| Maine | 2019 | Adults (-) Pending Sec. 1115 Waiver: Add a work requirement for many groups of traditional adults. Those who do not comply with work requirement would be limited to no more than 3 months coverage in a 36-month period.
All Groups (-) Pending Sec. 1115 Waiver: Eliminate retroactive eligibility. Adults (-) Pending Sec. 1115 Waiver: Apply a $5,000 asset test to all coverage groups that do not currently have an asset test (under current law there is no asset test for coverage groups based solely on low income (vs. old age/disability)). All Groups (-) Pending Sec. 1115 Waiver: Eliminate hospital presumptive eligibility. Expansion Adults (+): Implement ACA Medicaid expansion (approved by referendum in November 2017) via a SPA.15 Premiums (New) for Adults Ages 19 to 64 Pending Sec 1115 Waiver: Premiums of between $10 and $40 per month, not to exceed 2% of income. |
| Maryland | 2019 | Adults (+): Increased income threshold for limited family planning benefit from 200% FPL to 250% FPL, remove age limit, and expanded coverage to include men. Switched from 1115 to SPA authority (9,000 individuals). |
| Massachusetts | 2019 | Adults (-) Approved Sec. 1115 Waiver: Eliminate 90-day period of provisional eligibility for adults under age 65 without verified income. The following groups will continue to be eligible for 90-day provisional eligibility pending verification of income: (1) pregnant women with self-attested MAGI income less than or equal to 200% FPL; (2) individual with HIV-positive status with self-attested MAGI income less than or equal to 200% FPL; or (3) individual in active treatment for breast or cervical cancer with self-attested MAGI income less than or equal to 250% FPL. (135,000).16 |
| Michigan | 2019 | Expansion Adults 100-138% FPL (-) Pending Sec. 1115 Waiver: Disenroll individuals for non-payment of required premiums after reaching 48 months of cumulative Healthy Michigan Plan eligibility.
Expansion Adults 100-138% FPL (-) Pending Sec. 1115 Waiver: Disenroll individuals for failure to complete an annual healthy behavior requirement after reaching 48 months of cumulative Healthy Michigan Plan eligibility. Premiums (Increased) Pending Sec. 1115 Waiver: Require premium of 5% of income for expansion population with incomes between 100% and 133% FPL. |
| Missouri | 2018 | Aged & Disabled (+): Asset limit increase (phased increase from FY 2018 through FY 2022) (2,865 individuals). |
| 2019 | Aged & Disabled (+): Asset limit increase (phased increase from FY 2018 through FY 2022) (992 individuals) | |
| New Hampshire | 2019 | Expansion Adults (-): Approved Sec. 1115 Waiver: Work/community engagement requirement for expansion population, implementation beginning 1/1/2019.
Expansion Adults (-): Approved Sec. 1115 Waiver: Eliminate retroactive eligibility for expansion population. |
| New Jersey | 2019 | Family Planning Enrollees (+): Expansion of family planning to cover men and women ages 19 to 65 between 138% and 205% FPL (over 30,000 individuals). |
| New Mexico | 2018 | Aged & Disabled (-): Home equity exclusion changed from the federal maximum of $840,000 to the federal minimum of $560,000 (fewer than 5 individuals). |
| 2019 | Family Planning (-) Pending Sec. 1115 Waiver: Limit family planning to age 51 and under (or under 65 with Medicare) (15,200 individuals).
Most Managed Care Members (-) Pending 1115 waiver: Limit retroactive Medicaid to one month for most managed care members (8,000 individuals). Expansion Adults (-): Pending Sec. 1115 Waiver: Reasonable promptness waiver to delay coverage until the first day of the first month following receipt of the required premium (pending CMS approval of proposed premiums). Expansion Adults (-): Pending Sec. 1115 Waiver: Disenrollment and lock-out of coverage for non-payment of premiums. Transitional Medical Assistance Parents/Caretakers (-): Pending Sec. 1115 Waiver: Eliminate TMA coverage pathway for parents/caretakers. Premiums for Expansion Adults above 100% FPL (New) Pending Sec. 1115 Waiver: New monthly premiums, which could be lowered under provisions of the healthy behavior incentive program. |
|
| New York | 2018 | Former Foster Youth (#): Eliminate coverage category for individuals under age 26 who were in foster care and on Medicaid in another state at the time they aged out of the foster care system (0 individuals in this category). |
| Ohio | 2019 | Expansion Adults (-): Pending Sec. 1115 Waiver: Work/community engagement requirement for Group VIII (expansion) MAGI adults (701,707 individuals). |
| Pennsylvania | 2018 | Children Under Age 4 (+): Continuous eligibility (7,746 children). |
| South Carolina | 2018 | Children & Pregnant Women (+): Implemented the CHIPRA option to eliminate the 5-year waiting period on Medicaid eligibility for lawfully-residing immigrant children and pregnant women. |
| South Dakota | 2019 | Adults in Minnehaha and Pennington Counties (-): Pending Sec. 1115 Waiver: Work/community engagement requirement, with offer of 12 months TMA and an additional 12 months premium assistance to individuals who continue to meet the work requirement but whose income increases above the Medicaid eligibility limit as a result of meeting the requirement (1,300 individuals). |
| Utah | 2018 | Parents & Caretakers (+): Increased the Basic Maintenance Standard to 55% FPL (3,000 individuals).
Adults (+) Approved Sec. 1115 Waiver: New eligibility group for chronically homeless, justice-involved individuals and those in need of substance abuse and/or mental health treatment, with income below 5% FPL (2,800 individuals). Adults (-) Approved Sec. 1115 Waiver: Eliminate retroactive eligibility for Primary Care Network (PCN) adults. Adults (+) Approved Sec. 1115 Waiver: Twelve months continuous eligibility for targeted childless adult population. |
| Vermont | 2018 | Aged & Disabled (+): Increased asset level for Working People with Disabilities program (from $5,000 to $10,000 for an individual and from $6,000 to $15,000 for a couple) (70 individuals). |
| Virginia | 2018 | Disabled (+) Approved Sec. 1115 Waiver: Increased eligibility from 80% to 100% FPL for waiver services for people with serious mental illness (GAP waiver program, full restoration to pre-2016 level) (2,000 adults with SMI). |
| 2019 | Expansion Adults (+): ACA expansion of eligibility to non-caretaker, low-income adults between 0% and 138% of FPL (400,000 individuals). |
Table 3: Corrections-Related Enrollment Policies in all 50 States and DC, in Place in FY 2018 And Actions Taken in FY 2019
| States | Medicaid Coverage For Inpatient Care Provided to Incarcerated Individuals | Medicaid Outreach/Assistance Strategies to Facilitate Enrollment Prior to Release^ | Medicaid Eligibility Suspended Rather Than Terminated For Enrollees Who Become Incarcerated^ | |||||||||
| Jails | Prisons | Jails | Prisons | Jails | Prisons | |||||||
| In place FY 2018 | New or Expanded FY 2019 |
In place FY 2018 | New or Expanded FY 2019 |
In place FY 2018 | New or Expanded FY 2019 |
In place FY 2018 | New or Expanded FY 2019 |
In place FY 2018 | New or Expanded FY 2019 |
In place FY 2018 | New or Expanded FY 2019 |
|
| Alabama | X | X | X | X | X | X | ||||||
| Alaska | X | X | X | X | X | X | ||||||
| Arizona | X | X | X | X | X | X | ||||||
| Arkansas | X | X | X | X | X | X | ||||||
| California | X | X | X | X | X | X | ||||||
| Colorado | X | X | X | X | X | X | ||||||
| Connecticut | X | X | X | X | X | X | ||||||
| Delaware | X | X | X | X | X* | X* | ||||||
| DC | X | N/A | N/A | X | X | X | N/A | N/A | ||||
| Florida | X | X | ||||||||||
| Georgia | X | |||||||||||
| Hawaii | X | X | X | X | ||||||||
| Idaho | X | X | ||||||||||
| Illinois | X | X | X | X | ||||||||
| Indiana | X | X | X | X | X | X | ||||||
| Iowa | X | X | X | X | X | |||||||
| Kansas | X | X* | X | |||||||||
| Kentucky | X | X | X | X | X | X | X | X | X | X | ||
| Louisiana | X | X | X* | X | X | X | ||||||
| Maine | X | X | X | X | ||||||||
| Maryland | X | X | X | X | X* | X | X | |||||
| Massachusetts | X | X | X | X | X | X | ||||||
| Michigan | X | X | X | X | X | X | ||||||
| Minnesota | X | X | ||||||||||
| Mississippi | X | X | X | |||||||||
| Missouri | X | X | X | X | ||||||||
| Montana | X | X | X | X | X | X | ||||||
| Nebraska | X | X | X | X | ||||||||
| Nevada | X | X | X | X | X | |||||||
| New Hampshire | X | X | X | X | X | X | ||||||
| New Jersey | X | X | X | X | X | X | ||||||
| New Mexico | X | X | X | X | X | X | ||||||
| New York | X | X | X | X | X | X | ||||||
| North Carolina | X | X | ||||||||||
| North Dakota | X | X | X | |||||||||
| Ohio | X | X | X | X | X | |||||||
| Oklahoma | X | |||||||||||
| Oregon | X | X | X | X | X | X | ||||||
| Pennsylvania | X | X | X | X | X | X | ||||||
| Rhode Island | X | X | X | X | X | X | ||||||
| South Carolina | X | X | X | X | X | X | ||||||
| South Dakota | X | X | X | X | ||||||||
| Tennessee | X | X | X | X | ||||||||
| Texas | X | X | X | X | X | |||||||
| Utah | X | X | X | X | X | X | ||||||
| Vermont | X | X | X | X | ||||||||
| Virginia | X | X | X | X | X | X | ||||||
| Washington | X | X | X | X | X | X | ||||||
| West Virginia | X | X | X | X | X | X | ||||||
| Wisconsin | X | X | X | X | ||||||||
| Wyoming | ||||||||||||
| Totals | 42 | 1 | 48 | 1 | 32 | 5 | 38 | 4 | 35 | 2 | 37 | 1 |
|
NOTES: ^States with “Medicaid outreach assistance strategies to facilitate enrollment prior to release” include those implementing a variety of strategies. In many cases, staff of the prison or jail provide most of the assistance in collaboration with the Medicaid agency. ^States that continue Medicaid eligibility for incarcerated individuals but limit covered benefits to inpatient hospitalization are also included in the count of states that suspend eligibility. “*” indicates that a policy was newly adopted in FY 2019, meaning that the state did not have any policy in that category/column in place in FY 2018. N/A: The District of Columbia has jails but no prisons (however, individuals returning to DC from federal prisons may be placed in residential re-entry centers and have the opportunity to apply for Medicaid from there in order to attain coverage for 24 hour inpatient care and to facilitate enrollment prior to release). SOURCE: Kaiser Family Foundation Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2018. |
||||||||||||