COVID-19 and Workers at Risk: Examining the Long-Term Care Workforce
The COVID-19 pandemic is presenting significant challenges for many segments of the health care industry. For the long-term care (LTC) industry, which includes facility settings such as skilled nursing facilities (SNFs) and assisted living facilities (ALFs), and home health (HH) providers, which deliver clinical and personal care services in the home, coronavirus infections are a grave concern for LTC providers and service users alike. Since the COVID-19 pandemic first surfaced in the United States, outbreaks in LTC facilities have been widespread, and it is estimated that about one-fifth of all deaths from COVID-19 are tied to nursing facilities. Older adults and people with underlying health conditions are more vulnerable to becoming severely ill if they become infected with the novel coronavirus, and the congregate nature of long-term care facilities, such as SNFs and ALFs, can increases risk of transmission.
The highly transmissible nature of the coronavirus combined with the congregate nature of LTC facility settings and the close and personal contact that many long-term care workers have with patients puts them at elevated risk of infection. For many LTC workers, the services they provide cannot be suspended without compromising the health and well-being of patients. This analysis focuses on the characteristics of the 4.5 million people who work in LTC settings, based on the 2018 American Community Survey (see Methods for details on the data and methods).
Key Findings
- The long-term care workforce consists of a variety of occupations and workers with different levels of direct day-to-day patient contact, but most of the 4.5 million LTC workers are in close, frequent contact with patients. Aides and personal care workers, who provide medical and/or personal care and come into direct and frequent contact with patients, account for 53% (2.4 million) of all LTC workers. Other LTC workers include non-clinical support staff (13%); health care providers, such as nurses, doctors, and therapists (14%); social workers and other behavioral health workers (3%); and other support workers and managers (16%).
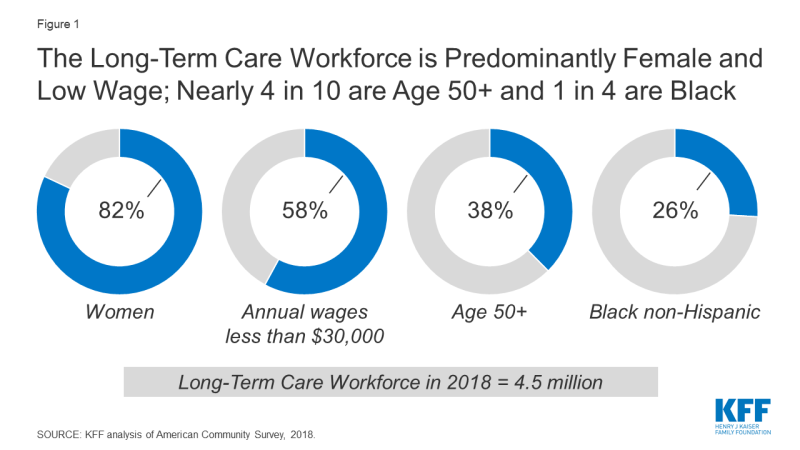
- LTC workers overall are disproportionately lower-wage workers. Nearly 6 in 10 (58%) LTC workers are in the bottom two wage quintiles for earners overall (i.e., the lowest paid 40% of workers), defined as those earning less than $30,000 in 2018, and only 8% are in the top quintile (workers earning above $73,000) (Figure 1).
- While most LTC workers are under 50 years of age, nearly 4 in 10 are 50 or older (38%), including 7% who are 65 and older. Among those LTC workers who most frequently come in direct contact with patients, 9% of direct contact support workers and 7% of aides and personal care workers are themselves age 65 or older, and based on their age alone are at risk of serious illness if infected.
- The vast majority of LTC workers are female (82%), and a disproportionate share are Black (26%). Among workers overall, only 48% are female and 12% are Black.
What Types of Jobs Do Long-Term Care Workers Have?
Of the 4.5 million long-term care workers included in this analysis, two-thirds work in facility settings – 42% (1.9 million) in SNFs and 25% (1.2 million) in residential care facilities such as ALFs – and one-third (33%, or 1.5 million) work in home health (see text box for further detail on these settings) (Figure 2).
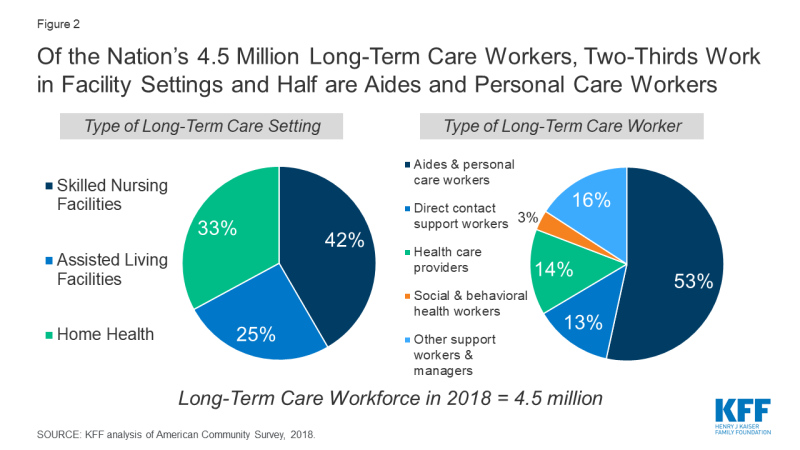
Figure 2: Of the Nation’s 4.5 Million Long-Term Care Workers, Two-Thirds Work in Facility Settings and Half are Aides and Personal Care Workers
Skilled nursing facilities (SNFs) provide round-the-clock nursing and personal care to residents who either need short-term rehabilitation following a hospitalization or injury or long-term care to residents with chronic medical and/or mental health conditions requiring access to 24-hour skilled care and assistance with activities of daily living (ADLs), or personal care. Residents of SNFs, especially those who stay long-term, are often elderly, bed-bound, and medically frail.
Assisted living facilities (ALFs) provide less-intensive care for a (typically elderly) population needing some assistance with personal care and instrumental activities of daily living (IADLs) such as housekeeping and meal preparation and basic medical services such as medication management.
Home health agencies provide skilled rehabilitative or post-acute care as well as long-term personal care for patients who do not require round-the-clock monitoring. The same skilled services provided by SNFs, such as nursing, occupational therapy (OT), and physical therapy (PT), are instead provided in the home, along with assistance with ADLs such as bathing, eating, and dressing, and some household activities such as meal preparation, medication management, and housekeeping.
The long-term care workforce consists of a variety of occupations and workers with different levels of direct day-to-day patient contact, but most LTC workers are in close, frequent contact with patients. We categorized LTC workers into five categories ranging from most to least patient contact:
- Aides and personal care workers (53% of all LTC workers) provide medical and/or personal care and come into direct and frequent contact with patients. Aides often have received some training or a state certification and may be asked to help residents with eating, bathing, and dressing as well as moving residents with limited mobility.
- Direct contact support workers (13% of all LTC workers) includes non-clinical support staff, such as maids/janitors, housekeeping and laundry, or food service workers, who do not provide medical or personal care but are likely to come into frequent contact with patients due to the nature of their work.
- Health care providers (14% of all LTC workers), such as registered nurses, nurse practitioners, physicians, and various types of therapists and technicians, provide direct (though possibly less frequent) clinical services to patients.
- Social workers and other behavioral health workers (3% of all LTC workers), including all providers of social work, counseling, and behavioral health services, provide less frequent but direct services to patients.
- Other support workers and managers (16% of all LTC workers), such as office and administrative managers and staff, receptionists, nutritionists, groundskeeping and facilities workers, are unlikely to come into regular direct contact with patients.
Not surprisingly, aides and personal care workers make up the largest category of the LTC workforce across all three settings, accounting for 72% of all HH workers, 49% of all SNF workers, and 37% of ALF workers (Table 1).
What Are the Job Characteristics of LTC Workers?
LTC workers overall are disproportionately lower-wage workers. Nearly 6 in 10 (58%) are in the bottom two wage quintiles for earners (i.e., the lowest paid 40% of workers), defined as workers earning less than $30,000 in 2018, and only 8% are in the top quintile (workers earning above $73,000). Among different categories of LTC workers, aides and personal care workers and direct contact support workers are much more likely to be low-wage earners; about one third of workers in each category (31% and 33%, respectively) are in lowest wage quintile, versus 12% or 13% for all other occupations (Figure 3). Across all care settings, 70% of aides and personal care workers earn less than the 40th percentile of overall worker earnings.
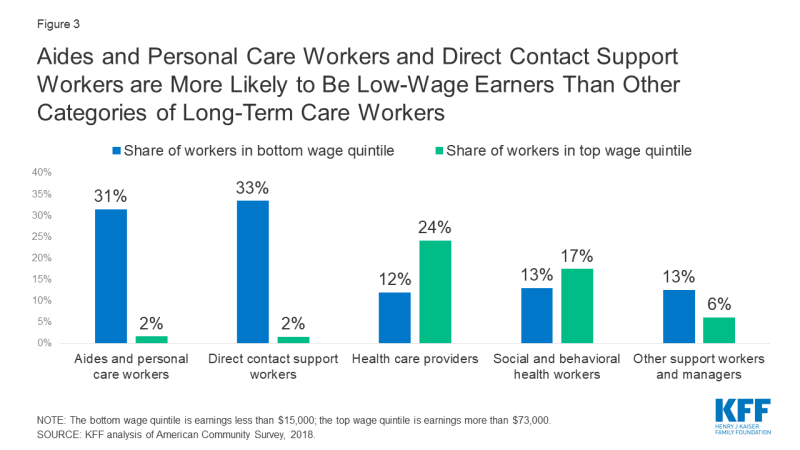
Figure 3: Aides and Personal Care Workers and Direct Contact Support Workers are More Likely to Be Low-Wage Earners Than Other Categories of Long-Term Care Workers
More than two-thirds of LTC workers overall (68%) are employed full time, but this varies somewhat by LTC setting and occupation. More than 70% of LTC workers in SNFs and ALFs are full-time workers, but just under 60% of home health workers work full time. A smaller share of aides and personal care workers (62%) and direct contract support workers (65%) are employed full time, compared to health care providers (74%), social and behavioral health workers (82%), and other support workers and managers (83%).
Overall, almost 6 in 10 LTC workers (56%) have employment-based health coverage, while 19% have Medicaid coverage, and 12% are uninsured, but insurance coverage varies by LTC setting and occupation. Among home health workers, 1 in 6 (16%) is uninsured, one fourth (25%) have Medicaid coverage, and fewer than half (43%) have employment-based coverage (either through their own job or as a dependent). The shares are similar among aides and personal care workers across all health care settings, with 15% uninsured, 26% covered by Medicaid, and 46% having employment-based coverage.
Who Works in the Long-Term Care Workforce?
While a majority of LTC workers are under 50 years of age (62%), nearly 4 in 10 are 50 or older (38%), including 7% who are 65 and older; the vast majority are female (82%); and a disproportionate share are Black (26%). Among those LTC workers who most frequently come in direct contact with patients, 10% of direct contact support workers and 7% of aides and personal care workers are themselves ages 65 and older (Table 2). Nearly half of aides and personal care workers are Black or Hispanic (32% and 16%, respectively) (Figure 4). Among workers overall, only 48% are female and 12% are Black.
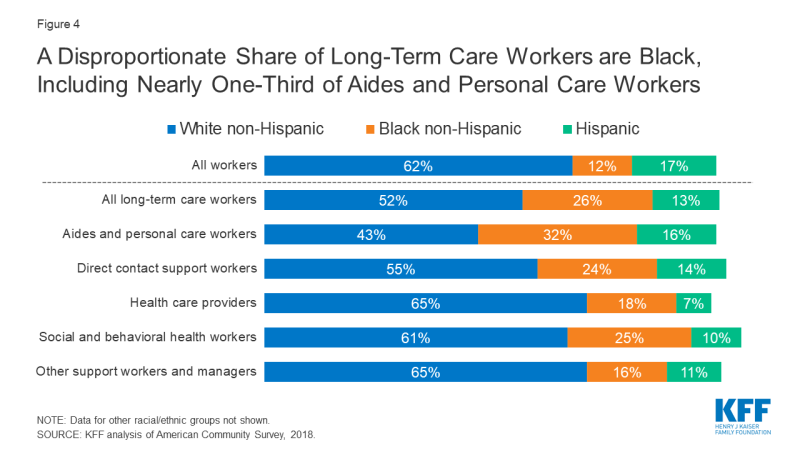
Figure 4: A Disproportionate Share of Long-Term Care Workers are Black, Including Nearly One-Third of Aides and Personal Care Workers
Nearly one third of LTC workers live in low-income families (families with combined earnings below twice the poverty level, or $26,200 for a family of four in 2020), and many have limited education to facilitate job opportunities. Nearly one-third (32%) live in a family with income below 200% of the poverty level, and nearly four in 10 (39%) have a high school diploma or less. Aides and personal care workers are more likely to live in poverty than other types of workers (15% versus 6%). A larger share of both aides and personal care workers and direct contact support workers have a high school diploma or less than LTC workers overall (48%, 60%, and 39%, respectively).
How Do Guidelines and Policies to Address COVID-19 Affect Long-Term Care Workers?
CMS Guidelines for LTC Facilities: The Centers for Medicare & Medicaid Services (CMS) has released guidance for long-term care facilities to help prevent coronavirus outbreaks from occurring. The guidance includes recommendations to comply with all infection-control guidance from CMS and CDC, restrict visitors and non-essential staff, screen staff for fever and respiratory symptoms at the start of their shifts, and require staff to wear personal protective equipment (PPE) when interacting with facility residents. CMS also has temporarily suspended routine inspections of nursing homes to refocus efforts on infection control deficiencies. Nearly 40% of all facilities had at least one infection control-related deficiency in 2017, and infection control continues to be the most commonly cited deficiency. Given the easily transmissible nature of the coronavirus, the focus on infection control efforts could help limit outbreaks in LTC facilities, protecting both LTC workers and residents alike.
Use of Personal Protective Equipment: Much attention has been paid to the needs of health care workers, particularly those who work in hospitals, in the context of the coronavirus pandemic. Shortages of PPE to protect front-line health care workers in inpatient settings has been a topic of particular concern raised by policymakers, the media, and health care workers themselves. Although coronavirus outbreaks in LTC facilities have been widespread since the crisis began, less attention has been paid to LTC workers’ access to PPE, despite reports of shortages in facilities. Home health workers, the majority of whom are low-wage aides, have been particularly overlooked in terms of their access to PPE, and many may be working without it.
The Centers for Disease Control and Prevention (CDC) has released a preparedness checklist for LTC facilities that recommends use of PPE by workers (among several other recommendations); however, this precaution may be difficult given current shortages. The recently passed Coronavirus Aid, Relief, and Economic Security (CARES) Act appropriates substantial federal funds to hospitals and other health care entities in order to offset the financial burden of the coronavirus pandemic, which could potentially be used to bolster PPE supplies, but the law does not allocate such funds to LTC facilities.
Medicaid Waiver Authority for HCBS: States are able to use Medicaid waiver authorities to support workers in home and community-based settings (HCBS). Under Section 1915(c) waiver Appendix K, states can increase Medicaid payment rates to home- and community-based providers to account for costs of medical supplies, including PPE and disinfectant supplies. Several states have specifically included provisions in their Appendix K waivers to cover supplies intended to protect HCBS workers. States may also use Appendix K to expand provider qualifications and allow previously unpaid caregivers, such family and neighbors, to receive payment. A number of states have also authorized retainer payments for HCBS providers in instances where their employing agency has closed or they are unable to enter a beneficiary’s home to minimize exposure risk.
Use of Telehealth for Home Health Services: CMS also has encouraged and expanded the use of telehealth instead of in-person visits for HCBS and Medicare home health services. CMS guidance on how states can use their Medicaid programs to cover telehealth services highlights that states have significant flexibility to deliver covered services through telehealth and provides policy options for states to reimburse Medicaid providers that provide telehealth services. States are able to use Appendix K waivers to expand telehealth services, with 22 states (as of April 16, 2020) allowing HCBS providers to provide care electronically for services such as case management, personal care services that require only verbal cues, and in-home habilitation. Providing HCBS and Medicare home health services via telehealth rather than face-to-face could reduce the potential for exposure among both LTC workers and users of these services.
Support and Economic Relief for Workers: While many low-wage workers are currently facing financial strain or job stress, LTC workers are likely facing added anxiety about their own health due to their higher risk of exposure to infection. In March, Congress passed the Family First Coronavirus Response Act (FFCRA), which provides two weeks paid leave for workers exposed to or who contract the novel coronavirus. However, the legislation stipulates that “health care providers,” including employees of nursing and retirement facilities, may be excluded from paid sick leave, and companies with over 500 or less than 50 employees may likewise be exempted. The CARES Act allocates up to $1,200 per person and $500 per child in the form of a one-time stimulus check intended to provide economic relief to households impacted by COVID-19. These funds may be particularly helpful for low-wage workers, including those in the LTC industry. Some lawmakers have signaled their support of hazard pay for health care and other essential workers facing increased risk of coronavirus infection, but it is unclear if such measures will garner sufficient support to become law.
Racial/Ethnic Disparities: Groups of color overall, and Black individuals in particular, are disproportionately represented among LTC workers. Groups of color also account for a disproportionate share of total COVID-19 cases in the U.S, and data indicates that groups of color face increased risk of severe illness if infected with coronavirus due to higher rates of certain underlying health conditions compared to White adults. For LTC workers of color, especially those who have frequent and direct contact with residents, the higher risk of infection they face as a result of their occupational duties may compound the risk that they face due to underlying health conditions. As policy continues to evolve to address both the health and economic consequences of the coronavirus pandemic, attention to the needs of the LTC workers who are providing ongoing health and personal care to older adults and people with disabilities may help protect both workers and patients alike.
| Methods |
| This analysis is based on KFF analysis of the 2018 American Community Survey (ACS), 1-year file. The ACS includes a 1% sample of the US population, the subset used here includes over 41,000 observations. The Long Term Care industry is defined as Home Health Care (8170), Nursing Care Facilities (8270), and Residential Care Facilities (8290). These industries capture the majority of workers providing long-term health services. They exclude some workers who may be providing ongoing non-health social services to individuals.
The ACS asks respondents about their health insurance coverage at the time of the survey. Respondents may report having more than one type of coverage; however, individuals are sorted into only one category of insurance coverage. We define the LTC workforce as all individuals who earned at least $1,000 during the year and indicated that their job was in one of the long term care industry codes listed above. Within these industry groups, we grouped people’s occupations into five different categories based on type of work and level of contact with patients. The five categories are:
Notably, the ACS does not include unpaid LTC caregivers, such as relatives and friends, who actually provide the majority of community-based long-term services and supports in the US. |