Data Note: How might Coronavirus Affect Residents in Nursing Facilities?
Introduction
While knowledge about COVID-19 continues to evolve daily, experts agree that certain populations are particularly vulnerable to severe cases of the infection – those with chronic conditions, compromised immune systems, and of old age. Nursing facilities provide care to populations with those characteristics, and residents in these facilities are particularly at risk of developing serious illness or dying if infected. In 2017, there were approximately 1.3 million residents receiving care across 15,483 nursing facilities in the US (Table 1). This data note provides key data points to highlight the potential implications of COVID-19 on nursing facility residents and overall operations.
Share of nursing home residents receiving respiratory treatment
Many residents in nursing facilities have underlying respiratory issues and may be at particular risk of illness should they contract coronavirus. One common symptom of coronaviruses is respiratory illness. About 16 percent of all residents in nursing facilities across the US received respiratory treatment in 2017, which includes using respirators/ventilators, oxygen, inhalation therapy, and other treatment. Given the implications of this virus on respiratory systems, these residents could be at higher risk of severe outcomes if they were to become infected. In states such as Colorado and Utah, over 30% of residents in nursing facilities are receiving respiratory treatment (Table 1). Ventilator supply is also crucial to consider, given the increased demand for this equipment for those severely impacted by COVID-19.
Share of nursing home residents with depression
Anxiety and depression are also common among nursing facility residents, and these health problems may be exacerbated by fear, worry, or social isolation due to COVID-19. Residents in nursing facilities are at risk of being diagnosed with psychiatric disorders, with nearly 40% having experienced symptoms of depression (Table 1). In Washington, where media attention has been centered on the outbreak of coronavirus in nursing facilities, almost half of residents have experienced depression or depressive symptoms. Research on family involvement in long-term care has shown that family visitation can have potentially positive effects on cognitive and behavioral health diagnoses.1 Thus, visitor restrictions in nursing facilities, which are currently being implemented to lower the risk of exposure among residents who would be vulnerable to illness if infected, may also have negative impacts on residents’ mental health and increase the incidence of depressive symptoms.2
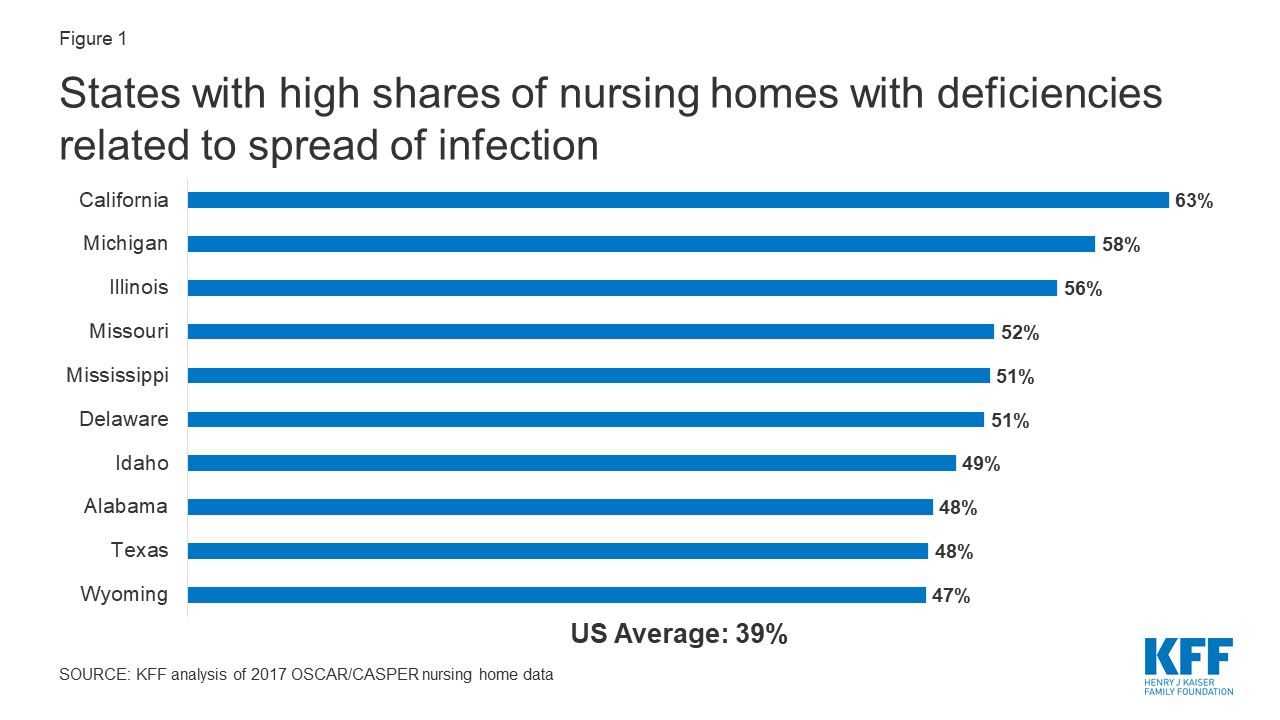
Share of nursing homes with deficiencies in infection control
Deficiencies related to the spread of infectious disease are relatively common in nursing facilities, with nearly 40% of facilities having at least one infection control deficiency in 2017 (Table 1). Deficiencies related to infection control are the most common deficiency that nursing facilities report, followed by food sanitation (36%) and accident environment (34%). In Delaware, Mississippi, Missouri, Illinois, Michigan, and California, over half of facilities reported at least one deficiency related to infection control (Table 1 and Figure 1). Given the importance of following infection control procedures in mitigating the spread of the virus, facilities that have historically reported infection control deficiencies could be at elevated risk of a COVID-19 outbreak.
Occupancy rates in nursing homes
Resident density could have an impact on how fast an outbreak of COVID-19 might spread in a particular facility. Nationally, four of every five nursing facility beds were filled in 2017, with some states such as New York and DC reporting even higher occupancy density (over 90%) (Table 1). Higher occupant density puts residents at risk of quicker spread.
In the early stages of the COVID-19 epidemic in the U.S., residents in nursing facilities have been affected more than any other group and account for a large share of deaths. These residents’ physical and mental health conditions, facilities’ abilities to deal with infectious disease, and occupancy rates are all important considerations when thinking about addressing the spread of COVID-19 in nursing homes and other vulnerable populations.
| Table 1: COVID-19 Related Nursing Home Data Indicators | ||||||
| State | Total number of nursing facilities | Total number of nursing facility residents | Share of residents in facilities receiving respiratory treatment | Share of residents in facilities with depression | Share of facilities with deficiencies related to infectious disease control | Facility occupancy rate |
| Alabama | 228 | 22,482 | 18% | 31% | 48% | 84% |
| Alaska | 18 | 608 | 12% | 35% | 33% | 88% |
| Arizona | 145 | 11,343 | 23% | 31% | 22% | 70% |
| Arkansas | 231 | 17,439 | 18% | 32% | 39% | 71% |
| California | 1198 | 101,030 | 16% | 23% | 63% | 85% |
| Colorado | 221 | 16,078 | 32% | 45% | 42% | 78% |
| Connecticut | 223 | 22,653 | 16% | 34% | 31% | 85% |
| Delaware | 45 | 4,181 | 15% | 32% | 51% | 87% |
| Dist. of Columbia | 18 | 2,380 | 14% | 24% | 39% | 92% |
| Florida | 690 | 72,741 | 17% | 32% | 42% | 87% |
| Georgia | 359 | 33,043 | 14% | 41% | 19% | 83% |
| Hawaii | 42 | 3,474 | 10% | 24% | 43% | 85% |
| Idaho | 71 | 3,319 | 28% | 49% | 49% | 63% |
| Illinois | 731 | 66,643 | 14% | 52% | 56% | 74% |
| Indiana | 552 | 38,682 | 15% | 41% | 35% | 73% |
| Iowa | 437 | 23,638 | 15% | 46% | 22% | 77% |
| Kansas | 276 | 14,657 | 18% | 47% | 34% | 77% |
| Kentucky | 285 | 22,760 | 20% | 36% | 37% | 85% |
| Louisiana | 277 | 26,169 | 12% | 26% | 29% | 77% |
| Maine | 100 | 5,947 | 13% | 49% | 15% | 87% |
| Maryland | 226 | 24,414 | 14% | 37% | 40% | 87% |
| Massachusetts | 399 | 38,673 | 11% | 38% | 30% | 84% |
| Michigan | 443 | 38,062 | 16% | 34% | 58% | 81% |
| Minnesota | 375 | 24,755 | 15% | 46% | 40% | 86% |
| Mississippi | 204 | 15,950 | 12% | 27% | 51% | 88% |
| Missouri | 518 | 37,874 | 16% | 38% | 52% | 70% |
| Montana | 72 | 4,153 | 20% | 43% | 42% | 65% |
| Nebraska | 214 | 11,394 | 18% | 50% | 31% | 72% |
| Nevada | 61 | 5,336 | 27% | 29% | 38% | 76% |
| New Hampshire | 74 | 6,442 | 15% | 41% | 26% | 87% |
| New Jersey | 364 | 44,033 | 16% | 25% | 31% | 84% |
| New Mexico | 74 | 5,693 | 24% | 39% | 36% | 79% |
| New York | 609 | 101,518 | 14% | 38% | 20% | 90% |
| North Carolina | 429 | 35,763 | 16% | 33% | 17% | 81% |
| North Dakota | 80 | 5,531 | 15% | 51% | 34% | 91% |
| Ohio | 966 | 73,826 | 17% | 52% | 28% | 82% |
| Oklahoma | 303 | 18,361 | 18% | 42% | 30% | 64% |
| Oregon | 136 | 7,317 | 17% | 32% | 33% | 65% |
| Pennsylvania | 693 | 76,652 | 18% | 36% | 46% | 87% |
| Rhode Island | 83 | 7,817 | 9% | 44% | 5% | 90% |
| South Carolina | 191 | 16,993 | 14% | 31% | 21% | 86% |
| South Dakota | 108 | 5,984 | 18% | 54% | 43% | 90% |
| Tennessee | 314 | 26,481 | 19% | 35% | 31% | 73% |
| Texas | 1,227 | 92,250 | 12% | 37% | 48% | 69% |
| Utah | 99 | 5,178 | 32% | 48% | 43% | 63% |
| Vermont | 36 | 2,440 | 14% | 49% | 14% | 79% |
| Virginia | 286 | 27,595 | 18% | 35% | 38% | 86% |
| Washington | 217 | 15,993 | 17% | 46% | 43% | 77% |
| West Virginia | 123 | 9,251 | 18% | 40% | 42% | 87% |
| Wisconsin | 374 | 24,239 | 15% | 45% | 38% | 77% |
| Wyoming | 38 | 2,428 | 29% | 47% | 47% | 82% |
| US TOTAL | 15,483 | 1,321,663 | 16% | 37% | 39% | 80% |
| SOURCES: KFF analysis of 2017 OSCAR/CASPER nursing facility data | ||||||
Endnotes
Gaugler, Joseph E. "Family involvement in residential long-term care: A synthesis and critical review." Aging & mental health 9.2 (2005): 105-118.
Vernon L. Greene, PhD, Deborah J. Monahan, MA, The Impact of Visitation on Patient Well-Being in Nursing Homes, The Gerontologist, Volume 22, Issue 4, August 1982, Pages 418–423