Disparities in Health and Health Care: 5 Key Questions and Answers
There has been heightened focus on health disparities and their underlying causes in recent years. These disparities are not new and reflect longstanding structural and systemic inequalities rooted in contemporary and historical racism and discrimination. This brief provides an introduction to what health and health care disparities are, why it is important to address them, what the status of disparities is today, recent federal actions to address disparities, and key issues related to addressing disparities in the future. More detailed information on this topic can be found in KFF’s Health Policy 101 chapter on Race, Inequality, and Health.
What are Health and Health Care Disparities?
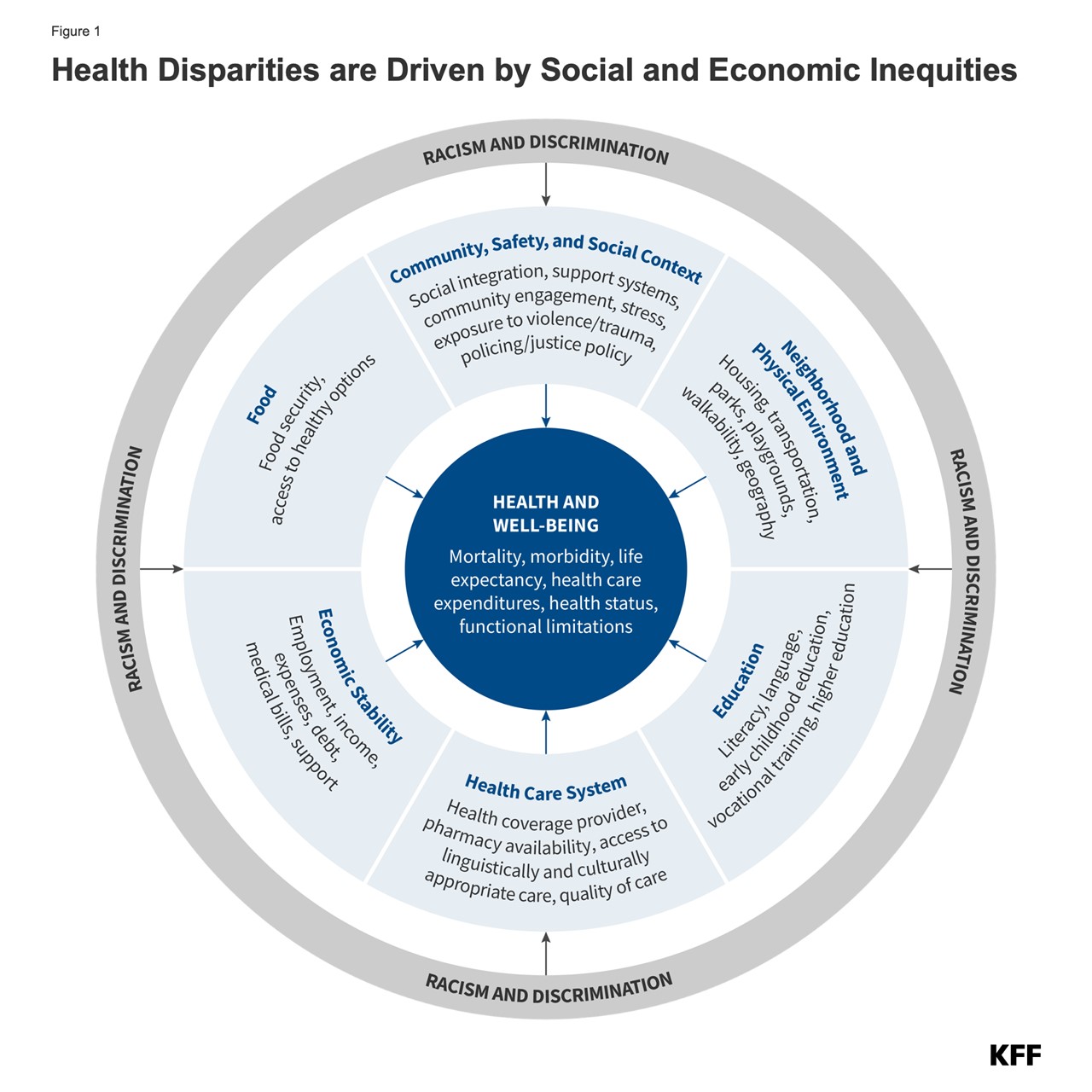
Health and health care disparities refer to differences in health and health care between groups that stem from broader social and economic inequities (Figure 1). Health disparities include differences in health outcomes, such as life expectancy, mortality, health status, and prevalence of health conditions. Health care disparities include differences between groups in measures such as health insurance coverage, affordability, access to and use of care, and quality of care. Disparities occur across multiple factors including race and ethnicity, socioeconomic status, age, geography, language, gender, disability status, citizenship status, and sexual identity and orientation. Reflecting the intersectional nature of people’s identities, some individuals experience disparities across multiple dimensions. The U.S. has a long history of exclusionary policies and events that have driven and continue to contribute to racial and ethnic disparities in health today.
Why is it Important to Address Disparities?
Addressing disparities in health and health care is important from an equity standpoint and for improving the nation’s overall health and economic prosperity. Racial and ethnic health disparities result in higher rates of illness and death across a wide range of health conditions. Research shows that these disparities are costly, resulting in excess medical care costs and lost productivity, as well as additional economic losses due to premature deaths. In addition, it is increasingly important to address health disparities as the population becomes more diverse. The U.S. Census Bureau projects that people of color will account for over half (52%) of the population by 2050, with the largest growth occurring among people who identify as Asian or Hispanic (Figure 2).
What is the Status of Disparities Today?
Despite the recognition and documentation of disparities for decades and overall improvements in population health over time, many disparities persist, and in some cases, have widened over time. Analysis across a broad range of measures of health finds that Black and American Indian or Alaska Native (AIAN) people fare worse than their White counterparts across half or more of these measures including infant mortality, pregnancy-related mortality, diabetes mortality, and cancer mortality. Data for Hispanic people are more mixed relative to White people, which reflects that some subgroups, such as recent immigrants, generally fare better on health outcomes despite faring worse on many measures of health access and social and economic factors that influence health. Asian people on aggregate fare the same or better than White people on most measures of health, but there are some subgroups of the population that face significant disparities. Disaggregated data for Native Hawaiian or Pacific Islander (NHPI) people are limited, but available data show that they fare worse than White people across the majority of examined measures.
Disparities in health occur across the life course. Black infants were more than two times as likely to die as White infants (10.9 vs. 4.5 per 1,000 live births), and AIAN (9.1 per 1,000 live births) and NHPI (8.5 per 1,000 live births) infants were roughly twice as likely to die as White infants in 2022 (Figure 3). Hispanic infants (4.9 per 1,000 live births) also have a slightly higher mortality rate than White infants. NHPI (62.8 per 100,000), Black (39.9 per 100,000) and AIAN (32 per 100,000) women had the highest rates of pregnancy-related mortality between 2017 and 2019. In 2022, the age-adjusted mortality rates for diabetes for NHPI (49.9 per 100,000), AIAN (47.7 per 100,000), and Black (42.9 per 100,000) people were about twice as high as the rate for White people (21.3 per 100,000); Hispanic people also had a higher diabetes death rate compared to White people (28.3 per 100,000). AIAN and Black people have consistently had a shorter life expectancy than White people, with gaps widening during the COVID-19 pandemic. Based on provisional data for 2022, life expectancy for Black people was about five years shorter than White people (72.8 vs. 77.5), and nearly ten years shorter for AIAN people (67.9).
There also are ongoing disparities in health coverage and access to care. For example, nonelderly AIAN, Black, Hispanic, and NHPI people are more likely to be uninsured than their White counterparts despite large gains in coverage since the Affordable Care Act (Figure 4).
What are Recent Federal Actions to Address Disparities?
Early in his presidency, President Biden issued a series of executive orders focused on advancing health equity and directing federal agencies to develop Equity Action Plans. The Centers for Medicare and Medicaid (CMS) released an updated framework to advance health equity for people covered by Medicare, Medicaid, the Children’s Health Insurance Program (CHIP) and the Health Insurance Marketplaces. The Administration and Congress took a range of actions to stabilize and increase access to health coverage amid the pandemic, with some extending beyond the Public Health Emergency and others ending; this included a temporary requirement of continuous enrollment in Medicaid which came to an end on March 31, 2023, with millions of Medicaid enrollees being disenrolled since. There has also been a growing focus by the Biden Administration on addressing maternal health disparities and increasing the availability of disaggregated racial and ethnic data to better identify and address disparities.
The Biden Administration also expanded the Child Tax Credit, which has contributed to reductions in child poverty and improvements in health and well-being. The Biden Administration temporarily increased the Child Tax Credit (CTC) as part of the American Rescue Plan in 2021. Research shows that this expansion was associated with significant reductions in child poverty rates for Black and Hispanic children and that it will likely lead to short- and long-term benefits for children’s health and well-being, particularly poor and younger children, stemming from improved outcomes associated with increased parental income. However, the expansion expired at the end of 2021, and poverty rates rebounded. A bipartisan bill that would provide a Child Tax Credit expansion primarily to children in low-income families is pending, although its future remains uncertain.
What are Key Issues Related to Health Disparities Looking Ahead?
Growing mental health needs, increasing climate-related health risks, policy changes, and the outcome of the 2024 presidential election will all have important implications for future efforts to address disparities. People of color face disproportionate barriers to accessing mental health care and there also have been large increases in drug overdose death rates for AIAN, Black, and Hispanic people compared to White people between 2019 and 2022, amplifying the focus on disparities in mental health. Growing climate-related health impacts may exacerbate disparities given their disproportionate impacts on marginalized communities. In addition, evolving federal and state policies related to reproductive health, Medicaid, and immigration impact disparities. For example, state variation in access to abortion in the wake of the Dobbs decision may exacerbate the already large racial disparities in maternal health. Coverage losses following the end of the Medicaid continuous enrollment provision may lead to widening disparities in coverage due to people of color being more likely to be covered by Medicaid. In addition, proposals to convert federal Medicaid funds to per capita caps or block grants could further exacerbate disparities in access to health coverage. On the other hand, take-up of the ACA Medicaid expansion in the remaining states that have not yet expanded as well as other Medicaid initiatives could narrow disparities. Evolving immigration policies may impact health care access for immigrants, who are more likely than U.S.-born people to be uninsured and to face challenges accessing health care. Finally, the 2024 presidential election will have far-reaching implications for these and other key health policy areas.
