State Medicaid Programs Respond to Meet COVID-19 Challenges: Results from a 50-State Medicaid Budget Survey for State Fiscal Years 2020 and 2021
Benefits, Cost-Sharing, and Telehealth
Prior to the COVID-19 pandemic, the most common state changes to Medicaid benefits were enhancements of mental health and substance use disorder (SUD) services. In recent years, the number of states reporting benefit expansions outpaced the number of states reporting benefit restrictions. For FY 2019 and FY 2020, more states reported policies to eliminate or reduce cost-sharing requirements than those that reported new or increased cost-sharing requirements.1 The COVID-19 pandemic has shifted state priorities for Medicaid benefits and cost-sharing, with states utilizing Medicaid emergency authorities to adopt new benefits, adjust existing benefits, and/or waive prior authorization requirements.2
In particular, states have focused on expanding telehealth access for Medicaid beneficiaries to increase health care accessibility and limit risk of exposure during the pandemic.3 Prior to the pandemic, the use of telehealth in Medicaid was becoming more common and all states had some form of Medicaid coverage for services delivered via telehealth; however, the scope of this coverage varied widely across states and many included restrictions on allowable services, providers, and originating sites.4 In response to COVID-19, states have utilized Medicaid emergency authorities to expand telehealth5 as well as taken advantage of broad authority to further expand telehealth without the need for CMS approval. To guide states considering telehealth expansions, CMS released a State Medicaid & CHIP Telehealth Toolkit on April 23, 2020 which identified key areas of telehealth for state consideration, including what services can be delivered via telehealth; what kinds of sites can serve as originating sites (patient location); payment rates for services; technological modalities that can be used to deliver services; and whether Medicaid managed care organizations (MCOs) are required to cover all services that are available in fee-for-service (FFS) Medicaid.6
Survey Findings
We asked states about non-emergency benefit and cost-sharing changes unrelated to COVID-19 planned for FY 2021. Further, to better understand the impact of COVID-19 on Medicaid benefit design and coverage policy, we asked about emergency benefit and cost-sharing changes made in response to the pandemic and, specifically, whether states planned to adopt the changes on a more permanent basis. Finally, we asked states about recent changes in FFS telehealth coverage policy and whether these changes were likely to continue past the public health emergency (PHE) period.
Non-Emergency Changes to Benefits and Cost-Sharing
Less than one-third of responding states plan to make benefit or cost-sharing changes that are not related to the COVID-19 pandemic in FY 2021 (12 states). Many states have not determined whether they will adopt any non-emergency benefit or cost-sharing changes (12 states), with at least one state noting that uncertainty regarding the length of the PHE period and its budgetary impact is a barrier to determining FY 2021 benefit and cost-sharing changes. Key reported changes for FY 2021, excluding telehealth coverage changes, include the following:
- Seven states are adding or expanding benefits (Alaska, California, Hawaii, Idaho, Montana, Texas, and Wisconsin). Reported benefit changes include expanded home and community-based (HCBS) services as well as behavioral health (BH) and SUD services, consistent with findings in prior years.7
- Two states are eliminating or restricting benefits (Alaska and Wyoming). Alaska is adding prior authorization requirements for benefits that include non-preventive dental, vision, and therapies. Wyoming is removing its chiropractic benefit for all individuals, limiting some HCBS services, and reducing its adult vision and dental benefits.
- Four states (Colorado, Idaho, Michigan, and South Dakota) will be implementing new or expanded co-payments for a variety of services, or other cost-sharing. Idaho and Michigan report that these changes will apply to the Medicaid expansion population.
- Two states (California and Massachusetts) will be eliminating or reducing certain co-payments in FY 2021.
Benefit Changes in Response to COVID-19
Approximately one-third of responding states intend to extend other benefit and cost-sharing changes adopted during the PHE period (15 states); many of these are pharmacy changes. (See the Pharmacy Cost Containment Actions section of this report for more information on state pharmacy changes.) Similar numbers of states said they would not extend changes adopted in response to the PHE (15 states) or that they had not yet determined whether the changes would be extended (13 states). The benefit changes states were most likely to extend beyond the PHE period include covering a 90-day drug supply (five states), relaxing various documentation and other authorization or referral requirements to qualify for long-term care or HCBS (six states), and relaxing or waiving certain prior authorization requirements for some services (five states). A few states also indicated they would retain other pharmacy changes, including paying for prescription deliveries (two states), allowing pharmacists to administer medications and/or vaccines (two states), and covering additional types of medication (two states).
Telehealth Policy Changes in Response to COVID-19
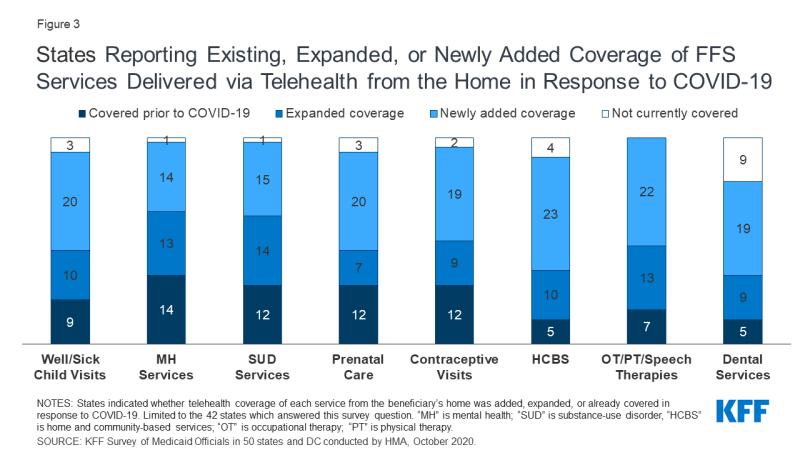
Figure 3: States Reporting Existing, Expanded, or Newly Added Coverage of FFS Services Delivered via Telehealth from the Home in Response to COVID-19
The majority of responding states report covering a range of FFS services delivered via telehealth when the originating site is the beneficiary’s home; most of these states newly added or expanded this coverage in response to the COVID-19 pandemic (Figure 3). States most commonly reported adding or expanding telehealth delivery from the beneficiary’s home for occupational therapy (OT), physical therapy (PT), and speech therapy (35 states), followed by home and community-based services (HCBS) (33 states) and well/sick child visits (30 states). Several states noted they had utilized Section 1915 (c) Appendix K emergency authority to expand telehealth in their HCBS waivers.8
Most states reported that FFS services delivered via telehealth from the beneficiary’s home have payment parity as compared to services delivered face-to-face. Payment parity for telehealth increases access for patients by incentivizing providers to offer services delivered via telehealth.9 Most states reported that reimbursement was the same for telehealth and in-person delivery of all FFS services asked about (well/sick child visits, mental health services, SUD services, prenatal care, contraceptive visits, HCBS, OT/PT/speech therapies, and dental services).
Just over half of responding states report plans to extend newly added/expanded FFS telehealth coverage when the beneficiary’s home is the originating site beyond the PHE period (Figure 4 and Table 3). Twenty-two states report that they will continue newly added/expanded telehealth coverage, at least in part and at least for some services. For most services with newly added/expanded coverage, however, the majority of states have not yet determined whether this coverage will continue beyond the PHE period. (See the Long-Term Services and Supports section for more information on state plans to retain telehealth or remote provision of long-term services and supports including HCBS after the end of the PHE).
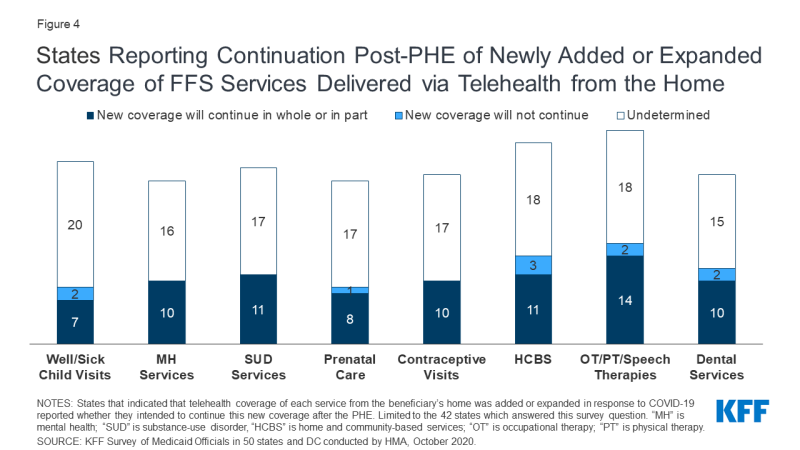
Figure 4: States Reporting Continuation Post-PHE of Newly Added or Expanded Coverage of FFS Services Delivered via Telehealth from the Home
States also reported other policies aimed at making telehealth widely accessible in response to COVID-19. Thirty-nine out of 42 responding states expanded available telehealth modalities in response to the pandemic, with telephone (or voice-only) most frequently reported. As one state noted, this expansion is important because beneficiaries may lack access to broadband internet. States also reported covering digital platforms, such as FaceTime, Zoom, and Skype. At least two states, Florida and Virginia, began allowing remote patient monitoring as a type of newly expanded telehealth service delivery. All responding states that contract with managed care organizations (MCOs) required MCOs to implement newly adopted FFS telehealth changes; three of these states required MCOs only to implement FFS telehealth changes in part. Tennessee, a state with 100% of its beneficiaries enrolled in managed care, indicated it worked closely with its MCOs to coordinate and increase use of telehealth.10 In Minnesota, some contracted MCOs cover virtual e-visits as an “in lieu of” services.11
TABLE 3: STATES PLANNING TO CONTINUE NEWLY ADDED OR EXPANDED COVERAGE OF FFS SERVICES DELIVERED VIA TELEHEALTH FROM THE BENEFICIARY’S HOME
|
Does State Plan to Continue Newly Added/Expanded Telehealth Coverage From the Home Post-PHE?
|
||||||||
|
States
|
Well/Sick Child Visits
|
Mental Health Services
|
SUD Services
|
Prenatal Care Visits
|
Contraceptive Visits
|
HCBS
|
OT, PT, Speech Therapies
|
Dental Services
|
|
Alabama
|
?
|
?
|
?
|
?
|
?
|
?
|
?
|
?
|
|
Alaska
|
NA
|
?
|
?
|
?
|
?
|
Yes, in part
|
Yes, in part
|
NA
|
|
Arizona
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
NA
|
NA
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
|
Arkansas
|
?
|
?
|
?
|
?
|
?
|
NA
|
?
|
NA
|
|
California
|
?
|
Covered Pre-PHE
|
?
|
Covered Pre-PHE
|
Covered Pre-PHE
|
?
|
Covered Pre-PHE
|
?
|
|
Colorado
|
NA
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Yes
|
Yes
|
?
|
|
Connecticut
|
?
|
Covered Pre-PHE
|
Covered Pre-PHE
|
?
|
?
|
Yes, in part
|
?
|
NA
|
|
Delaware*
|
||||||||
|
DC*
|
||||||||
|
Florida
|
?
|
?
|
?
|
NA
|
?
|
?
|
?
|
Covered Pre-PHE
|
|
Georgia
|
?
|
?
|
?
|
?
|
?
|
Covered Pre-PHE
|
?
|
Covered Pre-PHE
|
|
Hawaii
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
NA
|
?
|
?
|
|
Idaho
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
?
|
|
Illinois*
|
||||||||
|
Indiana
|
?
|
Yes, in part
|
Yes, in part
|
?
|
?
|
?
|
Yes, in part
|
NA
|
|
Iowa
|
?
|
?
|
?
|
?
|
?
|
?
|
?
|
Yes
|
|
Kansas
|
NA
|
?
|
?
|
NA
|
NA
|
?
|
?
|
NA
|
|
Kentucky
|
?
|
?
|
?
|
?
|
Covered Pre-PHE
|
?
|
Covered Pre-PHE
|
?
|
|
Louisiana
|
?
|
NA
|
NA
|
?
|
?
|
?
|
?
|
?
|
|
Maine
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Yes
|
Covered Pre-PHE
|
Yes
|
|
Maryland
|
||||||||
|
Massachusetts
|
Yes
|
Yes
|
Yes
|
Yes
|
Yes
|
?
|
Yes
|
?
|
|
Michigan
|
Yes
|
Yes
|
Yes
|
Yes
|
Yes
|
?
|
?
|
?
|
|
Minnesota
|
?
|
?
|
?
|
?
|
?
|
?
|
?
|
?
|
|
Mississippi
|
?
|
?
|
?
|
?
|
?
|
?
|
?
|
NA
|
|
Missouri
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Yes
|
Yes
|
|
Montana
|
Covered Pre-PHE
|
?
|
?
|
Covered Pre-PHE
|
Covered Pre-PHE
|
?
|
Covered Pre-PHE
|
Yes
|
|
Nebraska
|
?
|
Yes, in part
|
Yes, in part
|
?
|
?
|
NA
|
Yes, in part
|
Yes, in part
|
|
Nevada
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
?
|
?
|
Covered Pre-PHE
|
|
New Hampshire
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
|
New Jersey
|
?
|
?
|
?
|
?
|
?
|
?
|
?
|
?
|
|
New Mexico*
|
||||||||
|
New York*
|
||||||||
|
North Carolina
|
No
|
Yes, in part
|
Yes, in part
|
No
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
No
|
|
North Dakota
|
?
|
?
|
?
|
?
|
?
|
No
|
?
|
NA
|
|
Ohio*
|
||||||||
|
Oklahoma
|
No
|
Yes, in part
|
Yes, in part
|
Yes
|
Yes
|
Yes
|
No
|
No
|
|
Oregon
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
Yes, in part
|
Yes
|
Yes, in part
|
Yes, in part
|
|
Pennsylvania
|
Yes
|
Yes, in part
|
Yes, in part
|
Yes
|
Yes
|
?
|
Yes
|
Yes
|
|
Rhode Island*
|
||||||||
|
South Carolina
|
?
|
?
|
?
|
?
|
?
|
No
|
?
|
?
|
|
South Dakota
|
?
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
NA
|
Yes, in part
|
?
|
|
Tennessee
|
||||||||
|
Texas
|
?
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
No
|
No
|
NA
|
|
Utah*
|
||||||||
|
Vermont
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
|
Virginia
|
?
|
?
|
?
|
?
|
?
|
?
|
?
|
Yes
|
|
Washington
|
Yes, in part
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Yes, in part
|
Covered Pre-PHE
|
Covered Pre-PHE
|
?
|
|
West Virginia
|
?
|
?
|
?
|
?
|
?
|
?
|
?
|
?
|
|
Wisconsin
|
Yes
|
Yes
|
Yes, in part
|
Yes
|
Yes
|
Yes, in part
|
Yes
|
Yes, in part
|
|
Wyoming
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Covered Pre-PHE
|
Yes, in part
|
Yes, in part
|
NA
|
|
Yes, in all or part
|
7
|
10
|
11
|
8
|
10
|
11
|
14
|
10
|
|
No
|
2
|
0
|
0
|
1
|
0
|
3
|
2
|
2
|
|
Undetermined (?)
|
20
|
16
|
17
|
17
|
17
|
18
|
18
|
15
|
|
Covered Pre-PHE
|
9
|
14
|
12
|
12
|
12
|
5
|
7
|
5
|
|
NA, not covered
|
3
|
1
|
1
|
3
|
2
|
4
|
0
|
9
|
|
NOTES: States were asked whether newly added/expanded FFS telehealth coverage of each service from the beneficary’s home would continue after the PHE. SUD: Substance-use disorder. HCBS: Home and community-based services. OT: Occupational therapy. PT: Physical therapy. NA: State does not cover this service delivered via telehealth from the beneficiary’s home. Covered Pre-PHE (pre-public health emergency): the state covers this service delivered via telehealth from the beneficary’s home, but this coverage was not newly added/expanded in response to the PHE. “?” indicates that the state has newly added or expanded coverage of this service delievered via telehealth from the beneficiary’s home in response to the PHE, but has not yet determined whether to continue this coverage. “”*” indicates the state did not submit a survey by mid-August 2020 (DC, DE, IL, NM, NY, OH, RI, UT). Additionally, MD and TN submitted surveys but did not report data for this question.
SOURCE: KFF Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2020 |
||||||||
