Medicaid Coverage of Pregnancy and Perinatal Benefits: Results from a State Survey
An updated version of this report was released on May 19, 2022 and can be found here.
Correction: While KY and MS responded to the survey that their states cover doula services, subsequent research has found that the states do not cover doula services. To our knowledge, OR and MN, and as of January 2021, NJ, are the only states currently covering doula services.
Overview
Maternity care has emerged as a key issue in the current policy debates about the future of the Affordable Care Act (ACA) and Medicaid restructuring. While the inclusion of maternity care as an essential health benefit has been important to many women who gained private coverage because of the ACA coverage expansion, Medicaid has been the primary funding source for perinatal and maternal services for low-income women in the US for several decades. In 2010, Medicaid financed nearly 45% of all births in the United States.1 By federal law, all states provide Medicaid coverage for pregnancy-related services to pregnant women with incomes up to 133% of the federal poverty level (FPL) and cover them up to 60 days postpartum. All states must provide some level of maternity care free of cost-sharing to eligible pregnant women, although there are state level variations in the scope and type of services that states offer. In addition, many states extend eligibility to pregnant women with incomes considerably higher than this threshold. The ACA broadened Medicaid eligibility by allowing states to extend continuous Medicaid eligibility in 2014 to individuals with family income at or below 138% FPL and 31 states and the District of Columbia (DC) have adopted Medicaid expansion programs which extended coverage for new mothers beyond the postpartum period, where historically many women lost coverage. 2
Because there is no formal federal definition of what services states must cover for pregnant women beyond inpatient and outpatient hospital care, states have considerable discretion to determine the specific scope of maternity care benefits. While the ACA also does not define maternity benefits, states that have expanded Medicaid eligibility under the ACA must cover all preventive services recommended by the United States Preventive Services Task Force (USPSTF) for beneficiaries that qualify as a result of the ACA expansion. These now include many pregnancy-related services, such as prenatal screenings, folic acid supplements, and breastfeeding supports for those who qualify for Medicaid as a result of the expansion. This coverage requirement, however, does not apply to any of the Medicaid eligibility pathways that were available prior to the ACA (i.e., for parents or pregnant women). As a result, there is leeway for states to vary coverage standards for different Medicaid eligibility pathways (e.g. traditional Medicaid available prior to the ACA, ACA Medicaid expansion, or pregnancy-related eligibility).
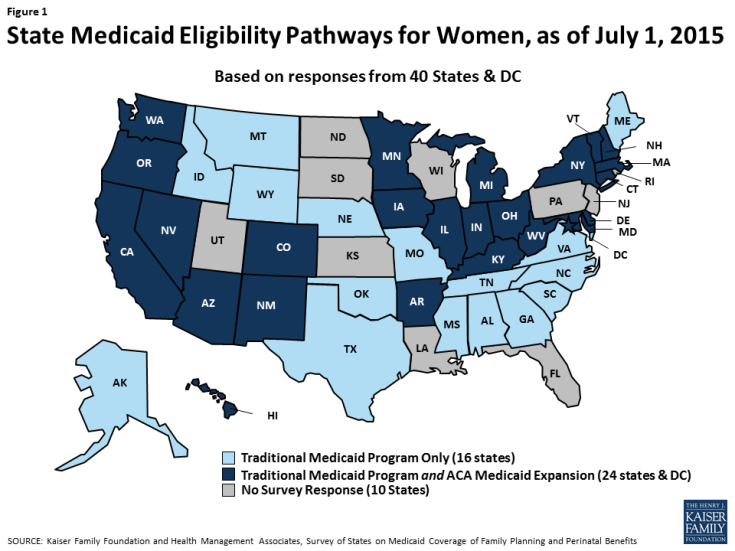
To understand how states were covering services under Medicaid in the wake of the ACA expansions, the Kaiser Family Foundation and Health Management Associates conducted a survey of states about the status of Medicaid benefit policies for perinatal and family planning services across the nation. With 31 states and DC adopting Medicaid expansions, the extent to which states had decided to make their programs consistent across the different eligibility categories was unknown. This report, a companion to the Family Planning Report, asked states about benefits in place as of July 1, 2015 for women enrolled in fee-for-service Medicaid through different eligibility pathways, including traditional pre-ACA Medicaid pathways, expansion, and pregnancy-related eligibility for the following services: basic prenatal care, counseling and support services, delivery and postpartum care, and breastfeeding supports. This report presents survey findings for the 40 states and DC that provided responses to the survey. Throughout the report, DC is counted as a state, totaling 41 respondents. As illustrated in Figure 1, of the 41 respondents, 24 states and DC had adopted the ACA Medicaid expansion as of July 1, 2015. This report is the only one we know of that has examined Medicaid benefits for maternity care since the ACA’s passage.
Key Findings
While the benefits requirements vary between eligibility pathways, one overarching finding from the survey is that most states provide the same benefits to beneficiaries who qualify through Medicaid’s pregnancy eligibility pathway and adult pathway. Some states reported that in fact, they do not distinguish between the traditional full-scope Medicaid and pregnancy eligibility pathways in terms of the covered benefits. The survey questions covered four broad topics: prenatal services, counseling and support services, delivery and postpartum care, and breastfeeding services. Key findings on these topics are:
Prenatal Services
Prenatal care services monitor the progress of a pregnancy and identify and address potential problems before they become serious for either the mother or baby. Routine prenatal care encompasses a variety of services, including provider counseling, assessment of fetal development, genetic screening and testing, prenatal vitamins that contain folic acid and other nutrients, and ultrasounds, which provide important information about the progress of the pregnancy.
- All survey states reported that they cover prenatal vitamins and ultrasounds for pregnant women. However, some states impose quantity limits or require a prescription for vitamins.
- Nearly all responding states (38/41) reported covering amniocentesis and chorionic villus sampling (CVS) tests across all eligibility pathways available in the state, but fewer states (33/41) reported covering genetic counseling, some of which limit the service to women with higher risk or that have a positive result in genetic screens.
Counseling and Support Services
There are a variety of support services that can aid pregnant and postpartum women with pregnancy, delivery, and child rearing and improve birth outcomes. These include educational classes on childbirth and infant care, transportation to appointments, and home visits during or after pregnancy to assist with basic medical care, counseling on healthy behaviors, and in-person infant care assistance.
- Less than half of the responding states report that they provide education services to support childbirth, infant care or parenting in any of the Medicaid eligibility pathways. However, in some states services may be available through other public programs.
- Nearly all responding states provide substance or alcohol abuse treatment services for pregnant or postpartum women in most of the Medicaid eligibility pathways.
- Approximately three-fourths of the responding states cover prenatal and postpartum home visits, which give the opportunity for nurses and other clinicians to assist pregnant women and new parents in their homes with pregnancy management and child rearing skills.
Delivery and Postpartum Care
While all states are required to cover inpatient hospital care for Medicaid enrollees, there is more variation in coverage for delivery at birth centers or home births. Coverage for deliveries at birth centers is required in all states that license such facilities. In addition, coverage for doula assistance, which pays for a trained non-clinician to assist a woman before, during and/or after childbirth, by providing physical assistance, labor coaching, emotional support, and postpartum care is rare.
- A majority of responding states cover deliveries in birth centers, while half of the states cover home deliveries.
- Of all the services covered in the survey, coverage was lowest for doula Only four states reported that they cover doula assistance for women.
Breastfeeding Services
- There is a range of supports that have been found to help women initiate and maintain breastfeeding. These include breast pumps, lactation counseling by certified consultants both inpatient and outpatient after delivery, and educational programs, which can begin during pregnancy and continue after the birth of a child. States are required to cover breast pumps and consultation services for Medicaid expansion beneficiaries under the ACA’s preventive services requirement. A majority of responding states cover both electric and manual breast pumps, but some report using various utilization controls such as prior authorization and quantity limits.
- While most responding states report that breastfeeding education and hospital-based lactation consultations are covered under traditional Medicaid, far fewer states continue coverage once the woman goes home.
Conclusion
The analysis of state responses to this survey found that overall most states cover a broad range of perinatal services in their full scope traditional Medicaid program, under full scope ACA Medicaid expansion, and pregnancy-related eligibility pathways. Most, but not all, of the 41 surveyed states report that they cover basic prenatal services such as ultrasounds and vitamins, prenatal genetic testing, home visits, delivery in birth centers, postpartum visits, and breast pumps for nursing mothers. Many states recognize that these services are critical to improving birth outcomes. Coverage for services that help women and their families care for their children after delivery, such as childbirth and parenting classes, breastfeeding education and lactation consultation is less common (Table 1). Only half of reporting states cover home births, and very few states cover doula supports despite research suggesting that this assistance results in better health outcomes.3 While coverage requirements differ between eligibility pathways, in general, there is strong alignment within states across the various pathways.
The Medicaid program has a long history and excellent record of providing coverage for low-income pregnant women, with nearly half of all births nationwide provided through the program. Regardless of the outcome of current debates over the future of Medicaid or the ACA, the millions of low-income pregnant women that are served by Medicaid will continue to need to have access to coverage that includes the broad range of pregnancy-related services that help assure healthy maternal and infant outcomes.
| Table 1: Summary Results on Coverage of Selected Perinatal Services | |
| States Reporting Coverage Under Traditional Medicaid: | |
| Prenatal Services | |
| Genetic Counseling (33/41 states) | AR, CA, CO, CT, DC, DE, GA, HI, IA, IL, IN, KY, MA, MD, ME, MI, MN, MO, MS, MT, NC, NH, NV, NY, OH, OK, OR, SC, TN, TX, VA, VT, WA |
| Chronic Villus Sampling and Amniocentesis (38/41 states) | AK, AR, AZ, CA, CO, CT, DC, DE, GA, HI, IA, ID, IL, IN, KY, MA, MD, ME, MI, MN, MO, MS, MT, NC, NH, NM, NV, NY, OH, OK, OR, SC, TN, TX, VA, VT, WA, WV |
| Counseling and Support Services | |
| Case Management (35/41 states) | AK, AL, AR, AZ, CA, CO, DC, DE, GA, IA, ID, IL, IN, KY, MA, ME, MN, MO, MS, MT, NC, NE, NM, NV, NY, OH, OK, OR, TN, TX, VA, VT, WA, WV, WY |
| Substance Alcohol Abuse Treatment (40/41 states) | AK, AL, AR, AZ, CA, CO, CT, DC, DE, GA, HI, IA, ID, IL, IN, KY, MA, MD, ME, MI, MN, MO, MS, MT, NC, NE, NM, NV, NY, OH, OK, OR, SC, TN, TX, VA, VT, WA, WV, WY |
| Prenatal and Postpartum Home Visits (30/41 states) | AK, AR, CA, CT, DC, DE, GA, IA, ID, IL, IN, MA, MI, MN, MO, MS, MT, NC, NE, NH, NM, NY, OH, OK, OR, SC, VA, VT, WA, WV |
| Childbirth Education Classes (14/41states) | AR, CA, DC, DE, GA, HI, MI, MN, MS, NC, OH, OR, VA, WA |
| Infant Care/ Parenting Education (17/41 states) | AL, AR, CA, DC, DE, GA, HI, KY, MI, MN, MS, NM, NV, OH, OR, VA, WA |
| Deliveries and Postpartum care | |
| Birth Center Deliveries (32/41 states) | AK, AL, AZ, CA, CO, CT, DC, DE, GA, IA, IL, IN, KY, MA, MD, MN, MO, MT, NC, NE, NH, NM, NV, NY, OH, OK, OR, SC, TN, TX, WA, WV |
| Home Births (21/ 41 states) | AK, AZ, CA, CO, CT, IA, ID, IL, MD, MO, NH, NM, NY, OH, OR, SC, TX, VA, VT, WA, WV |
| Doula Services (4/41 states) | KY, MN, MS, OR |
| Postpartum Visit (41/41 states) | AK, AL, AR, AZ, CA, CO, CT, DC, DE, GA, HI, IA, ID, IL, IN, KY, MA, MD, ME, MI, MN, MO, MS, MT, NC, NE, NH, NM, NV, NY, OH, OK, OR, SC, TN, TX, VA, VT, WA, WV, WY |
| Breastfeeding Services | |
| Breastfeeding Education (27/41 states) | AK, AL, AR, AZ, CA, CO, CT, DC, DE, GA, HI, ID, IN, MA, MI, MN, MO, MS, NC, NV, NY, OH, OK, OR, SC, TN, VA |
| Electric Breast Pumps in Traditional Medicaid Program (35/41 states) | AK, AZ, CA, CO, CT, DC, DE, GA, HI, ID, IL, IN, KY, MA, MD, ME, MI, MN, MO, MS, MT, NE, NH, NM, NY, OH, OK, OR, TN, TX, VA, VT, WA, WV, WY |
| Lactation Consultation in Hospital (26/41 states) | AK, AR, AZ, CA, CO, CT, DC, DE, HI, ID, IN, KY, MI, MN, MO, MS, NC, NE, NY, OH, OK, OR, SC, TN, VA, WA |
| Lactation Consultation in clinic and/or at home (16/41 states) | AR, CA, CO*, CT, DC, DE, HI, MN, MS, NC*, NY, OH, OK*, OR, VA*, WA* |
| NOTES: *CO, NC, OK, VA, & WA cover lactation consultation in clinic, but not in a home visit. | |
***