A View from the States: Key Medicaid Policy Changes: Results from a 50-State Medicaid Budget Survey for State Fiscal Years 2019 and 2020
Long-Term Services and Supports
|
Key Section Findings |
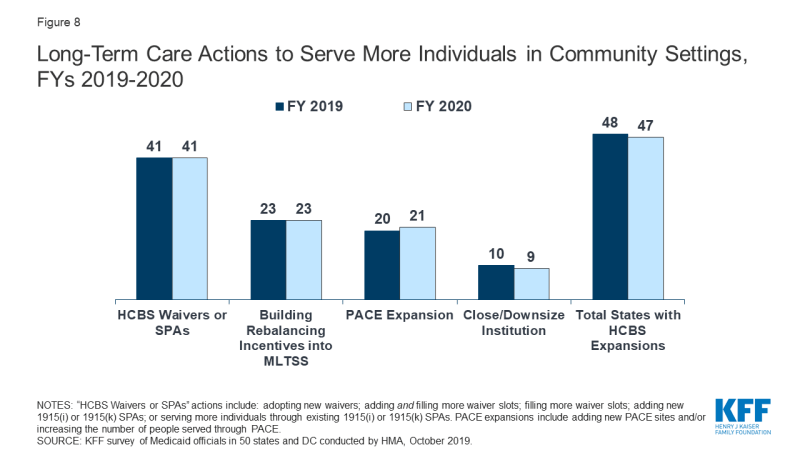
| Nearly all states in FY 2019 (48 states) and in FY 2020 (47 states) are employing one or more strategies to expand the number of people served in home and community-based settings. Of these states, the vast majority report using HCBS waivers and/or state plan options (i.e., 1915(c), Section 1115, 1915(i), and 1915(k)) to serve more individuals in the community. As of July 1, 2019, 25 states covered LTSS through one or more capitated managed care arrangements, and another two operated managed fee-for-service LTSS models.
What to watch:
Additional information on HCBS expansions implemented in FY 2019 or planned for FY 2020 as well as state-level details on capitated MLTSS models can be found in Tables 10 and 11. |
Medicaid is the nation’s primary payer for long-term services and supports (LTSS), covering a continuum of services ranging from home and community-based services (HCBS) that allow people to live independently in their own homes or in other community settings to institutional care provided in nursing facilities (NFs) and intermediate care facilities for individuals with intellectual disabilities (ICF-IDs). States have increasingly sought to expand home and community-based options and decrease reliance on institutional care in an effort to support beneficiaries’ preference to remain in their homes and community and rebalance their LTSS systems. In federal fiscal year 2016, spending on Medicaid LTSS totaled $167 billion, and HCBS represented 57% of these expenditures. In recent years, growth in Medicaid LTSS expenditures has been largely concentrated in HCBS.1
This year’s survey shows that nearly all states in FY 2019 (48 states) and FY 2020 (47 states) are using one or more strategies to expand the number of people served in home and community-based settings (Figure 8 and Table 10). States were asked about their use of the following rebalancing tools/methods: HCBS waivers and/or State Plan Amendments (SPAs) (including 1915(c), Section 1115, 1915(i), and 1915(k)); rebalancing incentives in managed care contracts; Programs of All-Inclusive Care for the Elderly (PACE); and efforts to downsize state institutions.
A large majority of states in FY 2019 (41 states) and in FY 2020 (41states) reported adopting new HCBS waivers/SPAs and/or serving more individuals through existing HCBS waivers/SPAs. Twenty-three states, or nearly all states that use an MLTSS model for at least some populations, reported using rebalancing incentives in their MLTSS contracts.2 For example, a number of states reported setting a blended nursing facility/HCBS rate for their long-term care population with assumptions built into the rates to incentivize plans to provide more home and community-based services. Nearly half of states (25 states) reported implementing PACE expansions in FY 2019 or FY 2020 by opening new PACE sites in one or both years (17 states) and/or expansion at existing sites. Fewer states reported efforts to downsize state institutions (likely because many states already have taken these actions in past years). No states took action to reduce or restrict the number of people receiving Medicaid HCBS in FY 2019 or FY 2020.
LTSS Direct Care Workforce
Many states are struggling to find sufficient numbers of trained direct care workers to meet the demand for services, including the demand for care in home and community-based settings.3,4 Low wages, few benefits, limited opportunities for career advancement, inadequate training, and high rates of worker injury are factors that contribute to a workforce shortage and high workforce turnover among paid LTSS direct care workers. The National Center for Health Workforce Analysis projects that demand for direct care workers (including nursing assistants, home health aides, personal care aides, and psychiatric assistants/aides) could grow by 48% between 2015 and 2030. Driven by demographic shifts, increased longevity, and increased prevalence of disability, this increased demand is expected to far exceed the available LTSS workforce supply.5
To address LTSS direct care workforce shortages and turnover, more states are reporting wage increases and workforce development activities (Exhibit 16). In FY 2019, 25 states reported implementing wage increases for Medicaid-reimbursed direct care workers, while 27 states reported implementing wage increases in FY 2020 (20 states in both years). This activity represents a significant uptick from FY 2018 when 15 states reported wage increases for direct care workers. In addition, 15 states had direct care workforce development strategies (e.g., recruiting, training, credentialing) in place in FY 2019, and 10 states reported expanding (7 states) or implementing new workforce development strategies (3 states) in FY 2020 (Exhibit 16).
| Exhibit 16: Strategies to Address LTSS Direct Care Workforce Shortages & Turnover | |||
| Fiscal Year | # of States | States | |
| Wage Increases | 2019 | 25 | AZ, CA, CO, CT, DC, DE, HI, IL, MA, MI, MT, NC, NH, NJ, NY, OK, OR, RI, SC, TN, UT, VT, WA, WI, WV |
| 2020 | 27 | AL, AR, AZ, CA, CO, CT, DC, DE, IL, LA, MA, MI, NH, NJ, NY, OH, OK, OR, PA, TN, TX, UT, VA, VT, WA, WI, WV | |
| Workforce Development (including recruiting, training, credentialing etc.) | In Place FY 2019 | 15 | AR, AZ, CA, CT, KY, MA, MN, MS, NY, OH, OR, PA, TN, WA, WI |
| New/Expanded FY 2020 | 10 | AZ, CT, MI*, MN, OR*, PA, RI*, TN, WA, WI | |
| MD and SD did not report; “*” above indicates “new” initiative in FY 2020 | |||
The following are examples of state direct care workforce development strategies reported:
- In FY 2020, Georgia is implementing structured family caregiving as a waiver service to address professional workforce shortages and provide formal training, support, and a stipend for family caregivers who live with and assist an elderly and/or disabled waiver participant requiring significant assistance with activities of daily living. Similarly, North Carolina plans to expand workforce options in FY 2020 by adopting a similar new live-in support service, coordinated caregiving, in their waiver serving seniors and people with disabilities.
- In Minnesota, for FYs 2019 and 2020, payments on behalf of enrollees who are eligible for 12 or more hours of state plan personal care assistant (PCA) services per day may be made at a higher reimbursement rate after the provider has completed required training. Starting on the date the worker qualifies, the PCA provider agency must pass the enhanced rate increase in wages and/or benefits to the specific direct care worker.
- Tennessee is pursuing a three-prong workforce development strategy which includes: 1) developing a competency-based education and training curriculum; 2) investing in collecting provider workforce data and in building provider capacity to improve recruitment and retention; and 3) developing wage incentives tied to competency-level (e.g., based on training/certification and/or tenure) as well as provider incentives for the adoption of evidence-based approaches to workforce recruitment and retention.
Housing Supports
Thirty-seven states reported offering at least some housing-related services in FY 2019 and/or FY 2020 under SPA, Section 1915 (c), or Section 1115 to promote community integration for individuals with disabilities, seniors in need of LTSS, individuals experiencing homelessness, or individuals with SMI/SUD (Exhibit 17). The availability of affordable, accessible housing has long been identified as a major barrier to state efforts to transition individuals from institutions and rebalance their LTSS systems.6 In 2015, CMS issued an Informational Bulletin to clarify how Medicaid can be used to support certain housing-related activities and promote community integration for targeted groups (individuals with disabilities, seniors in need of LTSS, and individuals experiencing chronic homelessness).7 While noting Medicaid funds generally cannot be used for room and board, the bulletin identified several categories of services that can be funded including: individual housing transition services, individual housing and tenancy sustaining services, and state-level housing related collaborative activities.8 A majority of the housing-related services described by states are offered through Section 1915 (c) waivers followed by housing services offered through Section 1115 waivers. Fewer states provide these services under their State Plan.
| Exhibit 17: Housing Support Services | |||
| States providing housing supports in FY 2019 and/or FY 2020 | 37 States | AK, AL, AR, AZ, CA, CO, CT, DC, DE, FL, HI, IL, IN, KY, LA, MA, MD, MI, MN, MT, NC, NE, NJ, NM, NV, NY, OH, OR, PA, TN, TX, UT, VA, VT, WA, WI, WV | |
| States implementing new or expanded housing supports in FY 2020 | 13 States | CT, HI, IL*, MA*, NC*, NJ*, NV*, NY*, OH*, UT*, VT, WA, WI | |
| “*” Indicates state reporting a new initiative in 2020 | |||
The following are examples of states implementing new or expanded housing supports in FY 2020:
- Illinois will be implementing new pre-tenancy and tenancy support services for beneficiaries with frequent ER utilization, two or more chronic conditions, and at risk of homelessness or institutional care.
- Massachusetts will be adding certain health-related social services under its Section 1115 waiver targeted at individuals experiencing homelessness, including pre-tenancy supports, tenancy sustaining supports, and home modifications.
- North Carolina recently received CMS approval of a Section 1115 waiver authorizing the state to establish a “Healthy Opportunities” pilot program in two to four regions within the state’s new Medicaid managed care delivery system. Under the pilot program, beneficiaries with certain health conditions (e.g., two or more chronic conditions) and social risk factors, including homelessness and housing insecurity, will receive evidence-based enhanced case management and other services designed to address enrollee needs related to housing, food, transportation and safety.9
- Ohio plans to expand community transition services under its Section 1915(c) HCBS waiver programs for adults with physical disabilities and individuals with developmental disabilities as well as add a new community integration service that will provide independent living assistance and community support coaching activities to enable individuals to live independently in the community.
Money Follows the Person
Money Follows the Person (MFP) is a federal grant program enacted under the Deficit Reduction Act of 2005 and extended through September 2016 by the Affordable Care Act, which operates in 44 states.10 Enhanced federal funding under MFP has supported the transition of over 90,000 individuals from institutional to home and community-based long-term care settings as of June 2018.11 This includes the transition of older adults, individuals with physical disabilities, individuals with mental illness, and individuals with I/DD. The program has also been a catalyst for development of housing-related activities as states have used these resources to offer new housing-related services and incorporate housing expertise within their Medicaid programs, among other activities to assist in expanding housing options available for individuals who choose HCBS.12,13
Although states were set to fully phase-out their MFP programs in federal fiscal year 2020, the Congress acted to provide $254 million in additional funds for a short-term extension of the program (authorized additional funding currently expires December 31, 2019).14 However, without a longer-term reauthorization, the future of the MFP program remains uncertain. In this year’s survey, states were asked about the status of their MFP funding and the services that would be impacted if MFP funds were exhausted and the program is not reauthorized. Thirty-six states reported they have not yet exhausted their MFP funds and most states expect their funding to last through federal fiscal year 2020. In contrast, seven states report having expended all of their MFP dollars.15 In anticipation of the phase-out of MFP, several states indicated they had been able to transition certain MFP services to their State Plan and/or 1915(c) waivers. A greater number of states identified a range of services and key administration activities they would expect to discontinue if/when MFP funding expires. These include certain community transition services; community case management; outreach specialists, housing specialists, and housing relocation assistance; training for family caregivers, care coordinators, and providers; among other activities. Of these, community transition services were most often cited as being at risk once MFP funds are exhausted.
Managed Long-Term Services and Supports (MLTSS)
States have increasingly turned to managed long-term services and supports – in particular, capitated MLTSS models. As of July 1, 2019, 27 states reported having an MLTSS model. Two states reported having a managed fee-for-service MLTSS model while roughly half of states (25 states) covered LTSS through one or more of the following types of capitated managed care arrangements:
- Medicaid MCO covering Medicaid acute care and LTSS (21 states)
- PHP covering only Medicaid LTSS (5 states)
- MCO arrangement for dual eligible beneficiaries covering Medicaid and Medicare acute care and Medicaid LTSS services in a single, financially aligned contract under the federal Financial Alignment Initiative (FAI) (9 states)
Of the 25 states that reported using one or more of these capitated MLTSS models, eight states reported using two models, and one state (New York) reported using all three. Of the states with capitated MLTSS, 18 states offered some form of MLTSS plan on a statewide basis for at least some LTSS populations as of July 1, 2019 (Table 11). Almost every MLTSS state includes both institutional and HCBS in the same contractual arrangement with a few exceptions: Ohio and Michigan report that coverage varies by MLTSS arrangement and Arkansas’ new PASSE program includes only HCBS.
In addition to these capitated models, two states (Alabama and Washington) report managed fee-for-service (FFS) LTSS models. Under these arrangements, states make payments to care coordination entities responsible for managing the care of individuals, while continuing to reimburse providers on a FFS basis for LTSS and other Medicaid services. Washington is the only state that has a managed FFS Financial Alignment Initiative in place (discussed in more detail below). In FY 2019, Alabama began contracting with a provider-led Integrated Care Network (ICN) to provide enhanced case management, education, and outreach services to most Medicaid long-term care recipients in both HCBS and institutional settings. The ICN is paid a per-member per-month (PMPM) payment with a portion of that payment contingent on the entity meeting state-established targets for nursing facility and HCBS mix.
As of July 1, 2019, nine states offered an MCO-based FAI (California, Illinois, Massachusetts, Michigan, New York, Ohio, Rhode Island, South Carolina, and Texas). These initiatives aim to provide more integrated care across Medicare and Medicaid, including LTSS, to dual eligible enrollees. The FAI model involves a three-way contract between an MCO, Medicare, and the state Medicaid program.16,17 In April 2019, CMS issued a state Medicaid director’s letter to encourage additional states to participate in an FAI demonstration model.18 Citing a lack of coordinated care for dual eligibles and a disproportionate share of Medicare and Medicaid spending for these beneficiaries, the letter outlined three opportunities for states to consider to test new models for dually eligible individuals – a capitated financial alignment model; a managed FFS model; and an alternative state-designed model. For states currently participating, the letter offered opportunities for multi-year extensions as well as possible revisions to existing FAIs; for example, expansion of the geographic scope of the demonstrations.19
States were asked whether they plan to take advantage of these new opportunities. Of the nine states currently participating in the capitated FAI model, five indicated that they planned to seek an extension and four indicated that a final determination on whether to pursue this opportunity had not been made. Washington also reported an intent to seek an extension to their current managed FFS FAI demonstration. For states without an FAI, only Tennessee affirmatively indicated plans to pursue a state-designed model.
| Washington State FAI Demonstration |
| Implemented in July 2013, Washington was the first state to partner with CMS on a Financial Alignment Initiative that utilized a managed fee-for-service model. Under the demonstration, Washington is building upon its Medicaid health home infrastructure, targeting dual eligible enrollees with chronic health conditions who are identified as high risk. The health homes are the lead local entities responsible for organizing enhanced integration of primary, acute, LTSS, and behavioral health services for Medicare-Medicaid enrollees participating in the demonstration. They are paid a tiered per-member per-month (PMPM) payment based on level and type of enrollee interaction and receive performance-based payments based on rates of engagement with beneficiaries. Results from the first three demonstration years indicate Washington’s FAI has resulted in estimated Medicare savings of more than 11% and evidence of positive beneficiary experience and quality trends.20,21 |
Many states encourage improved coordination and integration of services for the dually eligible population under MCO arrangements outside of the FAI. Under a Memorandum of Understanding (MOU) with CMS, Minnesota operates an administrative alignment demonstration (with no financial alignment) to test ways to streamline processes and better integrate care for dually eligible beneficiaries enrolled in the Minnesota Senior Health Options program. Increasingly, states are also utilizing the existing Medicare Dual Eligible Special Needs Plans (D-SNP) infrastructure as a platform to improve integration and coordination for individuals also enrolled in Medicaid managed care. Overall, 36 states indicated in this year’s survey having a contract with their D-SNPs to support better care coordination for dual eligible beneficiaries. Eleven states22 report that they require Medicaid-contracting MCOs to be Medicare Dual Eligible Special Needs Plans (D-SNPs)23 or Fully Integrated Dual Eligible (FIDE) Special Needs Plans24 in some or all MLTSS models offered in the state. Seven states report that they have or are planning to institute “default enrollment.” Under default enrollment, beneficiaries in a capitated Medicaid managed care plan may be automatically enrolled in an affiliated D-SNP plan when an individual becomes eligible for Medicare. Going forward, states are expected to continue to increase their reliance on D-SNPs as part of their MLTSS approach given recent CMS guidance promoting opportunities to use D-SNPs and new requirements enacted as part of the Balanced Budget Act of 2018 (effective in Calendar Year 2021) for D-SNPs to better integrate care for dual eligibles.25
MLTSS Enrollment
For geographic areas where capitated MLTSS operates, this year’s survey asked whether, as of July 1, 2019, certain populations were enrolled in MLTSS on a mandatory or voluntary basis or were always excluded. On the survey, states selected from “always mandatory,” “always voluntary,” “varies,” or “always excluded” for the following dually eligible and non-dually eligible populations: seniors, persons with I/DD, nonelderly persons with physical disabilities, medically fragile/technologically dependent children, and persons with SMI or SED. Dual eligible and non-dual eligible seniors and persons with physical disabilities were most likely to be enrolled on a mandatory basis (Exhibit 18). Dual and non-dual eligible persons with SMI or SED followed closely behind in terms of mandatory inclusion in these programs. In contrast, dual and non-dual eligible individuals with I/DD and medically fragile children were most likely to be excluded from mandatory enrollment in MLTSS. (Exhibit 18).
| Exhibit 18: MLTSS Enrollment by Populations (# of States) | |||||
| Non-Dual Eligibles | |||||
| Seniors | Persons w/ Physical Disabilities | Persons w/ I/DD | Medically Fragile Children | Persons with SMI/SED | |
| Always mandatory | 15 | 15 | 6 | 9 | 13 |
| Always voluntary | 3 | 3 | 5 | 1 | 2 |
| Varies | 1 | 2 | 8 | 5 | 5 |
| Always excluded | 6 | 5 | 6 | 10 | 5 |
| Dual Eligibles | |||||
| Always mandatory | 15 | 15 | 6 | 9 | 17 |
| Always voluntary | 3 | 3 | 5 | 1 | 4 |
| Varies | 1 | 2 | 8 | 5 | 2 |
| Always excluded | 6 | 5 | 6 | 10 | 2 |
MLTSS Population Changes
In FY 2019 and FY 2020, several states introduced new MLTSS programs or expanded existing MLTSS programs (Exhibit 19).
| Exhibit 19: MLTSS Population Expansions, FY 2019 and FY 2020 | ||
| FY 2019 | FY 2020 | |
| Geographic Expansions | MA, PA | ID, IL, PA |
| New Population Groups Added | OH, VA | TN |
| Implementing an MLTSS program for the First Time | AR | — |
Notable state MLTSS expansions include:
- In FY 2019, Pennsylvania continued to phase in implementation of its Community HealthChoices (CHC) MLTSS program for dual eligibles, older adults, and individuals with physical disabilities. In January 2019, Pennsylvania implemented CHC in the southeastern region of the state, which includes Philadelphia, and is scheduled to complete its statewide expansion in January of 2020.
- In FY 2019, Arkansas introduced a new capitated MLTSS model for persons with I/DD and behavioral health needs. The Provider-led Arkansas Shared Savings Entities (PASSEs) are responsible for managing the comprehensive health care needs, including home and community-based LTSS, of these populations.
- In July 2019, Illinois expanded managed LTSS for dual eligibles statewide beyond the greater Chicago region. HealthChoice Illinois health plans in these areas began managing health care services, including LTSS, for dual eligible beneficiaries not enrolled in the state’s FAI program who are in a nursing facility or are receiving certain HCBS waiver services.26
- In July 2019, Tennessee received CMS approval to add two new benefit groups to its Employment and Community First (ECF) CHOICES program, TennCare’s MLTSS program for individuals with I/DD. The new benefit groups include certain children and adults with I/DD and severe co-occurring behavioral health and/or psychiatric conditions. Tennessee is also proposing to establish a new Katie Beckett-like waiver program with capped enrollment, for children under age 18 with disabilities and/or complex medical needs who would be Medicaid eligible if they lived in an institution but are cared for at home and do not qualify because of their parents’ income. Those children with the most significant disabilities or complex medical needs will receive the full range of Medicaid benefits and home and community-based services through the state’s managed care program.27
Table 10: Long-Term Care Actions to Serve More Individuals in Community Settings in all 50 States and DC, FY 2019 and FY 2020
|
States |
Sec. 1915 (c) or Section 1115 HCBS Waiver |
Sec. 1915(i) HCBS State Plan Option |
Sec. 1915(k) “Community First Choice” Option |
Building Rebalancing Incentives into MLTSS |
PACE |
Close/ Downsize Institution |
Total States with HCBS Expansions |
|||||||
|
2019 |
2020 |
2019 |
2020 |
2019 |
2020 |
2019 |
2020 |
2019^ |
2020 |
2019 |
2020 |
2019 |
2020 |
|
|
Alabama |
X |
X |
X |
X |
X |
|||||||||
|
Alaska |
X |
X |
X |
X |
X |
X |
||||||||
|
Arizona |
X |
X |
X |
X |
||||||||||
|
Arkansas |
X |
X |
X* |
X |
X |
|||||||||
|
California |
X |
X |
X |
X |
X |
X |
X |
X |
X* |
X* |
X |
X |
X |
X |
|
Colorado |
X |
X |
X* |
X* |
X |
X |
||||||||
|
Connecticut |
X |
X |
X |
X |
X |
X |
X |
X |
X |
X |
||||
|
Delaware |
X |
X |
X |
X |
X |
X |
X |
X* |
X |
X |
||||
|
DC |
X* |
X |
||||||||||||
|
Florida |
X |
X |
X |
X |
X* |
X* |
X |
X |
||||||
|
Georgia |
X |
X |
X |
X |
X |
X |
||||||||
|
Hawaii |
X |
X |
X |
X |
||||||||||
|
Idaho |
X |
X |
X |
X |
X |
X |
X |
X |
||||||
|
Illinois |
X |
X |
X |
X |
X |
|||||||||
|
Indiana |
X |
X |
X |
X |
X* |
X |
X |
|||||||
|
Iowa |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|||||
|
Kansas |
X |
X |
X |
X |
X |
X |
||||||||
|
Kentucky |
||||||||||||||
|
Louisiana |
X |
X |
||||||||||||
|
Maine |
X |
X |
X |
X |
||||||||||
|
Maryland |
X |
X |
X |
X |
X |
X |
X |
X |
||||||
|
Massachusetts |
X |
X |
X |
X |
X* |
X |
X |
|||||||
|
Michigan |
X |
X |
X |
X |
X |
X |
X* |
X* |
X |
X |
||||
|
Minnesota |
X |
X |
X |
X |
X |
X |
X |
|||||||
|
Mississippi |
X |
X |
X |
X |
X |
|||||||||
|
Missouri |
X |
X |
X* |
X |
X |
|||||||||
|
Montana |
X |
X |
X |
X |
X |
X |
X |
|||||||
|
Nebraska |
X |
X |
X |
X |
X |
X |
||||||||
|
Nevada |
X |
X |
X |
X |
X |
X |
X |
X |
||||||
|
New Hampshire |
||||||||||||||
|
New Jersey |
X |
X |
X* |
X |
X |
|||||||||
|
New Mexico |
X |
X |
X |
X |
X |
X |
X |
|||||||
|
New York |
X |
X |
X |
X |
X |
X |
X |
X* |
X* |
X |
X |
X |
||
|
North Carolina |
X |
X |
X |
X |
X |
X |
X |
|||||||
|
North Dakota |
X |
X |
X* |
X* |
X |
X |
X |
X |
||||||
|
Ohio |
X |
X |
X |
X |
X |
X |
X |
X |
X |
X |
||||
|
Oklahoma |
X |
X |
X* |
X |
X |
|||||||||
|
Oregon |
X |
X |
X |
X |
X |
X |
X |
X* |
X |
X |
||||
|
Pennsylvania |
X |
X |
X |
X |
X* |
X |
X |
X |
||||||
|
Rhode Island |
X |
X |
X |
X |
X |
|||||||||
|
South Carolina |
X |
X |
X |
X |
X |
X |
X |
X |
X |
X |
||||
|
South Dakota |
X |
X |
||||||||||||
|
Tennessee |
X |
X |
X |
X |
X |
X |
||||||||
|
Texas |
X |
X |
X |
X |
X |
X |
X |
X |
X |
X |
||||
|
Utah |
X |
X |
X |
X |
||||||||||
|
Vermont |
X |
X |
X |
X |
||||||||||
|
Virginia |
X |
X |
X |
X |
X |
|||||||||
|
Washington |
X |
X |
X |
X |
X |
X* |
X |
X |
X |
X |
||||
|
West Virginia |
X |
X |
X |
X |
||||||||||
|
Wisconsin |
X |
X |
X |
X |
X |
X |
||||||||
|
Wyoming |
X |
X |
X |
X |
X |
X |
||||||||
|
Totals |
39 |
39 |
15 |
13 |
10 |
11 |
23 |
23 |
20 |
21 |
10 |
9 |
48 |
47 |
|
NOTES: 1915(c) or Sec. 1115 waiver actions include: adopting new waivers; adding and filling more waiver slots; or filling more waiver slots. Actions under 1915(i) and 1915(k) options include adding new 1915(i) or 1915(k) SPAs or serving more individuals through existing 1915(i) or 1915(k) SPAs. Actions under PACE include more individuals served in existing and/or new PACE sites, with “*” indicating which states expect new sites in FY 2019 or FY 2020. ^PA and ND reported adding a PACE site in FY 2019 but did not anticipate this would result in increased enrollment until FY2020. SOURCE: Kaiser Family Foundation Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2019. |
||||||||||||||
Table 11: Capitated MLTSS Models in all 50 States and DC, as of July 1, 2019
|
States |
Medicaid MCO |
PHP |
Financial Alignment Demonstration (FAD) for Duals |
Any MLTSS |
Statewide |
|
Alabama |
|||||
|
Alaska |
|||||
|
Arizona |
X |
X |
X |
||
|
Arkansas |
X |
X |
X |
||
|
California |
X |
X |
X |
||
|
Colorado |
|||||
|
Connecticut |
|||||
|
Delaware |
X |
X |
X |
||
|
DC |
|||||
|
Florida |
X |
X |
X |
||
|
Georgia |
|||||
|
Hawaii |
X |
X |
X |
||
|
Idaho |
X |
X |
|||
|
Illinois |
X |
X |
X |
X |
|
|
Indiana |
|||||
|
Iowa |
X |
X |
X |
||
|
Kansas |
X |
X |
X |
||
|
Kentucky |
|||||
|
Louisiana |
|||||
|
Maine |
|||||
|
Maryland |
|||||
|
Massachusetts |
X |
X |
X |
||
|
Michigan |
X |
X |
X |
||
|
Minnesota |
X |
X |
X |
||
|
Mississippi |
|||||
|
Missouri |
|||||
|
Montana |
|||||
|
Nebraska |
|||||
|
Nevada |
|||||
|
New Hampshire |
|||||
|
New Jersey |
X |
X |
X |
||
|
New Mexico |
X |
X |
X |
||
|
New York |
X |
X |
X |
X |
X |
|
North Carolina |
X |
X |
X |
||
|
North Dakota |
|||||
|
Ohio |
X |
X |
X |
||
|
Oklahoma |
|||||
|
Oregon |
|||||
|
Pennsylvania |
X |
X |
|||
|
Rhode Island |
X |
X |
X |
X |
|
|
South Carolina |
X |
X |
|||
|
South Dakota |
|||||
|
Tennessee |
X |
X |
X |
||
|
Texas |
X |
X |
X |
X |
|
|
Utah |
|||||
|
Vermont |
|||||
|
Virginia |
X |
X |
X |
||
|
Washington |
|||||
|
West Virginia |
|||||
|
Wisconsin |
X |
X |
X |
X |
|
|
Wyoming |
|||||
|
Totals |
21 |
5 |
9 |
25 |
18 |
|
NOTES: States were asked whether they cover long-term services and supports through any of the following managed care (capitated) arrangements as of July 1, 2019: Medicaid MCO (MCO covers Medicaid acute + Medicaid LTSS); PHP (covers only Medicaid LTSS); MCO arrangement for dual eligibles under the Financial Alignment Demonstration (Medicaid MCO covers Medicaid and Medicare acute + Medicaid LTSS). In addition to these capitated models, two states (Alabama and Washington) report managed fee-for-service (FFS) LTSS models. Under these arrangements, states make payments to care coordination entities responsible for managing the care of individuals, while continuing to reimburse providers on a FFS basis for LTSS and other Medicaid services. SOURCE: Kaiser Family Foundation Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2019. |
|||||