Amid Unwinding of Pandemic-Era Policies, Medicaid Programs Continue to Focus on Delivery Systems, Benefits, and Reimbursement Rates: Results from an Annual Medicaid Budget Survey for State Fiscal Years 2023 and 2024
Future Outlook: Key Priorities and Challenges in FY 2024 and Beyond
After three years of operating under the COVID-19 pandemic PHE and the Medicaid continuous enrollment provision, the PHE ended in May 2023, and the Consolidated Appropriations Act, 2023, was enacted, ending the Medicaid continuous coverage requirement as of March 31, 2023 and phasing out the pandemic-related enhanced federal matching funds by the end of 2023. At the time of the survey, all states remained heavily focused on completing Medicaid redeterminations and were employing a variety of strategies such as adopting unwinding waivers to streamline the process, conducting new and enhanced outreach to enrollees, and investing in system enhancements to increase automatic renewals designed to maintain coverage for eligible individuals. A number of states also commented on the challenges of completing the redeterminations while at the same time maintaining ongoing business operations and/or pursuing new high priority initiatives. Beyond unwinding of the continuous enrollment provision, states reported other pressing challenges and key priorities (Figure 17).
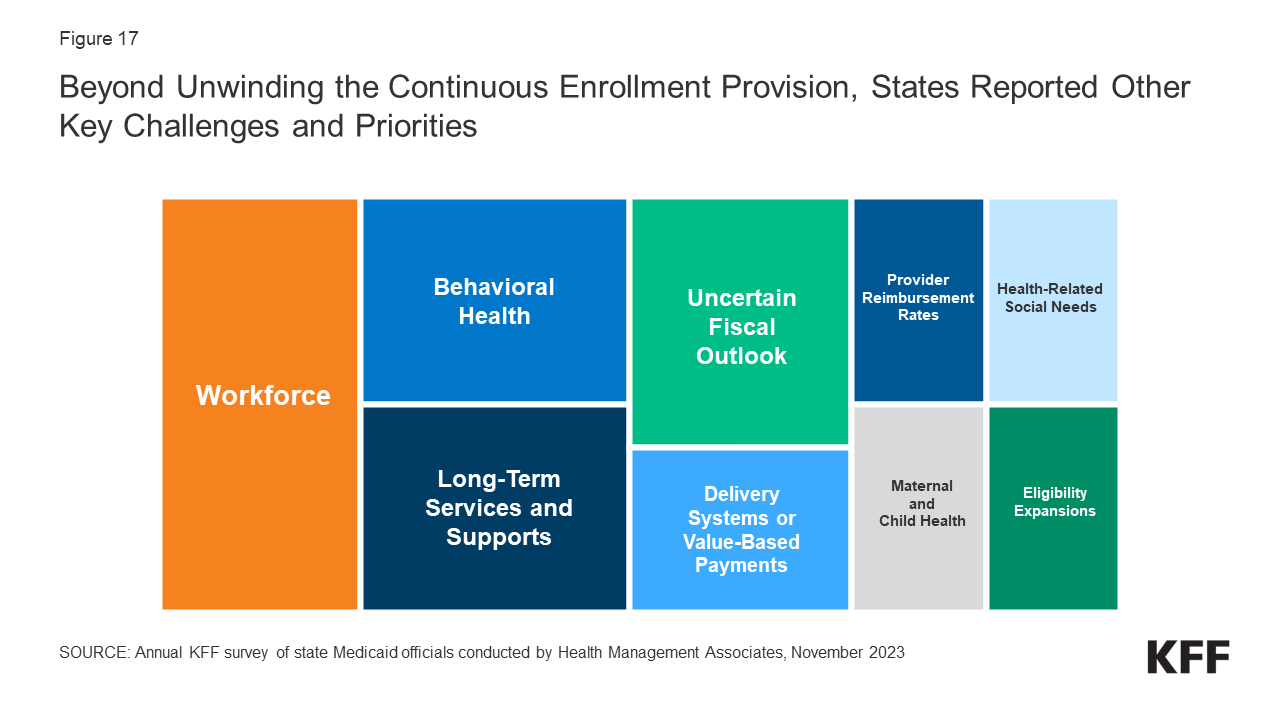
Figure 17: Beyond Unwinding the Continuous Enrollment Provision, States Reported Other Key Challenges and Priorities
Three quarters of responding states reported workforce challenges relating to health care providers, state staff, or both. States frequently reported shortages of nurses, direct care workers, and behavioral health providers often resulting in access challenges for children’s behavioral health services, dental services, primary and maternity care, home and community-based services (HCBS), and institutional services. One state also cited OB (obstetrics) deserts and hospital closures in rural areas as challenges affecting all payers, not just Medicaid. More than a third of responding states also cited state staff workforce challenges including the difficulty of recruiting and retaining staff with specialized technical expertise and the need for greater “bandwidth” to implement and manage complex projects. Other states noted losses of institutional knowledge within state staff, burnout, and the need to ramp up recruitment and succession planning in anticipation of a large number of state staff retirements in the next few years.
More than half of responding states identified behavioral health improvements as a key priority or challenge. For example, states are working to expand access to behavioral health services through efforts to build out the behavioral health continuum of care, integrate physical health and behavioral health services, implement mobile crisis services, expand behavioral health services in schools, and add coverage of evidence-based behavioral health service models. Several states commented on efforts to implement Certified Community Behavioral Health Clinics (CCBHCs) and others referred more generally to behavioral health reform or statewide behavioral health transformation efforts which may include but extend beyond the Medicaid program. In alignment with the state-identified behavioral health priorities, a quarter of responding states reported significant behavioral health challenges including workforce shortages, lack of access to behavioral health services, especially for children and youth, gaps in the behavioral health service continuum, and the challenge of integrating physical health and behavioral health.
More than half of responding states cited a key priority or challenge related to long-term services and supports (LTSS). Several states reported that sustaining implementation of HCBS expansions made possible by pandemic-related flexibilities and enhanced funding made available in the 2021 American Rescue Plan Act (ARPA) remained a top priority. Others reported LTSS priorities included nursing facility payment transformation and quality improvement, implementation of LTSS managed care, expansion of HCBS waiver slots, compliance with the HCBS Settings Rule, implementation of an Electronic Visit Verification system, and LTSS redesign efforts to enhance HCBS compliance and quality. Several states highlighted LTSS-related challenges including workforce shortages, the aging of the population, LTSS access, and nursing facility and HCBS provider financial challenges.
More than one-third of responding states reported a delivery system improvement or value-based payment initiative as a key priority. Several states commented on planned managed care re-procurements that would incorporate enhanced quality and outcomes expectations, two states (North Carolina and Oklahoma) reported planned or ongoing managed care implementations, and one state (Idaho) reported on the implementation of “value care organizations” (similar to Accountable Care Organizations). Other states reported on ongoing delivery system reform efforts under waiver authority, new quality incentive and value-based payment programs, initiatives to replace primary care case management programs with a new care management model or alternative payment model (APM), and efforts to strengthen managed care oversight.
While most states at the time of the survey reported favorable state fiscal conditions, over half of responding states noted an uncertain fiscal outlook. Some cited the expiration of one-time funding, especially ARPA funds for the HCBS services, while others noted the end of the pandemic-related enhanced federal matching funds as a challenge. Other states commented on the budgetary impacts of inflation, workforce challenges, provider pressure to increase reimbursement rates, the challenge of working with the legislature to craft the budget, and the general ongoing expectation for responsible budget management with sustainable growth. One state also commented on the need for contingency plans to address “potential headwinds.”
Other key priorities cited by more than one-quarter of responding states include: addressing health-related social needs, improving provider reimbursement rates and/or performing rate studies, implementing initiatives to improve maternal and child health, and expanding eligibility. Specifically, states mentioned implementing the option to expand postpartum coverage and preparing for the required implementation of 12-month continuous coverage for children as key eligibility expansions. Compared with past surveys, somewhat fewer states mentioned IT system modernization initiatives as key priorities, although nearly a quarter reported an IT system-related priority and several states reported significant IT challenges.
