Intrauterine Devices (IUDs): Access for Women in the U.S.
Intrauterine devices (IUDs) are one of the most effective forms of reversible contraception. IUDs, along with implants, are known as long-acting reversible contraception (LARCs) because they can be used to prevent pregnancy for several years. IUDs have been used in the U.S. for decades, but a safety controversy in the 1970s prompted the removal of all but one IUD from the U.S. market by 1986. The first new generation IUD was introduced to the U.S. market in 1988, following revised Food and Drug Administration (FDA) safety and manufacturing requirements. Recent controversies have focused on the mechanism of action of IUDs, the high upfront costs for the device, and variability in insurance coverage and access. This fact sheet reviews the various IUDs approved by the FDA, awareness, use, and availability of IUDs, and key issues in insurance coverage and financing of IUDs in the U.S.
What is an IUD?
IUDs are small devices placed into the uterus through the cervix by a trained medical provider to prevent pregnancy. A follow up visit is recommended post-insertion to confirm placement, and a visit to the provider is required for removal. IUDs are effective for three to 10 years, depending on the type of IUD. There are two major categories of IUDs – copper and hormonal – and within those categories, there are currently five IUDs approved by the FDA (Table 1). IUDs work by affecting the ovum and sperm to prevent fertilization and are more than 99% effective at preventing pregnancy. They do not protect against HIV and other sexually transmitted infections (STIs). IUDs do not affect an established pregnancy and do not act as an abortifacient.
| Table 1: Types of IUDs | ||||
| Copper IUD | Available Since | Years Effective | Use and FDA Approval | Possible side effects |
| Copper IUD (Paragard) | 1988 | 10 years | Approved only in parous women, but available to all women regardless of parity.
Can be used as Emergency Contraception when inserted within 5 days. |
Abnormal menstrual bleeding.
Higher frequency or intensity of cramps/ pain. |
| Hormonal IUDs | Available Since | Years Effective | FDA Approval | Possible side effects |
| Mirena | 2001 | 5 years | Approved only in parous women, but available to all women regardless of parity. | Inter-menstrual spotting in the early months.
Reduces menstrual blood loss significantly. Hormone-related: headaches, nausea, breast tenderness, depression, cyst formation. |
| Skyla | 2013 | 3 years | Approved for women regardless of parity. | |
| Liletta | 2015 | 6 years | Approved for women regardless of parity. | |
| Kyleena | 2016 | 5 years | Approved for women regardless of parity. | |
Non-Hormonal Copper-T Intrauterine Device
The copper IUD is a hormone-free T-shaped device wrapped in copper wire and is effective for up to 10 years.
- Marketed under the brand name ParaGard by Teva Women’s Health Pharmaceuticals, the copper IUD was approved by the FDA in 1984 and has been available in the US since 1988.
- The copper IUD begins working immediately after insertion and consequently does not require a woman to use a backup method of contraception after insertion. Because of this, the copper-IUD can also be used as emergency contraception within five days of unprotected intercourse or method failure and is more effective at preventing pregnancy than emergency contraceptive pills. Unlike Plan B emergency contraceptive pills, the effectiveness of IUDs does not vary based on a woman’s weight.
- Current evidence does not support prior theories that the copper IUD damages fertilized embryos or prevents implantation.
Hormonal Intrauterine Devices (LNG-IUD)
Four hormonal IUDs are available on the US market. They are also known as LNG-IUDs because they contain the progestin hormone levonorgestrel, which is released in small amounts each day. Today, most women who use IUDs use one of the hormonal products. Hormonal IUDs are not effective as emergency contraception.
- Mirena, manufactured by Bayer Healthcare Pharmaceuticals, is the hormonal IUD that has been on the market longest and is the most commonly used. In addition to preventing pregnancy, the FDA approved use of Mirena in women using this IUD as contraception to treat heavy menstrual bleeding. Mirena, as well as the copper IUD, are not FDA approved for women who have not had children (nulliparous), but research has found that they can be provided safely and effectively to these women.
- Skyla, also manufactured by Bayer, is slightly smaller than the Mirena, making it a better candidate for nulliparous women.
- Liletta was approved in 2015. Actavis in conjunction with Medicines360, a non-profit women’s pharmaceutical company, developed Liletta specifically to be low cost and available to public health clinics enrolled in the national 340B Drug Pricing Program at a significant discount. The 340B program provides reduced cost pharmaceuticals to providers that serve low-income populations. In 2019, the FDA approved Liletta for up to six years of use, making it the hormonal IUD with the longest approved duration.
- Kyleena, the newest IUD, was approved by the FDA in September 2016, and became available in October 2016. It’s also manufactured by Bayer and contains lower hormone levels than Mirena.
Use, Awareness, and Availability of IUDs
Use of IUDs in the U.S. has been increasing substantially since the early 2000s but is still lower than other methods. Attitudes regarding safety of IUDs have been shifting interest has grown, especially among younger providers and younger women who have less knowledge of the IUD controversies of the past.
Use
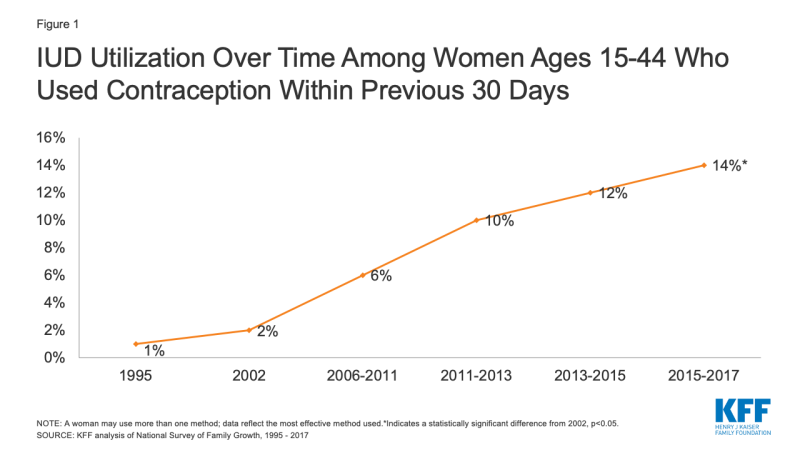
- Recent data estimates that 14% of women1 who use contraception ages 15 to 44 used an IUD in 2015-2017.2 Utilization among all women, but especially younger women, has risen (Figure 1).
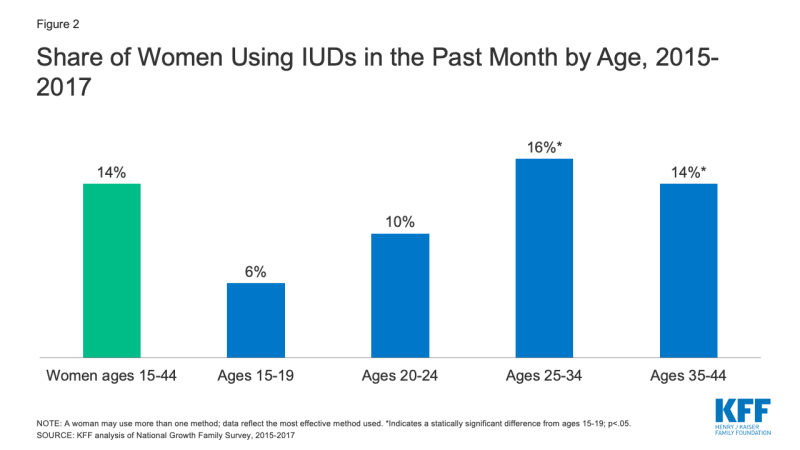
- IUD use is highest among women ages 25 to 34, 60% higher than the use rate among women ages 20 to 24 (Figure 2).
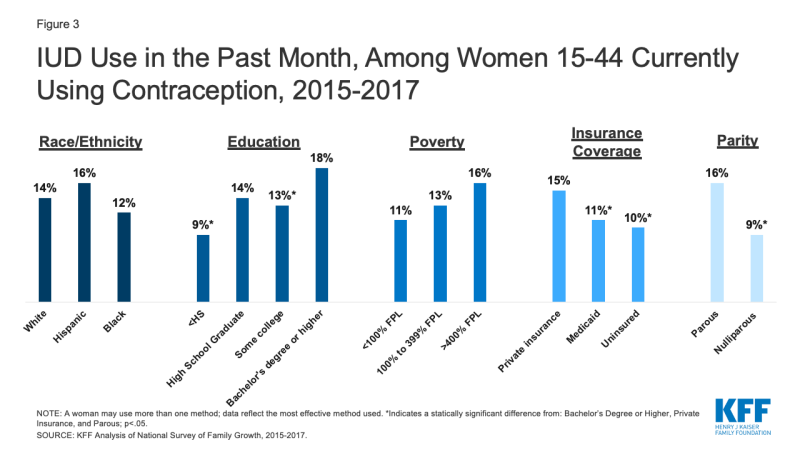
- Women with a Bachelor’s degree or higher, private insurance coverage, and women who have given birth are more likely to use IUDs compared to women without high school degrees, women who are uninsured or have Medicaid coverage, and women who have never given birth (Figure 3). While women with children report higher use of IUDs, this trend may be changing as newer IUDs are marketed to nulliparous women.
- Use of IUDs varies significantly between countries, but is higher in many other countries than in the U.S., especially western Europe where the Dalkon Shield, one of the products that resulted in harm to women in the U.S. in the 1970s, was never available.
- Since the FDA approved IUDs for younger women and those who have not had children, multiple provider groups including the American College of Obstetricians and Gynecologists (ACOG) and the American Academy of Pediatrics (AAP) have recommended the use of IUDs for all women.
Awareness and Availability
- A 2017 survey of providers found that almost all obstetricians and gynecologists (ob/gyns) provide IUDs in their practice (91%) and offer IUDs to patients under the age of 21 (92%). This is in contrast to findings from a 2013 survey that found that just two-thirds (63%) of ob/gyns who provided IUD services at that time believed IUDs were appropriate for nulliparous women and less than half (43%) believed they were appropriate for adolescents. This may reflect recent increases in provider education as well as approval of new IUDs targeted specifically towards younger women.
- Currently, many physicians require two visits for a woman seeking an IUD: a consultation and the follow up visit for insertion. Stocking IUDs onsite allows clinicians to provide same-day services to women, but some providers have been hesitant to stock IUDs because of the high upfront costs.
- Community health centers (CHCs) are an important source of care for many low-income and uninsured women of reproductive age. However, access to IUDs has been challenging for some CHCs due to a combination of reasons, including high upfront costs and limited training and staff capacity to provide IUDs. Over half of community health centers provide IUDs or implants as part of the family planning services they offer, meaning many women seeking services from clinics may not have immediate access to IUDs.
Post pregnancy
- Providing IUDs to women immediately following a delivery, miscarriage or abortion can be convenient and an effective strategy for averting unintended pregnancy. Women may be particularly motivated to begin using contraception in the immediate postpartum period, and data indicate women are more likely to obtain an IUD in the immediate postpartum period compared to a follow-up visit. Although expulsion rates of IUDs are higher for postpartum women, they are lower when the IUD is inserted approximately 10 minutes after the placental delivery than if the IUD is inserted up to four weeks after the birth.
- IUD insertion immediately postpartum is not common. A 2017 survey of providers found that only 19% of ob/gyns reported offering immediate postpartum IUDs. Some providers may be unaware that IUD insertion post-pregnancy is safe and effective. Less than half of ob/gyns interviewed in a 2013 study (46%) said an IUD could be inserted immediately after birth and only one-fifth (20%) said IUDs could be inserted after an abortion or a miscarriage. Women with IUDs have lower rates of repeat abortion than women who choose other methods.
Insurance Coverage and Financing of IUDs
The costs of IUDs have been a barrier to its use, for both patients and providers. Prices for an IUD typically range between $500 and $1,300, in addition to provider visits for insertion, removal and confirmation that the device was properly placed. While many insurance plans have covered IUDs for years, prior to the passage of the Affordable Care Act (ACA), women were likely to have out-of-pocket charges for the product as well as the associated visits. The ACA has eliminated these costs for many women.
Private Insurance
- The ACA includes a requirement that most private insurance plans must cover at least one type of all 18 FDA-approved contraceptive methods for women as prescribed without cost sharing. This means that most private plans (small and large group, self-funded, and individually purchased plans) must cover the copper IUD and at least one hormonal IUD at no cost to policy holders. Research has found two-thirds of women (64%) with private insurance paid $0 in out of pocket costs for an IUD in 2016, compared to 39% of women in 2012. Average out-of-pocket spending for IUDs went from $118 in 2012 to $28 in 2016. Studies have also found an increase in LARC initiation among women with private insurance coverage after the implementation of the ACA contraceptive mandate.
- Although insurers are required to cover at least one hormonal IUD, the plan determines which hormonal IUD is covered. Plans must cover an alternate hormonal IUD if medically necessary.
- Insurers can use medical management to help control costs and encourage beneficiaries to choose more affordable contraceptive methods. While insurers can require step therapy and prior authorization, federal guidance prohibits insurers from categorically restricting access to a method. Insurers can choose to cover generic contraceptives only while charging cost-sharing for the brand-name version, but since IUDs do not have a generic equivalent, the brand name version must be covered without cost sharing.
Medicaid
- Federal law requires Medicaid programs to cover family planning services and supplies without cost-sharing, but there are variations in coverage between states and between different Medicaid populations. For women enrolled in traditional Medicaid programs that were in place prior to the passage of the ACA, coverage of IUDs is determined by each state program. States policies may limit coverage to only certain brands or types or apply medical management protocols to restrict availability.
- Women who qualify for Medicaid under the ACA’s expansion of the program must receive coverage for both the copper and at least one hormonal IUD because the ACA requires these expansion programs to cover all FDA approved methods for women without cost-sharing, which is the same as the requirement for private insurance plans.
- States are considering and adopting a variety of payment policies to facilitate postpartum LARC insertion. Labor and delivery services are typically reimbursed through a single global fee and many providers have reported that the global fee is not sufficient to cover the costs of providing a LARC postpartum at the time of delivery or at the follow up postpartum visit. The absence of a separate fee or an increase in reimbursement has been a disincentive for some providers to provide postpartum LARC. Most states continue to reimburse hospitals through a global fee for postpartum LARC services.
- Currently, 26 states extend Medicaid coverage for family planning services, including contraception, to some uninsured women who do not qualify for full scope Medicaid. States retain the flexibility to decide whether and which IUDs are covered by these programs.
Uninsured
- The federal Title X National Family Planning Program funds a network of clinics to provide family planning care to millions of low-income and uninsured people at reduced or no cost. In previous years the Title X program had emphasized provision of LARCs, but 2019 regulations by the Trump administration now allow clinics that only provide a single family planning method to participate in the Title X program, “as long as the entire project offers a broad range of such family planning methods and services.” This means that clinics that do not provide the full range of methods, including IUDs, may be included in the Title X program.
- Federal recommendations for Providing Quality Family Planning Services (QFP) released by the Centers for Disease Control and Office of Population Affairs recommend that providers offer the full range of FDA approved contraceptive methods to patients who wish to delay or postpone pregnancy. These guidelines recommend that providers talk to patients about their contraceptive options using a tiered approach—talking first about the most effective methods (which include IUDs and implants) before talking about less effective methods.
- As interest in LARC use has grown so have concerns around the promotion of LARCs as the “most effective” methods and the potential for coercion. Some people have reported that they have felt pressured to choose a method of contraception during contraceptive counseling, and have felt that their providers preferred and were even pushing them towards a LARC method. Others reported that their physicians have been resistant and even unwilling to remove their IUDs early. In one study, physicians reported having negative feelings about early IUD removal and some had encouraged patients not to remove their IUD early. Researchers have recommended that instead of first talking about LARCs and how effective they are, providers should first discuss with their patients their contraceptive preferences and reproductive goals, and help patients choose a contraceptive method that meets their lifestyle needs.
- Community health centers (CHCs) play a major role in providing reproductive health care to low-income people and medically underserved communities. CHCs are required to provide “voluntary family planning” services but have significant leeway in determining what specific services they provide. A 2017 survey of CHCs found that over half of sites provided LARC methods on-site—64% offered hormonal IUDs (such as Mirena, Skyla, Liletta) and 55% offered copper IUDs. The same survey found that sites that received Title X funds were consistently more likely to offer IUDs compared to sites that did not receive Title X funding.
- Some manufacturers operate programs that offer reduced price or fully subsidized IUDs for some low-income people. IUD manufacturers may also offer installment plans for those who purchase IUDs directly and have no other coverage.
- Studies have found young women are very likely to choose the most effective methods of contraception when cost barriers are removed. The Contraceptive CHOICE Project offered young women seeking care at Title X clinics in Colorado and at Washington University in St. Louis, contraception without cost-sharing. More than half of women chose an IUD as their method of contraception. Continuation rates among participants who chose IUDs (77-79%) were significantly higher than non-LARC users (41%) 24 months after choosing their method. High continuation rates among IUD users have been documented in other studies looking at national claims data.
Conclusion
IUDs are one of the most effective forms of reversible contraception and interest in continues to grow. While use of IUDs is still relatively low compared to some other methods, the ACA’s requirement for coverage of contraceptive services and supplies without cost-sharing removes cost barriers for millions of women with private coverage. The elimination of the cost related barriers along with greater awareness and acceptance of IUDs among clinicians and patients will likely continue to increase the use of one of the most effective methods of contraceptive available in the U.S.
Endnotes
Data and research often presume cisgender identities and may not systematically account for people who are transgender and non-binary. The language used in this brief attempts to be as inclusive as possible while acknowledging that the data we are citing uses gender labels that we cannot change without misrepresenting the data.
KFF analysis of the National Growth Family Survey, 2015-2017.