Trends in State Medicaid Programs: Looking Back and Looking Ahead
Section 5: Managed Care and Delivery System Reform
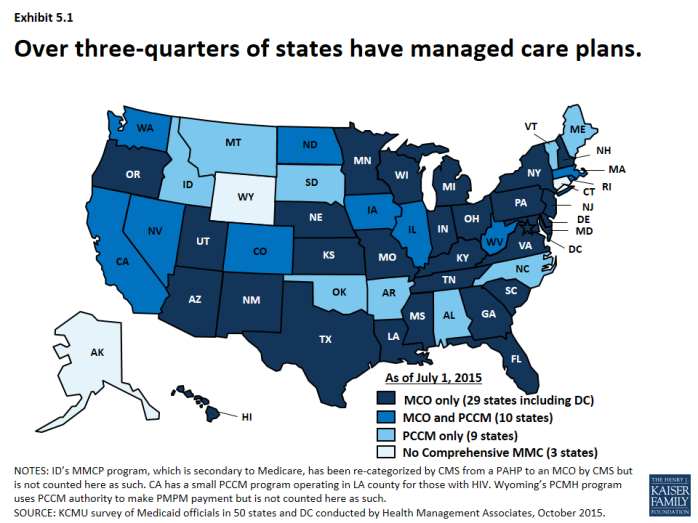
Managed care has become the predominant delivery system for Medicaid in most states, as Medicaid programs have increasingly turned to managed care as a means to help ensure access, improve quality and achieve budget certainty. As of July 2015, a total of 48 states used some form of managed care to serve the Medicaid population, including 39 states (including DC) that contracted with risk-based managed care organizations (MCOs) to serve their Medicaid enrollees. (Exhibit 5.1) States have also increased their focus on new and emerging models of delivery system and payment reform efforts, such as patient-centered medical homes, health homes accountable care organizations among others.
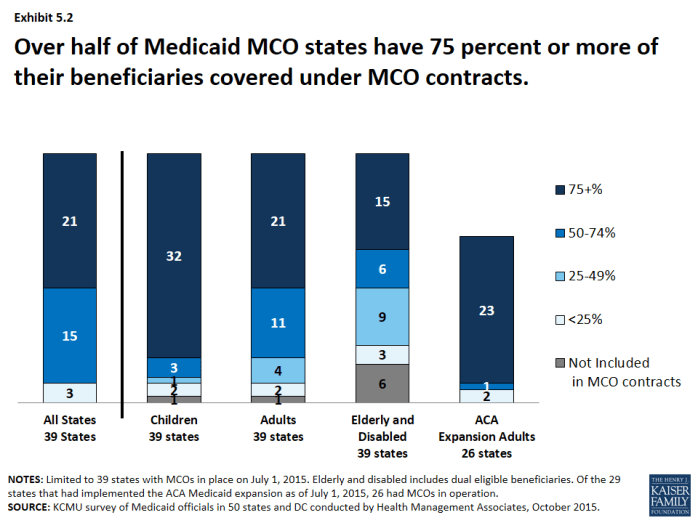
Over the last 15 years, Medicaid delivery systems have significantly shifted to managed care. States have continued to expand their use of managed care by expanding geographically to new regions, adding new populations, making managed care enrollment mandatory for new populations among other changes. States have also been shifting from primary care case management programs (PCCMs) to MCOs. As of July 2015, 21 states with Medicaid MCOs reported at least 75 percent of all Medicaid beneficiaries were enrolled in MCOs. (Exhibit 5.2)
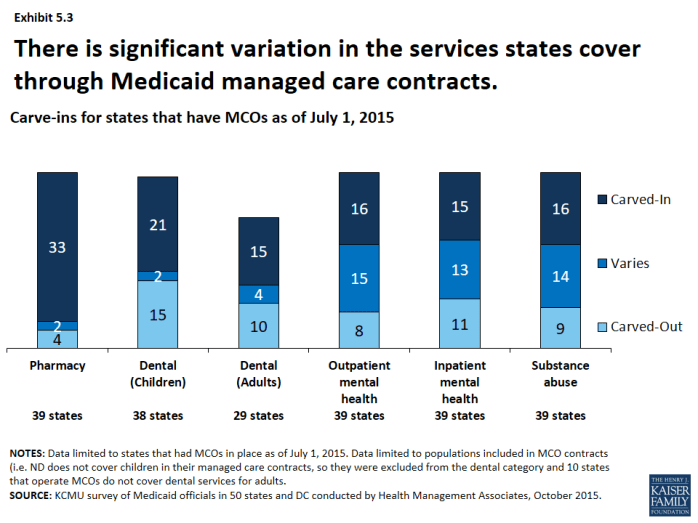
A growing number of states are focusing on integration of physical health, behavioral health and long-term services and supports (LTSS) under the umbrella of managed care. In SFY 2015, most states with MCOs had pharmacy services carved-in for the populations covered by their MCOs1 as well as dental services (for both children and adults in those states that cover this benefit for adults). There was more variation in managed care’s role in the delivery of behavioral health, though more states are looking at carving such services into MCO contracts. (Exhibit 5.3) Additionally, more states are exploring capitated arrangements for long term services and supports though this varies significantly.
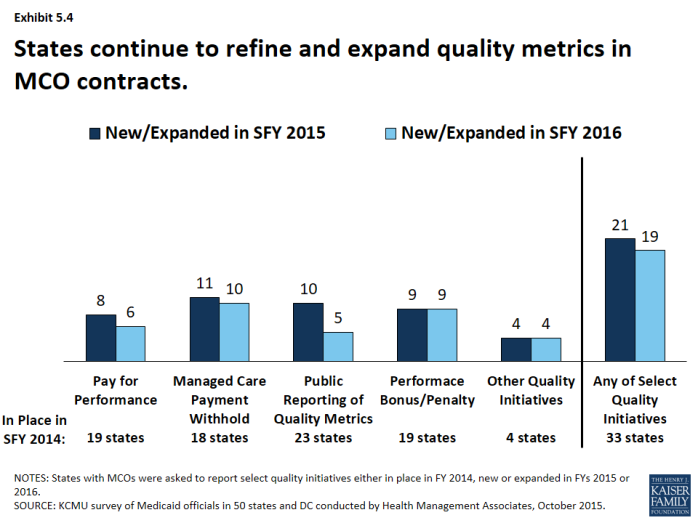
With greater utilization of MCOs has come greater focus on quality performance. All states with MCO programs track one or more quality measures and require other health plan quality activities to improve health care outcomes and plan performance. A majority (23 states) publicly reported or required MCOs to publicly report quality metrics (e.g., a “report card”), and over one-third had pay-for-performance provisions, capitation withholds, and performance bonuses or penalties in place in SFY 2014 as well. (Exhibit 5.4) In SFY 2015, a total of 21 states implemented new or expanded quality initiatives and 19 states planned to do so in FY 2016. The most common new or expanded initiative in SFYs 2015 and 2016 was managed care payment withholds tied to quality performance.
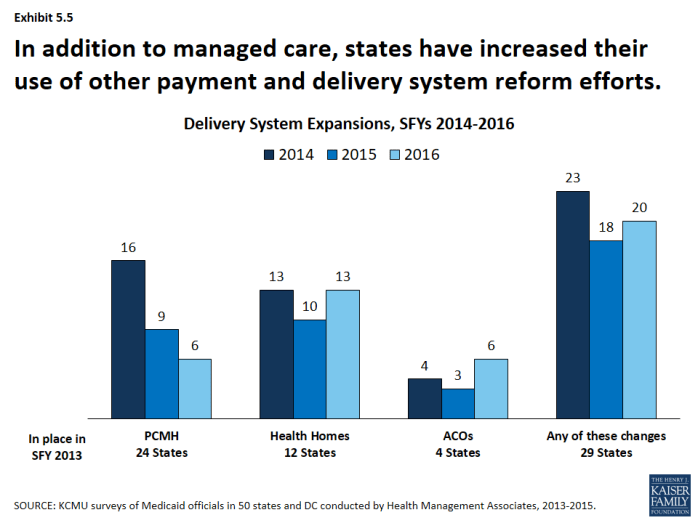
States are also adopting other payment and delivery reforms including patient-centered medical homes, health homes accountable care organizations among others. Nearly half of states had PCMHs in place in SFY 2013. Additionally, twelve states had at least 1 health home, an option made available under the ACA, in place in SFY 2013 and 4 states had Accountable Care Organizations in place in SFY 2013. Interest in all of these options has been growing; one-third to almost half of states have reported actions to expand or newly implement these reforms either in conjunction with or independently of managed care contracts. (Exhibit 5.5) A few states have also implemented episodes of care payment structures as well as other payment reforms under DSRIP waivers. States also continue to explore these and other innovations in payment and delivery system reform with a heightened focus on integration of physical and behavioral health services, social determinants of health and population health.