Community Health Centers and Medication-Assisted Treatment for Opioid Use Disorder
Introduction
As the country struggles to respond to the coronavirus pandemic, emerging evidence suggests drug overdoses are increasing sharply, with an estimated 18% increase in overdoses since the start of stay-at-home orders in March through May 2020.1 The increase in overdoses is driven in part by the isolation, stigma, economic turmoil, and disruption in access to health care services caused by coronavirus.2,3 Many of these overdoses are also related to the ongoing opioid crisis, which affects roughly two million Americans with opioid use disorder (OUD) and was linked to over 50,000 opioid overdose deaths in 2019.4,5 Even prior to the coronavirus pandemic, access to OUD treatment was limited—only one in five people experiencing OUD received addiction treatment in 2018.6 Existing gaps in OUD treatment services have likely been exacerbated by the current crisis.
Community health centers play a significant role in addressing the opioid crisis as community-based primary care providers with the capacity to screen, treat, refer, and provide supportive services such as case management to patients experiencing OUD. Increasingly, health centers are providing medication-assisted treatment (MAT), which is considered to be the standard of care for OUD treatment.7 MAT includes treatment with one of three medications (methadone, naltrexone, and buprenorphine) along with counseling.8 Health centers primarily serve low-income populations who may otherwise have difficulty accessing affordable health care. Residents of the medically underserved communities in which health centers operate, including those experiencing OUD, are disproportionately uninsured, enrolled in Medicaid, or earn less than 200% of the federal poverty level.9
Between 2016 and 2019, the Health Resources and Services Administration (HRSA) awarded more than $1.4 billion in federal grants10,11,12,13,14 to enable health centers to expand access to mental health and substance use disorder (SUD) services. Health centers used these grants to increase staff, to improve the integration of behavioral health and primary care, and to expand delivery of MAT.15 National data show that health centers increased their mental health and SUD staff by 51% from 2016-2019,16 with the vast majority (95%) of health centers offering mental health and/or SUD services onsite in 2018 (the latest year these data are available).17 Currently, health centers are eligible for a number of other federal grants to mitigate the steep revenue losses due to the coronavirus pandemic,18 although these grants are meant to support health center capacity generally or to provide COVID-19 testing, rather than targeting OUD services specifically. Given the considerable federal investment in health centers to combat the opioid crisis as well as the increasing need for OUD services during the pandemic, it is important to understand health centers’ capacity to deliver MAT and the barriers they continue to face in providing OUD services.
This brief presents findings from a survey of health centers conducted in 2019, focusing on questions that examine community health centers’ provision of MAT services and capacity. Where possible, we highlight one-year trends from a 2018 community health center survey. We also highlight differences across health centers in Medicaid expansion and non-expansion states when the differences are significant. While the findings reflect health center responses before the coronavirus pandemic, they provide important context for understanding the issues health centers faced in providing MAT services prior to the pandemic and challenges that will likely persist following the pandemic’s resolution.
Treating Patients with Opioid Use Disorder
Over seven in ten health centers (71%) reported an increase in the number of patients with OUD from 2018 to 2019. Similar shares of health centers reported an increase in the number of patients with prescription OUD (62%) and nonprescription OUD, such as fentanyl or heroin (65%, Figure 1). These findings are generally consistent with provisional data on opioid overdose deaths in the U.S. that show an increase for 2019.19 The growth in health center patients experiencing OUD was likely due to a variety of factors, including new patients with OUD seeking care, improved screening practices to identify patients experiencing OUD, or an improved capacity at health centers to provide OUD services to more patients.
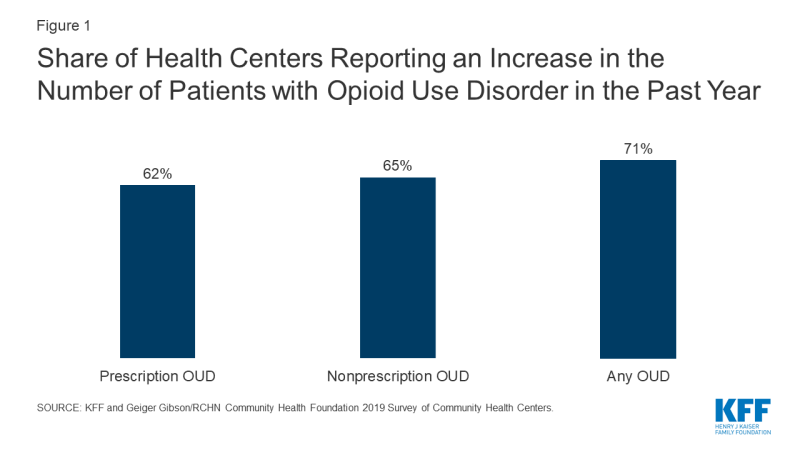
Figure 1: Share of Health Centers Reporting an Increase in the Number of Patients with Opioid Use Disorder in the Past Year
There was substantial growth in the number of health centers providing onsite MAT services from 2018 to 2019, particularly in Medicaid expansion states. Nearly two-thirds of health centers (64%) reported that they provide MAT medications, up from 48% in 2018, and the vast majority of these (87%) provide counseling as well. Health centers in Medicaid expansion states were more likely than those in non-expansion states to provide onsite MAT services (70% vs. 50%, Figure 2). The difference in MAT availability may be attributable to a greater OUD prevalence in Medicaid expansion states, which experienced an opioid-involved death rate of 16.1 per 100,000 population in 2018 (the latest year these data are available), compared to 11.4 per 100,000 in non-expansion states.20 However, the difference in MAT availability is also likely related to increased revenue for OUD services in expansion states, since the Medicaid program reaches many of the adults most at risk for OUD. Other research has demonstrated a connection between Medicaid expansion and health center capacity.21,22 At the same time, the availability of grant funding since 2016 has helped to ensure that health centers in both expansion and non-expansion states have been able to expand mental health and SUD services.
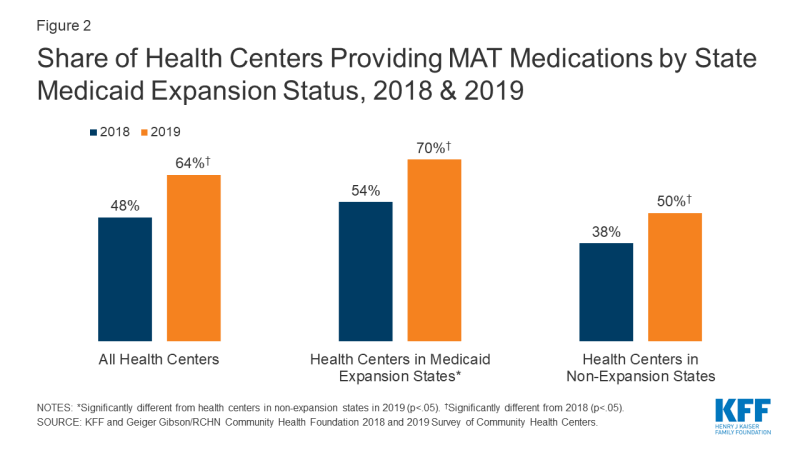
Figure 2: Share of Health Centers Providing MAT Medications by State Medicaid Expansion Status, 2018 & 2019
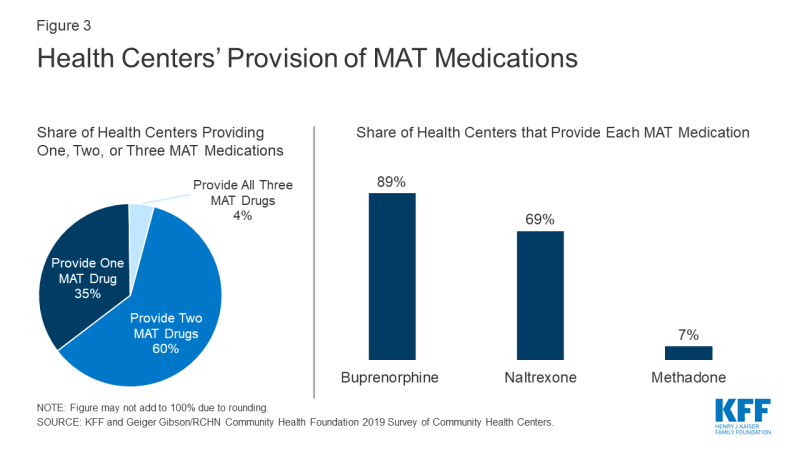
Most health centers that provide MAT services offer more than one medication, which gives providers options to meet patients’ needs. Among health centers that reported providing MAT, 60% offer two MAT drugs and 4% offer all three, while roughly one-third (35%) offer only one MAT drug (Figure 3). The most widely available drug is buprenorphine, with 89% of health centers that provide MAT medications reporting they provide it. A slightly smaller share (69%) reported offering naltrexone, and only 7% of health centers providing MAT medications reported offering methadone. Facilities must be certified as opioid treatment programs (OTPs) in order to dispense methadone, while buprenorphine and naltrexone can be prescribed in any setting where providers have a Drug Abuse Treatment Act of 2000 (DATA) waiver from the federal government.23 Currently, all state Medicaid programs cover buprenorphine and naltrexone, although only 41 state programs cover methadone.24 As part of a broader initiative to combat the opioid crisis, the SUPPORT Act, signed into law in 2018, will require all state Medicaid programs to cover all three MAT medications, counseling services, and behavioral therapy from October 2020 through September 2025,25,26 although providers will still need to be certified OTPs to dispense methadone.
Health centers with a MAT program are more likely than those without to refer patients to services across the continuum of care for OUD. Depending on patients’ needs, OUD treatment may require services other than MAT. Some may require less intensive care such as recovery coaches or peer mentors. Others experiencing OUD may require more intensive services such as partial hospitalization programs, residential treatment programs, and inpatient detox programs. Health centers with MAT programs are more likely than health centers without a program to refer to providers offering specific services that are generally unavailable in health centers or other primary care settings, such as partial hospitalization and residential treatment programs (Figure 4). In contrast, health centers without a MAT program are more likely to refer to outpatient providers who could offer MAT, including health departments, certified behavioral health clinics, opioid treatment programs, and some primary care clinics. Relatively few health centers (7%) do not make any referrals for patients with OUD, and it is unclear whether the few that make no referrals do so because there is no perceived need for referrals or because there is a lack of OUD treatment providers in the community that accept Medicaid and uninsured patients, among other plausible explanations.
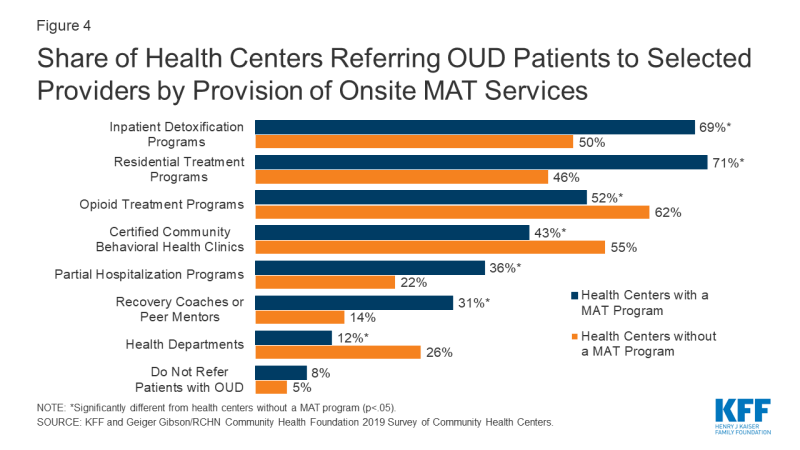
Figure 4: Share of Health Centers Referring OUD Patients to Selected Providers by Provision of Onsite MAT Services
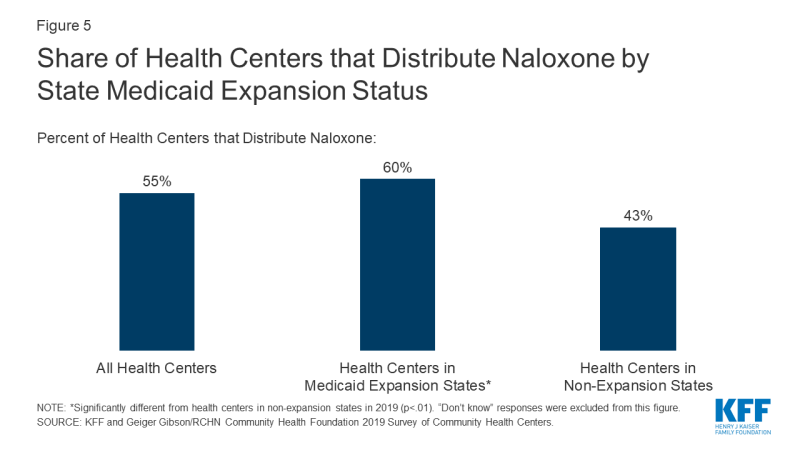
Roughly half of health centers (55%) distribute naloxone, an opioid overdose reversal drug. Even though naloxone is different from medications used in MAT for addiction, the continued, high rates of opioid overdose deaths have made naloxone (brand names include Narcan and Evzio) a critical tool in minimizing fatalities due to the opioid crisis, especially as suspected overdoses have risen during the coronavirus pandemic. Health centers in Medicaid expansion states were more likely to report providing naloxone than those in non-expansion states (60% vs. 43%, Figure 5), which could reflect underlying pharmacy policy, such as availability of naloxone without prior authorization, in these states.27
Treatment Capacity Challenges
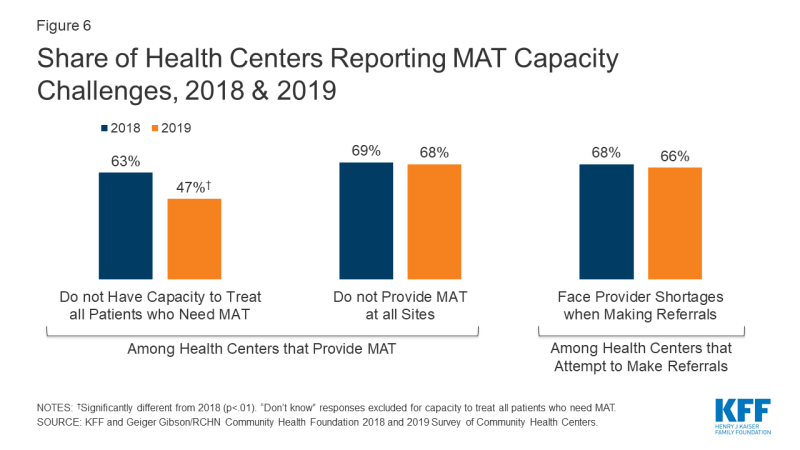
Health centers faced many challenges in meeting the high demand for treatment among their patients with OUD even before the recent surge in need. Nearly half (47%) of health centers operating a MAT program reported that they do not have the capacity to treat all patients seeking MAT (Figure 6). However, fewer health centers reported capacity issues in 2019 compared to 2018, when 63% of health centers operating a MAT program reported that they could not provide MAT services to all patients in need. Nearly seven in ten (68%) health centers that offer MAT services did not provide them at all sites, a rate that was stable between 2018 and 2019. Nearly three-quarters (74%) of all health centers (whether they provide MAT onsite or not) reported they refer patients for MAT services to other providers in the community. Among those health centers, two-thirds (66%) reported facing provider shortages when they attempted to refer patients, which was similar to the 68% reported in 2018.
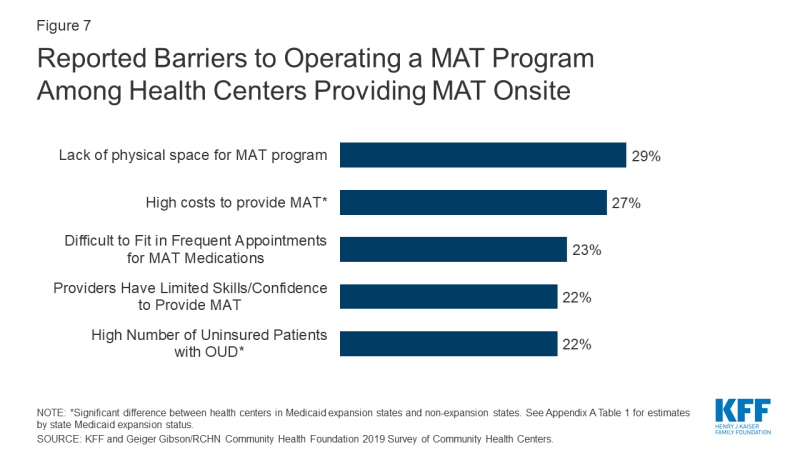
Health centers with a MAT program cited a lack of physical space and high costs as top barriers to operating their programs. Nearly three in ten (29%) health centers with a MAT program reported that a lack of physical space was a barrier to operating their MAT program, which generally requires dedicated counseling space (for individual or group sessions) in addition to visits for prescriptions (Figure 7). Additionally, over a quarter (27%) of health centers with a MAT program said high costs hindered MAT program operations. Health centers in non-expansion states were more likely than health centers in expansion states to cite high costs (40% vs. 23%) and high numbers of uninsured patients (41% vs. 16%) as barriers to operating a MAT program (Appendix A Table 1). While federal grants have helped to increase the number of health centers providing MAT, those grants do not seem to be covering all operating expenses. Health centers in Medicaid expansion states appear to benefit from greater Medicaid enrollment, which results in payment for MAT program expenses that can make their programs sustainable, although high costs are still a significant barrier in both expansion and non-expansion states alike.
Health centers without a MAT program cited provider concerns as a top barrier to establishing a MAT program. Limited skills and/or confidence among providers to provide MAT services was the most common barrier (42%) to establishing a MAT program reported by health centers without a program, underscoring limited resources, capacity, or availability for provider training and technical assistance (Figure 8). Additionally, these health centers reported provider concerns about diversion – where patients transfer prescribed MAT medications to others – as a common barrier (33%). The second-most common barrier (37%) reported by health centers without a MAT program was a lack of physical space (Appendix A Table 2). This problem persists for health centers with or without a MAT program, as many health centers face the common challenge of balancing limited resources with patient needs. For example, 18% of health centers without a MAT program reported that either OUD was not a significant problem at their health center and/or their health center leadership have not identified OUD as a priority area of focus, likely reflecting the wide range of health needs in the communities in which health centers operate.

Figure 8: Reported Barriers to Establishing a MAT Program Among Health Centers that do not Provide MAT Onsite
Looking Ahead
As a nationwide resource of community-based, safety net primary care providers, health centers play a key role in combatting the ongoing opioid crisis, especially as new reports show increases in suspected drug overdoses during the coronavirus pandemic. The majority of health centers provide MAT services to address the treatment needs of patients with OUD, and many health centers also distribute naloxone for opioid overdose reversal. Because of the broader coverage of patients and treatment services in Medicaid expansion states, health centers in expansion states appear to be better equipped to address demand for OUD services, including by providing MAT onsite and distributing naloxone. Although SUD service expansion grants helped to establish new MAT programs and bolster existing services, these grants do not fully address the ongoing, long-term costs associated with operating a MAT program, and health centers still reported challenges recruiting providers even with grant funding. While health centers in Medicaid expansion states were less likely than those in non-expansion states to cite costs as a barrier to operating MAT programs, costs still remain a barrier for many health centers, regardless of their state’s expansion status.
Health centers will face ongoing challenges in meeting demand for OUD treatment, including many new challenges caused by the social and economic disruptions from the coronavirus pandemic that were not captured in this survey. Health centers have had to fundamentally revamp their service delivery model due to social distancing measures, demand for testing services, and drops in patient visits, while at the same time facing revenue declines, temporary site closures, and a shrinking workforce.28 In response, health centers have increased the use of telehealth as some states have eased restrictions on e-prescribing MAT medications. However, access to MAT treatment remains limited in some areas and returning to normal operations will be difficult for the foreseeable future and even after a coronavirus vaccine allows life to return to some normalcy. Given the role that health centers play in delivering MAT services, particularly in areas with the greatest accessibility barriers, their ability to continue providing these services during the pandemic and after will influence broader efforts to address the opioid crisis.