Medicaid Coverage of Pregnancy and Perinatal Benefits: Results from a State Survey
Kathy Gifford, Jenna Walls, Usha Ranji, Alina Salganicoff, and Ivette Gomez
Published:
Executive Summary
An updated version of this report was released on May 19, 2022 and can be found here.
Correction: While KY and MS responded to the survey that their states cover doula services, subsequent research has found that the states do not cover doula services. To our knowledge, OR and MN, and as of January 2021, NJ, are the only states currently covering doula services.
Overview
Maternity care has emerged as a key issue in the current policy debates about the future of the Affordable Care Act (ACA) and Medicaid restructuring. While the inclusion of maternity care as an essential health benefit has been important to many women who gained private coverage because of the ACA coverage expansion, Medicaid has been the primary funding source for perinatal and maternal services for low-income women in the US for several decades. In 2010, Medicaid financed nearly 45% of all births in the United States.1 By federal law, all states provide Medicaid coverage for pregnancy-related services to pregnant women with incomes up to 133% of the federal poverty level (FPL) and cover them up to 60 days postpartum. All states must provide some level of maternity care free of cost-sharing to eligible pregnant women, although there are state level variations in the scope and type of services that states offer. In addition, many states extend eligibility to pregnant women with incomes considerably higher than this threshold. The ACA broadened Medicaid eligibility by allowing states to extend continuous Medicaid eligibility in 2014 to individuals with family income at or below 138% FPL and 31 states and the District of Columbia (DC) have adopted Medicaid expansion programs which extended coverage for new mothers beyond the postpartum period, where historically many women lost coverage. 2
Because there is no formal federal definition of what services states must cover for pregnant women beyond inpatient and outpatient hospital care, states have considerable discretion to determine the specific scope of maternity care benefits. While the ACA also does not define maternity benefits, states that have expanded Medicaid eligibility under the ACA must cover all preventive services recommended by the United States Preventive Services Task Force (USPSTF) for beneficiaries that qualify as a result of the ACA expansion. These now include many pregnancy-related services, such as prenatal screenings, folic acid supplements, and breastfeeding supports for those who qualify for Medicaid as a result of the expansion. This coverage requirement, however, does not apply to any of the Medicaid eligibility pathways that were available prior to the ACA (i.e., for parents or pregnant women). As a result, there is leeway for states to vary coverage standards for different Medicaid eligibility pathways (e.g. traditional Medicaid available prior to the ACA, ACA Medicaid expansion, or pregnancy-related eligibility).
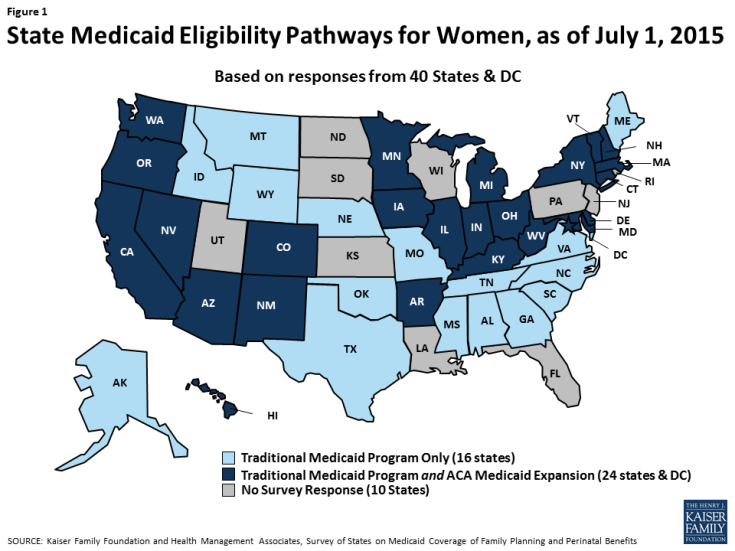
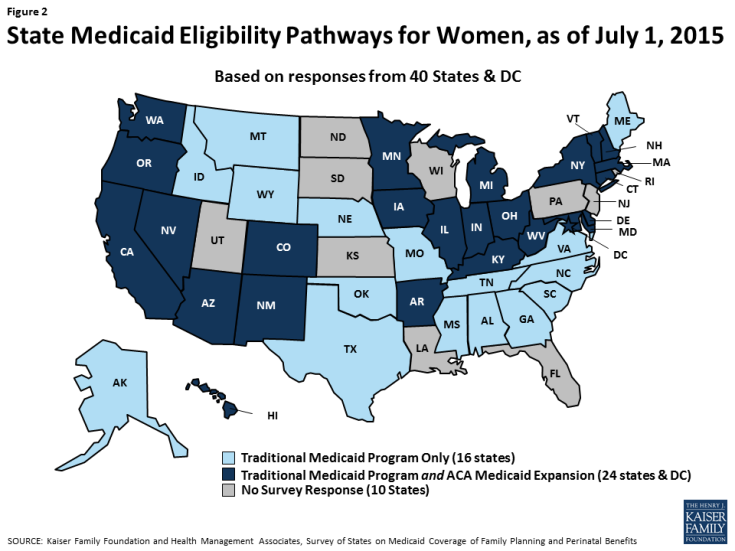
To understand how states were covering services under Medicaid in the wake of the ACA expansions, the Kaiser Family Foundation and Health Management Associates conducted a survey of states about the status of Medicaid benefit policies for perinatal and family planning services across the nation. With 31 states and DC adopting Medicaid expansions, the extent to which states had decided to make their programs consistent across the different eligibility categories was unknown. This report, a companion to the Family Planning Report, asked states about benefits in place as of July 1, 2015 for women enrolled in fee-for-service Medicaid through different eligibility pathways, including traditional pre-ACA Medicaid pathways, expansion, and pregnancy-related eligibility for the following services: basic prenatal care, counseling and support services, delivery and postpartum care, and breastfeeding supports. This report presents survey findings for the 40 states and DC that provided responses to the survey. Throughout the report, DC is counted as a state, totaling 41 respondents. As illustrated in Figure 1, of the 41 respondents, 24 states and DC had adopted the ACA Medicaid expansion as of July 1, 2015. This report is the only one we know of that has examined Medicaid benefits for maternity care since the ACA’s passage.
Key Findings
While the benefits requirements vary between eligibility pathways, one overarching finding from the survey is that most states provide the same benefits to beneficiaries who qualify through Medicaid’s pregnancy eligibility pathway and adult pathway. Some states reported that in fact, they do not distinguish between the traditional full-scope Medicaid and pregnancy eligibility pathways in terms of the covered benefits. The survey questions covered four broad topics: prenatal services, counseling and support services, delivery and postpartum care, and breastfeeding services. Key findings on these topics are:
Prenatal Services
Prenatal care services monitor the progress of a pregnancy and identify and address potential problems before they become serious for either the mother or baby. Routine prenatal care encompasses a variety of services, including provider counseling, assessment of fetal development, genetic screening and testing, prenatal vitamins that contain folic acid and other nutrients, and ultrasounds, which provide important information about the progress of the pregnancy.
- All survey states reported that they cover prenatal vitamins and ultrasounds for pregnant women. However, some states impose quantity limits or require a prescription for vitamins.
- Nearly all responding states (38/41) reported covering amniocentesis and chorionic villus sampling (CVS) tests across all eligibility pathways available in the state, but fewer states (33/41) reported covering genetic counseling, some of which limit the service to women with higher risk or that have a positive result in genetic screens.
Counseling and Support Services
There are a variety of support services that can aid pregnant and postpartum women with pregnancy, delivery, and child rearing and improve birth outcomes. These include educational classes on childbirth and infant care, transportation to appointments, and home visits during or after pregnancy to assist with basic medical care, counseling on healthy behaviors, and in-person infant care assistance.
- Less than half of the responding states report that they provide education services to support childbirth, infant care or parenting in any of the Medicaid eligibility pathways. However, in some states services may be available through other public programs.
- Nearly all responding states provide substance or alcohol abuse treatment services for pregnant or postpartum women in most of the Medicaid eligibility pathways.
- Approximately three-fourths of the responding states cover prenatal and postpartum home visits, which give the opportunity for nurses and other clinicians to assist pregnant women and new parents in their homes with pregnancy management and child rearing skills.
Delivery and Postpartum Care
While all states are required to cover inpatient hospital care for Medicaid enrollees, there is more variation in coverage for delivery at birth centers or home births. Coverage for deliveries at birth centers is required in all states that license such facilities. In addition, coverage for doula assistance, which pays for a trained non-clinician to assist a woman before, during and/or after childbirth, by providing physical assistance, labor coaching, emotional support, and postpartum care is rare.
- A majority of responding states cover deliveries in birth centers, while half of the states cover home deliveries.
- Of all the services covered in the survey, coverage was lowest for doula Only four states reported that they cover doula assistance for women.
Breastfeeding Services
- There is a range of supports that have been found to help women initiate and maintain breastfeeding. These include breast pumps, lactation counseling by certified consultants both inpatient and outpatient after delivery, and educational programs, which can begin during pregnancy and continue after the birth of a child. States are required to cover breast pumps and consultation services for Medicaid expansion beneficiaries under the ACA’s preventive services requirement. A majority of responding states cover both electric and manual breast pumps, but some report using various utilization controls such as prior authorization and quantity limits.
- While most responding states report that breastfeeding education and hospital-based lactation consultations are covered under traditional Medicaid, far fewer states continue coverage once the woman goes home.
Conclusion
The analysis of state responses to this survey found that overall most states cover a broad range of perinatal services in their full scope traditional Medicaid program, under full scope ACA Medicaid expansion, and pregnancy-related eligibility pathways. Most, but not all, of the 41 surveyed states report that they cover basic prenatal services such as ultrasounds and vitamins, prenatal genetic testing, home visits, delivery in birth centers, postpartum visits, and breast pumps for nursing mothers. Many states recognize that these services are critical to improving birth outcomes. Coverage for services that help women and their families care for their children after delivery, such as childbirth and parenting classes, breastfeeding education and lactation consultation is less common (Table 1). Only half of reporting states cover home births, and very few states cover doula supports despite research suggesting that this assistance results in better health outcomes.3 While coverage requirements differ between eligibility pathways, in general, there is strong alignment within states across the various pathways.
The Medicaid program has a long history and excellent record of providing coverage for low-income pregnant women, with nearly half of all births nationwide provided through the program. Regardless of the outcome of current debates over the future of Medicaid or the ACA, the millions of low-income pregnant women that are served by Medicaid will continue to need to have access to coverage that includes the broad range of pregnancy-related services that help assure healthy maternal and infant outcomes.
| Table 1: Summary Results on Coverage of Selected Perinatal Services | |
| States Reporting Coverage Under Traditional Medicaid: | |
| Prenatal Services | |
| Genetic Counseling (33/41 states) | AR, CA, CO, CT, DC, DE, GA, HI, IA, IL, IN, KY, MA, MD, ME, MI, MN, MO, MS, MT, NC, NH, NV, NY, OH, OK, OR, SC, TN, TX, VA, VT, WA |
| Chronic Villus Sampling and Amniocentesis (38/41 states) | AK, AR, AZ, CA, CO, CT, DC, DE, GA, HI, IA, ID, IL, IN, KY, MA, MD, ME, MI, MN, MO, MS, MT, NC, NH, NM, NV, NY, OH, OK, OR, SC, TN, TX, VA, VT, WA, WV |
| Counseling and Support Services | |
| Case Management (35/41 states) | AK, AL, AR, AZ, CA, CO, DC, DE, GA, IA, ID, IL, IN, KY, MA, ME, MN, MO, MS, MT, NC, NE, NM, NV, NY, OH, OK, OR, TN, TX, VA, VT, WA, WV, WY |
| Substance Alcohol Abuse Treatment (40/41 states) | AK, AL, AR, AZ, CA, CO, CT, DC, DE, GA, HI, IA, ID, IL, IN, KY, MA, MD, ME, MI, MN, MO, MS, MT, NC, NE, NM, NV, NY, OH, OK, OR, SC, TN, TX, VA, VT, WA, WV, WY |
| Prenatal and Postpartum Home Visits (30/41 states) | AK, AR, CA, CT, DC, DE, GA, IA, ID, IL, IN, MA, MI, MN, MO, MS, MT, NC, NE, NH, NM, NY, OH, OK, OR, SC, VA, VT, WA, WV |
| Childbirth Education Classes (14/41states) | AR, CA, DC, DE, GA, HI, MI, MN, MS, NC, OH, OR, VA, WA |
| Infant Care/ Parenting Education (17/41 states) | AL, AR, CA, DC, DE, GA, HI, KY, MI, MN, MS, NM, NV, OH, OR, VA, WA |
| Deliveries and Postpartum care | |
| Birth Center Deliveries (32/41 states) | AK, AL, AZ, CA, CO, CT, DC, DE, GA, IA, IL, IN, KY, MA, MD, MN, MO, MT, NC, NE, NH, NM, NV, NY, OH, OK, OR, SC, TN, TX, WA, WV |
| Home Births (21/ 41 states) | AK, AZ, CA, CO, CT, IA, ID, IL, MD, MO, NH, NM, NY, OH, OR, SC, TX, VA, VT, WA, WV |
| Doula Services (4/41 states) | KY, MN, MS, OR |
| Postpartum Visit (41/41 states) | AK, AL, AR, AZ, CA, CO, CT, DC, DE, GA, HI, IA, ID, IL, IN, KY, MA, MD, ME, MI, MN, MO, MS, MT, NC, NE, NH, NM, NV, NY, OH, OK, OR, SC, TN, TX, VA, VT, WA, WV, WY |
| Breastfeeding Services | |
| Breastfeeding Education (27/41 states) | AK, AL, AR, AZ, CA, CO, CT, DC, DE, GA, HI, ID, IN, MA, MI, MN, MO, MS, NC, NV, NY, OH, OK, OR, SC, TN, VA |
| Electric Breast Pumps in Traditional Medicaid Program (35/41 states) | AK, AZ, CA, CO, CT, DC, DE, GA, HI, ID, IL, IN, KY, MA, MD, ME, MI, MN, MO, MS, MT, NE, NH, NM, NY, OH, OK, OR, TN, TX, VA, VT, WA, WV, WY |
| Lactation Consultation in Hospital (26/41 states) | AK, AR, AZ, CA, CO, CT, DC, DE, HI, ID, IN, KY, MI, MN, MO, MS, NC, NE, NY, OH, OK, OR, SC, TN, VA, WA |
| Lactation Consultation in clinic and/or at home (16/41 states) | AR, CA, CO*, CT, DC, DE, HI, MN, MS, NC*, NY, OH, OK*, OR, VA*, WA* |
| NOTES: *CO, NC, OK, VA, & WA cover lactation consultation in clinic, but not in a home visit. | |
***
Introduction
Overview
Medicaid is the leading source of financing for births in the U.S., covering nearly half in 2010.1 While the federal and state governments jointly finance the program, states operate their programs and establish benefits, eligibility and coverage policies subject to broad federal guidelines. While states must provide eligible pregnant women with coverage of inpatient and outpatient medical care, they can make different choices regarding the broad range of pregnancy-related support services and other non-hospital care offered to pregnant women. To understand variations in the scope of coverage for perinatal and family planning services and related state Medicaid policies across the nation, the staff of the Kaiser Family Foundation and Health Management Associates surveyed states about perinatal and family planning services benefit policies that were in place as of July 1, 2015.
The survey was conducted between October 2015 and February 2016. Forty states and the District of Columbia (DC) responded to the survey. Non-responding states are: Florida, Kansas, Louisiana, New Jersey, North Dakota, Pennsylvania, Rhode Island, South Dakota, Utah and Wisconsin. The survey asked states to consider only state Medicaid policies under fee-for-service when responding to the questions. As illustrated in Figure 2, of the 41 respondents, as of July 1, 2015, 24 states and DC had adopted the ACA’s Medicaid expansion and 16 states had not.2
This report presents the survey findings on 41 states’ Medicaid coverage of perinatal services under fee-for-service as of July 2015 (DC is referred to as a state throughout this report, for simplicity). Summary tables are presented throughout the report and more detailed, state-level tables are presented in Appendix A. A companion report summarizing state Medicaid coverage of family planning services is available on the Kaiser Family Foundation’s website.
Background
For decades, Medicaid has been a critical safety net program for pregnant women. In response to increasing rates of infant mortality, Medicaid eligibility levels were increased incrementally throughout the late 1980s and early 1990s to promote access to early prenatal care and to improve birth outcomes. Prior to the ACA, federal law extended mandatory categorical Medicaid eligibility to pregnant women with family incomes up to 133% of the Federal Poverty Level (FPL), although states had the option of setting income thresholds above this level. Furthermore, pregnancy was considered a preexisting condition in the individual insurance market, and most individual policies required a waiting period or costly riders for maternity coverage. Therefore, Medicaid was virtually the only pathway to coverage for uninsured, low-income, pregnant women.
Coverage under the pre-ACA eligibility pathway for “pregnancy-related services” continued for up to 60 days postpartum. At that point, some women qualified for traditional Medicaid coverage as the parent of a dependent child, but many did not as the income threshold for parents was typically much lower than for pregnant women. This means that some women lost Medicaid coverage 60 days after the birth of a child, although their infant would remain eligible for one year.
The ACA allowed states to extend Medicaid coverage to nearly all individuals with incomes up to 138% FPL regardless of category, creating the structure for continuous coverage before, during, and after pregnancy for many more low-income women. In the 19 states that have not adopted the ACA’s Medicaid expansion, pregnant women typically still lose coverage after the 60-day postpartum period because they are no longer eligible for coverage. Since the ACA’s passage, there are now three major pathways to obtain Medicaid coverage for pregnant women (Table 2).
| Table 2: Medicaid Eligibility Pathways for Pregnant Women |
| Pregnancy-only eligibility – Medicaid coverage available prior to the ACA for pregnant women through 60 days postpartum; all states required to cover pregnant women up to at least 133% FPL |
| Traditional Medicaid – Medicaid coverage available prior to the Affordable Care Act (ACA) based on an individual having income below a state’s threshold as well as being in one of the program’s eligibility categories: pregnant woman, parent of children 18 and younger, disabled, or over age 65 |
| ACA Medicaid Expansion – The ACA allowed states to eliminate categorical requirements and extend Medicaid to most women and men with family income at or below 138% FPL. States that have adopted this expansion must cover all recommended preventive services without cost sharing for beneficiaries in this pathway. |
In addition to increasing income eligibility levels, states have taken other steps to facilitate Medicaid coverage for pregnant women, such as presumptive eligibility, which allows providers to grant immediate, temporary Medicaid coverage to women who meet certain criteria while a formal eligibility determination is being made. For example, regular Medicaid coverage may overlay the presumptive eligibility period and provide a full range of services including prenatal vitamins, genetic counseling, case management services for high risk women, non-emergency medical transportation, and substance or alcohol abuse treatment. Pregnant beneficiaries also cannot be charged any cost-sharing under Medicaid.
Prior to the ACA, there were no federal requirements regarding the scope of services provided to pregnant women in traditional Medicaid or under the pregnancy-only pathway and no requirement to standardize coverage across the pathways. For the ACA Medicaid expansion population, however, the law defines a minimum “Alternative Benefit Plan” (ABP) that states must provide to beneficiaries under the Medicaid expansion option. The ACA specifies that the ABP must include 10 “essential health benefits,” including maternity care and preventive care which must be provided at no cost to the patient.3 The preventive care under this policy includes several services related to maternity care, such as prenatal visits, screening tests, folic acid supplements, and breastfeeding supports and equipment rental (Table 3). Benefit policies for traditional (pre-ACA) Medicaid programs and for pregnancy-only eligibility programs, are not bound by the ABP requirements, which means that the benefit packages can vary within states for different Medicaid populations based on their eligibility pathway.
| Table 3: Preventive Services for Pregnant Women Required for Coverage under ACA Medicaid Expansion |
| Anemia screening on a routine basis for pregnant women |
| Bacteriuria urinary tract or other infection for pregnant women |
| Breastfeeding comprehensive support and counseling from trained providers, as well as access to breastfeeding supplies including pumps, for pregnant and nursing women |
| Depression Screening for all adults, including pregnant and postpartum women |
| Folic Acid supplements for women who may become pregnant |
| Gestational diabetes screening for women 24-28 weeks pregnant and those at high risk of developing gestational diabetes |
| Hepatitis B screening for pregnant women at their first prenatal visit |
| HIV screening for all pregnant women, including those in labor who are untested or with unknown HIV Status |
| Rh Incompatibility screening for all pregnant women, and follow-testing for women at higher risk |
| Tobacco use screening and interventions for all women, and expanded for pregnant tobacco users |
| Syphilis screening for all pregnant women and other women at increased risk |
| SOURCE: HHS, Preventive Services Covered Under the Affordable Care Act, September 27, 2012 |
This survey asked states about the scope of coverage for pregnancy-related benefits under multiple eligibility pathways for Medicaid. Detailed findings from 40 states and DC on commonalities and differences between and within states are presented for routine prenatal services, counseling and support services, delivery and postpartum care, and breastfeeding supports. Coverage of postpartum contraception is discussed in a companion report on coverage of family planning services, available on the Kaiser Family Foundation’s website.
Report
Survey Results
Correction: While KY and MS responded to the survey that their states cover doula services, subsequent research has found that the states do not cover doula services. To our knowledge, OR and MN, and as of January 2021, NJ, are the only states currently covering doula services.
Prenatal Services
Prenatal care services monitor the progress of a pregnancy and identify and address potential problems before they become serious for either the mother or baby. Increasing the share of pregnant women who begin care in the first trimester is one of the national objectives of the federal government’s Healthy People 2020 initiative.1 Routine prenatal care encompasses a variety of services, including provider counseling, assessment of fetal development, screening for genetic anomalies, prenatal vitamins that contain folic acid and other nutrients, and ultrasounds, which provide important information about the progress of the pregnancy.
PRENATAL VITAMINS AND ULTRASOUND
| Key Finding: Prenatal Vitamins and Ultrasound |
| All states cover prenatal vitamins and ultrasounds for pregnant women. Some states impose quantity limits or require a prescription for vitamins. |
All states that responded to the survey reported that they cover prenatal vitamins and ultrasounds for pregnant women regardless of eligibility pathway (Table 4). Some states impose limitations on this coverage however, such as requiring a prescription for prenatal vitamins or limits on the number of ultrasounds allowed during the course of a pregnancy.
| Table 4: Coverage and Utilization Controls for Prenatal Vitamins and Ultrasounds | ||||
| Traditional Medicaid (n=41) |
Medicaid ACA Expansion (n=25) |
Pregnancy Only Medicaid (n=41) |
||
| Prenatal Vitamins | 41 | 25 | 41 | |
| Ultrasound | 41 | 25 | 41 | |
| Limitations and Utilization Controls | ||||
| Prenatal Vitamins | Ultrasound | |||
| Prescription or other documentation (4) | AK, CO, CT, NY | |||
| Price/quantity controls (6) | AR | AL, CO, MO, SC, TX | ||
| Prior Authorization to exceed state quantity limits (3) | AL, SC, TX | |||
| Age limitations (1) | MS – limited to ages 8-50 | |||
| Preferred Drug List (PDL) (1) | MS | |||
| Pregnancy status (e.g. high-risk) (2) | TX, WV | |||
Appendix Table A1 provides state detail for states’ prenatal service coverage policies.
Genetic Screening Services
| Key Finding: Genetic Screening Services |
| Nearly all responding states reported covering CVS and amniocentesis across all eligibility pathways available in the state, but fewer states reported covering genetic counseling service, which is generally limited to women with higher risk or for those that have a positive result in genetic screens. |
| Table 5: State Coverage for Genetic Lab and Counseling Services | ||||
| Traditional Medicaid (n=41) |
ACA Medicaid Expansion (n=25) |
Pregnancy Only (n=41) |
Not Covered in Any Pathway (n=41) |
|
| Genetic Counseling | 33 | 21 | 33 | 8 |
| Chronic Villus Sampling | 38 | 24 | 38 | 3 |
| Amniocentesis | 39 | 24 | 39 | 2 |
Routine prenatal care typically includes ultrasound and blood marker analysis to determine the risk of certain birth defects such as sickle cell, down syndrome, or other birth abnormalities. While these tests are effective screening tools to determine risk, they are not diagnostic. If the results of screening tests are abnormal, genetic counseling is recommended and additional testing such as chorionic villus sampling (CVS) or amniocentesis may be needed.
States were questioned about their policies with respect to genetic counseling, CVS, and amniocentesis testing for pregnant women. Of the 41 responding states, 33 reported covering all three services across all eligibility pathways (Table 5). Genetic counseling is covered in fewer states than either of the screening tests. The eight states that do not provide genetic counseling services through any Medicaid pathway are Alabama, Alaska, Arizona, Idaho, Nebraska, New Mexico, West Virginia, and Wyoming. Only one state, Nebraska, does not cover any of the three services under any of its eligibility pathways, but the state noted that genetic testing is covered for the mother and baby with prior authorization after delivery. Few states reported utilization controls or limitations. Medical necessity and an indication of risk for genetic anomalies were the most frequently noted restrictions. Appendix Table A2 provides detail on state Medicaid policies for genetic testing and counseling.
Counseling and Support Services
There are a variety of support services that can aid pregnant and postpartum women with pregnancy, delivery, and child rearing. These include educational classes on childbirth and infant care, transportation to appointments, and home visits during or after pregnancy to assist with basic medical care, counseling on healthy behaviors, and in person infant care assistance.
Childbirth and Parenting Education
| Key Finding: Childbirth & Parenting Education |
| Less than half of the responding states report that they provide education services to support childbirth, infant care or parenting in any of the Medicaid eligibility pathways. |
Less than half of responding states reported that they cover childbirth and parenting education for pregnant women (Table 6). The 13 states that cover both services are: Arkansas, California, District of Columbia, Delaware, Georgia, Hawaii, Michigan, Minnesota, Mississippi, Ohio, Oregon, Virginia and Washington. Conversely, two-thirds of states indicated they do not cover childbirth education in any of their programs (27 of 41 states) and over half indicated they do not cover formal or standalone infant care or parenting education (24 of 41 states). Among the states that reported that they do not cover educational services, some stated that such services are available through other public programs and some reported they provide education as part of prenatal visits. See Appendix Table A3 for details on states’ coverage of childbirth and parenting education.
| Table 6: State Coverage for Childbirth and Parenting Education Services | ||||
| Traditional Medicaid (n=41) |
Medicaid ACA Expansion (n=25) |
Pregnancy Only Medicaid (n=41) |
Not Covered in Any Medicaid Program |
|
| Childbirth Education | 14 | 9 | 14 | 27 |
| Infant care/Parenting education | 17 | 12 | 17 | 24 |
Case Management and Substance Abuse Treatment
| Key Finding: Case Management and Substance Abuse Services |
| Over three quarters of responding states indicated that they cover case management services for pregnant women across all Medicaid eligibility pathways. Nearly all states surveyed reported that they cover substance/alcohol abuse treatment for pregnant women |
Case management can help pregnant women obtain and coordinate services that may be available from multiple providers. Six states do not provide case management in any Medicaid pathway: Connecticut, Hawaii, Maryland, Michigan, New Hampshire, and South Carolina. While the service is not separately billable, Connecticut notes that case management would be covered as part of a hospital admission or through a clinic or office visit. Most of the remaining 35 states provide case management through all eligibility pathways, with exceptions noted in Appendix Table A4.
Case management is often limited to women at higher health risk, or with medical conditions. For instance, Missouri noted that participants must qualify for case management services; Nebraska does not provide the benefit universally, rather it is based on the need of the individual; West Virginia provides the service through its targeted case management program based on medical need. Four states also noted that the case management benefit is provided through managed care or utilization management contracts.
Misuse of alcohol and other substances during pregnancy is correlated with a wide range of negative infant outcomes, including premature birth, fetal alcohol syndrome, and infant drug withdrawal. The ACA requires states to cover counseling services for alcohol misuse for beneficiaries enrolled under the ACA’s Medicaid expansion option.
All states surveyed reported that they cover substance/alcohol abuse treatment for pregnant women in at least one Medicaid eligibility pathway and most states align coverage across pathways (Table 7). New Hampshire is the only state that reported it does not cover substance abuse treatment in its traditional Medicaid pathway. Appendix Table A4 provides detail around state coverage of case management services and substance and alcohol use treatment for pregnant women.
| Table 7: Number of States Covering Counseling and Support Services | |||||
| Traditional Medicaid (n=41) |
ACA Medicaid Expansion (n=25) |
Pregnancy Only (n=41) |
Not Covered in Any Program (n=41) |
Utilization Controls | |
| Case Management | 35 | 19 | 32 | 6 |
|
| Substance/ Alcohol Abuse Treatment | 40 | Required | 38 | ||
Home Visiting Services
| Key Finding: Home Visiting Services |
| Most of the responding states indicated they cover prenatal and postpartum home visits. |
Home visits both during and after pregnancy can help pregnant and postpartum women care for themselves as well as their newborns. Typically conducted by nurses and social workers, they may use the time at home visits to counsel new and expectant parents on a wide range of subjects related to healthy pregnancies and raising healthy children, such as diet and nutrition, basic infant care, breastfeeding, and positive child development. These visits are meant to provide the time for deeper, one-on-one contact and counseling that pregnant women and new parents may not have during routine prenatal and well-baby appointments. Research has found that home visits are associated with a variety of positive outcomes, including lower severity of postpartum depression and improved mother-child interactions.2 Home visits may also cover management of substance abuse, depression, and other chronic conditions. As shown in Table 8, over a quarter of responding states do not provide prenatal home visit supports in any Medicaid program (11 of 41 states). Nearly one fifth (8 of 41 states) do not provide postpartum home visit supports. Of the 30 states that cover both prenatal and postpartum home visits, nearly all provide the service across all eligibility pathways.
Three states provide postpartum home visits but do not provide prenatal home visits through any pathway: Alabama, Maryland and Tennessee. Some states cover prenatal or postpartum home visits under limited circumstances. For example, Michigan notes that the state allows three postpartum home visits only when a physician has determined the mother or newborn to be at risk. Appendix Table A5 details state coverage policies on home visiting services.
| Table 8: Number of States Covering Prenatal and Postpartum Home Visits | |||||
| Traditional Medicaid (n=41) |
ACA Medicaid Expansion (n=25) |
Pregnancy Only (n=41) |
Not Covered in Any Program (n=41) |
Utilization Controls | |
| Home Visit- Prenatal | 30 | 17 | 29 | 11 |
|
| Home Visit- Postpartum | 33 | 19 | 31 | 8 |
|
Delivery and Postpartum Care
| Key Finding: Delivery & Postpartum Care |
| A majority of responding states reported that they cover deliveries in birth centers but only half cover home deliveries. Very few states noted utilization controls for delivery options, and usually restrictions are related to provider requirements. Four states reported covering doula assistance. |
The survey questioned states about the provision of specific delivery services including deliveries at birth centers, home births, doula assistance, and postpartum visits. A doula is a trained non-clinician who assists a woman before, during and/or after childbirth, by providing physical assistance, labor coaching, emotional support, and postpartum care.
Birth center delivery is more likely to be a covered benefit than is home birthing (Table 9). Over three-quarters of responding states (32 of 41) cover deliveries in birth centers compared with about half (21 of 41) covering home births. All states that cover the options within their traditional Medicaid program also provide coverage across all eligibility pathways available within the state. Per the ACA, coverage for deliveries at birth centers is required in all states that license such facilities. There is no comparable requirement for coverage of home births, but in states that have chosen to cover home births, some such as Colorado and Virginia reported that the births must be performed by Certified Nurse Midwives.
All states covered postpartum visits in all eligibility pathways except Oklahoma which does not cover the benefit in its program for pregnant women. Illinois and Texas allow reimbursement for one postpartum procedure per pregnancy. In Texas, the reimbursement covers all postpartum care regardless of the number of visits provided.
Conversely, the only states that cover doula services are Kentucky, Minnesota, Mississippi and Oregon, and they cover the service in all available eligibility pathways.3 Appendix Table A6 presents state coverage of delivery options and postpartum care.
| Table 9: States Covering Delivery Services | ||||
| Traditional Medicaid (n=41) |
ACA Medicaid Expansion (n=25) |
Pregnancy Only Medicaid (n=41) |
Not Covered in Any Program | |
| Birth Centers | 32 | 21 | 32 | 9 |
| Home Births | 21 | 15 | 21 | 20 |
| Doula Services | 4 | 3 | 4 | 37 |
| Postpartum Visit | 41 | 25 | 40 | 0 |
Breastfeeding Services
Raising breastfeeding rates is one of the country’s national Healthy People 2020 goals.4 There is a range of supports that have been found to help women initiate and maintain breastfeeding, including breast pumps, lactation counseling by certified consultants both inpatient and outpatient after delivery, and educational programs, which can begin during pregnancy and continue after the birth of a child. States are required to cover breast pumps and consultation services for Medicaid expansion beneficiaries under the ACA’s preventive services requirement.
Breast Pumps
| Key Finding: Breast Pump Coverage |
| A majority of responding states cover both electric and manual breast pumps, but some report using various utilization controls such as prior authorization or quantity limits. |
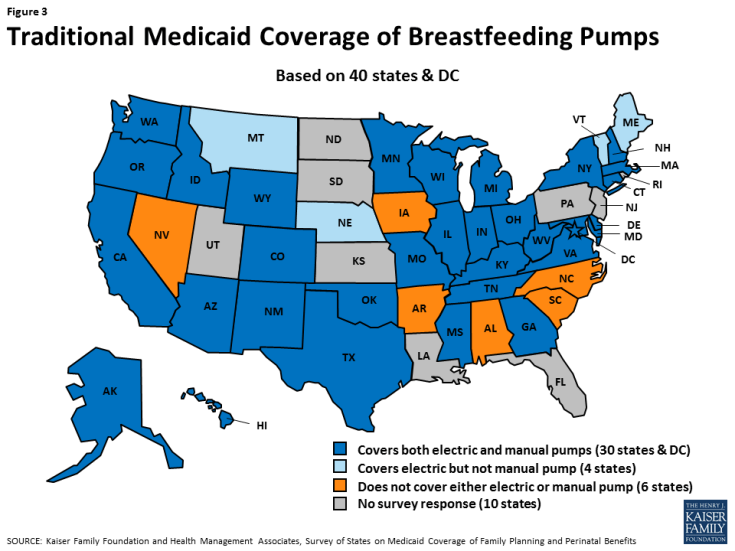
Most responding states report that they cover electric breast pumps (35 of 41 states) and manual pumps (31 of 41 states) in their traditional Medicaid program (Table 10).5 All states that cover pumps in their traditional Medicaid program also cover the benefit in all eligibility pathways except Illinois and Oklahoma, which do not provide the benefit in their program for pregnant women. Six states do not provide either electric or manual pumps under either their traditional Medicaid program or their pregnancy-only eligibility pathway: Alabama, Arkansas, Iowa, North Carolina, Nevada, and South Carolina (Figure 3).6
| Table 10: Breastfeeding Supplies | |||
| Traditional Medicaid (n=41) |
Pregnancy Only Medicaid (n=41) |
Not Covered in Any Pathway (n=41) |
|
| Electric Breast Pump | 35 | 33 | 6 |
| Manual Breast Pump | 31 | 29 | 10 |
| *While coverage of breast pumps is required for all ACA Medicaid expansion enrollees, coverage detail regarding the type of pump covered was not reported by Arkansas, Iowa or Nevada. | |||
Breast Pump Utilization Controls
Several states reported utilization controls for breast pumps. As shown in Table 11, prior authorization is the most frequently employed utilization control, followed by quantity/time limits. Some states noted multiple utilization policies. For instance, Colorado requires prior authorization for electric pumps. The state allows rental or purchase of a breast pump based on the situation of the infant or mother. The state covers rental of an electric pump when the infant is expected to be hospitalized for less than 54 days, but allows breast pump purchase for hospital stays expected to last longer than this.
For quantity/time limits, Massachusetts limits the purchase of either an electric pump or manual to one per member every five years. Ohio limits electric pumps to one every five years, and a manual pump to one every 24 months but did not specify rental or purchase requirements. Texas limits the purchase of an electric or manual breast pump to one every three years, but does not time-limit the rental of a hospital grade pump. Appendix Table A7 provides policy detail around state Medicaid coverage for breast pumps.
| Table 11: Utilization Controls Applied to Breast Pump Benefit | |
| Utilization Control | States with Utilization Policy |
| Prior Authorization (7) | CO, MA*, MI*, MO, MT, OH*, WA |
| Limited to mothers with critical care/NICU infants (3) | CO, MI, TN |
| Quantity/time limits (4) | MA, MI, OH, TX, |
| Conditions determine rental or purchase (3) | CO, MI, TX* |
| Limited to rental (2) | Rental: MT, WA |
| *MI: Prior authorization is not required when standards of care are met. It is required for rental beyond 3 months. MA and OH: Prior authorization required to exceed quantity limit. TX: Purchase of a breast pump is limited to one per three years. Rental is not time-limited. |
|
Breastfeeding Education and Lactation Consultation
| Key Finding: Breastfeeding Education and Lactation Consultation |
| Most responding states reported that breastfeeding education and hospital-based lactation consulting services are covered under traditional Medicaid, but most states do not provide lactation consultation in settings other than a hospital. |
The survey asked about coverage for breastfeeding education such as classes and about coverage for lactation consultation in the hospital, clinic/outpatient, and home settings. There is more variation across the states in the coverage of breastfeeding education and consultation than for breast pumps. As shown in Table 12, 27 of 41 responding states cover breastfeeding education under traditional Medicaid. Individual lactation consultant services are most likely to be covered in the hospital setting. Nearly two-thirds of states responding to the survey stated they cover services in the hospital compared with a little over one-third of responding states providing the service in an outpatient/clinic setting, and less than a quarter of states providing the benefit for postpartum women in their homes.
States did not report utilization controls for breastfeeding support services but a few states noted provider requirements. For example, Connecticut allows the services in hospital and clinic settings if provided by any of these licensed provider types: Physician, DO, Physician Assistant, Advanced Practice Registered Nurse (APRN), or Certified Nurse Midwife (CNM), and is a component of the hospital or clinic reimbursed services. In New York, qualified practitioners for Medicaid reimbursable lactation counseling must be state licensed, registered, or certified health care professionals who are International Board Certified Lactation Consultants (IBCLCs) credentialed by the International Board of Lactation Consultant Examiners (IBLCE) and one of the following: Physician, Nurse Practitioner, Midwife, Physician Assistant, Registered Nurse.
| Table 12: State Coverage for Breastfeeding Support Services | ||||
| Traditional Medicaid (n=41) |
ACA Medicaid Expansion (n=25) |
Pregnancy-Only Medicaid (n=41) |
Not Covered in Any Program (n=41) |
|
| Breastfeeding Education | 27 | 15 | 26 | 14 |
| Individual Lactation Consultation | ||||
|
26 | 16 | 25 | 15 |
|
16 | 12 | 15 | 25 |
|
11 | 10 | 11 | 30 |
Alignment Across Eligibility Pathways and Reimbursement Mechanisms
In the 27 states that cover breastfeeding education in their traditional Medicaid program, coverage is aligned across the three Medicaid eligibility pathways, except in Nevada, which provides the service under traditional Medicaid, but not through the ACA Medicaid expansion or through the state’s program for pregnant women.
However, there is more variation between eligibility pathways for coverage of lactation consultation. Of the 26 states that cover individual lactation services, only 11 cover hospital-based, outpatient, and home consultations services in all of the eligibility pathways available in the state: Arkansas, California, Connecticut, District of Columbia, Delaware, Hawaii, Minnesota, Mississippi, New York, Ohio, and Oregon. All of the 26 states cover inpatient consultation in all of their pathways, with the exception of Oklahoma in the pregnancy only pathway.
Many states reported that reimbursement for lactation consultation is not a separately reimbursable service but is included as a component of other services provided (Table 13), most frequently as a component of hospital reimbursement (11 states). For example, Connecticut noted that the service is not a separately billable service but it is covered as part of a clinic/office visit or hospital stay.
| Table 13: Reimbursement Methodologies for Lactation Consultant Services | ||
| Included in Hospital DRG or Global Fee (10) | Included in Outpatient Clinic Visit (3) | Included in Home Visit (2) |
|
|
|
| * Colorado provides the service as a part of problem specific care, or a special program service such as the Nurse Home Visitor Program but not separately reimbursable. | ||
Appendix Table A8 reports coverage policies for breastfeeding education services across the states. Appendix Table A9 presents information on states’ coverage of lactation consultation and Appendix Table A10 compares coverage within states between eligibility pathways.
Conclusion
The survey of state responses found that in 2015, most states cover a broad range of perinatal services in their full scope traditional Medicaid program, under full scope ACA Medicaid expansion, and pregnancy-related eligibility pathways. Most of the 41 surveyed states report that they cover basic prenatal services such as ultrasounds and vitamins, prenatal genetic testing, home visits, delivery in birth centers, postpartum visits, and breast pumps for nursing mothers. Coverage for services that help women and their families care for their children after delivery, such as childbirth and parenting classes, breastfeeding education and lactation consultation is less common. In particular, very few states cover doula supports despite research suggesting that this assistance results in better health outcomes.1 While coverage requirements differ between eligibility pathways in some cases, for the most part, there is strong alignment within states for the various pathways.
Maternity care is typically reimbursed with a global fee that covers all care for pregnant women through the postpartum period. Some states reported that support services, such as childbirth and breastfeeding education are included in the global fee and are not reimbursed separately. In these cases, the structure of the benefit is not clear, particularly who would provide these services and the scope of services available to beneficiaries.
Medicaid enrollment across the country has risen significantly since the ACA’s passage but in states that have not expanded eligibility under the ACA, many women lose coverage after 60 days postpartum and become uninsured. Furthermore, it is important to recognize the ACA’s role in establishing a floor of benefits for pregnant women enrolled in the program in expansion states. The ACA’s requirement that newly eligible beneficiaries are covered for federally recommended preventive services means that pregnant women on the program in expansion states are guaranteed coverage for folic acid supplements, breast pumps, and several screening tests. Many states have structured their programs so all pregnant women on Medicaid are covered for their services regardless of the eligibility pathway that qualifies them for coverage.
The Medicaid program has a long history and excellent record of providing coverage for low-income pregnant women, with almost half of the nation’s birth covered under the program. Regardless of the outcome of current debates over the future of Medicaid or the ACA, the millions of low-income pregnant women that are served by Medicaid will continue to need to have access to coverage that includes the broad range of pregnancy-related services that help assure healthy maternal and infant outcomes.
Acknowledgements
The authors express appreciation for the assistance of several individuals who assisted with the preparation, testing, and refinement of the survey instrument, including Yali Bair of Ursa Consulting, Amy Moy from the California Family Health Council, Tasmeen Weik of the federal Office of Population Affairs, Melanie Reece of Colorado’s Department of Health Care Policy and Financing, and Lisa DiLernia of Michigan’s Department of Health and Human Services.
We thank the following colleagues from Health Management Associates: Joan Henneberry for guidance and subject matter expertise; Dennis Roberts for database development and management; and Nicole McMahon for assistance with compiling the state data tables.
We also thank the Medicaid directors and staff in the 40 states and the District of Columbia who completed the survey on which this brief is based.
Appendices
Appendix A: State-Level Survey Results (.pdf)
Appendix B: Methodology (.pdf)
Appendix C: Perinatal Services Questionnaire (.pdf)
Endnotes
Executive Summary
Kaiser Family Foundation; Births Financed by Medicaid
Kaiser Family Foundation; Status of State Action on the Medicaid Expansion Decision.
The American Congress of Obstetricians and Gynecologists. Safe Prevention of the Primary Cesarean Delivery. March 2014.
Introduction
Markus AR, Andres E, West KD, Garro N, Pellegrini C. Medicaid Covered Births, 2008 Through 2010, in the Context of the Implementation of Health Reform. Women’s Health Issues. Sept-Oct 2013
Kaiser Family Foundation; Status of State Action on the Medicaid Expansion Decision; As of January 12, 2016; Since July 1, 2015 Alaska implemented a Medicaid expansion (9/1/2015) as did Montana (1/1/2016) and Louisiana (7/1/2016).
Kaiser Family Foundation. Women’s Health Insurance Coverage. October 2016.
Report
Survey Results
Healthy People 2020. Maternal, Infant, and Child Health. Office of Disease Prevention and Health Promotion.
Horowitz JA, Murphy CA, Gregory K, Wojcik J, Pulcini J, & Solon L. (2013). Nurse Home Visits Improve Maternal-Infant Interaction and Decrease Severity of Postpartum Depression. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 42(3), pp 287-300.
New Mexico reported that some managed care entities provide Doula services but it is not a Medicaid covered benefit. Ohio noted that there are no certified Doulas in the state currently.
Healthy People 2020: Breastfeeding Objectives.
Virginia reported that both electric and manual pumps are covered as a benefit through managed care. Fee-for-service coverage was added effective 1/1/2016.
Alabama notes that breast pumps are provided through the WIC program and through the Alabama Department of Public Health. South Carolina also noted provision through its Health Department.
Conclusion
The American Congress of Obstetricians and Gynecologists. Safe Prevention of the Primary Cesarean Delivery. March 2014.