Serious Illness in Late Life: The Public’s Views and Experiences
Section 2: Experience of Older Adults with Serious Illness
In order to better understand how older people with serious illness are faring and what challenges they face in accessing and affording care and support services, the survey included interviews with people who have experience with serious illness, either personally or with a family member.
Individuals were classified as being an older adult with serious illness if they met each of the following criteria:
- they were 65 or older,
- they reported functional limitations due to a health or memory problem such as difficulty preparing meals, shopping for groceries, taking medications, getting across a room, eating, dressing, bathing, or using the toilet,
- they said they have been diagnosed with at least one of the following conditions: diabetes or high blood sugar; asthma, lung disease, emphysema, or COPD; heart disease or had a stroke; cancer, not including skin cancer; Alzheimer’s disease, dementia or memory loss; depression, anxiety or other serious mental health problems; or, chronic kidney disease or kidney failure.
Individuals qualified as a family member of someone with serious illness if their loved one currently met the criteria above or they did so before they recently died. In order to be included, family members also must have said they knew at least something about their family member’s medical care. About 11 percent in the “serious illness experience” group for this survey are themselves dealing with serious illness, 52 percent are family members of someone living with a serious illness, and 37 percent are family members of someone who has died after a period of serious illness. For most family members, their loved one with serious illness is a parent (56 percent), while 21 percent say the person is a grandparent, 9 percent say it is their spouse, and 7 percent say it is an in-law.
Profile of Older Adults with Serious Illness
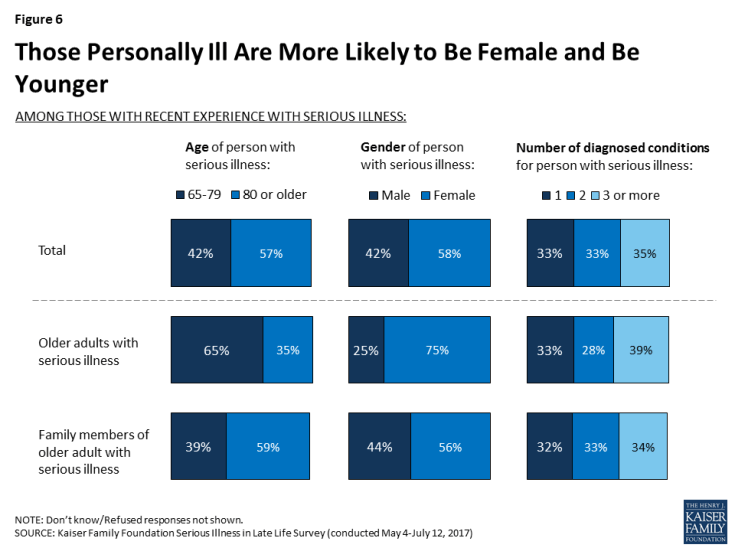
Among those identified in this survey as older adults with serious illness, 58 percent are women, 57 percent are age 80 or older, and two-thirds (67 percent) report having two or more chronic conditions. However, there are some differences in the personal characteristics of those who are personally dealing with serious illness and those whose family member is answering on their behalf.1 For example, while by the definition used in the survey, all older adults with serious illness are (or were) 65 or older, those answering about themselves tend to be younger (65 percent are 65 to 79), while family members’ seriously ill loved ones are usually older (59 percent are 80 or older). In addition, a bigger majority of those answering about themselves are women (75 percent) than family members’ loved ones (56 percent).
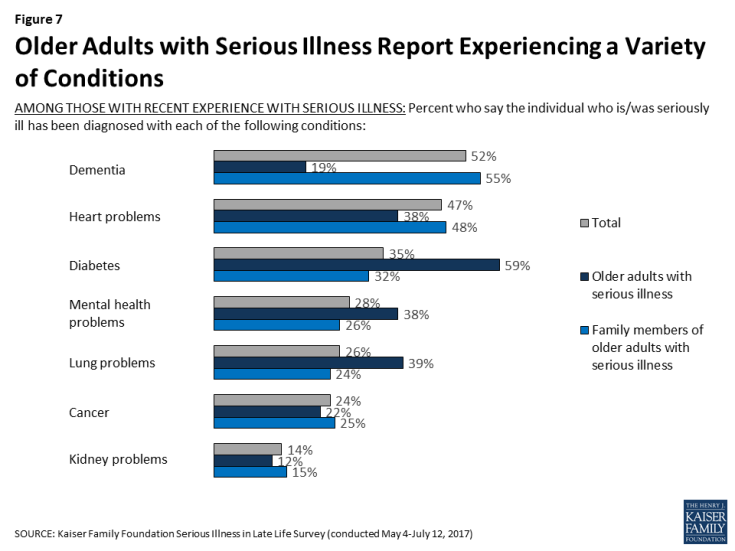
While this survey’s definition of serious illness includes several different conditions, some are more common than others, and reports of these conditions vary by whether someone is personally dealing with serious illness themselves or if they’re responding about a family member. Overall, 52 percent report they or their loved one has been diagnosed with dementia, Alzheimer’s disease, or memory loss, 47 percent report being diagnosed with heart disease or having a stroke, followed by diabetes (35 percent), mental health problems such as anxiety or depression (28 percent), asthma, lung disease, emphysema, or COPD (26 percent), cancer (24 percent), and chronic kidney disease or kidney failure (14 percent). Those responding about their own experience as an older adult with serious illness are more likely to say they have been diagnosed with diabetes (59 percent), while 55 percent of family members of older adults with serious illness say their loved one has dementia and half (48 percent) say their loved one has heart disease. Some of these differences are at least in part related to the group of seriously ill people that were able to be interviewed, in that they had to be well enough to answer the telephone and not be institutionalized. As a result, the group of older adults who themselves are dealing with serious illness tends to be a group in somewhat better health or potentially at an earlier stage of illness than those with a family member answering on their behalf.
How Older Adults with Serious Illness Compare to Others 65 or Older
There are also some key differences in the personal characteristics of those 65 or older who are seriously ill and those who are 65 who are not classified as seriously ill. Older people with serious illness are much more likely than their peers to be female (75 percent versus 53 percent), widowed (42 percent versus 24 percent), have an annual income of less than $40,000 (64 percent versus 38 percent), and have a high school education or less (71 percent versus 40 percent). They are also somewhat more likely than their peers to be Black (18 percent versus 9 percent) or Hispanic (12 percent versus 5 percent).
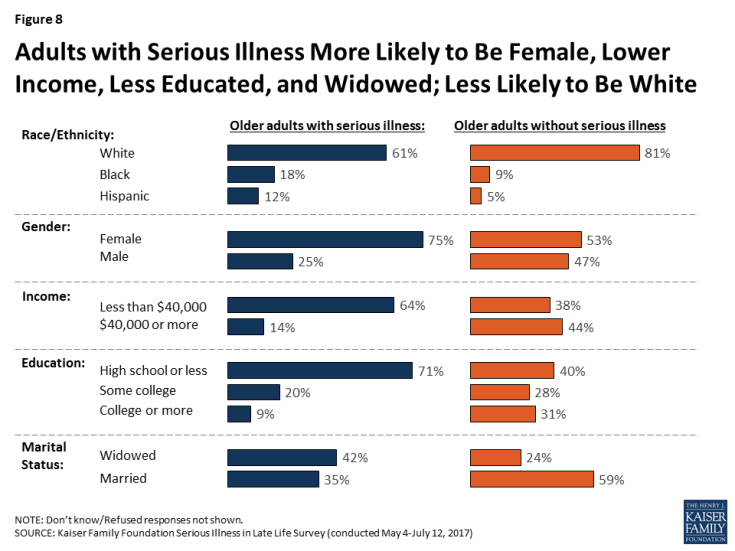
Figure 8: Adults with Serious Illness More Likely to Be Female, Lower Income, Less Educated, and Widowed; Less Likely to Be White
Utilization of Medical Services Among Older Adults with Serious Illness
Among older adults and family members of older adults with serious illness, about two-thirds (64 percent) report that they went to the emergency room in the past year (or in the year before they died for those with a deceased family member), including 10 percent who say they went more than five times. In addition, about six in ten (58 percent) say that the seriously ill person stayed overnight in the hospital in the past year, or in the year before they died. Those whose loved one is deceased are more likely than others to say they had gone to the emergency room (75 percent) or stayed in the hospital overnight in the year before they died (78 percent).
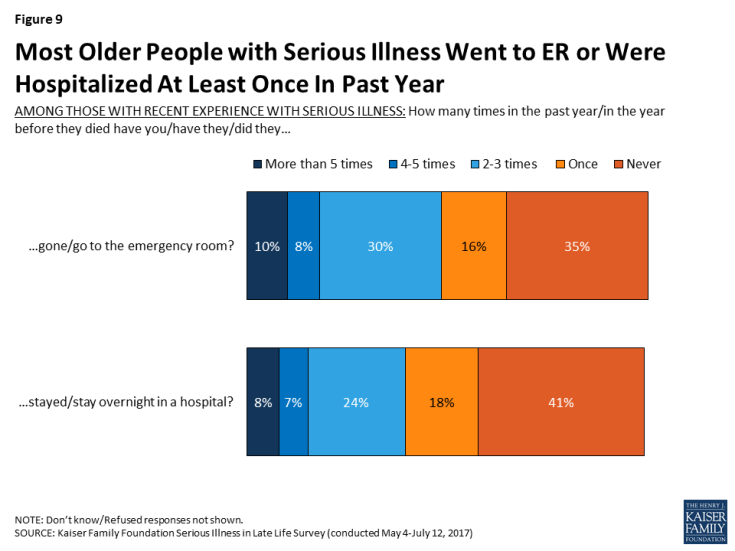
Figure 9: Most Older People with Serious Illness Went to ER or Were Hospitalized At Least Once In Past Year
Among those family members whose loved one is deceased, 61 percent say their loved one had some experience with hospice in the year before they died. Family members most commonly say their loved one had hospice care at home (27 percent), followed by in a nursing home (17 percent), in a hospice facility (9 percent), and in a hospital (6 percent).
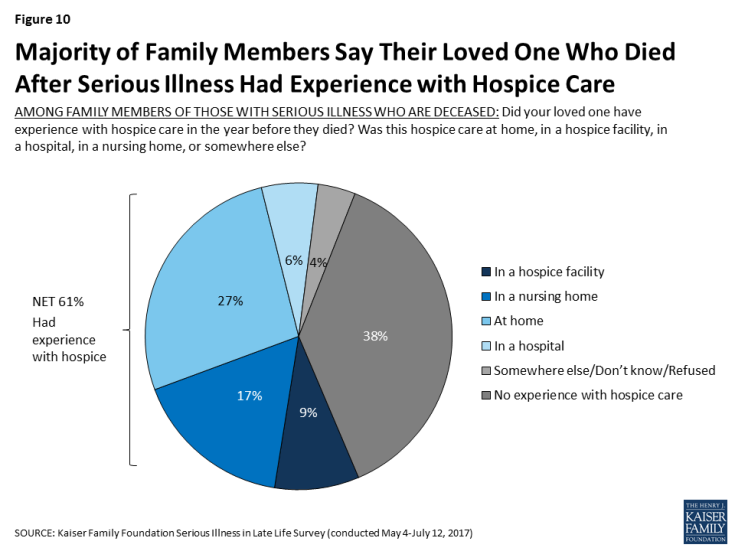
Figure 10: Majority of Family Members Say Their Loved One Who Died After Serious Illness Had Experience with Hospice Care
Problems Faced by Older Adults with Serious Illness
People with serious health needs can face a variety of challenges, ranging from difficulty managing daily tasks independently to having trouble affording medical care and support services. Nearly half (48 percent) of individuals and family members of older adults with serious illness say that in the past year they had a problem understanding instructions for medications and medical care. Those ages 80 or older (53 percent) are more likely than those between 65 and 79 to say they had problems understanding medical instructions (41 percent). In addition, reports of trouble understanding instructions for medical care and medications are about twice as common for those with dementia than for those without (64 percent versus 30 percent).
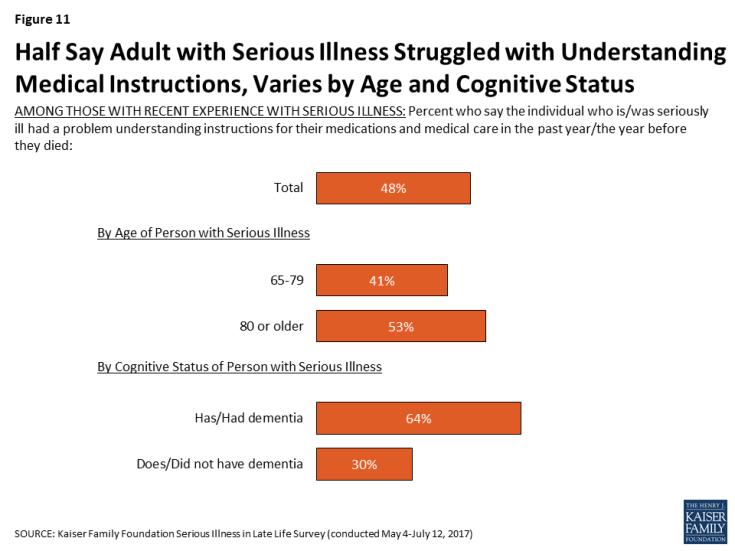
Figure 11: Half Say Adult with Serious Illness Struggled with Understanding Medical Instructions, Varies by Age and Cognitive Status
Focus Group Insights: Family members of those with serious illness noted that managing medications is often a challenge. People expressed concern about the number of medications their loved ones were taking as well as the medications that are needed to treat side effects of other medications, and the side-effects in general.
“It took me an hour and a half after mom got out of the hospital, just to do two weeks of morning and evening pills. … She was already on a lot of medications. Just sorting it all out, it was crazy.”
Older adults with serious illness report other problems as well. About four in ten (39 percent) say they or their family member with serious illness had trouble preparing meals in the past year, 30 percent say they had trouble getting to appointments because of their health, 24 percent say they had trouble getting transportation or running errands, and 20 percent say they had trouble finding someone to provide support services.
In addition, being able to afford the things they need is an issue for some. About one in five say they have trouble paying for support services (20 percent), medications (20 percent), and medical tests or treatments (17 percent). Relatively few say they have had trouble paying for housing (12 percent). Those with lower incomes (less than $40,000 annually) are more likely than those earning $40,000 or more to say that they or their family member had trouble paying for medications (33 percent versus 13 percent), medical treatments (27 percent versus 11 percent), and housing (16 percent versus 9 percent).
It is important to note that while Medicare covers the basic medical care that older people require, it does not typically pay for long-term care and support services that people with serious illness may need. As a result, many must pay for these types of services out-of-pocket, with the exception of those with incomes low enough to qualify for Medicaid. In light of this, it may be surprising that problems paying for medical care and problems paying for support services rank similarly. However, this may be at least in part because the question asks about those who have had difficulty paying for care and does not reflect those who may not have tried to get this type of help because they felt they couldn’t afford it.
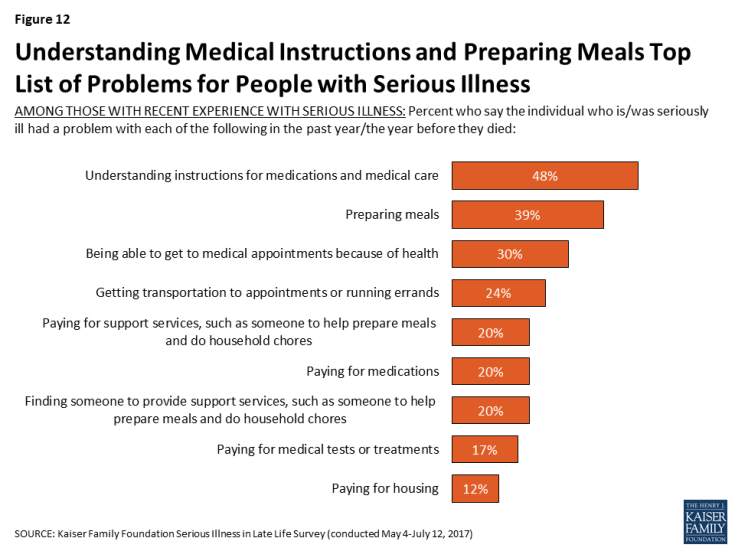
Figure 12: Understanding Medical Instructions and Preparing Meals Top List of Problems for People with Serious Illness
In addition to issues paying for support services, medications, medical treatments or housing, about three in ten family members of those currently living with serious illness are not confident that their loved one will have enough income and assets to last for the rest of their life, while a majority are at least somewhat confident (71 percent).
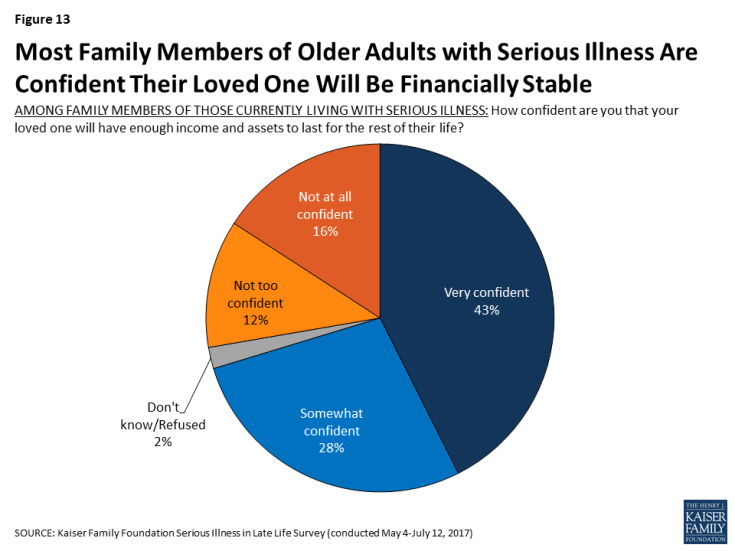
Figure 13: Most Family Members of Older Adults with Serious Illness Are Confident Their Loved One Will Be Financially Stable
Problems with Mood or Cognition
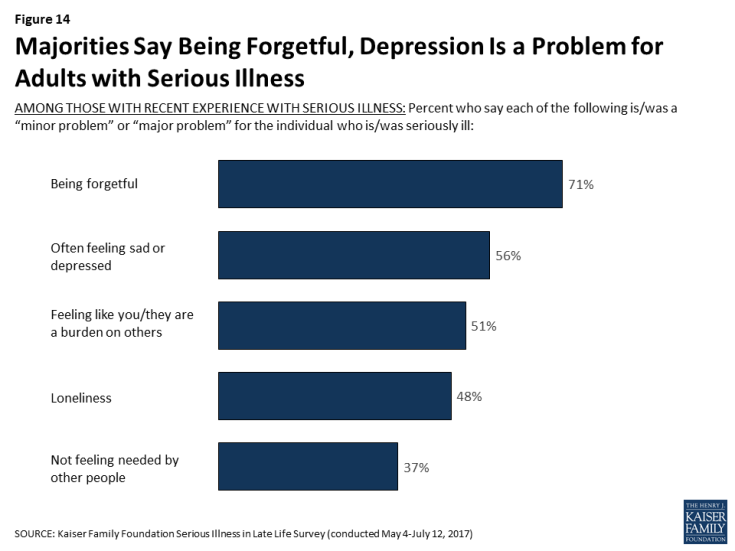
Many older adults with serious illness and their family members report issues with memory – seven in ten say being forgetful is at least a minor problem, including nearly half who say it is a major problem. Many also report issues with mood such as often feeling sad or depressed (56 percent), feeling like a burden on others (51 percent), and loneliness (48 percent), which can have a negative impact on health. Fewer, 37 percent, report that not feeling needed by other people is a problem.
Assistance For Older Adults with Serious Illness
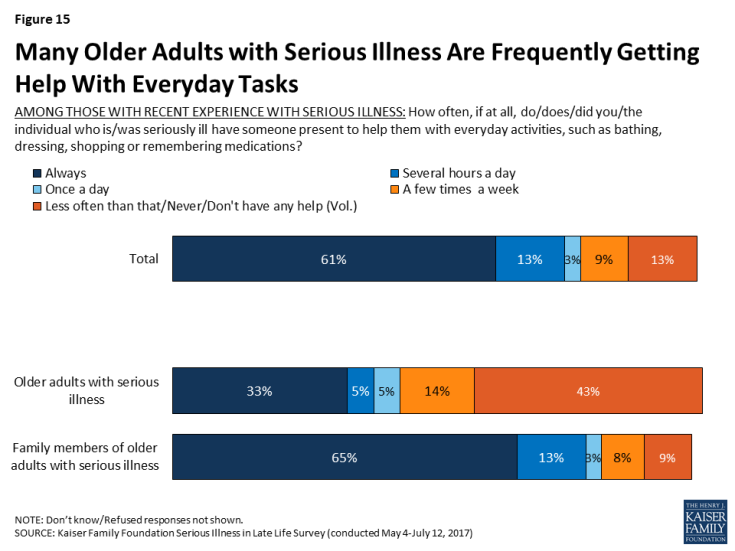
Many older adults who are seriously ill report getting frequent help. Six in ten (61 percent) say they or their loved one always has someone present to help them with everyday activities like dressing, bathing, shopping, or remembering medications, and an additional 13 percent say they have someone present several hours a day.
There are big differences for those responding to the survey who are dealing with serious illness themselves – 33 percent say they always have someone present to help, but 16 percent say they never do and 27 percent say they have help less than a few times a week. In contrast, the majority of those with family members with serious illness say their loved one always has someone present to help (65 percent). As noted earlier, this is likely related to the fact that those answering about themselves are relatively younger and in somewhat better health than the loved ones family members are referring to.
Slightly over half feel they or their family member are getting help with daily activities often enough, but over four in ten feel like they need help more often than they are getting. Those getting care just a few times a week or less are more likely than others to say they need help more often (59 percent versus 40 percent).
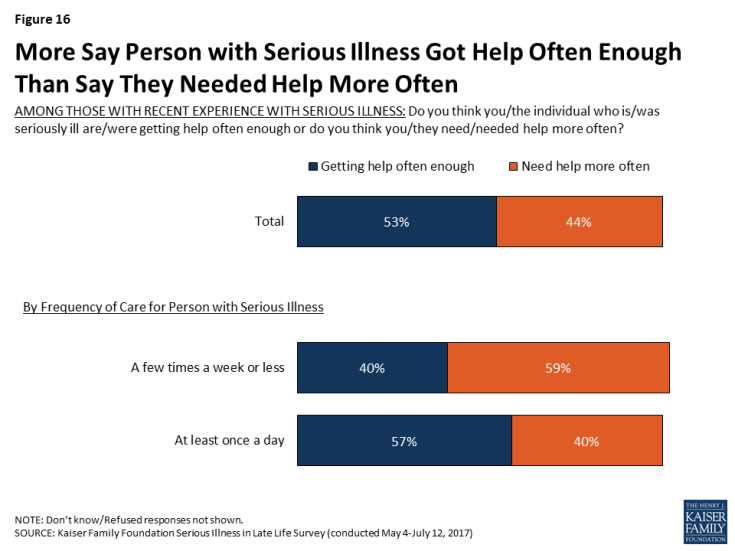
Figure 16: More Say Person with Serious Illness Got Help Often Enough Than Say They Needed Help More Often
While most (71 percent) say it is easy to get the help needed with everyday activities, about a quarter (27 percent) say it is either somewhat (19 percent) or very difficult (8 percent) to get the help needed. In addition, about one-fifth of those with experience with an older adult with serious illness (18 percent) say that in the past year, there was a time they did not get the help they needed with everyday activities because of the cost.
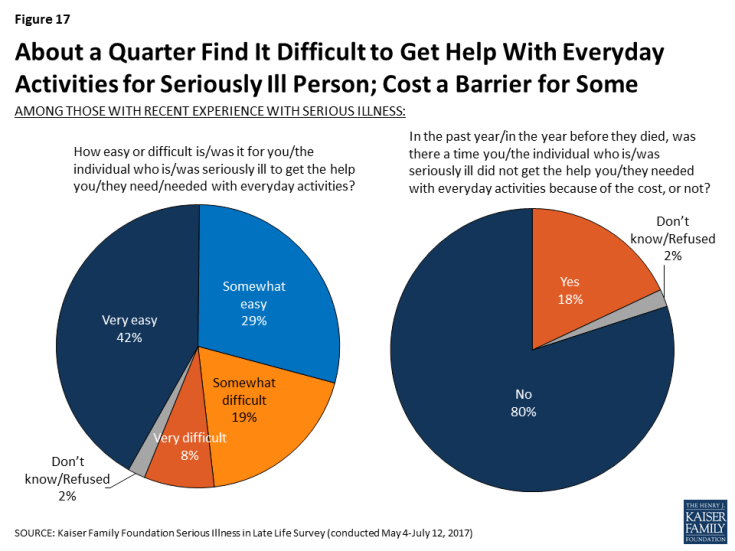
Figure 17: About a Quarter Find It Difficult to Get Help With Everyday Activities for Seriously Ill Person; Cost a Barrier for Some
Focus Group Insights: Family members of those with serious illness reported non-medical help – for example, providing companionship, household chores, and errands – is crucial but often difficult to find and afford.
“I’m going to be looking for some help coming up in the next three or four weeks. I’m really not sure which direction to go…I’m going to try and find some people that know what they’re doing and will be there for you.”
Who is Providing Help?
Family members are a primary source of help with everyday activities for older people with serious illness – 84 percent report that the older adult with serious illness receives help from a family member. Over half of older adults who themselves are dealing with serious illness (56 percent) say a family member helps them with everyday activities. In addition, 57 percent of family members say they personally help their loved one with daily activities, but a large majority (73 percent) also say that another family member provides help, including 79 percent of those family members who do not personally provide care. Professional caregivers are also a key source of help for those with serious illness, with over half (55 percent) saying paid nurses or health care aides help with everyday activities. In addition, a quarter say that friends are helping with daily activities (25 percent).
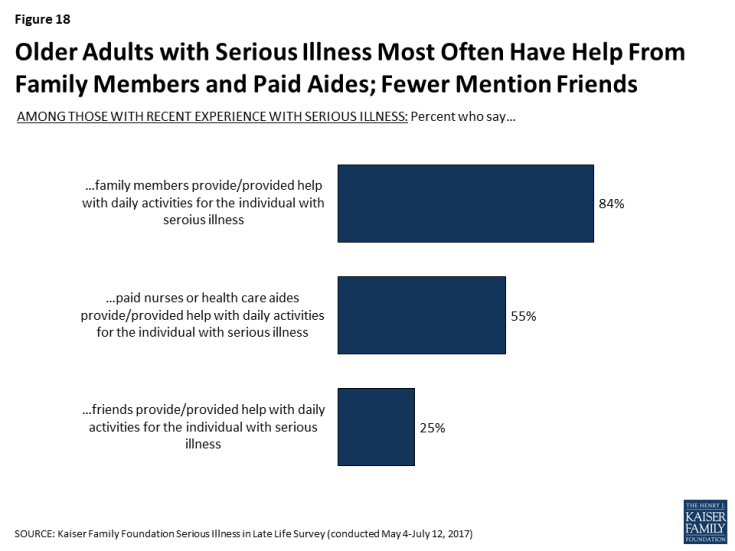
Figure 18: Older Adults with Serious Illness Most Often Have Help From Family Members and Paid Aides; Fewer Mention Friends
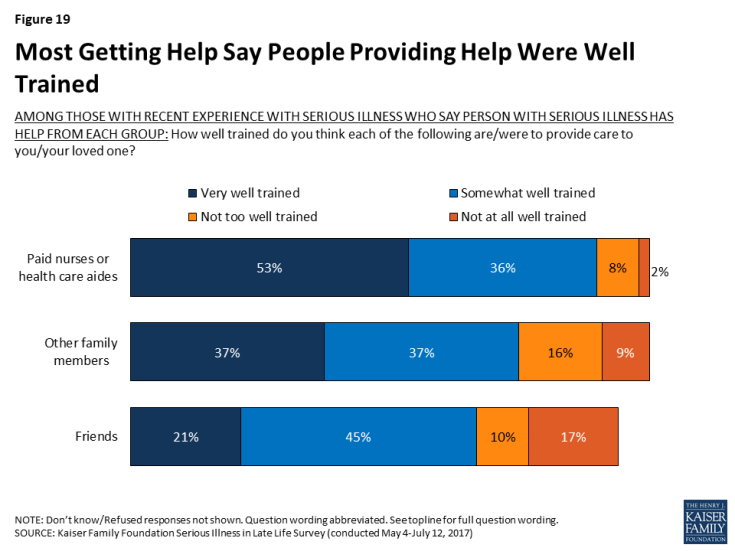
Most of those getting paid help say the nurse or health care aide is well trained (89 percent) and rate the quality of the care provided as very good or excellent (63 percent), however a few report being less satisfied with the help, including 10 percent who say the people helping them were not well trained and 12 percent who rate the care as fair or poor. Family members who report that other family members play a role in providing help most often say that the other family members were well trained (74 percent), and most getting help from friends feel they were well trained as well (66 percent).
Family Members Personally Providing Care
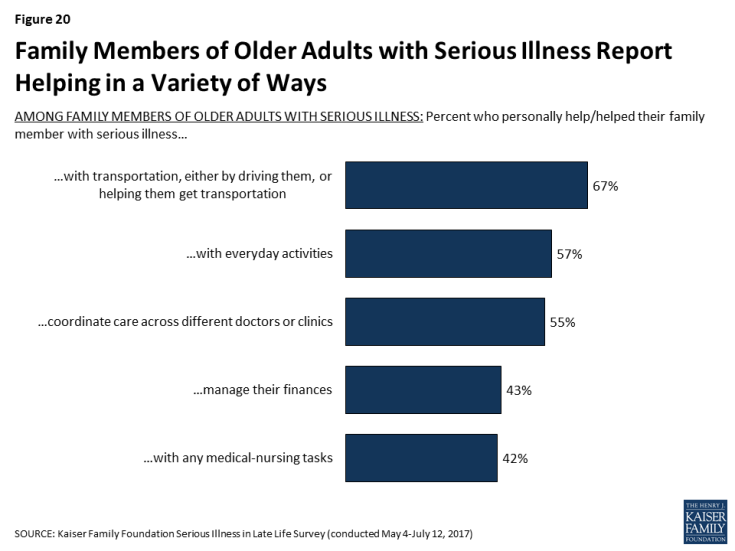
Family members of older adults with serious illness report helping with a variety of tasks. Most commonly, family members report helping their loved one with transportation (67 percent), but, as noted above, nearly six in ten also say they help with daily activities (57 percent), and over half say they help with coordinating care across different doctors or clinics (55 percent). In addition, about four in ten say they help with managing their loved one’s finances (43 percent) or with medical-nursing tasks, including things like giving medicines, monitoring blood pressure or blood sugar, helping with incontinence, or operating equipment like hospital beds (42 percent).
About half of family members who provide some type of assistance say they are doing so several hours a day or constantly, while 24 percent say a few hours a week and 13 percent say less often than that. Most of those providing help with daily activities said there was someone that could provide respite (79 percent), but 21 percent of family members, including 24 percent of family members who are providing care for at least an hour a day say that there is no one that can give them a break from caring for their loved one.
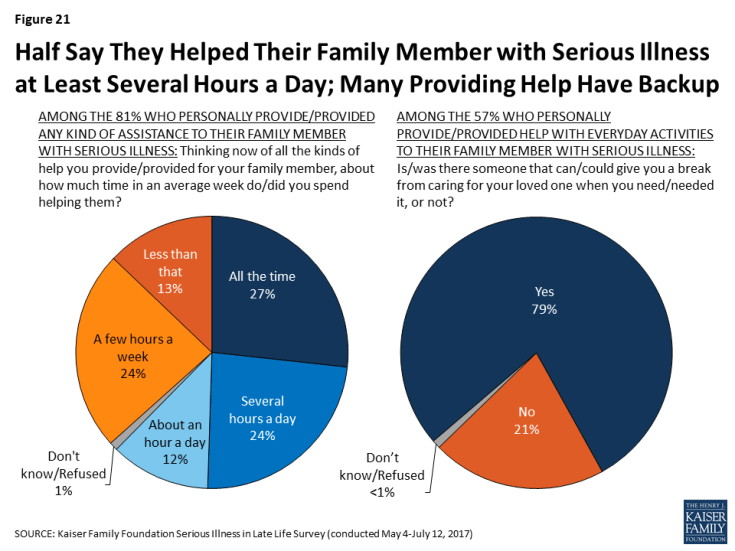
Figure 21: Half Say They Helped Their Family Member with Serious Illness at Least Several Hours a Day; Many Providing Help Have Backup
Focus Group Insights: Caregivers are faced with making difficult decisions about how much time they should devote to caring for a loved one. Those who care-give full-time make substantial sacrifices.
“Yeah, I watched 18 years go by when I quit working. I was there all the time. If I went out, somebody had to be there with her, so no. I kind of gave up my life for a while.”
******
Having support and relief for caregivers is key, as it’s both physically and emotionally taxing.
“We have to take care of ourselves because if we don’t they’re not going to have anybody to take care of them. I was to the point where I was about ready to split. I was tired and wasn’t thinking right. I started asking people, ‘Could you come and stay? Let me just get out for a little while.’ That’s happened. It’s a lot better. Your brain gets a little crazy when you’re tired.”
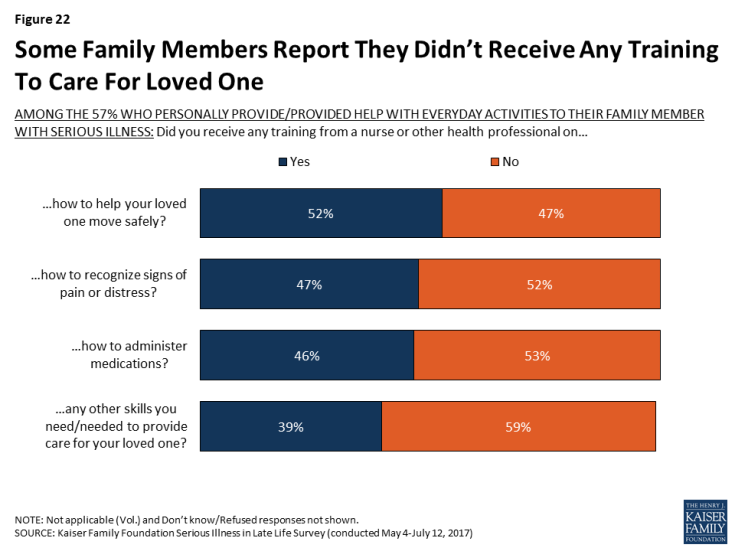
In terms of the specific types of training that family members received from a nurse of other health professional, significant shares of those providing help with daily activities say they received training on how to move their loved one safely (52 percent), how to recognize signs of pain or distress (47 percent), and how to administer medications (46 percent). Still, about half say they did not receive training in each of these areas, and 31 percent say they did not receive any of these types of training.
A large majority (82 percent) of family members who report personally helping their loved one with everyday activities feel they were at least somewhat well trained to provide care, but about one in five feel they were not well trained (18 percent). Family members who report getting at least one of these types of training from a nurse or health professional are more likely than others to say they feel they were well trained to provide care to their loved one (91 percent versus 62 percent). During focus groups with family members of those with serious illness, some said they learned how to care for their loved one independently, from family members, or through online resources, which may in part explain why more family members feel well trained than say they received training from a nurse or health professional.
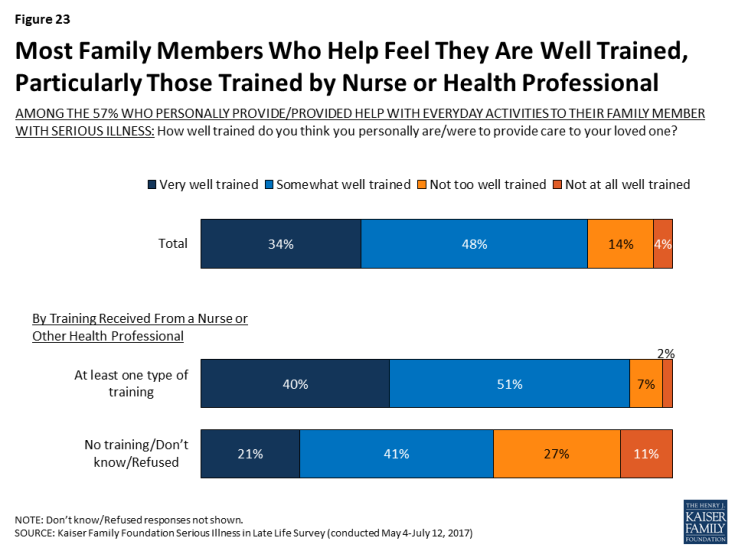
Figure 23: Most Family Members Who Help Feel They Are Well Trained, Particularly Those Trained by Nurse or Health Professional
Those providing medical-nursing types of care are much more likely than family members who are not doing medical-nursing tasks but are providing help more generally to say they received training from professionals. For example, over half of family members who report helping with nursing tasks say they received training from a nurse or another health professional on how to help their loved one move safely (58 percent) and how to administer medications (54 percent), shares that are much higher than for family members who help with daily activities but who aren’t providing nursing care (33 percent and 24 percent, respectively). The vast majority of family members helping their loved one with nursing tasks feel they were well-trained (89 percent), including 41 percent who say they were ‘very’ well trained.
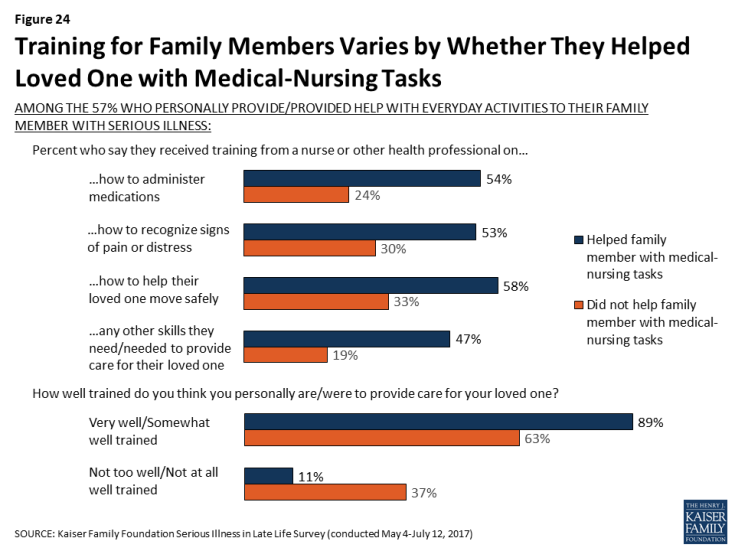
Figure 24: Training for Family Members Varies by Whether They Helped Loved One with Medical-Nursing Tasks
Focus Group Insights: Some suggested classes for family members that provided information on a person’s illness and prognosis or basic caregiving training.
“The one thing I would say, for my family members, I was able to show them how to wash hair, how to change the bed with the person in it, those things. But it would have been so helpful if the hospital, community center, anybody, had offered some basic classes.”
“I had to learn for myself. It’s the best way to do that from my end. I have sisters and brothers that help me with the medications, set it up and all that stuff but just to be hands on and do it myself and learn it, watch different videos on it and just research myself.”
Seriously ill person’s needs being met
While many say that the person with serious illness could use help more often than they’re getting, large shares report that their or their seriously ill family member’s needs are often or always being met in specific areas, particularly in regard to help understanding their health condition and treatment (73 percent), coordinating care across different doctors or clinics (73 percent), being able to continue living where they want to be living (71 percent), expressing their wishes for medical care (71 percent), relieving pain (69 percent), and getting what they want out of life while sick (61 percent). In addition, just over half say they or their loved one often or always gets the help they need with spiritual support or counseling and to manage feelings of anxiety or sadness. However, there are some who say their needs are just sometimes, rarely, or never met, most often in help to manage feelings of anxiety or sadness (40 percent), in spiritual support or counseling (37 percent), and in getting what they want out of life while sick (34 percent).
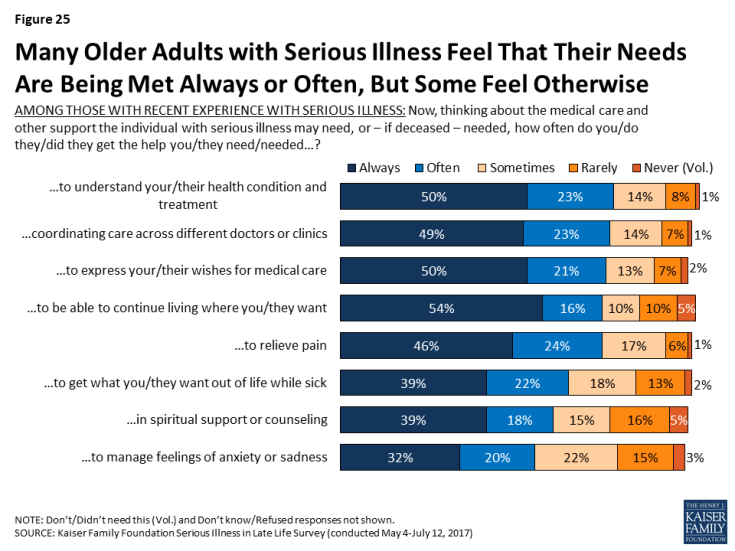
Figure 25: Many Older Adults with Serious Illness Feel That Their Needs Are Being Met Always or Often, But Some Feel Otherwise
Focus Group Insights: Aspects of care that family members of seriously ill people said were challenging included things like coordinating care across many different providers and getting treatment information from providers.
“Trying to get in touch with your primary care is like trying to get in touch with the president, you can’t.”
Family Members’ Needs Being Met
While seriously ill people themselves have many needs that must be met, family caregivers are also often in need of emotional and logistical support. Most of those who are family members of an older person with serious illness say they often or always get the help they need understanding their loved one’s condition and with coordinating care across different clinics and providers. However, like people with serious illness themselves, the areas where more family members are less often getting the care they need is with spiritual support and managing feelings of anxiety or sadness, with about four in ten saying their personal needs in these areas were just sometimes, rarely, or never met (40 percent and 45 percent respectively). These findings hold true for those personally providing help at least an hour a day (43 percent and 48 percent, respectively).
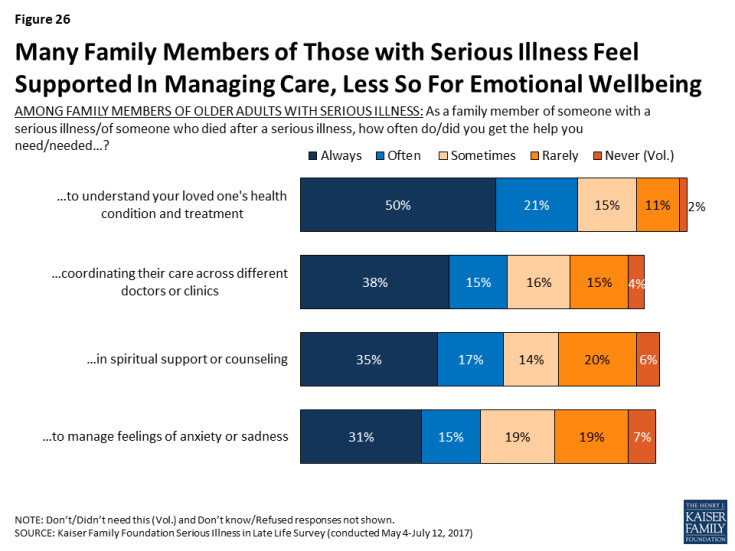
Figure 26: Many Family Members of Those with Serious Illness Feel Supported In Managing Care, Less So For Emotional Wellbeing
Focus Group Insights: Because of challenges with care coordination, some family members of those with serious illness felt the level of care was dependent on a family’s ability to advocate and be there for their loved one.
“You really have to be aggressive and keep up with every single thing when you’re in the hospital. Because they will fall through the cracks.”
******
Many family members of those with serious illness mentioned efforts to research conditions on the internet and feeling like they needed more ‘big picture’ information from medical providers about the course of illness and what they could expect down the line.
“I don’t know if they assume that you know what all is going to happen to you when you have chemotherapy and cancer, and they don’t walk you through it, or if that’s just common not to be taught what to expect.”