Medicaid Initiatives to Improve Maternal and Infant Health and Address Racial Disparities
Introduction
Despite continued advancements in medical care, rates of maternal mortality and morbidity and pre-term birth have been rising in the U.S. Maternal and infant mortality rates in the U.S. are far higher than those in similarly large and wealthy countries and stark racial disparities in maternal and infant health persist. Improving maternal and infant health is key for preventing unnecessary illness and death and advancing overall population health. Moreover, growing calls for racial justice and the disparate impact of the COVID-19 pandemic for people of color have brought a heightened focus to health disparities, including the inequities in maternal and infant health. In particular, there has been broader recognition of the principles of reproductive justice, which emphasize the role that the social determinants of health and other factors play in reproductive health for communities of color.
A range of initiatives are underway that are designed to improve maternal and infant health and reduce disparities. Medicaid is key in these efforts given the substantial role the program plays in covering low-income pregnant women and children, particularly among people of color. This brief provides a summary of Medicaid’s role for pregnant women and infants and key Medicaid initiatives to improve maternal and infant health.
Medicaid’s Role for Pregnant Women and Infants
Medicaid provides a nationwide base of coverage for low-income pregnant women and children. Under federal rules, all states must extend Medicaid eligibility for pregnant women and children to at least 138% of the federal poverty level (FPL) ($29,974 per year for a family of three as of 2020). States can extend eligibility to higher levels through options in Medicaid as well as CHIP. As of January 2020, nearly all states (49 including DC) cover infants with family incomes up to at least 200% FPL ($43,440 per year for a family of three) through Medicaid and CHIP. Moreover, nearly all states (49) extend eligibility for pregnant women beyond the federal minimum of 138% FPL, with 35 extending eligibility to at least 200% FPL. Infants born to mothers on Medicaid are automatically covered for their first of life, while coverage for pregnant women ends after 60 days postpartum.
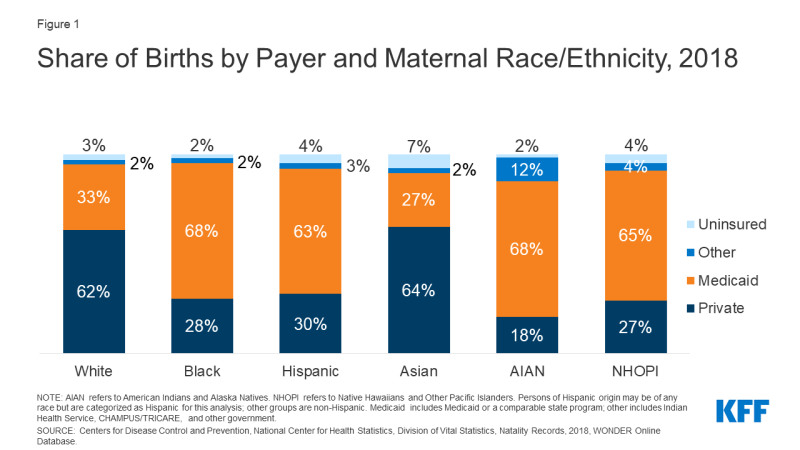
Reflecting this broad base of eligibility for pregnant women, Medicaid covers 45% of all births. The programs play an even larger role in covering births for women of color given their lower incomes and more limited access to private coverage. Medicaid covers about two-thirds of births among Black, AIAN, and NHOPI women and six in ten births among Hispanic women, compared to one in three births among White women (Figure 1).
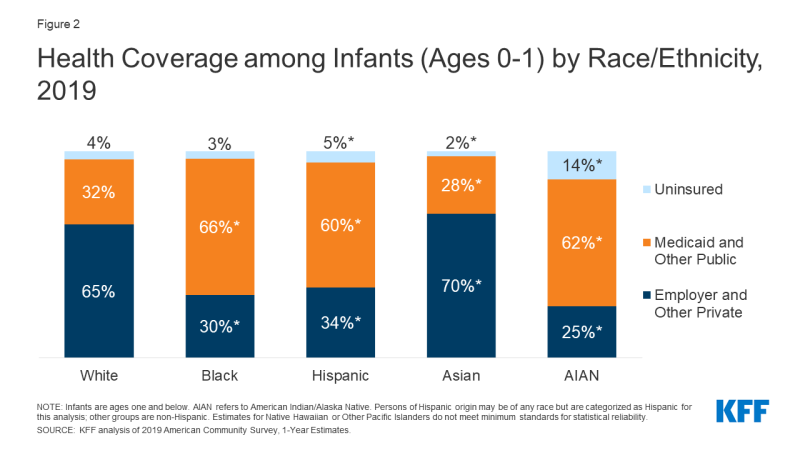
Medicaid, along with CHIP, also cover nearly half (46%) of all infants, and the programs play a particularly large role covering infants of color. Over six in ten Black, Hispanic, and AIAN infants are covered by Medicaid and CHIP compared to one-third of White infants (Figure 2). Even with these higher rates of Medicaid and CHIP coverage, Hispanic and AIAN infants remain more likely to be uninsured compared to White infants.
Research shows that coverage before, during, and after pregnancy facilitates access to care that supports healthy pregnancies, as well as positive maternal and infant outcomes after childbirth. For low-income women, Medicaid is comparable to private insurance in terms of many measures of access to care. Research also documents that Medicaid coverage of pregnant women and children has contributed to dramatic declines in infant and child mortality in the United States. A growing number of studies show that Medicaid eligibility during childhood also has long-term positive impacts, including reduced teen mortality, reduced disability, improved long-run educational attainment, and lower rates of emergency department visits and hospitalization in later life.
Medicaid Expansion Effects on Maternal and Infant Health
Through the ACA Medicaid expansion to low-income adults, states have increased coverage options for pregnant women who would otherwise lose eligibility at the end of the postpartum period. As noted, under federal rules, states must extend Medicaid eligibility to pregnant women with incomes up to at least 138% FPL and provide this coverage through 60 days postpartum. Nearly all states have expanded pregnant women eligibility beyond the minimum level, with the median eligibility level at 255% FPL as of January 2020. Prior to the ACA, many pregnant women would lose coverage at the end of the 60-day postpartum period because state eligibility levels for parents were much lower compared to the levels for pregnant women—below half of poverty in many states. The ACA expanded Medicaid eligibility to nearly all adults with incomes up to 138% FPL, increasing coverage options for pregnant women at the end of the postpartum period in expansion states. As of August 2020, 39 states, including DC, have adopted the Medicaid expansion.
Studies suggest that the ACA Medicaid expansion has had positive impacts on maternal and infant access to and use of care and health outcomes and helped to narrow racial disparities in certain measures. For example, one study found increased coverage stability and use of postpartum care during the six months postpartum in a Medicaid expansion state compared to a neighboring non-expansion state.1 Another study found that infants in non-expansion states are approximately two and half times more likely to be born into a household without health insurance compared to infants in expansion states.2 Several studies suggest that Medicaid expansion has narrowed disparities for Black and Hispanic people in certain measures of maternal and infant health, including health coverage, maternal mortality, infant mortality, low birthweight, and preterm birth.3,4, 5, 6
Even with the ACA Medicaid expansion, many women still may lose coverage at the end of the 60-day postpartum coverage period. Eligibility levels for pregnant women remain higher than those for parents in both expansion and non-expansion states, with the starkest differences in non-expansion states (Figure 3). Analysis finds that nearly half of women in non-expansion states and nearly one in three women in expansion states experience an insurance disruption from pre-pregnancy to postpartum.7 Another study on maternal insurance status during the preconception, delivery, and postpartum periods found that women of color experienced higher uninsured rates during each period compared to White women, and that disruptions in coverage disproportionately affected Hispanic, Black, and AIAN women.8
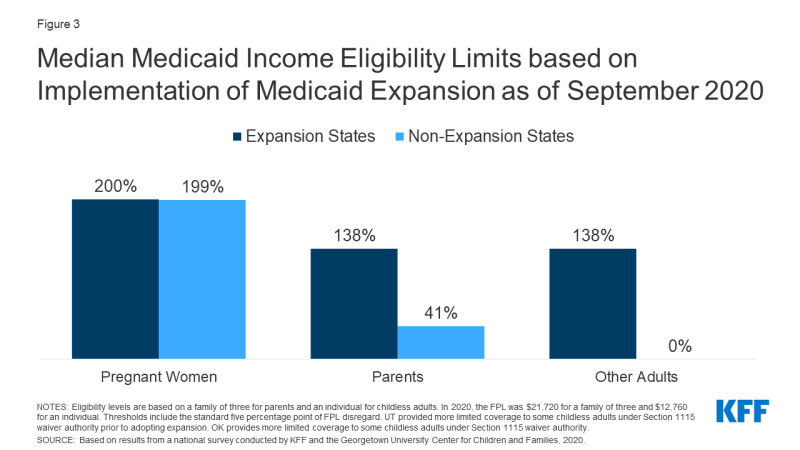
Figure 3: Median Medicaid Income Eligibility Limits based on Implementation of Medicaid Expansion as of September 2020
Medicaid Efforts to Improve Maternal and Infant Health
There has been interest at the state and federal level in extending the postpartum Medicaid eligibility period to further reduce coverage losses for women in the postpartum period. Extending the postpartum Medicaid eligibility period would increase state and federal spending, but could help reduce preventable maternal deaths and improve maternal health outcomes considering that approximately 30% of maternal deaths (excluding those caused by suicide or overdose) occur 43 to 365 days postpartum.9 One analysis estimates that approximately 217,000 uninsured low-income new mothers would benefit from the extended postpartum period.10
- As of November 2020, several states are pursuing action to extend the postpartum period. In many cases, this activity is still in the planning stage or has been set aside as the COVID-19 pandemic response takes fiscal priority in state budgets. However a few states have developed specific proposals. As of August 1, 2020, California has allocated $34.3 million in state funds to extend postpartum coverage for women diagnosed with a mental health condition. Georgia has allocated $19 million in state funding to extend coverage to 6 months postpartum, and Texas is offering a set of postpartum care services for up to 12 months for women who are eligible for the state’s family planning program. Indiana is requesting Section 1115 waiver authority to extend postpartum coverage to one year for mothers with opioid use disorder.
- Federal legislative proposals also have emerged. The Helping Medicaid Offer Maternity Services (MOMS) Act of 2020, which was passed by the House in September 2020, would provide a new state option to extend coverage for one year postpartum and increase the federal matching rate for states to take up the option. The Congressional Black Maternal Health Caucus has introduced a package of bills known as the Momnibus aimed at stemming maternal health disparities that includes measures such as diversifying the perinatal workforce and greater investment in social determinants of health. Notably, as part of COVID-19 response efforts, legislation requires states to provide continuous enrollment to Medicaid enrollees as a condition of receiving enhanced federal funding. This provision is designed to help protect against coverage losses during the pandemic, and states cannot disenroll pregnant women at the end of the postpartum period for during the public health emergency.
Most state Medicaid programs report being engaged in efforts to advance maternal and infant health. In a recent KFF survey, about two-thirds of states reported new or expanded Medicaid initiatives in FY 2019 or planned for FY 2020 to improve birth outcomes and/or address maternal mortality, with over a quarter of states focused on pregnant women with substance use disorder (SUD). These include efforts to expand eligibility for pregnant women, expand Medicaid coverage for perinatal services, and implement payment and delivery models that incentivize improvements in maternal care and outcomes.11 Some state Medicaid programs also offer benefits specifically for pregnant women such as behavioral health services, dental services, and home visiting services.12 Several states are engaged in efforts to include Medicaid coverage for doula services. Research suggests that doula services can improve health outcomes for women and infants, reduce interventions during delivery, and facilitate communication between pregnant women and health care providers.13 Having a trained advocate can be particularly important for women of color, who are more likely to encounter discrimination in the health care system. Currently, two states (Oregon, Minnesota) allow doulas to participate in their Medicaid networks statewide and other states are testing pilot programs to assess the feasibility of broader coverage. An important component for incorporating doulas in the Medicaid program is assuring adequate and timely reimbursement, which has been a challenge in some pilot programs.14
The Centers for Medicare and Medicaid Services (CMS) has launched recent initiatives focused on addressing maternal and infant health. In 2019, the Center for Medicare and Medicaid Innovation (CMMI) awarded grants to ten states (Colorado, Indiana, Louisiana, Maryland, Maine, Missouri, New Hampshire, Tennessee, Texas, and West Virginia) for its new Maternal Opioid Misuse Model, which is intended to address the fragmented care of pregnant and postpartum persons with opioid use disorder.15 It also recently released a request for information seeking input on opportunities to improve health care access, quality, and outcomes for women and infants in rural communities before, during, and after pregnancy. Further, CMS recently released its 2020 Maternity Core Set of 11 measures for voluntary reporting by state Medicaid and CHIP agencies to help evaluate maternal and perinatal health in Medicaid and CHIP.
Outside of Medicaid, the federal government, states, providers and health systems, foundations, and communities also are engaged in a broad range of efforts to advance maternal and child health and reduce disparities. For example, some Medicaid initiatives are part of broader statewide approaches to advance maternal health and reduce disparities. Moreover, outside of Medicaid, the federal government provides funding for and engages in efforts to advance maternal and infant health through the Maternal and Child Health Block Grant, the Health Resources and Services Administration, the CDC, and other agencies. The CDC recently launched the Hear Her campaign to support improved communication between pregnant and postpartum women and maternity providers, which is particularly important given the growing recognition of the role racism plays in contributing to adverse maternal health outcomes. Several states have perinatal and maternal quality collaboratives as well as maternal mortality review committees that collect and analyze data on maternal and infant health outcomes and work to improve health care delivery for women and infants. Several of these committees have focused on collecting local data by race and ethnicity, highlighting differences by both race/ethnicity and geography. Improved data collection and analysis are important tools for identifying and understanding the disparate outcomes between different subpopulations as well as for developing and targeting quality improvement initiatives within the delivery system.16 In 2019, California became the first state to require perinatal providers to obtain training on implicit bias. Further, the city of San Francisco recently launched a project that gives a group of Black and Pacific Islander pregnant persons an income supplement during pregnancy and through the infant’s first six months of life to help address some of the known health and income inequities.17
Conclusion
Maternal and infant mortality rates in the U.S. are far higher than those in similarly large and wealthy countries, and stark racial disparities in maternal and infant health persist. The COVID-19 pandemic further highlights the urgency and importance of addressing health disparities in health care more broadly, and maternal and infant health specifically.
Healthy birth outcomes and early identification and treatment of health conditions among mothers and infants helps to prevent death and illness and advance overall population health. Healthy People 2030, which provides 10-year national health objectives to set the national public health agenda, identifies the prevention of pregnancy complications and maternal deaths and improvement of women’s health before, during, and after pregnancy as a public health goal.18 Pregnancy and birth provide opportunities to identify health risks in women and children. Moreover, early identification and treatment of health conditions or complications can prevent death and disability in both mother and child, enable children to reach their full potential, as well as improve overall population health. Recent research finds that as many as 60% of all maternal deaths in the U.S. are preventable and that increasing access to preconception, prenatal, and interconception care can reduce pregnancy-related complications.19
As a primary source of coverage for pregnant women and infants, particularly among people of color, Medicaid is key to improving maternal and infant health and reducing racial disparities. A number of efforts are underway through Medicaid to improve maternal and infant health, including efforts to provide more continuous coverage, expand benefits, and implement new payment and delivery models. However, coverage is only one factor affecting maternal and infant health, and there is growing recognition that it is important for efforts to improve health and reduce racial disparities to address broad social and economic factors that influence health and racism and discrimination.