Background
The share of people in the United States who identifies as LGBT+ has increased substantially in recent years, particularly among younger generations, yet health disparities and health access-related challenges persist across multiple dimensions. Understanding the health care needs and experiences of the more than 7% of LGBT+-identified people in the United States, including the one-in-five younger adults from Generation Z, is important for addressing barriers and facilitating access to care and coverage.
While in some areas, the health experiences of LGBT+ people mirror those of their non-LGBT+ counterparts, studies have found that this population experiences certain challenges at higher rates than those who identify as heterosexual and cisgender, challenges which intersect with factors beyond sexual orientation and gender identity to include race/ethnicity, class, nationality, and age, among other aspects of identity. Recognizing this, the National Institutes of Health (NIH) identified sexual and gender minorities as a “health disparity population” to encourage and support research in this area. Further, the Biden administration has taken multiple steps to address equity in the LGBTQ community, including with respect to data collection and health care, including issuing multiple executive orders in this area, announcing that the HHS Office for Civil Rights (OCR) would include gender identity and sexual orientation as it interprets and enforces the ACA’s prohibition against sex discrimination (Section 1557), opposing state actions aimed at limiting access to gender-affirming care for transgender and gender non-conforming people, adopting protections for LGBTQ+ youth and working to provide protections for health care workers delivering gender affirming care, and issuing a Federal Evidence Agenda on LGBTQI+ Equity, a “roadmap for federal agencies” regarding “data-driven and measurable [sexual orientation and gender identity] SOGI Data.”
Despite progress in researching these issues over the past decade and increased federal commitment, much population-based research still does not include measures of sexual orientation and gender identity, limiting the ability of policymakers, policy implementers, and researchers to assess national trends and disparities, and identify needed interventions. With this report, we add to the knowledge base in this area by analyzing nationally representative data from a 2022 KFF survey of 6,442 adults ages 18 to 64, including 958 LGBT+ people, conducted primarily online from May 10, 2022, to June 7, 2022. For this survey, LGBT+ people include those who identified their sexual orientation as lesbian, gay, bisexual, or “something else,” and those who identified their gender as transgender, non-binary, “other,” or whose reported gender does not correspond to their reported sex assigned at birth. See the Methodology for additional detail.
The survey collected data on a range of demographic characteristics and issues from general well-being to experiences engaging in the health system, use of preventive services including HIV and STI testing, reproductive health, and mental health. (See also our issue brief Mental Health Care Needs and Experiences Among LGBT+ People).
Demographics
The demographics of LGBT+ adults generally mirror those of non-LGBT+ adults in many ways, with age and income being notable exceptions (Figure 1).
- LGBT+ adult demographics look similar to non-LGBT+ adults with respect to gender, race/ethnicity, urbanicity, and working status.
- Yet LGBT+ adults are significantly younger, with almost two-thirds (62%) between the ages of 18 and 35 compared to 36% of non-LGBT+ adults.
- LGBT+ people are also more likely than non-LGBT+ people to have lower incomes, with 44% of LGBT+ people earning less than 200% of the federal poverty level ($13,590 per year in 2022 for an individual) compared to 36% of non-LGBT+ people.
Health Status
LGBT+ people were more likely to be in fair or poor health than non-LGBT+ people despite being a younger population overall (Figure 2).
- One-quarter (25%) of LGBT+ people reported being in fair or poor health compared to 18% of non-LGBT+ people. This was especially common among LGBT+ people with low incomes2 and those covered by Medicaid.
- There were no statistically significant differences by race/ethnicity or gender.
LGBT+ people were managing chronic conditions and living with disabilities that impact daily life at higher rates than non-LGBT+ people (Table 1).
- Half (50%) of LGBT+ people reported that they had an ongoing health condition that requires regular monitoring, medical care, or medication, a higher share than non-LGBT+ people (45%).
- Additionally, a larger share of LGBT+ people reported having a disability or chronic disease that keeps them from participating fully in work, school, housework, or other activities than non-LGBT+ people (25% v. 16%). There were also notable differences within the LGBT+ community.
- LGBT+ adults between the ages of 45-64 reported markedly higher rates of ongoing conditions requiring care or medication than younger LGBT+ adults ages 18-44 (44% v. 70%).
- A larger share of LGBT+ people ages 18-44 reported having a disability or chronic disease (26%) than non-LGBT+ people in this age range (12%) (data not shown in table).
- LGBT+ people with Medicaid faced especially high rates of disability, which is one of the eligibility pathways into the program, compared to LGBT+ people with private insurance coverage (45% v. 15%).

Insurance Coverage and Access to Care
A smaller share of LGBT+ people had private insurance (59%) and more had Medicaid coverage (21%) than their non-LGBT+ counterparts (64% and 16%, respectively), reflecting their lower incomes which were driven, at least in part, by being a younger population (Figure 3). Similar shares were uninsured.
Most LGBT+ people reported having a regular doctor or health care provider, though they were less likely to have one than non-LGBT+ people.
- LGBT+ people reported lower rates of having a regular doctor or provider than their non-LGBT+ counterparts (72% v. 77%) (Figure 4). Research has found that having a usual source of care is associated with increased use of preventive care and better health outcomes.
- Among LGBT+ people, rates were significantly lower for those ages 18-44 than those ages 45-64 (68% v. 86%) and among those who were uninsured (36%).
Nearly three-quarters (74%) of LGBT+ people with a usual source of care got that care at a doctor’s office, though one in five (20%) obtained their routine care at a clinic, such as a health department, health center, school clinic, urgent care center, or clinic inside a store or pharmacy. Smaller shares went to an emergency room or some other place (6%) (Figure 5). The type of location where care was received was similar among LGBT+ and non-LGBT+ people (data not shown in figure).
Telehealth has become an increasingly common way to access care, including among LGBT+ people, who reported higher use of telehealth visits over the past two years than did non-LGBT+ people (63% v. 53%) (Figure 6).
- There were no statistically significant demographic differences among LGBT+ people who used telehealth in the past two years except for those who were uninsured, who reported lower rates of telehealth use (39%) than those with Medicaid (67%) or private insurance (64%). Similarly, non-LGBT+ people without insurance reported lower rates of telehealth use than those with Medicaid and private insurance (data not shown in figure).
- About one in ten (9%) LGBT+ people reported using an online prescribing platform or app, such as Nurx, The Pill Club, Roman, or hims/hers to receive a prescription or health care service, similar to the share among non-LGBT+ people (6%) (data not shown in figure).
Use of Health Care Services
More than nine in ten (93%) LGBT+ people saw a doctor or health care provider in the past two years but fewer than three-quarters (73%) of this group had a general check-up or well-woman visit3 in that period. Both findings were similar to the share among non-LGBT+ people (Table 2).
- LGBT+ people who were uninsured were significantly less likely than those with health coverage (either Medicaid or private insurance) to have seen a provider (80% v. 94%) or had a wellness check-up in the past two years (57% v. 74%).
Use of preventive cancer screenings can lead to early identification of conditions when they are more responsive to medical interventions and potentially avert serious complications. While uptake of colonoscopies among LGBT+ people was similar to that of non-LGBT+, slightly higher shares of non-LGBT+ people reported having had a pap smear in the past two years than LGBT+ people (Figure 7).
- Slightly smaller shares of LGBT+ people assigned female at birth4 ages 21-64 reported having had a pap smear in the past two years than their non-LGBT+ counterparts (54% v. 59%).
- Forty-five percent of LGBT+ people ages 45-64 reported having had a colon cancer screening in the past two years, similar to non-LGBT+ people (37%).
A higher share of LGBT+ people reported taking at least one prescription medication on a regular basis than non-LGBT+ people, despite being a younger population overall (62% v. 55%) (Figure 8).
- As with non-LGBT+ people, prescription use among LGBT+ people increased with age.
- However, the share of LGBT+ taking a prescription was higher across each age group, except those ages 45 to 64, when compared to non-LGBT+ people.
- Looking at the youngest group, more than half (54%) of LGBT+ people ages 18 to 24 reported regularly taking a prescription compared to just over one-third (36%) of non-LGBT+ people in the same age group.
Sexual and Reproductive Health
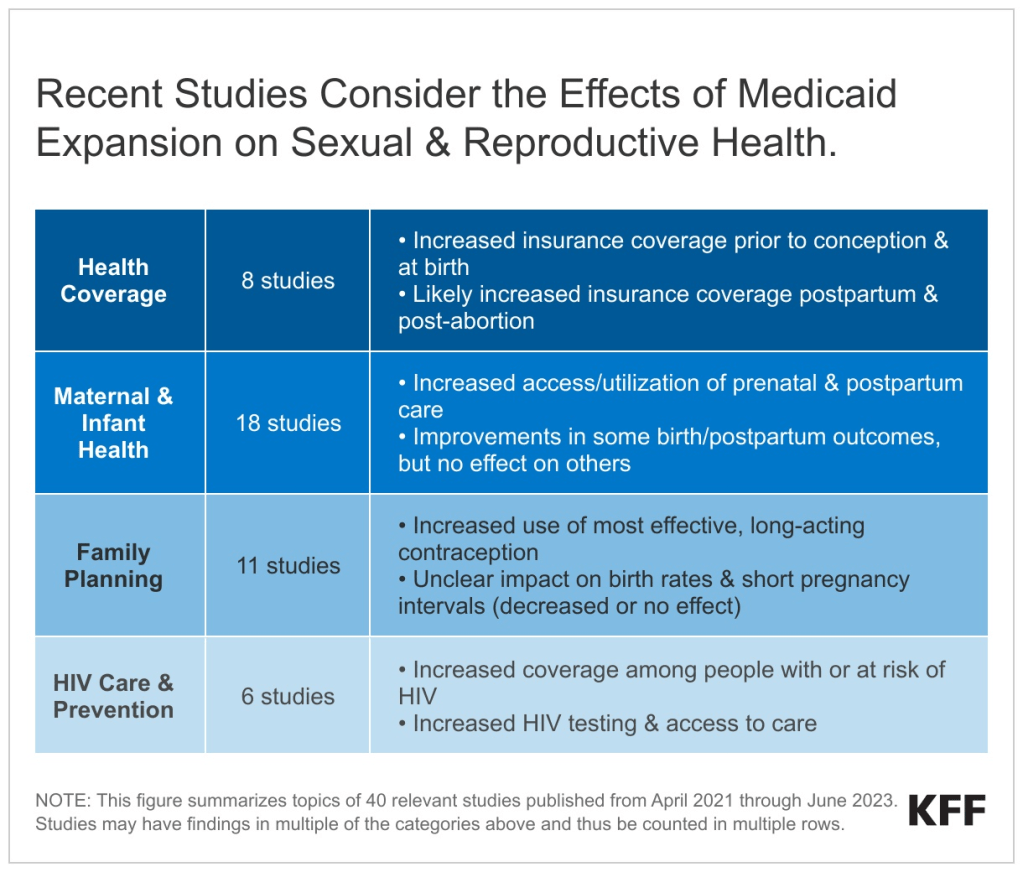
LGBT+ people reported higher rates of receiving testing for sexually transmitted infections (STIs) and for HIV than their non-LGBT+ counterparts, services that are recommended for early detection, treatment, and preventing transmission (Table 3).
- However, uptake is still relatively low. Thirty-five percent (35%) of LGBT+ people ages 18-64 have been tested for HIV in the past two years, higher than the share of non-LGBT+ people (19%).
- Among LGBT+ people, testing rates were highest among those ages18-44.
- Nearly four in ten (37%) LGBT+ people ages 18-64 have been tested for an STI (other than HIV) such as chlamydia or herpes in the past two years, higher than the share of non-LGBT+ people (19%).
- Among LGTB+ people, STI testing rates were also higher among those who were younger (43%).

The majority (70%) of LGBT+ people assigned female at birth5 have used contraception in their lifetime, compared to 77% of their non-LGBT+ counterparts, and most used more than one type of contraception across their lifetime (70%). Three in four (75%) sexually active reproductive-age (18-49) LGBT+ people assigned female at birth who were not pregnant reported using contraception in the past year. The share of LGBT+ people using contraceptives is largely driven by bisexual women.
- Over half (55%) of LGBT+ reproductive-age people assigned female at birth who used contraception in the past year did so for a reason other than preventing pregnancy compared to 35% of their non-LGBT+ counterparts. This share includes the nearly one in five (18%) LGBT+ people who used contraception solely for a reason other than preventing pregnancy, like managing a medical condition or preventing an STI (Figure 9).
The share of LGBT+ reproductive-age people assigned female at birth had similar contraceptive method use patterns to non-LGBT+ females (Table 4).
- However, larger shares of LGBT+ people said they used injectable contraception, contraceptive patches, contraceptive implants, and male condoms compared to non-LGBT+ females.
Across the lifespan, four in ten LGBT+ people ages 18-64 assigned female at birth have ever been pregnant compared to seven in ten non-LGBT+ females (Figure 10).
- Lower shares of LGBT+ people said their pregnancies resulted in a birth, while higher shares said they have experienced a miscarriage compared to their non-LGBT+ counterparts.
Mental Health
Two-thirds (67%) of LGBT+ people reported needing a mental health service over the past two years, compared to four in ten (39%) non-LGBT+ people (Figure 11). Surveys regularly find that LGBT+ people are more likely than non-LGBT+ people to experience mental health conditions such as depression and anxiety, which can result from ongoing experiences of discrimination, stigma, and violence.
- Among LGBT+ people, self-reported need for mental health care was higher for those who were younger (ages 18-34) compared to those ages 35-64 and for those with Medicaid compared to those with private insurance (data not shown in figure but available in Mental Health Care Needs and Experiences Among LGBT+ People).
While the reported need for mental health services was high among LGBT+ people, not all of those with a need for services sought or received them.
- Sixty-five percent (65%) of LGBT+ people who reported needing a mental health service sought one, a higher share than among non-LGBT+ people (58%), but more than one-third (35%) did not (Figure 12).
For additional detail on mental health and LGBT+ people see our companion issue brief on this topic, Mental Health Care Needs and Experiences Among LGBT+ People.
Provider Interactions
LGBT+ people were more likely to report a range of negative provider experiences in the past two years compared to non-LGBT+ people. This may limit their willingness to seek care, which could be especially problematic for this group which has higher rates of certain health conditions compared to non-LGBT+ people. Negative interactions included having a provider not believe they were telling the truth, suggesting they were personally to blame for a health problem, assuming something about them without asking, or dismissing their concerns. LGBT+ people were more likely to report experiencing discrimination based on their age, gender, race, sexual orientation, religion, or some other personal characteristic during a health care visit (Figure 13).
- Altogether, nearly half (45%) of LGBT+ people who had visited a health care provider in the past two years reported at least one of these negative experiences with a provider or during a health care visit, compared to one-third (33%) of non-LGBT+ people. LGBT+ people were twice as likely as non-LGBT+ people to report that they had been discriminated against during a health care visit over the past two years (12% v. 6%).
Among LGBT+ people, these negative provider experiences were more commonly reported by women, younger groups, those with low incomes, and those with a disability or chronic disease. Large shares, in most cases more than half, of LGBT+ people in these groups reported having at least one of these negative provider experiences in the past two years (Table 5).
Communication is an important component of health care quality but three in ten (29%) LGBT+ people said it is difficult to find a doctor who explains things in a way that is easy to understand, higher than the share of non-LGBT+ people (19%) (Figure 14).
- LGBT+ people who were younger, low-income, and had Medicaid coverage or were uninsured had more difficulty finding a doctor who provides clear explanations than those who were older, higher income, or had private insurance.
Health Care Costs
LGBT+ people reported having problems with health care costs at similar rates as non-LGBT+ people, with nearly one-third (29%) of LGBT+ people and one-quarter (25%) of non-LGBT+ people reporting they or a household member had problems paying medical bills in the past 12 months (Figure 15). Given that LGBT+ people tend to be younger, have lower incomes, and have greater health needs, costs could be an outsized barrier to care for this group.
- Among LGBT+ people, this challenge was especially acute for those who reported being in fair or poor health, with 42% saying they have had problems paying medical bills.
- Not surprisingly, those with low incomes, the uninsured, and those in fair or poor health reported these challenges at higher rates than their counterparts but there were no statistically significant differences by gender.
Medical bills have consequences on LGBT+ people’s financial well-being, including their ability to afford basic necessities.
- Among the 29% LGBT+ people who reported having trouble paying medical bills in the past 12 months, six in ten (61%) said they used up all or most of their savings (Figure 16). About the same share said they had to set up a payment plan with a doctor or hospital (59%) or had difficulty paying for basic necessities (57%), and over half (53%) said they have been contacted by a collection agency, while 47% said they borrowed money from family or friends as a result of these bills. Non-LGBT+ people experience these consequences at similar rates.
Conclusion
While in many cases LGBT+ people have similar health and health care experiences to non-LGBT+ people, we find some notable differences. For example, LGBT+ people’s self-reported health status was poorer than non-LGBT+ people, despite being a younger population. They also reported wider prescription usage, and younger LGBT+ people reported higher rates of disability than younger non-LGBT+ people. Additionally, LGBT+ people reported a higher need for mental health services, which could relate to ongoing experiences of stigma and discrimination. Indeed, LGBT+ people reported higher rates of discrimination during a health care visit and were more likely to report a range of recent negative provider experiences, most commonly among LGBT+ women, those who were younger, had low incomes, and reported a disability or chronic disease. These experiences suggest a gap in clinical attention and/or competency for reaching LGBT+ people, especially those with intersecting marginalized identities.
More broadly, while data collection on LGBT+ people is improving, particularly at the federal level, it is still not standard, and as such, knowledge gaps remain, including with respect to health status, health needs, and health care access. Lack of research in this area limits the ability of those in both policy and health care sectors to address health needs and disparities within the LGBT+ population. As efforts aimed at limiting LGBT+ people’s access to social institutions, including health care, increase, continuing to monitor the community’s well-being and responding to discrimination and health challenges is especially timely.