Public Knowledge and Attitudes About Sexually Transmitted Infections: KFF Polling and Policy Insights
Key Findings:
There are an estimated 20 million new sexually transmitted infections (STIs) every year in the United States with rates of reported STIs continuing to rise, reaching record-breaking levels in 2018. This poll provides new data on the public’s knowledge and attitudes about STIs.
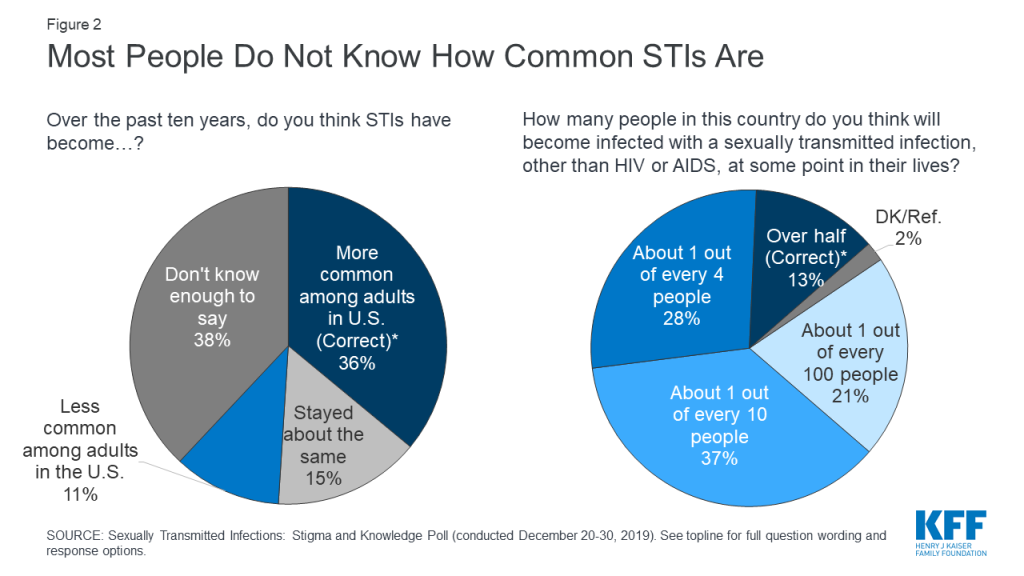
- Large majorities of the public are unaware of how common STIs are among adults in the U.S. About one-third (36%) are aware that STIs have become more common over the past decade and few (13%) know that over half of people in the U.S. will get an STI sometime during the lifetime.
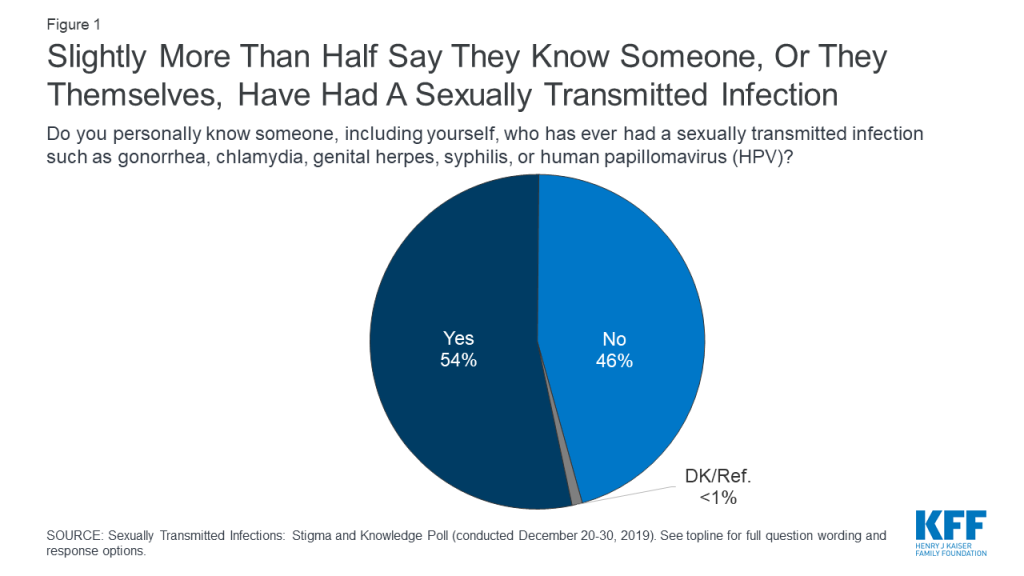
- Slightly more than half (54%) say they know someone who has had an STI, including those who say they have personally had an STI. There are some differences by key demographic groups with larger shares of women and younger adults saying they personally know someone who has had an STI.
- Small shares of the public (8%) are worried about contracting an STI in the next year, with larger shares of younger people, ages 18-29, expressing concern (20%). About one in ten Black adults (13%) and Hispanic adults (13%) and 5% of White adults say they are worried they may personally contract an STI in the next year.
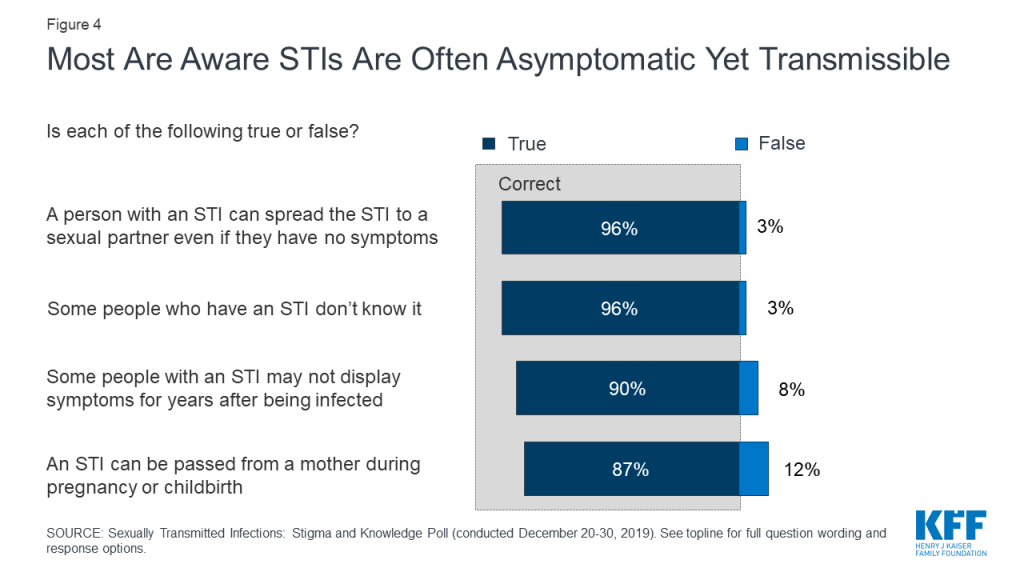
- Overall, the public is aware that STIs are often asymptomatic, yet transmissible. Large majorities know that STIs can be transmitted even when that person is not showing any symptoms (96%) as well as during pregnancy and childbirth (87%). Equally large shares are aware some people who have an STI might not even know it (96%) and symptoms may not display in some people with an STI for years (90%).
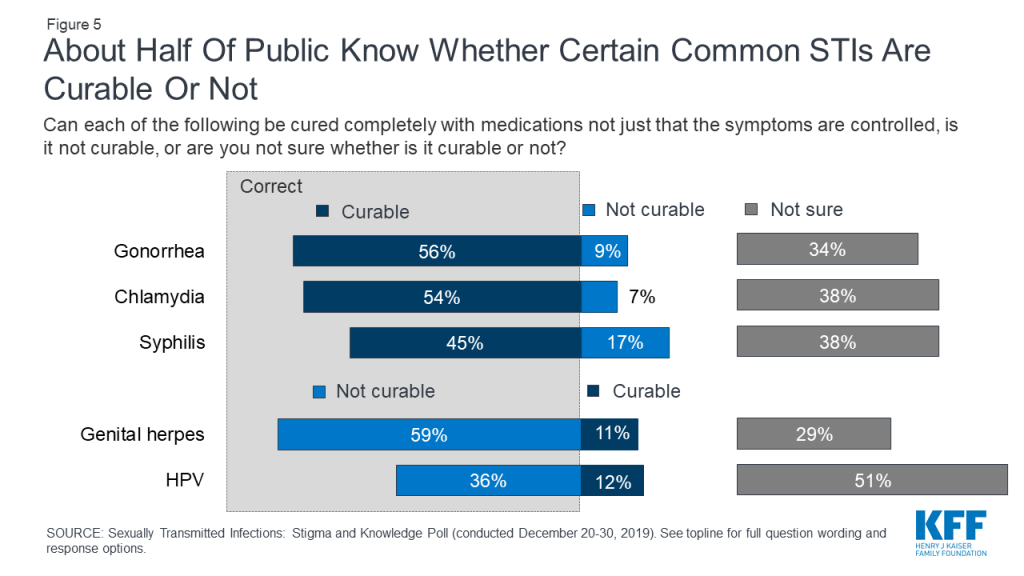
- About half know chlamydia (54%), gonorrhea (56%), and syphilis (45%) are curable. More than half (59%) know that genital herpes is not curable.
Sexually Transmitted Infections
Slightly more than half (54%) of adults say they personally know someone, including themselves, who has had an STI such as gonorrhea, chlamydia, genital herpes, syphilis, or human papillomavirus (HPV). Nearly six in ten women (58%) say they know someone who has ever had an STI, as do half of men. Older adults are less likely to know someone compared to younger age groups (18-29 year olds: 54%; 30-49 year olds: 63%; 50-64 year olds: 57%; 65 and older: 36%).
Despite this, few know how common STIs are in the U.S. today and that STIs are on the rise. One-third of adults (36%) are aware that STIs have become “more common” over the past ten years, but this is similar to the share who say they “don’t know enough to say” (38%) and only ten percentage points higher than the share (26%) who either say STIs have become “less common” or “stayed about the same.” About one-third of men (32%) are aware that STIs have become more common over the past decade and about four in ten women are aware (39%). Awareness is also higher among Black adults (48%) compared to White adults (33%). Four in ten Hispanic adults are also aware STIs have become more common.
Additionally, a small percentage (13%) know that “over half of the people in the U.S.” will have an STI, other than HIV, at some point in their lifetime.
How Common Are Sexually Transmitted Infections?
- Sexually transmitted infections (STIs) are very common, and over half of people in the U.S. will have an STI in their lifetime. In fact, the CDC estimates there are over 110 million sexually transmitted infections among men and women in the U.S., with 20 million new cases each year.
- HPV is the most common STI (79 million cases), followed by genital herpes (24 million), trichomoniasis (3.7 million) and chlamydia (1.6 million). Gonorrhea, syphilis, hepatitis B and HIV are less common, although rates of syphilis, gonorrhea and chlamydia are rising, up 71%, 63% and 19% respectively from 2014 to 2018.
- While STIs are most common among adolescents and young adults aged 15-24, all age groups are affected.
About one in ten (8%) are worried that they personally will contract a new STI over the next year, yet there are some groups who worry more about contracting an STI. Larger shares (20%) of younger adults (18-29) report being worried which is consistent with data from the CDC which states that this age group is the group at the highest risk for STIs. Additionally, STI rates are higher among Black adults and Hispanic adults compared to White adults. At least one in ten Hispanic adults (13%) and Black adults (13%) say they were worried about contracting an STI, compared to 5% of White adults.
| Table 1: Share of U.S. Adults Who Are Worried They Will Contract A New STI Over The Next Year | |
| Percent who say they are either “very worried” or “somewhat worried”: | |
| Total adults | 8% |
| Men | 10 |
| Women | 6 |
| 18-29 years old | 20 |
| 30-49 years old | 9 |
| 50-64 years old | 4 |
| 65 and older | 1 |
| White, Non-Hispanic | 5 |
| Black, Non-Hispanic | 13 |
| Hispanic | 13 |
About one in eight say they are uncomfortable discussing STIs with a sexual partner (12%) and one in seven (15%) are uncomfortable talking about STIs with a doctor. In fact, large majorities of the public say they are “very comfortable” or “somewhat comfortable” talking about STIs with their doctor or health care provider (84%) or sexual partners (75%). Smaller majorities are comfortable talking about STIs with their close friends (67%) or family (61%). Similar shares also report feeling comfortable talking about their sexual health with these different groups. In a survey conducted more than two decades ago, KFF found that more than one-third of the public were uncomfortable discussing STIs with a sexual partner (37%) and three in ten (31%) were uncomfortable talking with a doctor about getting an STI test (compared to 12% and 15% in the most recent survey).
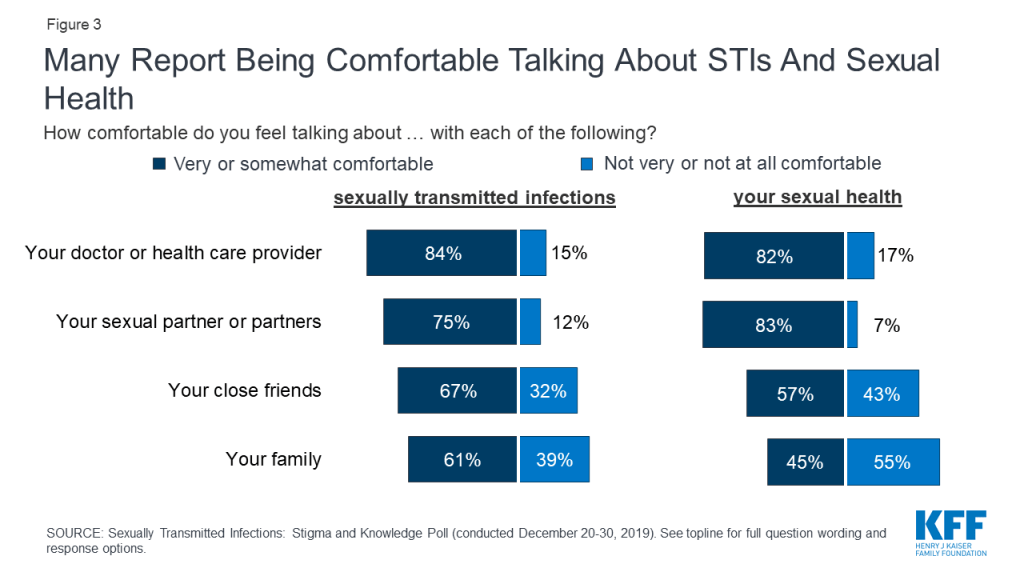
There are some differences by age and gender in how comfortable people are talking about the topic. A higher share of women than men said they were comfortable talking with their close friends about STIs (71% vs. 61%, respectively) and their sexual health (62% vs. 52%).
While most new STIs are among young adults, older adults are also at risk. A smaller share of those 65 and older say they are comfortable talking about STIs and their sexual health with a variety of audiences, compared to younger adults.
| Table 2: Comfort Level Talking About STIs and Sexual Health, by Age | ||||
| Share who feel very or somewhat comfortable talking about: | Adultsages 18-29 | Adultsages 30-49 | Adultsages 50-64 | Adultsages 65+ |
| Sexually transmitted infections with their… | ||||
| Doctor or health care provider | 83% | 87% | 88% | 77% |
| Sexual partner(s) | 79 | 85 | 75 | 60 |
| Close friends | 69 | 71 | 68 | 57 |
| Family | 51 | 59 | 71 | 60 |
| Sexual health with their… | ||||
| Doctor or health care provider | 80 | 80 | 86 | 81 |
| Sexual partner(s) | 84 | 90 | 84 | 69 |
| Close friends | 66 | 68 | 51 | 38 |
| Family | 38 | 52 | 52 | 33 |
| NOTE. Grey box indicates statistical significance at p<.05 compared to all other age groups. | ||||
Understanding of STI Transmission and Treatment Options
The vast majority of adults are aware that STIs are often asymptomatic, yet transmissible. More than nine in ten adults are aware that a person with an STI can spread it to a sexual partner even if they do not have any symptoms (96%) as well as during pregnancy and childbirth (87%). Equally large shares are aware some people who have an STI might not even know it (96%) and that some people with an STI may not display symptoms for years after contracting the STI (90%).
Large shares of the public are unsure about whether many STIs are curable with medication or not. Slightly more than half of adults know gonorrhea and chlamydia are curable with medication (56% and 54%, respectively), and genital herpes is not curable with medication (59%). Fewer are aware that syphilis is curable with medication (45%). About half (51%) of the public say they are unsure if HPV is curable with medication or not. HPV is a common STI that has more than 150 different strains (including some associated with cervical and other cancers and others that cause genital warts). There is no medical treatment for HPV, however, most people who acquire HPV (specifically those not associated with cancer or warts) will clear the infection on their own and without health problems. There is a vaccine available to protect against some of the more serious types of HPV.
In 1998, less than half of the public knew gonorrhea and chlamydia could be cured with medications (48% and 32%, respectively), while now more than half are aware of this (56% and 54%, respectively). Awareness that both genital herpes and HPV are not curable with medications has not changed over the past two decades.
| STI Treatment and Management | |
| STI | Treatments |
| Gonorrhea | Curable with antibiotics |
| Chlamydia | Curable with antibiotics |
| Syphilis | Curable with antibiotics |
| Trichomoniasis | Curable with antiparasitic medications |
| Genital Herpes (HSV) | Lifelong infection, but symptoms can be treated with antiviral medication |
| Human Papillomavirus (HPV) | Most people who acquire HPV will clear the infection on their own and without associated health problems. There is a vaccine for some types of HPV associated with cervical cancer that is recommended beginning at age nine. |
Knowledge around treatment of STIs is generally higher among those who are under the age of 65. Majorities of younger adults are aware that chlamydia and gonorrhea are curable and that genital herpes is not curable with medication, compared to less than half of adults 65 and older who are aware of this. For each STI assessed, individuals aged 65+ were significantly less likely to correctly identify whether they are curable or not, compared to adults younger than 65 years old.
| Table 3: Awareness of STI Treatment and Management, by Age | ||||
| Percent who correctly know the following: | Adults ages 18-29 | Adults ages 30-49 | Adults ages 50-64 | Adults ages 65+ |
| Chlamydia is curable | 57% | 66% | 55% | 34% |
| Gonorrhea is curable | 56 | 60 | 61 | 46 |
| Syphilis is curable | 34 | 49 | 53 | 39 |
| Genital herpes is not curable | 57 | 68 | 66 | 41 |
| HPV is not curable | 46 | 49 | 30 | 15 |
| NOTE. Grey box indicates statistical significance at p<.05 compared to all other age groups. | ||||
There were also some differences by gender and race. A larger share of women than men correctly reported that chlamydia is curable and that HPV is not curable (even though most people who acquire HPV will clear the infection on their own and there is a vaccine for HPV prevention), while awareness about other infections was similar between women and men. A higher share of Black adults know that chlamydia, gonorrhea and syphilis are curable, compared to other races. A previous 2017 KFF survey showed a higher share of Black and Latina women compared to White women said their physician discussed STIs with them.
| Table 4: Awareness About STI Treatment and Management, by Gender and Race/Ethnicity | |||||
| Percent who correctly know the following: | Gender | Race/Ethnicity | |||
| Women | Men | Black | White | Hispanic | |
| Chlamydia is curable | 61% | 47% | 74% | 51% | 49% |
| Gonorrhea is curable | 56 | 57 | 75 | 55 | 48 |
| Syphilis is curable | 44 | 46 | 54 | 44 | 39 |
| Genital herpes is not curable | 62 | 56 | 64 | 62 | 53 |
| HPV is not curable | 40 | 33 | 32 | 39 | 35 |
| NOTE. Grey box indicates statistical significance at p<.05 compared to all other groups in demographic category. | |||||