Rising Cases in Long-term Care Facilities Are Cause for Concern
Over the last month, many states have seen a surge of coronavirus cases, particularly in states that have loosened social distancing requirements. Data shows that younger people make up a growing percentage of new coronavirus cases in cities and states, and much recent media coverage has focused on the resurgence of the pandemic being driven by cases among younger adults. Less attention has been paid to recent trends in cases among residents and staff in long-term care facilities and how these relate to surges in “hotspot” states.
Coronavirus cases in long-term care facilities continue to rise. Over a 14-day period that ended on July 10th, cases increased by 11% in long-term care facilities across the 35 states for which we were able to trend this data over this period (Table 1 and Figure 1). Long-term care facilities have implemented the strictest protocols in the country not only to prevent the virus from entering facilities, but also to prevent the spread of the virus once it is in the facility. Some of these policies include universal testing for residents and staff in long-term care facilities, strict visitor restrictions, and isolating positive-testing residents. Regardless of these measures, facilities continue to see a rise in cases. A rise in cases in long-term care facilities is particularly concerning, given that those who live in long-term care facilities are more vulnerable to severe illness and death from the virus than the general population.
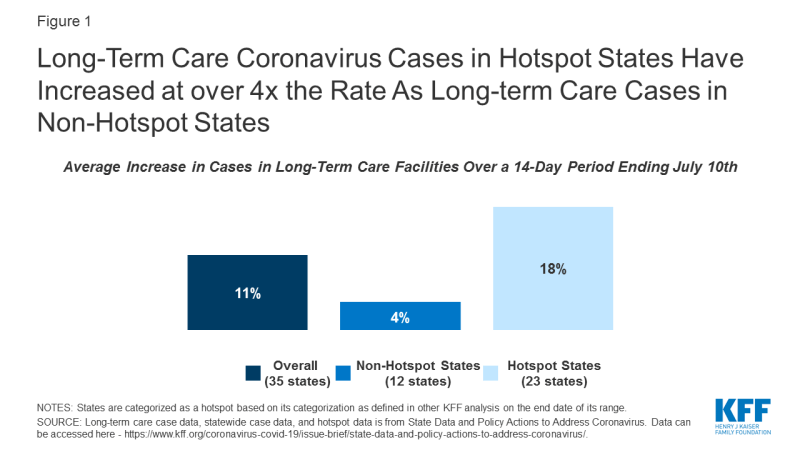
Figure 1: Long-Term Care Coronavirus Cases in Hotspot States Have Increased at over 4x the Rate As Long-term Care Cases in Non-Hotspot States
Long-term care cases in “hotspot states” with wider community transmission have risen at four times the rate as long-term care cases in non-hotspot states. Long-term care facility cases in 23 hotspot states where data are available rose by 18% over a 14 day period (from 123,000 cases to 144,800 cases), while long-term care cases in 12 non-hotspot states rose by 4% over a similar 14-day period (from 125,500 cases to 130,300 cases). (Figure 1). These patterns indicate likely connection between widespread community transmission and long-term care cases, despite precautions in place in most long-term care facilities.
The two states with the highest overall increase in cases statewide, Texas and Florida, also report the highest increase in cases in long-term care facilities, with both states reporting an increase of approximately 50% in long-term care cases between June 24th and July 9th and nearly a doubling of cases during this time period (Table 1). These states, in particular, have garnered media attention, given the record-breaking numbers of new cases every day in these states. Experts have attributed these spikes to their quick pace of reopening, lack of social distancing measures such as face mask requirements, and increased population movement due to warmer weather. Increased cases in long-term care facilities may be attributed in part to increased testing of long-term care residents, but it likely represents a real increase in infections connected to the near doubling of all cases across the state in this 14-day period. The share of tests coming back positive in Texas and Florida are well over 10%, suggesting that community transmission is widespread and increasing.
Another factor that may contribute to continued long-term care case increases is resource shortages, with nearly 1 of 3 nursing homes reporting a staffing shortage, PPE shortage, or both. As of June 28th, nearly 3,000 nursing homes across the country indicated a shortage of nursing staff, clinical staff, aides, or other staff. Nearly 2,700 nursing homes indicated a shortage of PPE supplies, which includes N95 masks, surgical masks, eye protection, gowns, gloves, and hand sanitizer. About 4,800 nursing homes (nearly 1 in 3 nursing homes) reported either a staffing shortage or a PPE shortage, indicating relatively widespread resource shortages. These shortages look similar between hotspot and non-hotspot states, with about 30% of nursing homes in each group of states reporting any shortages of staff or PPE (2,800 of 9,400 nursing homes in hotspot states and 1,000 of 3,300 nursing homes in non-hotspot states).1
Methods
This analysis includes data from 35 states that reported the number of COVID-19 cases in long-term care facilities over a recent two-week period. The definition of “long-term care facility” differs by state, but data reflect a combination of nursing facilities, assisted living facilities, adult care centers, intermediate care facilities, and/or other long-term care facilities. Data primarily reflects cumulative cases for residents and staff, where available. States update their data on different schedules, many weekly, so we chose the most recent two-week period for each state. The starting date of the time period analyzed ranges from 6/17-6/25, and the ending date ranges from 7/2-7/10. Long-term care data availability is limited by state’s reporting. Thus, the “2-week period” or “14-day time period” for which we calculate the case increase rate ranges between 13 and 17 days, depending on how often a state updates its data. Some states that report long-term care case data were excluded from this analysis because of inconsistent reporting (e.g. data comes from inconsistently available media reports), changes in reporting over the two-week period (e.g. the addition of staff cases), or the inability to identify new cases over the course of the two-week period. States are categorized as a hotspot based on its categorization as defined in other KFF analysis on the end date of its range. Detailed state-level data is available in Table 1.
