Two Year Trends in Medicaid and CHIP Enrollment Data: Findings from the CMS Performance Indicator Project
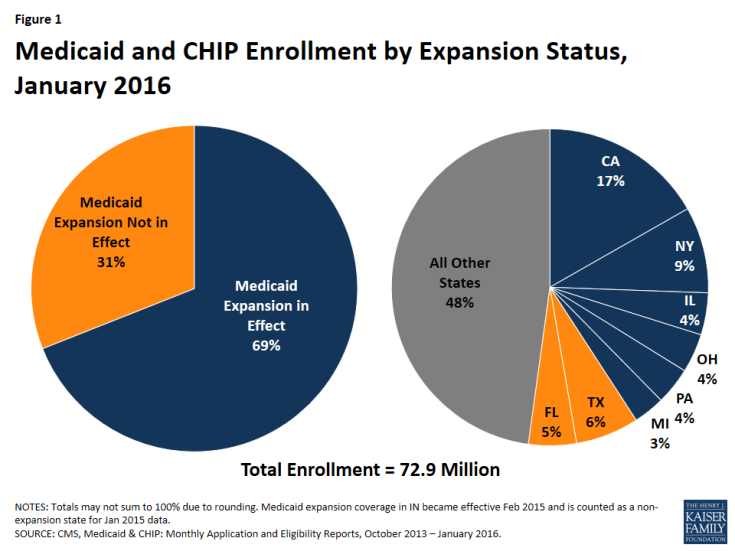
As of the end of January 2016, 72.9 million people were enrolled in Medicaid or CHIP coverage nationwide. Over two-thirds (50.1 million of the 72.9 million) of all Medicaid and CHIP enrollees resided in states that have implemented the Medicaid expansion (Figure 1). A combination of expansion and non-expansion states have the highest Medicaid enrollment. California, New York and Texas account for just about one-third of all Medicaid enrollment. Together with Florida, Illinois, Ohio, Pennsylvania, and Michigan these eight states account for just over half of all Medicaid enrollment. (See Appendix Table B for state tables on enrollment.)
Between Summer 2013 and January 2016, there was a net increase of nearly 15.5 million people enrolled in Medicaid and CHIP among the 49 states reporting data for both periods. Most of this growth was in large states that implemented the Medicaid expansion (Figure 2). Overall, 82% of the net enrollment growth occurred in expansion states, and 48% was in the West, reflecting sizeable enrollment gains in large western states like California and recent expansion decisions in Montana and Alaska. Half (50%) of the 15.5 million net increase is attributable to growth in six expansion states (CA, NY, WA, KY, OH, and CO), with California accounting for 29% of the overall net growth. Changes in total enrollment over this period reflect varied factors including both net gains in enrollment and changes in the number of states reporting data.1
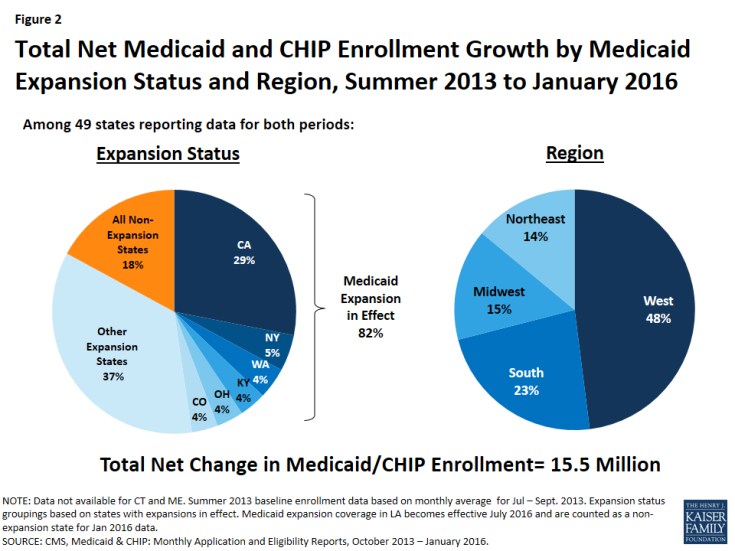
Figure 2: Total Net Medicaid and CHIP Enrollment Growth by Medicaid Expansion Status and Region, Summer 2013 to January 2016
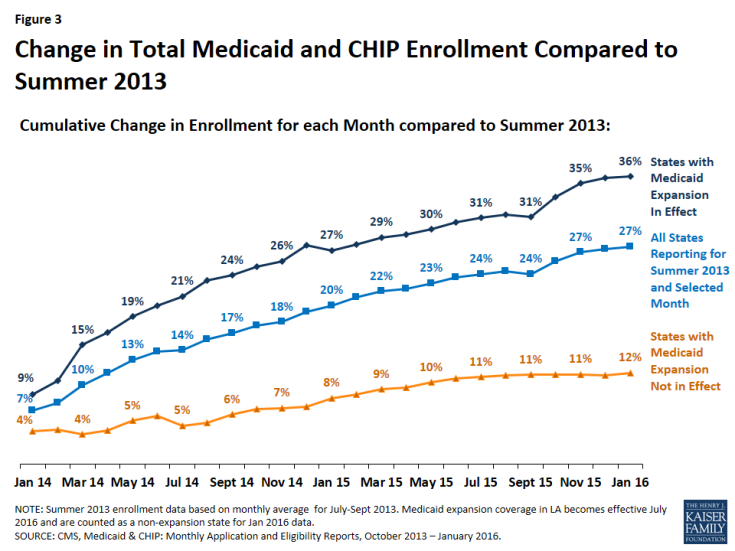
States that expanded Medicaid have experienced significantly greater net Medicaid and CHIP enrollment growth since prior to the beginning of open enrollment than states that have not expanded. Nationally, total Medicaid and CHIP enrollment grew by 27% between Summer 2013 and January 2016. Growth was over three times higher (37%) in states that implemented the expansion compared to states where the Medicaid expansion is not in effect (12%) (Figure 3). However, there is significant variation in total growth across individual states from a high of 95% growth in Kentucky to slightly negative growth in Wyoming and Nebraska. (Figure 4)
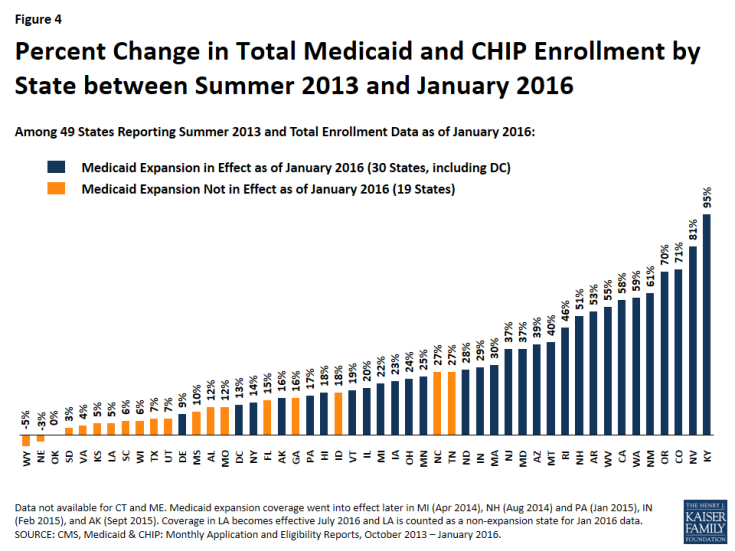
Figure 4: Percent Change in Total Medicaid and CHIP Enrollment by State between Summer 2013 and January 2016
Most growth occurred in the first year, with growth rates tapering off from January 2015-January 2016. Across all states, enrollment had increased by 20% compared in January 2015, to the Summer baseline data. Growth rates tapered in the following year to 7% with cumulative growth of 27% over the period. Across all states that implemented the expansion in January 2014, growth rates have slowed in the second year of implementation. (Figure 5)
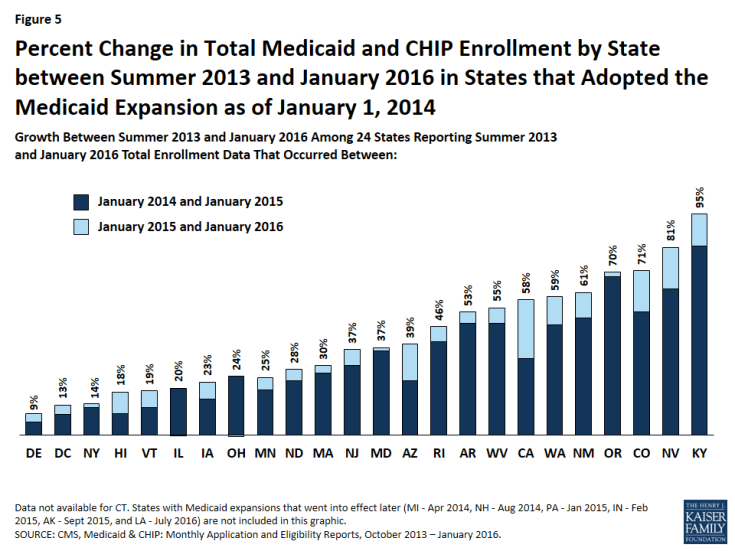
Figure 5: Percent Change in Total Medicaid and CHIP Enrollment by State between Summer 2013 and January 2016 in States that Adopted the Medicaid Expansion as of January 1, 2014
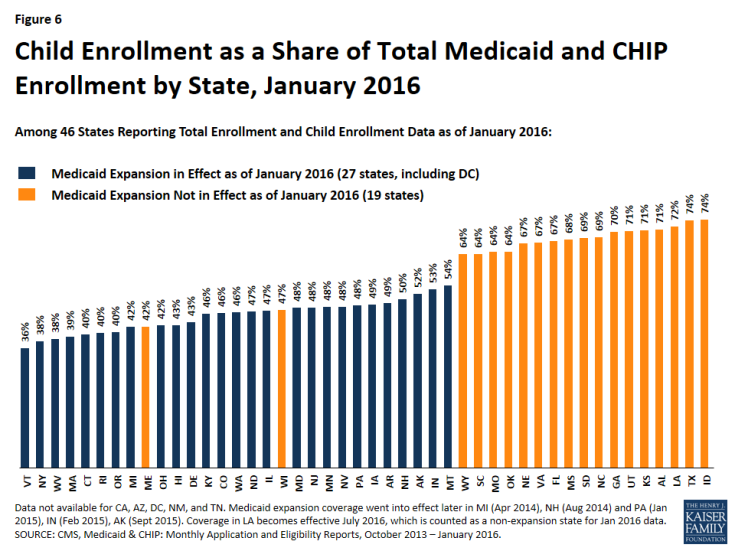
Children account for a greater share of total Medicaid and CHIP enrollment in nearly all states that have not expanded Medicaid. Among the 46 states reporting data for child and total enrollment as of January 2016, children made up just over half (53%) of total Medicaid and CHIP enrollment. They accounted for over two-thirds of total enrollment (68%) in states that have not expanded Medicaid compared to well under half (44%) among the states that have expanded and enrolled many new adults (Figure 6). The pattern is reflective of the fact that children’s eligibility levels are higher than those for adults in states that have not expanded.
Between January 2014 (the earliest children data reported) and January 2016, child enrollment increased by 1.9 million or 8% across the 36 states reporting data for both periods. Growth was 8% cumulative between January 2014 and January 2016 with a 6% increase in the first year and a 2% increase in the second year. Percent change over the two year period ranged from an increase of 23% in North Carolina to a decrease of 9% in Wyoming.
Conclusion
Data show that there has been significant net growth in Medicaid and CHIP enrollment since the major ACA coverage expansion went into effect, and states that have expanded Medicaid have experienced significantly greater growth compared to non-expansion states. Growth rates appear to be tapering off in year two following the implementation of the ACA.
Reflecting higher eligibility levels for children, children make up a greater share of total Medicaid and CHIP enrollees in non-expansion states compared to states that have expanded to adults. As a broader set of performance data is reported over time, the data will provide greater understanding of state Medicaid and CHIP eligibility and enrollment experiences, although they will not provide information on the number of newly eligible adults enrolled through the ACA Medicaid expansion. The performance data will complement other data initiatives at the federal level as well as additional reporting at the state level to provide more comprehensive and timely information on Medicaid and CHIP eligibility and enrollment that can support data-driven quality-improvement efforts and overall program management and oversight efforts at both the national and state level.