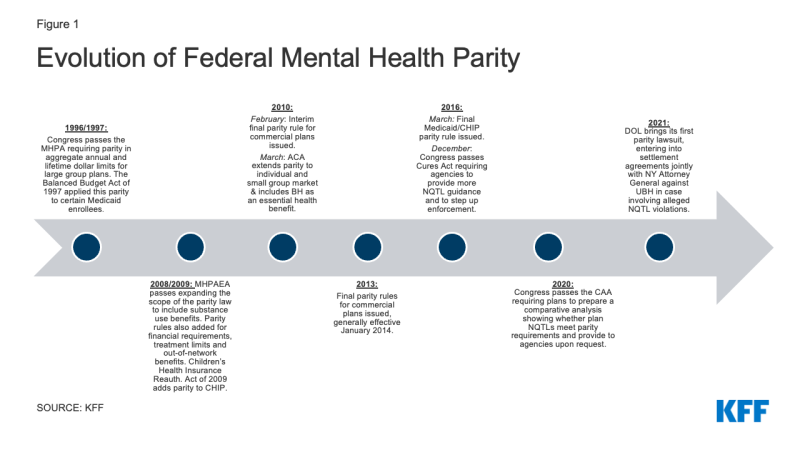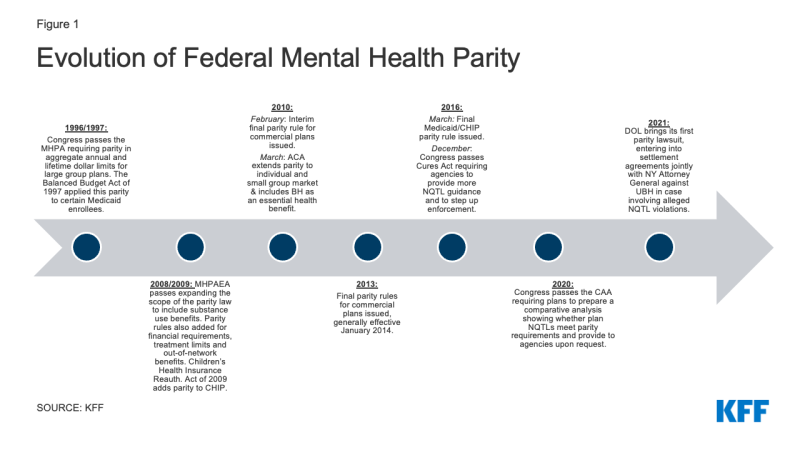
Figure 1: Evolution of Federal Mental Health Parity
| Topic |
Commercial |
Medicaid |
| Definition of behavioral health |
Plans define what is considered behavioral health versus medical care. |
State Medicaid agencies can define what is behavioral health versus medical care. MCOs, PHIPs and PAHPs must follow the state’s definition. |
| Long term care services |
Long term care services are considered “excepted benefits” that do not have to comply with parity. |
Long term care services generally must meet parity standards. |
| Out-of-network classifications |
Plans must evaluate parity for out-of-network inpatient care and out-of-network outpatient care. |
The two out-of-network classifications do not apply to Medicaid MHPAEA. |
| Network tiers |
Plans can determine parity separately for each provider network tier in a classification. |
Medicaid parity regulations do not give Medicaid plans with network tiers the ability to evaluate parity within each tier. Parity is evaluated for all care within a classification. |
| Cumulative Quantitative Treatment Limits |
Quantitative treatment limits (such as a limit on the number of visits for a service per year) cannot accumulate separately for behavioral health and medical. |
Quantitative treatment limits can accumulate separately for behavioral and medical services if certain standards are met. |
| Disclosure of reasons for denial of a claim |
Plans subject to ERISA must provide the denial reason in the form/manner included in ERISA claims review rules that are separate from commercial parity rules. NonERISA plans that follow this form and manner are deemed to comply with this parity requirement. |
Medicaid is subject to its own form/manner notice standards for providing the reason for a claim denial in adverse action notice regulations that are separate from Medicaid parity rules. |
| Cost exemption |
Plans can qualify for a temporary exemption from meeting the MHPAEA standards if they meet certain requirements for cost increases. |
Medicaid regulations do not apply the cost exemption to Medicaid. |
| SOURCE: 70 Federal Register 68240-68296; 80 Federal Register 18390-18445 |
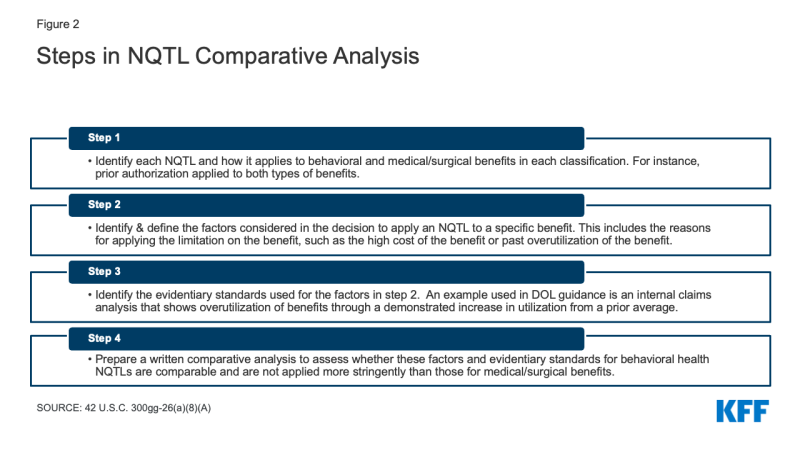
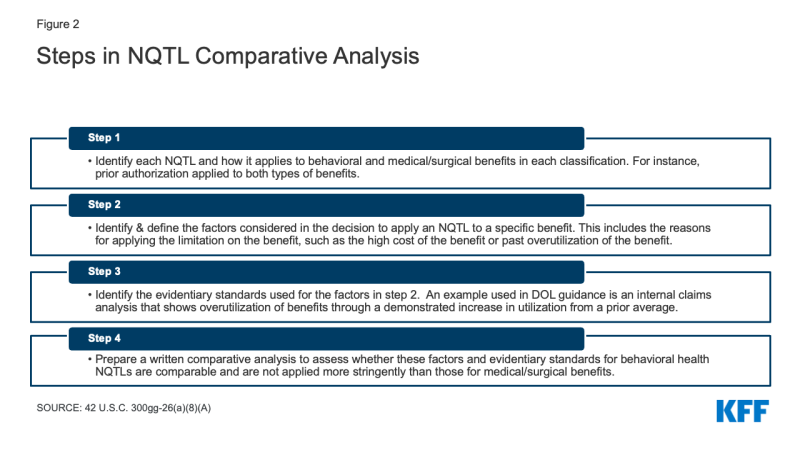
Figure 2: Steps in NQTL Comparative Analysis