Medicaid Home and Community-Based Services Programs: 2012 Data Update
Medicaid HCBS Participants and Expenditures in 2012
Participants in Medicaid Home Health and Personal Care State Plan Services and § 1915(c) Waivers
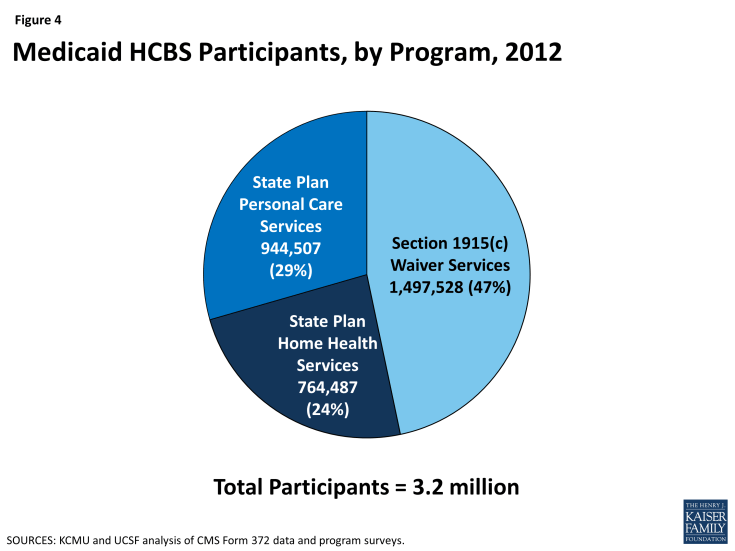
In 2012, over 3.2 million individuals received services through the three main Medicaid HCBS programs (Table 1A). Of those participants, 764,487 individuals received home health services through the mandatory state plan benefit, 944,507 individuals received personal care services through the optional state plan benefit, and 1,497,528 individuals were served through § 1915(c) waivers (Figure 4). All states and DC offered the mandatory home health services state plan benefit in their Medicaid programs (Table 1B), while 32 states actively offered the optional personal care services state plan benefit, with Kansas as the latest state to elect this option in 2007 (Table 1C). (Delaware and Rhode Island had approval from the Centers for Medicare and Medicaid Services (CMS) to offer personal care state plan services but did not report any participants in their programs.) Forty-seven states and DC operated multiple § 1915(c) waivers in 2012 (Table 1D).
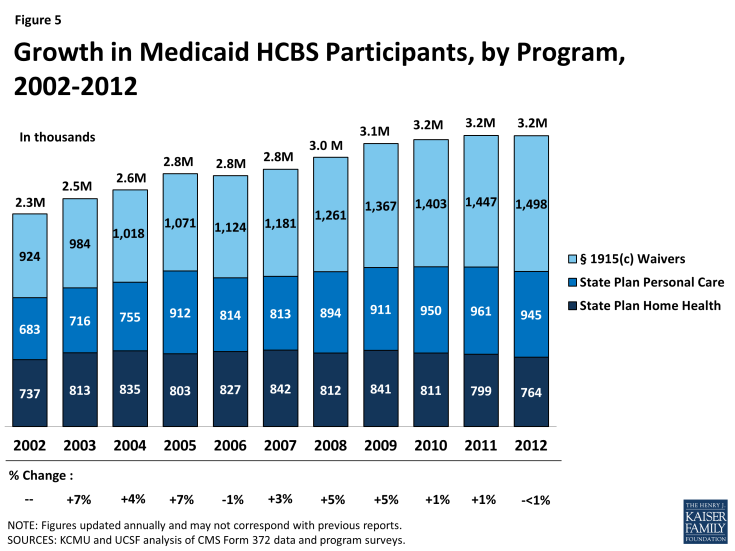
Participation in the three main HCBS programs declined by less than one percent between 2011 and 2012, the first annual decline since 2006, following two years of slight growth. This was also well below the 10-year average growth rate of three percent (Table 1A and Figure 5).
Leading the 13 states with a decline in total HCBS enrollment between 2011 and 2012 was Texas, with a 17 percent decline reported. Louisiana recorded the second largest decline with a 9 percent drop in total HCBS enrollment between 2011 and 2012 (Table 1A). Both Texas and Louisiana’s declines in total HCBS enrollment were led by a drop in their § 1915(c) waiver enrollment as the number of waivers declined in both states. Three waivers in Texas were terminated (one for people with I/DD and 2 for the aged/disabled population), while another was converted to a § 1115 Managed Care waiver in 2012. Louisiana terminated one large aged and disabled waiver. On the other hand, Idaho, Minnesota, and Maine saw the largest increases (27%, 15%, and 14%, respectively) in total HCBS participants in 2012. Idaho’s participant growth was driven by large increases in its two state plan programs while both Minnesota and Maine experienced relatively high participant growth in their home health programs.
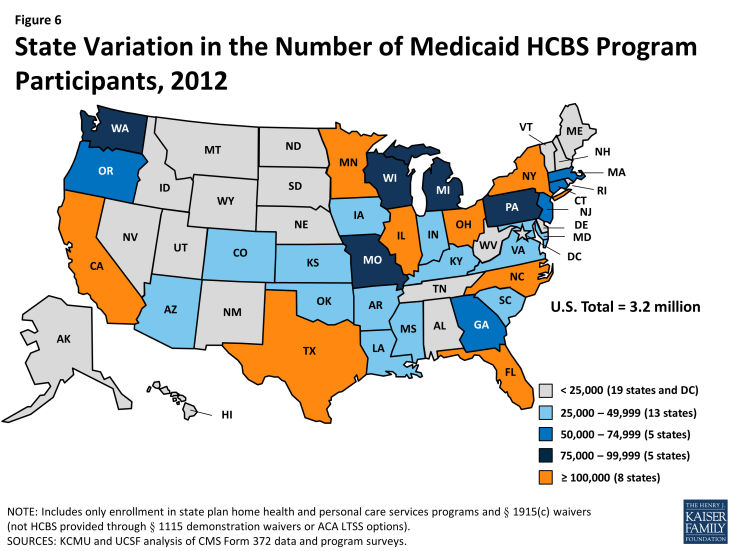
The decline in total HCBS enrollment in 2012 was led by declines in participation in both the home health state plan program (-4%) and in the personal care state plan services program (-2%) (Tables 1B and 1C). Nebraska led the decline in home health program enrollment with a 27 percent drop, due to a change in reporting when the state moved to managed care, while Maine led the decline in personal care state plan participation with a 33 percent drop in 2012, also due to a change in reporting. Nationally, § 1915(c) waiver program participation increased by three percent from 2011 to 2012, and seven states reported declines in participation led by Louisiana (-24%) and Texas (-19%) as noted above (Table 1D). Figure 6 illustrates the variation in total Medicaid HCBS program participation among the states.
Expenditures in Medicaid Home Health and Personal Care State Plan Services and § 1915(c) Waivers
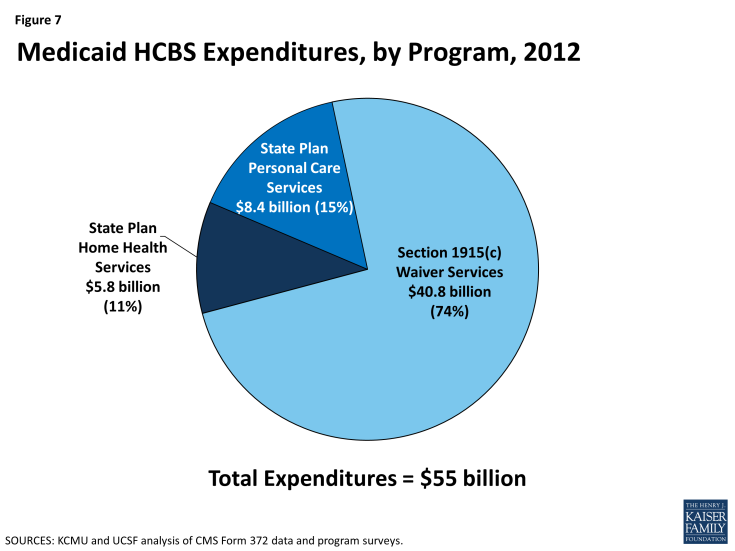
In 2012, total Medicaid spending on HCBS across the three main programs was $55 billion (Table 2A). The large majority of Medicaid spending on HCBS was for § 1915(c) waivers. In 2012, Medicaid spending on § 1915(c) waivers was $40.8 billion, compared to $8.4 billion on personal care state plan services and $5.8 billion on home health state plan services (Tables 2B, 2C, 2D and Figure 7).
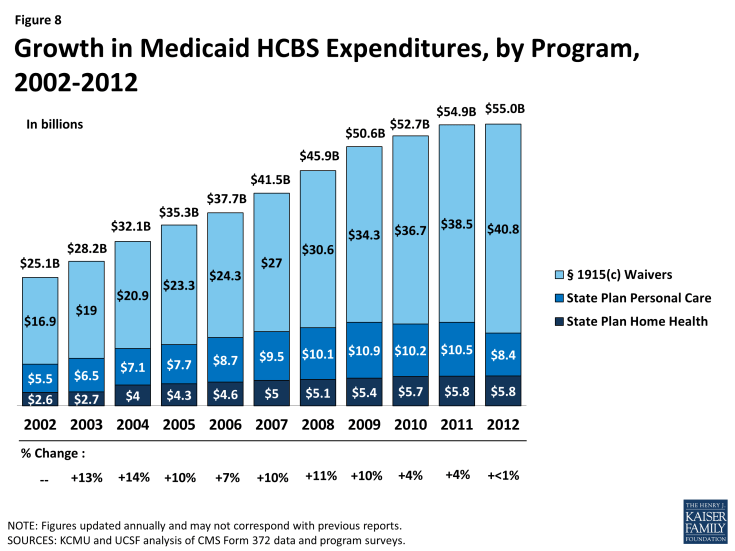
Between 2002 and 2012, total annual Medicaid spending on HCBS in the three main programs increased by almost $30 billion (119%) with an average annual increase of eight percent (Figure 8). HCBS spending recorded slight growth between 2011 and 2012, the lowest rate of growth within the 14-year study period. However, this low rate of growth in HCBS spending was still more than the decline of four percent recorded for total Medicaid acute and LTSS expenditures in the same period, which corresponded with a decline in total Medicaid spending growth.1 Amid the stagnant growth in HCBS expenditures, 11 states reported a decline in total Medicaid HCBS expenditures between 2011 and 2012. Declines were led by Texas and Wyoming (both -21%) (Table 2A).
However, Medicaid HCBS expenditures as a proportion of total Medicaid LTSS expenditures continued to increase between 2011 and 2012 as they have done every year since 1995.2
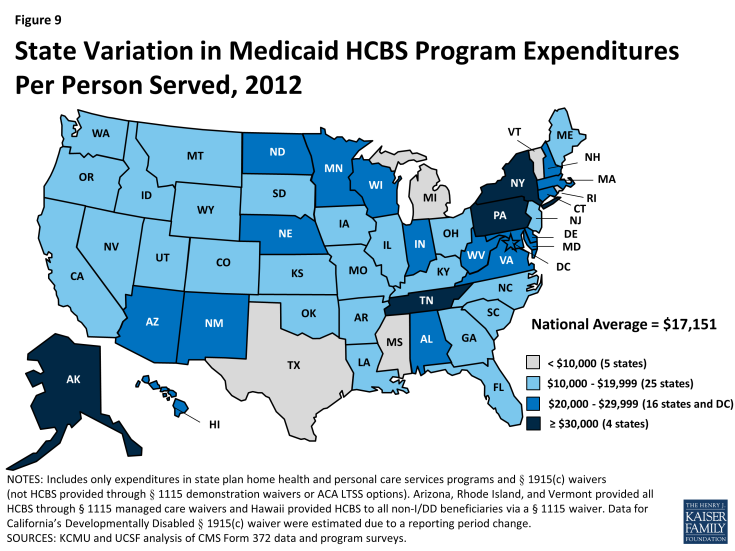
National total Medicaid HCBS expenditure data mask state-to-state variations in spending across the three major programs. First, while national per participant spending on Medicaid HCBS averaged $17,151 in 2012, state spending ranged from $8,787 in Mississippi to $42,556 in Tennessee (Figure 9, Table 3A).
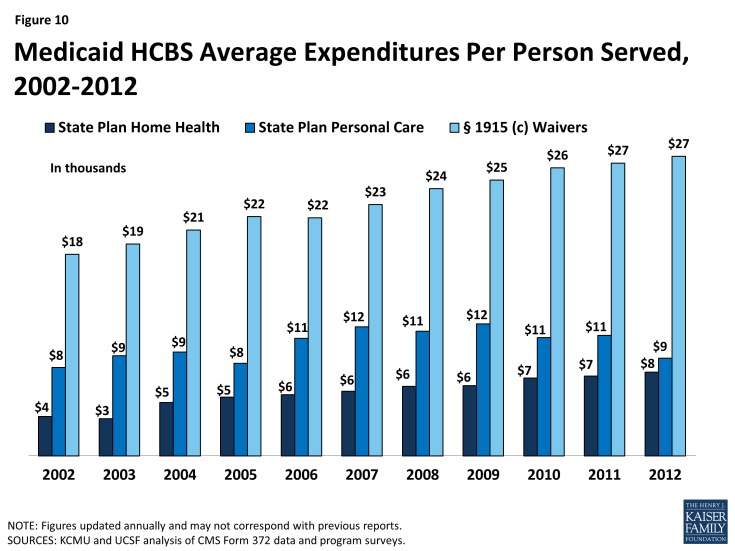
Second, differences exist in spending across the three major Medicaid HCBS programs. National per participant expenditures ranged from $7,617 for home health state plan services participants to $27,232 for § 1915(c) waiver participants in 2012 (Table 3B, 3C, 3D and Figure 10). This difference was likely due to the types and extent of services provided in each of the three main HCBS programs. The lower national per participant spending on home health state plan services likely reflects shorter periods of per participant service utilization compared to either § 1915(c) waivers or the personal care services state plan option. Third, there was also significant per participant expenditure variation among § 1915(c) waivers targeted to different populations (Tables 4 and 7).
Medicaid § 1915(c) Waivers
Between 2011 and 2012, the number of § 1915(c) waivers declined slightly to 290. In 2012, with the exception of Arizona, Rhode Island, and Vermont, which operate their entire Medicaid LTSS programs through § 1115 waivers and therefore do not offer any § 1915(c) waivers, every state and DC had § 1915(c) waivers targeted to populations that would otherwise require institutional care. These beneficiary groups include: the aged (age 65 and over), aged or disabled, individuals with physical disabilities, individuals with I/DD, children who are medically fragile or technology-dependent, individuals with HIV/AIDS, and individuals with traumatic brain and/or spinal cord injury (TBI/SCI).
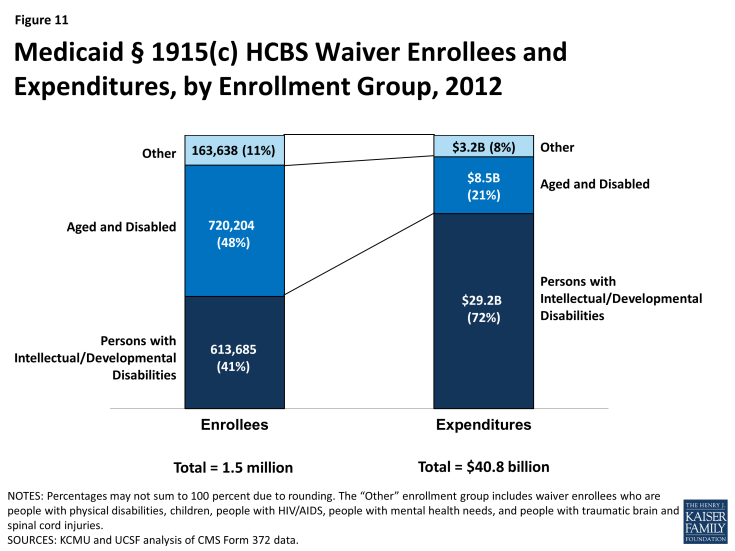
Table 4 details, by waiver type, § 1915(c) waiver enrollment, total expenditures, and per participant expenditures for the two most recent reporting years. In 2012, 1,497,528 participants were served through Medicaid § 1915(c) waivers (Tables 4 and 5). The three percent (or 50,147 beneficiaries) increase from 2011 to 2012 is the same rate of increase as between 2010 to 2011. The largest share of § 1915(c) waiver participants in 2012 (720,204 beneficiaries, or 48%) received services through waivers that targeted the aged and aged or disabled. The next largest group of waiver participants (613,685) was enrolled in § 1915(c) waivers for persons with I/DD, representing 41 percent of national § 1915(c) waiver enrollment (Table 5 and Figure 11). Enrollment in waivers targeted solely to persons with physical disabilities accounted for only six percent (87,017) of § 1915(c) waiver participants nationwide. The § 1915(c) waivers with the smallest enrollment were those for children who are medically fragile or technology-dependent (41,950), individuals with TBI/SCI (17,072), individuals with HIV/AIDS (13,538), and individuals with mental health disabilities (4,061) (Tables 4 and 5). The § 1915(c) waivers with the largest annual increase in participation were those targeted to people with mental health disabilities (12%), followed by those serving aged individuals (8%). There was a slight decline (less than 1%) in participants for waivers serving aged and disabled individuals, the only decline recorded among all waiver groups (Table 4).
In 2012, overall expenditures for § 1915(c) waivers increased to $40.8 billion, a six percent increase compared to 2011, and the same rate of increase as between 2010 to 2011. The vast majority of spending on § 1915(c) waivers was for individuals with I/DD. Although individuals enrolled in I/DD waivers accounted for just 41 percent of total waiver participants, expenditures for this population accounted for 72 percent of all § 1915(c) waiver spending (Tables 4 and 6 and Figure 10). Between 2011 and 2012, the annual rate of expenditure growth was highest for mental health waivers (15%), mainly due to growth in the five existing § 1915(c) waivers for persons with mental health disabilities. There was a four percent decline in expenditures on waivers serving aged and disabled individuals as well as a less than one percent decline recorded in waivers serving individuals with HIV/AIDS (Table 4).
Growth in § 1915(c) waiver expenditures per participant remained at two percent in 2011-2012, the same as the growth rate in 2010-2011, but lower than the 10-year average of five percent (Tables 4 and 7). Persons with I/DD had the highest spending per participant served ($47,522) (Tables 4 and 7). This amount was more than four times higher than average waiver spending on both aged ($11,490) and aged or disabled ($11,834) waiver participants (Tables 4 and 7). Per participant expenditures grew by eight percent from 2011 to 2012 for waivers serving children who are medically fragile or technology-dependent, with waivers serving the aged and disabled, physically disabled and persons with HIV/AIDS all showing slight declines in per participant spending (Table 4).
Medicaid § 1915(c) Waiver Services
As part of the collection of participant and expenditure data for § 1915(c) waivers, service type data were also collected for individual waivers. States may provide many different services within waivers, which have been collapsed into six categories here: (1) case management; (2) respite/home health/personal care; (3) habilitation/day care; (4) nursing/therapy; (5) residential/foster care; and (6) other services. Participants within a waiver may use more than one service, and, as such, the sum of these participants does not equal the unduplicated total waiver participants. Most participants received “other” services including assistance with chores, meals, transportation, and home modifications. More than 799,000 waiver participants received respite, home health or personal care services within waivers in 2011, with Ohio providing these services to the most waiver enrollees (75,334) (Table 8).
Of the total $40.8 billion spent on § 1915(c) waivers in 2012, almost 38% ($15.4 billion) was spent on habilitation or adult day care services, with New York spending more than $5 billion and Pennsylvania spending almost $1.5 billion. States spent more than $11.5 billion on respite, home health or personal care services within waivers, with Ohio spending almost $1.4 billion on such services (Table 9). The most expensive waiver service on a per participant basis in 2012 was habilitation or adult day care services, with more than $28,000 spent per waiver participant nationwide. There is large inter-state variation in habilitation or adult day care services spending per participant, ranging from $1,702 in Georgia to $59,387 in Connecticut. Case management was the least expensive § 1915(c) waiver service nationwide at $1,647 per participant (Table 10).
HCBS and Managed LTSS within § 1115 Waivers
In addition to the Medicaid home health and personal care services state plan benefits and § 1915(c) waivers, states can deliver HCBS through § 1115 demonstration waivers.3 Section 1115 of the Social Security Act allows the Secretary of the Department of Health and Human Services to waive state compliance with certain federal Medicaid requirements and authorizes the use of federal Medicaid funds in ways that are not otherwise allowable. Section 1115 waivers enable “experimental, pilot or demonstration project[s] which, in the judgment of the Secretary, [are] likely to assist in promoting the objectives [of the Medicaid program].”4 Section 1115 waivers have been used to implement a variety of initiatives related to HCBS, such as self-direction of personal care services,5 payments to spouses who provide personal care services, and managed LTSS.
In 2012, three states (Arizona, Rhode Island, and Vermont) use § 1115 waivers to administer statewide Medicaid capitated managed care programs that include all covered HCBS for all populations and services; these states do not offer any § 1915(c) waivers. In 2012, Arizona spent $1 billion on HCBS for 43,231 participants, Rhode Island spent $446 million on HCBS for 4,632 participants, and Vermont spent $247 million on HCBS for 3,675 participants.6 Vermont’s model is unique in that the state serves as the managed care entity. Other states that administer Medicaid managed care programs that include HCBS contract with private health plans to provide covered services for a capitated per member per month rate. In addition to Arizona, Rhode Island, and Vermont’s statewide programs, another five states7 (Delaware, Hawaii, New York, Tennessee, and Texas) use § 1115 waivers for Medicaid capitated managed care programs that include HCBS for at least some geographic areas and/or populations in 2012; these states also offer § 1915(c) waivers for other HCBS.8 Other states implement Medicaid managed LTSS programs through combination § 1915(b)/(c) waivers (Section 1915(b) waivers allow states to offer Medicaid services in a managed care model or otherwise limit a beneficiary’s choice of providers).9