Medi-Cal Managed Care: An Overview and Key Issues
Executive Summary
California’s Medicaid program, Medi-Cal, is the largest state Medicaid program in the nation, insuring almost one-third of California’s more than 38 million residents. In the early 1970s, California was the first state to enter into risk contracts with managed care plans to serve some Medicaid beneficiaries, rather than pay for services on a fee-for-service (FFS) basis. Over the decades since that time, Medi-Cal has been progressively moving more beneficiaries into managed care. More than three-quarters of all Medi-Cal beneficiaries, including low-income children, adults, seniors, and people with disabilities, are now enrolled in managed care plans. Besides being the earliest Medicaid managed care program and, by far, the largest in the nation, at nearly 10 million enrollees, the Medi-Cal managed care program has a unique structure, an outgrowth of underlying historical differences in the health care systems and traditions in different counties of the state. As other state Medicaid programs increase their use of risk-based managed care, and policymakers, plans and providers, and advocates seek to understand and learn from developments in this area to guide future change, a review of Medi-Cal’s managed care evolution is both timely and illustrative. It also serves to illuminate some potential implications of the proposed rule on Medicaid managed care issued by the federal Centers for Medicare & Medicaid Services (CMS) and expected to be finalized in the Spring of 2016, which represents a major overhaul of current regulatory requirements and standards.
A number of observations stand out from this review:
- County-based structure. California’s managed care program is unique, involving six different managed care models, shaped by the historical and continuing role of counties in financing and delivering primary care, public hospital services, mental health services, and certain long-term services and supports to poor and medically indigent residents. More than two-thirds of all Medi-Cal managed care enrollees are enrolled in public safety-net plans; the others are served by a mix of commercial and private non-profit health plans.
- Phased managed care expansion. In the early days of the state’s managed care program, in a limited number of counties, managed care enrollment was mandated for nearly all Medi-Cal beneficiaries, including seniors and people with disabilities. Over time, California has expanded mandatory managed care to additional counties and to broader segments of the beneficiary population, including seniors and people with disabilities statewide, under the state’s “Bridge to Reform” section 1115 waiver (2011); children who were transitioned from CHIP to Medi-Cal (2013); low-income adults covered previously through the state Low Income Health Program and those newly eligible for Medi-Cal under the ACA (2014); and, under the state’s seven-county Financial Alignment Demonstration and on a voluntary basis, beneficiaries dually eligible for Medicare and Medicaid (2014).
- Access to care. Problem with access to care in Medi-Cal FFS carry over into managed care, challenging Medi-Cal health plans to establish adequate provider networks and improve care. Gaps in access to certain specialists, including psychiatrists and other behavioral health providers, and long-term care services, are the most significant gaps. Providers have cited Medi-Cal’s low payment rates as a barrier to their participation in the program and sued the state on the basis that the fees violate federal Medicaid payment standards. Language and cultural gaps in access to care and gaps in rural access are additional issues.
- Benefit carve-outs. Medi-Cal managed care plans provide for most primary and acute care services. However, certain services are “carved out” from managed care contracts. In particular, while mental health services for mild or moderate mental illness are included in plan contracts, specialty mental health services and substance use disorder treatment continue to be delivered through county mental health departments and local and county alcohol and drug programs. In most counties, nursing home care and certain home and community-based services (HCBS) are also carved out of managed care.
- Managed long-term services and supports. In 2014, under its Coordinated Care Initiative in seven counties, California required all Medi-Cal beneficiaries, including dually eligible enrollees who were previously exempt from managed care, to enroll in a managed care plan to receive their Medi-Cal benefits, including nursing home and certain HCBS.
- Transitions for people with complex needs. California’s experience shows that robust transition planning is necessary to minimize disruptions in care for beneficiaries with complex needs who are required to move from FFS to managed care. Beneficiary and provider engagement, timely transfers of data, continuity of care protections, beneficiary information and navigation assistance, and coordination with carve-out services emerge as essential elements of sound transitions.
- Increasing focus on metrics, performance, and accountability. California has taken significant steps to improve the data reported by Medi-Cal managed care plans, which are needed for rate-setting, managed care monitoring, efforts to move to value-based purchasing. The state also established a managed care performance dashboard that makes plan-level quality and other data available to the public, increasing the program’s transparency and plan accountability.
- Major current issues. Two recent developments – CMS’ proposed modernization of the Medicaid managed care regulations and the approval of “Medi-Cal 2020,” the renewal of California’s section 1115 waiver – can be expected to bear on the Medi-Cal managed care program, by increasing plan- and state-level requirements and state oversight responsibilities, and by setting the stage for potential changes in the role and operation of managed care plans in a transforming health care delivery and payment system.
Issue Brief
California’s Medicaid program, Medi-Cal, is the largest state Medicaid program in the nation. Insuring almost one-third of California’s more than 38 million residents,1 Medi-Cal is a key source of health coverage in the state and the main source of coverage for low-income children, adults, and people with disabilities. It also provides wrap-around coverage for many elderly Medicare beneficiaries in the state.
For several decades, Medi-Cal has been transitioning away from a fee-for-service (FFS) payment and delivery system to one that relies on risk-based managed care. Under the FFS system, beneficiaries could see any provider who accepted Medi-Cal, and providers were reimbursed for each individual service or visit. Under managed care, the state contracts with health plans to deliver Medi-Cal benefits to enrollees in exchange for a monthly premium, or “capitation” payment for each enrollee. The plans are accountable for and at financial risk for providing the services in the contract.
California was the first state to pilot managed care in Medicaid, beginning in the early 1970s, and the Medi-Cal managed care program has a unique structure that grew out of the different health care delivery and financing systems in different counties of the state. Over time, California has transitioned progressively more Medi-Cal beneficiaries into managed care, and its program is, by far, the largest Medicaid managed care program in the nation, with nearly 10 million children, adults, seniors, and people with disabilities – or more than three-quarters of all Medi-Cal beneficiaries – enrolled in plans.
In its early managed care pilot programs, California awarded contracts to health plans to serve Medi-Cal beneficiaries in a specified county or service area. Over time, the Department of Health Care Services (DHCS), California’s Medicaid agency, expanded the reach of its managed care program to include additional counties. Later, as part of the “California Bridge to Reform Demonstration,” a Section 1115 waiver approved by CMS in November 2010,2 the state extended mandatory managed care to seniors and people with disabilities enrolled in Medi-Cal. California opted to expand Medi-Cal eligibility under the Affordable Care Act (ACA), greatly increasing the number of Medi-Cal beneficiaries overall and in managed care plans. As of July 2015, 77% of Medi-Cal beneficiaries were enrolled in Medi-Cal managed care plans,3 and in October 2015, over 10 million beneficiaries were enrolled in Medi-Cal managed care plans.4 In addition, DHCS has collaborated with the Centers for Medicare and Medicaid Services (CMS) to launch a demonstration program in seven large counties under which beneficiaries who are dually eligible for Medicare and Medicaid may enroll in capitated managed care plans that provide the full range of services covered by both programs, including managed long-term services and supports (MLTSS).
As other states increase their reliance on risk-based managed care to serve their Medicaid beneficiaries, this review of California’s transition to a largely managed care-based Medicaid program is both timely and informative for Medicaid’s many stakeholders. It also serves to highlight some potential implications for Medi-of CMS’ proposed rule on Medicaid managed care, a major overhaul of the current regulations that is expected to be finalized in the Spring of 2016.
Structure of Medi-Cal Managed Care Program
County-Based Managed Care Models
A distinguishing feature of Medi-Cal’s managed care program is that different managed care models operate in different counties (Figure 1), shaped strongly by the historical role of the counties in the financing and delivery of primary care, public hospital services, mental health services, and certain long-term services and supports to poor and medically indigent residents. In the 1980’s, the first Medi-Cal managed care programs began as County Organized Health System (COHS) plans, including the Health Plan of San Mateo and Santa Barbara Regional Health Authority, operating under Section 1915(b) waivers. COHS plans were created by counties, with mandatory enrollment for virtually all Medi-Cal beneficiaries in the county service area (including seniors and persons with disabilities) and with almost all Medi-Cal services covered. In the early 1990’s, Medi-Cal expanded its managed care program by adding more COHS plans (e.g., Partnership Health Plan serving Solano and Napa Counties, CalOptima serving Orange County, and Central California Alliance for Health serving Santa Cruz and Monterey Counties).
Medi-Cal Managed Care Models
County Organized Health System (COHS). A health plan created and administered by a County Board of Supervisors. Within a COHS county, all managed care enrollees are in the same plan. (22 counties)
Two-Plan Model. This model is comprised of a publicly-run entity (a “Local Initiative”) and a commercial plan. (14 counties)
Geographic Managed Care (GMC). In this model, DHCS contracts with a mix of commercial and non-profit plans that compete to serve Medi-Cal beneficiaries. (2 counties)
Regional Expansion Model. DHCS contracts with two commercial plans in each county. (18 counties)
Imperial Model. This model only operates in Imperial County where DHCS contracts with two commercial plans.
San Benito (Voluntary) Model. This model only operates in San Benito County where DHCS contracts with one commercial plan.
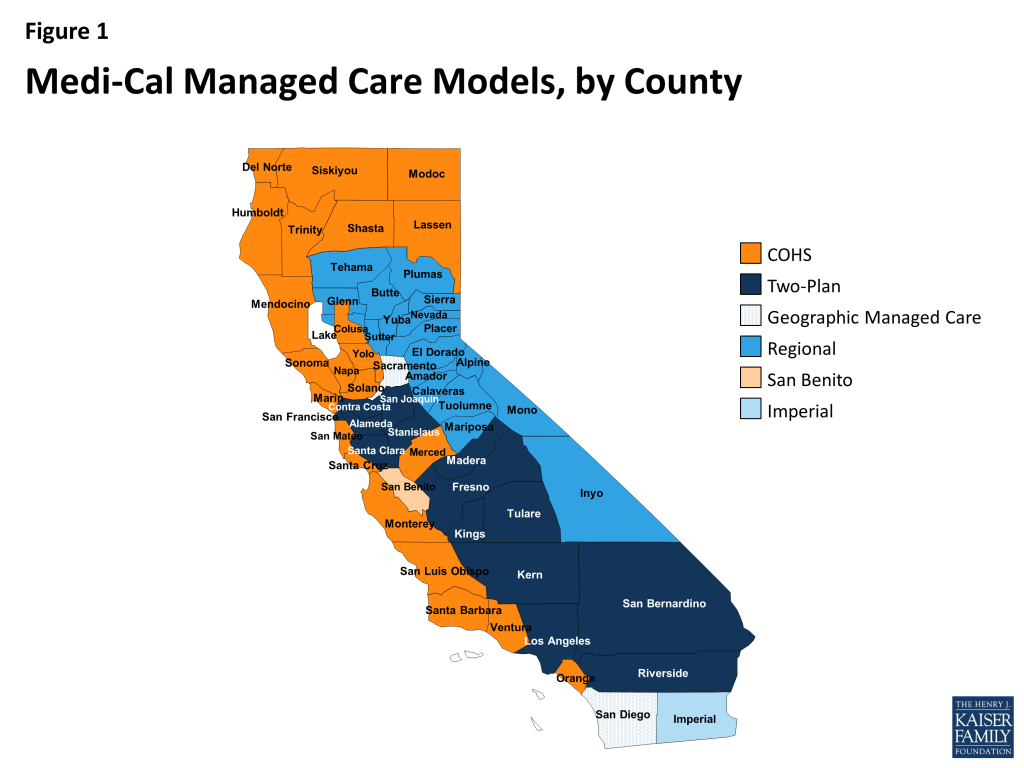
The state also created the Two-Plan Model, which was designed to shift large segments of the Medi-Cal population into managed care while preserving the role of traditional safety-net providers,5 and the Geographic Managed Care Model (GMC) in Sacramento and San Diego Counties. The Two-Plan Model offers enrollees a choice between one commercial plan and one “Local Initiative” public plan. Like COHS plans, Local Initiative plans are public entities and are expected to work collaboratively with county public hospitals and safety-net providers to support the safety-net delivery system. In general, Two-Plan Model counties tend to be ones with large Medi-Cal populations and public hospital systems critical to the safety-net; they include nine of California’s 12 public hospital health system counties6 .
Local Initiative plans enjoy strong local support and have generally secured a 65%-85% Medi-Cal market share, with commercial plans in their service areas playing a smaller role. Notably, although there is only one Local Initiative plan in each county, some of them subcontract with one or more commercial plans, effectively providing Medi-Cal enrollees in these counties with more than two plan options. For example, L.A. Care, the Local Initiative plan in Los Angeles County, subcontracts with Anthem Blue Cross, Care1st, and Kaiser Permanente, in addition to providing health plan services directly to enrollees.7
The GMC Model relies on a mix of commercial and non-profit health plans but does not include Local Initiative plans. Enrollees in GMC counties have more than two plan options.8 Like in COHS, enrollment in both the Two-Plan and GMC Models is mandatory for low-income adults and children, but, unlike in COHS, enrollment in the Two-Plan and GMC Models was initially voluntary for seniors and persons with disabilities, becoming mandatory in 2012.
Finally, the Regional Expansion, Imperial, and San Benito (Voluntary) Models were created when Medi-Cal began expanding managed care to rural areas in late 2013. Both the Regional Expansion and Imperial Models involve contracts with two commercial plans. When children in the Healthy Families Program – California’s Children’s Health Insurance Program (CHIP) – who were enrolled in Kaiser Permanente’s Healthy Families plan transitioned to Medi-Cal coverage in 2013, the state contracted with Kaiser Permanente in three Regional Expansion Model counties to ensure continuity of care for these children.9 The San Benito Model allows Medi-Cal enrollees in San Benito County to choose between FFS and the one contracted commercial plan.
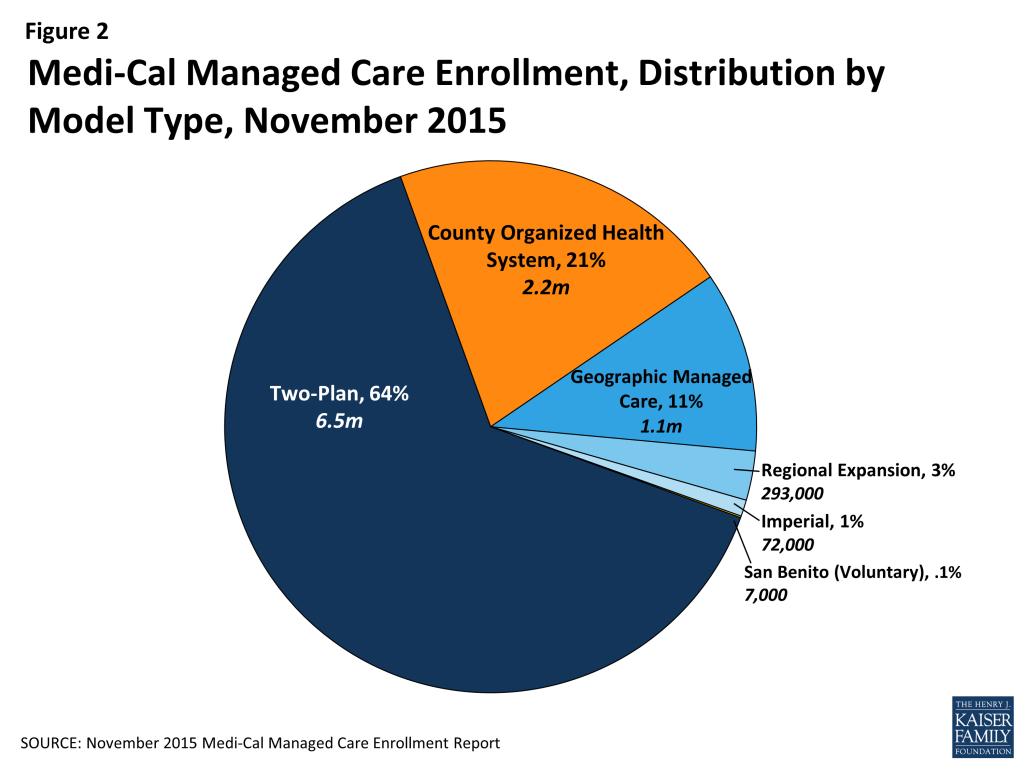
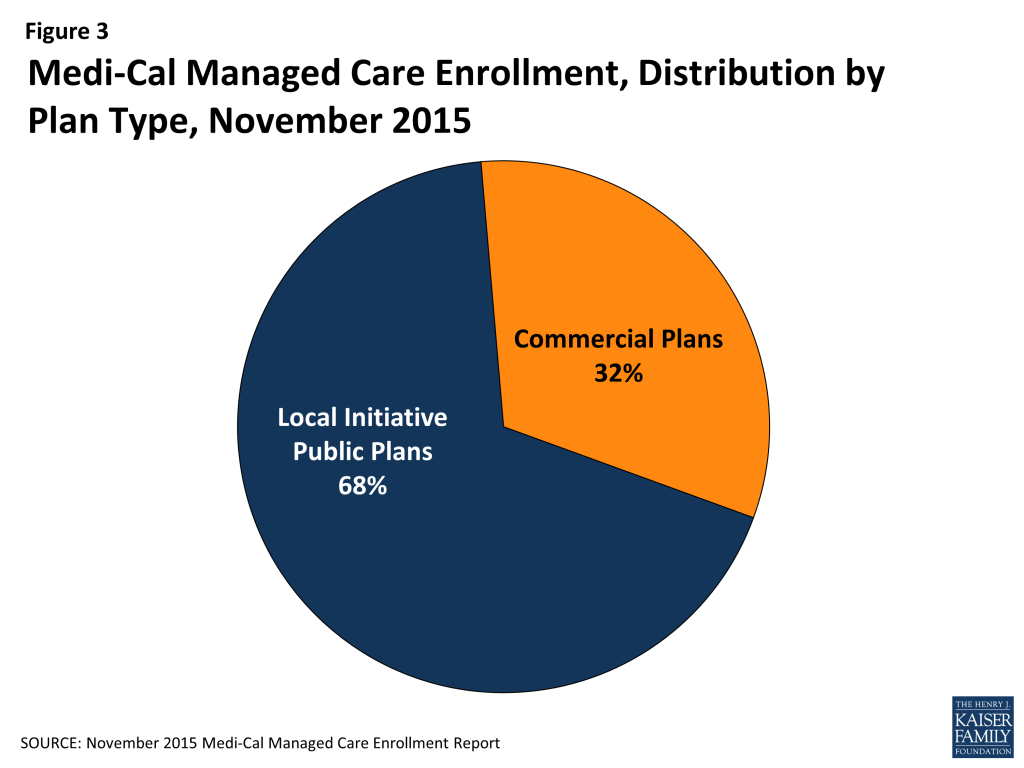
In all then, six different managed care models operate across California’s 58 counties today.10 Reflecting population distribution across the state, the largest share of Medi-Cal beneficiaries – nearly two-thirds as of October 2015 (64%) – were enrolled in the Two-Plan Model. Another 21% were enrolled in the COHS Model, and 11% were enrolled in the GMC Model (Figure 2). A large majority of Medi-Cal managed care enrollees (68%) were served through local public plans (COHS plans and Local Initiative plans under the Two-Plan Model), while about one-third were served through commercial plans (Figure 3).
Key Programmatic Dimensions of Medi-Cal Managed Care
· Managed Care Plan Enrollment
People can apply for Medi-Cal in several ways: by mail, in person, by phone through their County Social Services Office, or, since the launch of the ACA coverage expansions in 2014, online via the Covered California website (www.coveredca.com). Once their eligibility is determined, individuals are enrolled in Medi-Cal and issued a Benefits Identification Card. They then choose from two or more health plan options, or are auto-assigned to a plan if they do not select a plan. In COHS counties, a single plan administers Medi-Cal and all enrollees are mandatorily enrolled in that plan. In San Benito County, only one health plan is available and beneficiaries may enroll in that plan or choose to stay in Medi-Cal FFS.
· Primary Care Provider Selection
Upon enrollment in a health plan, beneficiaries choose a primary care physician (PCP) who is in the health plan’s network or, if they do not choose a PCP, the health plan will assign them one. Notably, California established special provisions regarding PCP selection for ACA Medicaid expansion adults in the 12 counties with public hospital health systems11 that previously served these adults through Low Income Health Programs12 (discussed below) and county indigent programs. As in other counties, Medicaid expansion adults in these counties either select or are automatically assigned by their health plan to a PCP. However, to maintain support for the county public hospital health systems, for the period January 1, 2014 through December 31, 2016, plans must auto-assign at least 75% of newly eligible adults who do not select a PCP to a PCP in the county hospital health system until the system meets its enrollment target or notifies the plan that it is at capacity. The required percentage drops to 50% beginning January 1, 2017.13 14
· Benefits and Carve-Outs
Medi-Cal covers comprehensive primary and acute care, behavioral health care, and long-term services and supports (LTSS) for beneficiaries. While most primary and acute care benefits for managed care enrollees are provided by the managed care plans, the following services are generally “carved out” and provided on a FFS basis:
- Dental care;
- Specialty mental health services, such as targeted case management, partial hospitalization, and outpatient and inpatient mental health services (delivered through county mental health departments, which are responsible for intake, triage, and treatment of people who meet specific eligibility criteria for serious mental illness);
- Substance use disorder treatment services (delivered by local and county alcohol and drug programs);
- In-Home Supportive Services, which include personal assistance and other services that enable seniors and persons with disabilities to live safely in their homes (administered by counties, except in the seven MLTSS counties, where these services are provided by the health plan);
- Home and community-based waiver services (HCBS), such as case management, continuing care nursing, day care, and respite services, for beneficiaries who would otherwise meet the functional eligibility criteria for institutional care (except in the seven MLTSS counties, where services authorized under the Multipurpose Senior Services HCBS waiver are covered by the health plan); and
- Skilled nursing facility services beyond 91 days (except in COHS counties and the seven MLTSS counties, where these services are provided by the health plan).
· Provider Network Adequacy and Other Access Standards
Except for most COHS plans, Medi-Cal managed care plans are licensed by the California Department of Managed Health Care (DMHC) and are subject to statutory and regulatory consumer protections, including network adequacy requirements.15 In addition, all DHCS contracts with health plans specify network adequacy standards. The COHS plans (except for the Health Plan of San Mateo) are exempt from statutory licensure requirements but are subject to the network adequacy requirements contained in their Medi-Cal contracts. (Appendix Table 1 describes network adequacy standards in Medi-Cal managed care. Appendix Table 2 describes standards for timely appointments in Medi-Cal managed care.)
Recent Medi-Cal Managed Care Expansions
To prepare for the implementation of the ACA coverage expansions in 2014, California applied for its “Bridge to Reform” Section 1115 demonstration waiver, which CMS approved in November 2010.16 This section 1115 demonstration waiver allowed the state to implement the Low Income Health Program, an expansion of county-based coverage programs for low-income adults, who would later become eligible for new ACA coverage options.). The waiver also allowed the state to pursue fundamental program changes intended to improve health outcomes and ensure the long-term financial sustainability of the Medi-Cal program. Mandatory enrollment of seniors and persons with disabilities (SPDs) in managed care was among these changes. Waiver amendments in subsequent years further expanded managed care to additional populations and geographic areas. Ultimately, over the period 2011-2014, California transitioned or enrolled almost 5 million Medi-Cal beneficiaries into managed care under authority provided by the Bridge to Reform waiver, including beneficiaries in rural counties; seniors and persons with disabilities; children previously covered by Healthy Families, the state’s Children’s Health Insurance Program (CHIP); individuals previously enrolled in the Low-Income Health Program; and adults newly eligible for Medi-Cal under the ACA.
· Seniors and Persons with Disabilities (SPDs)
Prior to 2011, California mandated managed care enrollment for seniors and persons with disabilities (SPDs) only in COHS counties. In all other managed care models, enrollment of seniors and persons with disabilities was voluntary. However, in 2011, after the Bridge to Reform waiver was approved, the state began to transition these beneficiaries, excluding those dually eligible for Medicare and Medicaid, into managed care in 16 additional counties that had managed care for other Medi-Cal populations at the time, and where managed care for seniors and persons with disabilities had previously been voluntary. During the 12 months beginning June 2011, nearly 240,000 SPDs were enrolled into managed care plans in these counties, where they were offered a choice of at least two plans. As California began to expand mandatory managed care to rural counties in 2013, SPDs in these counties were also enrolled in plans.17 As of September 2014, 647,968 seniors and persons with disabilities (non-dually eligible) were enrolled in Medi-Cal managed care, making up 7.7% of all Medi-Cal managed care enrollment statewide.18
· Children Enrolled in the Healthy Families Program
Starting in 2013, children enrolled in the Healthy Families Program were moved into Medi-Cal. This change was intended to simplify eligibility and coverage for children and families; improve children’s coverage through retroactive eligibility, increased access to vaccines, and expanded mental health benefits; and eliminate premiums for lower-income children in the Healthy Families Program.19 The shift was also expected to produce budget savings for the state, as average rates paid to Medi-Cal plans were generally lower than those paid under the Healthy Families Program for a largely equivalent benefit package (after adjustments for carve–outs).20 DHCS identified approximately 750,000 children eligible to be transitioned to Medi-Cal; the transition was implemented in four phases to minimize service disruptions and ensure continued access to care.21
· Adults in Low Income Health Program and Newly Eligible Adults under the ACA
Through the Low Income Health Program (LIHP), county and local entities strengthened their primary and specialty care delivery systems, implemented primary care medical homes, and enrolled over 630,000 uninsured adults ages 19-64 with incomes up to 200% of the federal poverty level in coverage. On January 1, 2014, all but 24,000 LIHP enrollees (whose incomes qualified them instead for subsidies for Marketplace plans) became eligible for Medi-Cal under the ACA Medicaid expansion and were enrolled in managed care plans.
Recently Added Services in Managed Care
Since 2011, California has expanded the benefits covered under managed care contracts through amendments to its Bridge to Reform waiver. The services added include adult day health services, mental health services and, in seven demonstration counties, certain long-term services and supports, as further described below.
· Community-Based Adult Services (CBAS) Benefit
Prior to 2011, Adult Day Health Care (ADHC), a community-based day care program that provided health, therapeutic, and social services for persons at risk of nursing home placement, was offered as an optional Medicaid State Plan service on a FFS basis. To achieve budget savings, Governor Brown’s January 2011 budget plan proposed to eliminate the ADHC benefit, and in March 2011, the state legislature voted to eliminate the ADHC benefit, subject to CMS approval (which was delayed until April 2012).22 In August 2011, DCHS began transitioning ADHC participants from FFS to managed care plans, which were to coordinate their medical and social support needs. Later, under a settlement with the ADHC providers, the Community-Based Adult Services (CBAS) benefit — utilizing the same ADHC providers — was created to replace ADHC as a managed care benefit only. In effect, the former ADHC benefit was carved into managed care as the new CBAS benefit. Accessible only to managed care enrollees, Community-Based Adult Services became the first community-based LTSS managed care plan benefit. Currently, CBAS providers serve 31,000 managed care enrollees statewide.
· Managed Long-Term Services and Supports (MLTSS)
In January 2012, Governor Jerry Brown proposed his Coordinated Care Initiative (CCI), aimed at improving health outcomes and beneficiary satisfaction for low-income seniors and persons with disabilities, while achieving substantial savings from rebalancing the delivery of long-term services and supports toward home and community-based care.23 The CCI proposal was enacted by the state legislature in 2012 to be implemented in seven counties in 2014.24 One component of the CCI was a mandatory managed long-term services and supports (MLTSS) program. The second component, a demonstration program for persons dually eligible for Medicare and Medicaid, is described later.
In the seven CCI counties, Medi-Cal beneficiaries, including dually eligible enrollees who were exempt from managed care before 2014, are required to enroll in a managed care plan to receive their Medi-Cal benefits, including the following long-term services and supports: consumer-directed In-Home Supportive Services, Community-Based Adult Services, the Multipurpose Services and Supports Program (the state’s HCBS waiver services for frail elders), and long-term (over 91 days) skilled nursing facility services. Other HCBS waiver services (such as those under the state’s Assisted Living waiver and the waiver for persons with intellectual and developmental disabilities) remain carved out. MLTSS coverage began on April 1, 2014. As of October 2015, over 300,000 dually eligible beneficiaries were enrolled in the MLTSS program in the seven counties.
· Mental Health Services and Autism Care
In 2014, mental health services for mild or moderate mental illness were added to managed care contracts (specialty mental health services continue to be carved out and provided through the counties). Also, in 2015, behavioral health therapy for beneficiaries with autism or autism spectrum disorder was added as a Medi-Cal-covered benefit and will be covered by managed care plans in 2016.
Other Managed Care Initiatives
Dual Eligible Demonstration
As mentioned earlier, the seven-county CCI also provided for a three-year Financial Alignment Demonstration (“Dual Demonstration”), as authorized by the ACA to promote coordinated health care delivery for individuals dually eligible for Medicare and Medicaid. Under the demonstration, called “Cal MediConnect,” dually eligible enrollees can elect to receive all of their Medicare and Medicaid services, including medical, behavioral health, and institutional and home and community-based long-term services and supports, through a single managed care plan. Plan participation in the Dual Demonstration is limited to Medi-Cal plans already serving the area. Participating plans contract with other entities to provide some services, such as behavioral health and In-Home Supportive Services, although the goal is that dually eligible beneficiaries receive all their care in a single, organized delivery system. A Memorandum of Understanding (MOU) between the state and CMS authorizing the Dual Demonstration outlines its principles and operational plan.25
The Dual Demonstration puts many new demands on Medi-Cal health plans, including the requirement to cover Medicare Part A, B, and D benefits as well as Medi-Cal long-term services and supports. To accomplish this, plans must organize providers who have not previously contracted with managed care plans or who have not previously provided services to Medicare beneficiaries. Under the Dual Demonstration, plans are also subject to specific and detailed DHCS and CMS contract requirements to maintain continuity of care, perform health risk assessments, and use person-centered, interdisciplinary care management teams. Enrollment in the Dual Demonstration is voluntary; as of December 1, 2015, 115,743 dually eligible enrollees – about one-quarter of the eligible population – were enrolled in it.26
Managed Care Data Initiatives and Dashboard
In late 2012, DHCS initiated the statewide Encounter Data Improvement Project (EDIP). The goal of the EDIP is to improve the timeliness, accuracy, and completeness of encounter data reported by managed care plans, to improve rate-setting and managed care monitoring, and to prepare for value-based purchasing. As part of the project, DHCS develops performance metrics and works with managed care plans to address their data collection and reporting deficiencies. This collaborative effort on data and metrics is critical in connection with performance reporting and will be foundational to value-based purchasing in the future.
To increase transparency regarding the quality of managed care plans, DHCS has created a Managed Care Performance Dashboard that provides plan-reported data on a variety of measures to help DHCS and other stakeholders examine and understand managed care activity and performance at the state level, by managed care model, and at the individual plan level. The dashboard contains metrics related to enrollment, enrollee health care utilization, appeals and grievances, and quality of care. The dashboard stratifies the plan-reported data by beneficiary population.27
Key Challenges and Lessons
Access to Care
Provider payment rates and participation. Managed care plans are required to maintain adequate provider networks and capacity to ensure access to care for their members. Historically, Medi-Cal FFS payment rates have been among the lowest Medicaid fees in the nation.28 Research has shown a positive relationship between fee levels and physician participation in Medicaid.29 30 31 In managed care, although provider payment rates are a contractual matter between plans and providers, the role of persistent low rates in depressing provider participation and beneficiary access continues to be a major issue. California providers have sued the state on the basis that Medi-Cal rates violate the “equal access” provision of federal Medicaid law.32 33 This provision requires that payment rates be “consistent with economy and efficiency… and sufficient to enlist enough providers so that care and services are available under the plan at least to the extent that such care and services are available to the general population in the geographic area.”34 On November 2, 2015, CMS issued a final rule implementing the equal access provision, which requires states to conduct access reviews on a regular basis and to consider the findings from those reviews in setting provider rates. However, CMS limited application of the latter requirement to FFS rate-setting, stating that standards for capitation payment rates are set in the June 1, 2015 proposed rule on Medicaid managed care.35
Data from a 2012 survey of Medi-Cal enrollees show that the vast majority of beneficiaries found it easy to find a provider who accepted Medi-Cal, but almost 1 in 5 enrollees had difficulty. Fewer than half of Medi-Cal enrollees said it was easy to find a specialist or mental health provider who accepted Medi-Cal; enrollees in fair or poor health were particularly likely to report difficulty finding specialists.36 A separate analysis, based on national survey data, found that Medi-Cal adults were significantly more likely than adults with Medicaid in other states not to have a doctor visit (37% vs. 30%) or a specialist visit (48% vs. 36%) and to delay care because of difficulty getting an appointment.37 Along with medical groups and other physicians, federally qualified health centers (FQHCs) and community clinics play an important role in providing primary care for Medi-Cal beneficiaries, but arranging specialist referrals for patients in these settings is an ongoing challenge.
A recent federal report shows that 54% of office-based physicians in California were accepting new Medicaid patients in 2013, compared to nearly 69% of office-based physicians nationally who were doing so.38 A 2013 California survey of physicians, including facility-based physicians, found a higher rate overall — 62% accepting new Medi-Cal patients, compared to 75% for Medicare and 79% for privately insured patients.39 The rate was 70% among pediatricians, but just over 50% among other primary physicians. Facility-based specialists were mostly likely to accept new Medi-Cal patients, and only 36% of psychiatrists did so. In June 2015, the California State Auditor issued a report identifying major gaps in state oversight of Medi-Cal plan provider networks to ensure their adequacy, a high volume of unanswered calls to the office of the Medi-Cal managed care ombudsman, and inconsistent monitoring of Medi-Cal plans to ensure they meet Medi-Cal beneficiaries’ medical needs.40
Linguistic and cultural gaps in access. Another challenge in Medi-Cal is the lack of linguistic and cultural concordance between the current provider workforce and the low-income population in California. A 2013 analysis by the state showed that 40% of Californians eligible for Medi-Cal reported a language other than English as their primary language and that 13 languages met the state’s definition of a “Threshold Language” spoken at a high proportional rate within a geographic area.41 A separate study documented that nearly 40% of all Californians and approximately 50% of Medi-Cal beneficiaries are Latino, but that only 5% of licensed physicians in California are Latino and only 6% of California physicians speak Spanish.42
Rural areas. While access to care is generally sufficient in most urban areas, securing access to care in rural areas is more challenging for publicly and privately insured patients alike. FQHCs, rural health centers (RHCs), and other health clinics form the backbone of the ambulatory care delivery system serving low-income populations in rural counties, and these safety net provider play an increasingly critical role in Medi-Cal managed care networks in rural as well as other areas of the state.43
Transitions to Managed Care
California’s shift of seniors and people with disabilities from FFS to managed care yielded important lessons about the importance of appropriate planning to foster smooth transitions and avoid disruptions in care, especially for people with complex health care needs.
Stakeholder engagement. Robust stakeholder engagement is needed to support smooth managed care transitions.44 In implementing the Healthy Families and Low Income Health Program transitions and the Dual Demonstration, DHCS increased its engagement with beneficiaries, advocates, providers, and plans. For example, in the Dual Demonstration, the state held extensive webinars, workshops, and stakeholder meetings, which state officials said resulted in better and more effective outreach.45 DHCS also established a dedicated webpage to report on all meetings, updates, and notices.
Data issues. In the SPD transition, inaccurate enrollee contact information, privacy rules that prevented plans and providers from accessing beneficiary medical records, and other data problems made timely implementation of care coordination challenging for Medi-Cal plans. The state was able to improve its data-sharing processes in the Dual Demonstration to give plans more time to contact incoming enrollees and prepare for their needs. Still, contacting beneficiaries to complete health assessments to support care management remains a challenge for plans, particularly in the case of individuals newly eligible for Medi-Cal and people without stable addresses.
Continuity-of-care protections. SPDS were permitted to request continued access to an out-of-network provider for 12 months following their plan enrollment.46 However, lack of plan, provider, and beneficiary understanding of this provision led to unnecessary disruptions in established patient-provider relationships. In subsequent managed care transitions, DHCS and plans increased their engagement with enrollees and providers to improve understanding of the continuity-of-care protection. DHCS also incorporated specific continuity-of-care requirements in its managed care contracts.
Enrollment processes. In the lead-up to the Dual Demonstration, advocates and plans urged greater transparency in the enrollment process and beneficiary protections, including the right to opt out of or disenroll from the Demonstration. In response, the state published the enrollment schedule and the mailing dates for notices to beneficiaries, to help advocates and insurance assisters prepare and stage beneficiary outreach and education efforts. The state also published issues that arose in the beneficiary notice/enrollment process and the steps the state took to address them. Advocates and plans also worked with DHCS to improve the managed care enrollment process for beneficiaries with LTSS needs and dually eligible beneficiaries.
Coordination with carve-out services. Coordination between plan and carve-out services is an ongoing challenge. This came up in the SPD transition, particularly in the context of mental health care, as prescription drugs were provided by plans, while specialty mental health services were carved out and provided by county mental health departments.47 In the MLTSS transition, plan coordination with waiver services that remained carved-out was also difficult. Differences between waiver service care managers and health plans in their assessments of beneficiary needs and care goals can create access barriers for beneficiaries.
Improving Quality
Performance measurement and monitoring. Managed care contracting enables states to measure and require accountability for quality. Through its contracts, California requires Medi-Cal managed care plans to periodically submit various quality-related reports, including Consumer Assessments of Healthcare Providers and Systems (CAHPS) survey findings, Healthcare Effectiveness and Data Information Set (HEDIS) scores, reports on member complaints, grievances, and resolutions, and other statistical reports.
Transparency. DCHS collection and monitoring of quality data and the public availability of data on plan performance in the Managed Care Performance Dashboard strengthen the foundation for state oversight of managed care, transparency of plan quality, and value-based purchasing strategies. DHCS works with Medi-Cal plans to improve its quality measures and refine its enforcement mechanisms. This work includes developing corrective action plans to improve plans’ quality reporting and outcomes and reporting formats that capture data accurately and completely. DHCS also conducts an annual quality forum to publicly recognize plans for their progress and achievements in quality performance. Poor-performing plans may be subject to enforcement actions or corrective action plans, or may lose out under the state’s auto-assignment algorithm.
Special reports for Dual Demonstration plans. All plans participating in the Dual Demonstration must submit additional reports to CMS that include data on quality metrics for both Medi-Cal and Medicare services. DHCS and CMS review these reports and work with the plans to ensure that data are reported consistently to support evaluation purposes. DHCS recently published the first quarterly Health Risk Assessment Dashboard, which compares the plans’ compliance with the requirement to complete Health Risk Assessments for Dual Demonstration members.48
Major Current Issues
Medicaid Managed Care Rule
CMS’ proposed rule on Medicaid managed care would modernize and fundamentally redraw the current regulatory framework for managed care. It would strengthen beneficiary protections and network adequacy requirements, establish requirements to increase the fiscal integrity of capitation rates, address health care delivery and payment reform in managed care, increase state and plan accountability for access and quality, and strengthen oversight of Medicaid managed care programs.49 If these provisions are preserved in the final rule, expected in the Spring of 2016, they could have significant bearing on provider networks and beneficiary access to care, provider payment, and other issues in the Medi-Cal managed care program.
In a letter to CMS submitted during the public comment period on the rule, the California Hospital Association expressed support for the overall direction of the rule and many of its specifics, but also identified some major concerns. Chief among them is the concern that the rule’s proposed limitations on states’ ability to direct plan expenditures and plan payments to specific providers would interfere with current supplemental payments targeted to certain hospitals– typically, safety-net and public hospitals that serve large numbers of Medicaid beneficiaries.50 The letter to CMS also commented on many other provisions of the proposed rule, recommending stronger standards in some areas and increased flexibility in others, and stressing the need for adequate state resources to audit and enforce the regulatory standards.
Section 1115 Waiver Renewal
California’s Bridge to Reform demonstration waiver expired on October 31, 2015. DHCS applied for a five-year extension of the waiver under the name “Medi-Cal 2020” and, on December 30, 2015, the terms of that waiver were announced. Among the key components of the waiver is the Public Hospital Redesign and Incentives in Medi-Cal (PRIME) fund, a pool of up to almost $7.5 billion in combined federal and state spending over the five-year waiver period for delivery system reform in California’s public hospital systems. The PRIME pool builds off the Delivery System Reform Incentive Program (DSRIP) included in California’s original waiver. DHCS will use it to fund public provider system projects to change care delivery and strengthen the ability of these systems to be paid under risk-based alternative payment models (APMs) that hold providers accountable for quality and the cost of care. The waiver documents state that CMS and the state will measure the success of PRIME, in part, by assessing the progress in moving to APMs for designated entities through Medi-Cal managed care.51 It remains to be seen exactly how the DSRIP and PRIME pools will interact with the Medi-Cal managed care program and what the implications will be for plans and their Medi-Cal members.
Medi-Cal 2020’s “Whole Person Care Pilots,” intended to provide more integrated care for vulnerable, high-utilizing beneficiaries, also involve Medi-Cal plans. In these county-based pilots, Medi-Cal managed care plans, safety-net providers, and other community-based service providers and affordable housing providers, are expected to develop innovative partnerships to address social determinants of health as well as integrate physical and behavioral health care and improve beneficiary health and well-being.
Looking Ahead
In the short time from 2011 to 2015, California expanded managed care to 28 rural counties, transitioned or enrolled almost 5 million beneficiaries into managed care, carved adult day health and mental health services into managed care, and, in seven counties, launched a managed long-term services and supports program and a Dual Demonstration. Currently, Medi-Cal managed care plans operate in all 58 counties in California and cover over three-quarters of all Medi-Cal enrollees. To absorb the influx of new members, including many with complex care needs, Medi-Cal plans have been challenged to expand their provider networks and reinforce their operations rapidly to handle increased demand for services, increased demand on call centers, and utilization management, care management, quality improvement, and claims processing on a larger scale. In addition, the state has been challenged to provide adequate notice and education to enrollees transitioning to managed care and to ensure that health plans receive data on a timely basis.
Other states considering managed care expansions – especially, expansions to Medicaid populations with more complex care needs – can learn from California’s experience. Managed care is unlikely to solve longstanding access problems attributable to systemic provider shortages and/or low Medicaid payment rates and limited provider participation. As states expand their managed care programs to more Medicaid beneficiaries, including those with high needs, ensuring that plan networks are adequate to serve their enrollees could be more challenging for both plans and states. Robust transition planning is essential to minimize disruptions in care when states mandate that new groups of FFS beneficiaries enroll in managed care plans. Engaging beneficiaries, providers, consumer advocates, and other stakeholders in this planning process and its implementation is necessary to ensure that beneficiaries know how to navigate their plans to obtain needed services and assistance and are fully informed about their rights and options. Data-sharing systems and procedures to support managed care transitions, and information systems and data analytics capacity to support ongoing monitoring, oversight, and performance improvement are integral to both plan and state accountability for Medicaid managed care programs.
California, like many other states, is increasingly oriented toward achieving better performance from its managed care contractors. Key areas of focus include further delivery system transformation to improve care while reducing costs; enhanced care integration; expansion of managed long-term services and supports; transparency regarding health outcomes of managed care enrollees; and improving population health. To meet these challenges, managed care plans will need to develop new ways to engage beneficiaries, partner with community-based social services and supportive housing organizations, and structure provider payment models to promote health care quality and outcomes – all in the context of limited federal and state funding. Finally, if, as managed care evolves in new ways, its potential to provide more coordinated and integrated care is to be optimized and gaps in access are to be minimized, close state monitoring of managed care plans and rigorous enforcement of federal and state managed care requirements will continue to be essential.
The authors wish to acknowledge valuable input and assistance from Michael Engelhard, Donna Laverdiere, and Lisa Shugarman, all of Health Management Associates.
Appendix
| Appendix Table 1: Network Adequacy Standards in Medi-Cal Managed Care | ||
| Knox-Keene Act Standardsa | Medi-Cal Two-Plan and GMC Contract Standardsb | COHS Contract Standardsb |
| General Requirements | ||
| Comprehensive range of primary, specialty, institutional, and ancillary services readily available at reasonable times to all enrollees. | Maintain network adequate to serve 60% of all eligible beneficiaries within the service area and provide full scope benefits. Ensure appropriate provider network, including PCPs, specialists, and other personnel and an adequate number of inpatient facilities within the service area. | Submit a complete provider network adequate to provide covered services to eligible beneficiaries within the service area. Increase capacity of the network to accommodate growth. |
| Time and Distance Standards | ||
| Primary care and hospital services must be available within 30 minutes or 15 miles of enrollee’s residence or workplace. Laboratory, pharmacy, and similar services available at locations within a reasonable distance from PCP. | Maintain a network of PCPs located within 30 minutes or 10 miles of a member’s residence unless MCO has an approved alternative standard. | Maintain a network of PCPs located within 30 minutes or 10 miles of a member’s residence unless MCO has an approved alternative standard. |
| Provider-to-Enrollee Ratios and Other Access Standards | ||
| · PCPs: 1: 2,000 · Total physicians: 1: 1,200 · Complete network of PCPs and specialists with admitting staff privileges at least one contracting hospital equipped to provide range of basic health care services · Emergency 24/7 · Access to medically required specialists | · PCPs: 1: 2,000 · Total physicians: 1: 1,200 · Non-physicians not to exceed provider/patient caseload of 1: 1,000 · Emergency services 24/7 · Adequate number and type of specialists | · PCPs: 1: 2,000 · Total physicians: 1: 1,200 · Non-physicians not to exceed provider/patient caseload of 1: 1,000 · Emergency services 24/7 · Adequate number and type of specialists
|
| a Title 28, California Code of Regulations, §1300.51.H and §1300.67.2.b COHS Boilerplate Contract and Two Plan Boilerplate Contract, available at http://www.dhcs.ca.gov/provgovpart/Pages/MMCDBoilerplateContracts.aspx | ||
| Appendix Table 2: Timeliness Standards for Appointments in Medi-Cal Managed Care | |
| Type of Appointment | Standard for Timeliness |
| Urgent care, no prior authorization | 48 hours* |
| Urgent care, prior authorization | 96 hours |
| Non-urgent primary care | 10 business days of request |
| Specialist care | 15 business days of request |
| Non-urgent ancillary services for diagnosis or treatment of injury, illness, or other health condition | 15 business days of request |
| First prenatal visit | 10 business days |
| Urgent dental care | 72 hours |
| Non-urgent dental care | 36 business days |
| Preventive dental care | 40 business days |
| * The COHS contract has a more stringent urgent care provision that requires that a member needing urgent care be seen within 24 hours. | |
Endnotes
- Cite to new SHFO CPS data once posted. ↩︎
- Most of the state’s Medi-Cal managed care programs were included in the California “Bridge to Reform” Section 1115 waiver amendment effective for the 2010 – 2015 time period. The waiver amendment also expanded the managed care programs to include seniors and persons with disabilities, expanded managed care to additional counties, and added benefits. California Bridge to Reform Section 1115 Demonstration Fact Sheet, Updated August 2015. Accessed at http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ca/ca-bridge-to-health-reform-fs.pdf ↩︎
- See https://modern.kff.org/medicaid/state-indicator/managed-care-penetration-rates-by-eligibility-group/ ↩︎
- Medi-Cal Managed Care Enrollment Report, October 2015, available at http://www.dhcs.ca.gov/dataandstats/reports/Documents/MMCD_Enrollment_Reports/MMCEnrollRptOct2015.pdf ↩︎
- Medi-Cal Managed Care, Medi-Cal Facts No. 8, March 2000, Medi-Cal Policy Institute, a project of the California Health Care Foundation. Accessed at http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/PDF%20M/PDF%20mmc2.pdf ↩︎
- California’s 12 public hospital health system counties are: Alameda, Contra Costa, Kern, Los Angeles, Monterey, Riverside, San Bernardino, San Francisco, San Joaquin, San Mateo, Santa Clara, and Ventura. All Plan Letter 13-022, California Department of Health Care Services, July 25, 2014, available at http://www.dhcs.ca.gov/formsandpubs/Documents/MMCDAPLsandPolicyLetters/APL2013/APL13-022.pdf. These 12 counties are served under the Two Plan Model, except for Monterey, San Mateo, and Ventura counties, which are served by COHS plans. . ↩︎
- L.A. Care Health Plan website, Plan Partners page. Accessed at http://www.lacare.org/health-plans/medi-cal/plan-partners ↩︎
- As of August 2015, there are four plan choices in Sacramento County and five in San Diego County. Medi-Cal Managed Care Enrollment Report, August 2015. Accessed at http://www.dhcs.ca.gov/dataandstats/reports/Pages/MMCDMonthlyEnrollment.aspx ↩︎
- Medi-Cal Update, Part 1 – Program and Eligibility, October 2013. Accessed at http://files.medi-cal.ca.gov/pubsdoco/bulletins/artfull/part1201310.asp ↩︎
- California Department of Health Care Services, Medi-Cal Managed Care Program Fact Sheet – Managed Care Models, November 2014. Accessed at http://www.dhcs.ca.gov/provgovpart/Documents/MMCDModelFactSheet.pdf; Medi-Cal Managed Care Enrollment Report, August 2015. Accessed at http://www.dhcs.ca.gov/dataandstats/reports/Pages/MMCDMonthlyEnrollment.aspx ↩︎
- California’s 12 public hospital health system counties are: Alameda, Contra Costa, Kern, Los Angeles, Monterey, Riverside, San Bernardino, San Francisco, San Joaquin, San Mateo, Santa Clara, and Ventura. See All Plan Letter 13-022, op. cit. ↩︎
- California’s “Bridge to Reform” section 1115 waiver, approved in November 2010, created the Low Income Health Program (LIHP), which allowed counties to receive federal Medicaid reimbursement for providing health services through the LIHP to residents who would become newly eligible for coverage under the ACA Medicaid expansion in 2014. ↩︎
- All Plan Letter 13-022, op. cit. ↩︎
- MCOs can avoid oversight action associated with not meeting the 75% auto-assignment standard if they demonstrate that they have attempted to meet it but are constrained by regulatory geographic access standards. ↩︎
- Knox-Keene Health Care Service Plan Act of 1975, §1367.03, and Title 28, California Code of Regulations §1300.51 and §1300.67.2. ↩︎
- Bridge to Reform Waiver Resources, California Department of Health Care Services, available at http://www.dhcs.ca.gov/provgovpart/Pages/1115-Bridge-to-Reform.aspx ↩︎
- SPDs in an additional 19 rural counties (Alpine, Amador, Butte, Calaveras, Colusa, El Dorado, Glenn, Imperial, Inyo, Mariposa, Mono, Nevada, Placer, Plumas, Sierra, Sutter, Tehama, Tuolumne, and Yuba) began to transition to mandatory enrollment in Medi-Cal managed care in December 2014. ↩︎
- Medi-Cal Managed Care Performance Dashboard, , California Department of Health Care Services, accessed at: http://www.dhcs.ca.gov/services/Documents/MMCD/20150305MMCPDashboard.pdf ↩︎
- 2012-2013 Governor’s Budget Highlights Department of Health Care Services, January 6, 2012, available at http://www.dhcs.ca.gov/Documents/2012-13%20Budget%20Highlights.pdf ↩︎
- The 2012-13 Budget: Analysis of the Governor’s Healthy Families Program Proposal, Legislative Analyst’s Office, February 17, 2012. Accessed at http://www.lao.ca.gov/analysis/2012/health/healthy-families-021712.aspx ↩︎
- California Department of Health Care Services, Healthy Families Program Transition to Medi-Cal: Final Comprehensive Report, February 4, 2014. Accessed at http://www.dhcs.ca.gov/provgovpart/Documents/Waiver%20Renewal/AppendixCHFP.PDF ↩︎
- Legislative Analyst’s Office, Recent History of Adult Day Health Care and Transition of Seniors and Persons With Disabilities Into Managed Care, March 7, 2012. Accessed at http://www.lao.ca.gov/handouts/Health/2012/Recent_History_ADHC_3_7_12.pdf ↩︎
- California Demonstration to Integrate Care for Dual Eligible Beneficiaries, May 31, 2012, Proposal to CMS. Accessed at https://www.cms.gov/medicare-medicaid-coordination/medicare-and-medicaid-coordination/medicare-medicaid-coordination-office/downloads/caproposal.pdf ↩︎
- Senate Bill (SB) 1008 (Chapter 33, Statutes of 2012); SB 1036 (Chapter 45, Statutes of 2012); and SB 94 (Chapter 37, Statutes of 2013). ↩︎
- Memorandum of Understanding (MOU) Between CMS and The State of California Regarding a Federal-State Partnership to Test a Capitated Financial Alignment Model for Medicare- Medicaid Enrollees, California Demonstration to Integrate Care for Dual Eligible Beneficiaries (2013). Accessed at http://www.cms.gov/Medicare-Medicaid-Coordination/Medicare-and-Medicaid-Coordination/Medicare-Medicaid-Coordination-Office/FinancialAlignmentInitiative/Downloads/CAMOU.pdf ↩︎
- Cal MediConnect Monthly Enrollment Dashboard as of October 1, 2015, California Department of Health Care Services. Accessed at http://www.calduals.org/wp-content/uploads/2015/10/CMC-Enrollment-Dashboard-October-Final-102015.pdf ↩︎
- See: http://www.dhcs.ca.gov/services/Pages/MngdCarePerformDashboard.aspx ↩︎
- S. Zuckerman, A. Williams, and K. Stockley (Urban Institute), Medi-Cal Physician and Dentist Fees: A Comparison to Other Medicaid Programs and Medicare , California Healthcare Foundation, April 2009; accessed at http://www.chcf.org/publications/2009/04/medical-physician-and-dentist-fees-a-comparison-to-other-medicaid-programs-and-medicare ↩︎
- S. Decker, “In 2011, Nearly One-Third Of Physicians Said They Would Not Accept New Medicaid Patients, But Rising Fees May Help,” Health Affairs, 31, no.8, available at http://content.healthaffairs.org/content/31/8/1673.full.pdf+html ↩︎
- P. Cunningham and L. Nichols, “The Effects of Medicaid Reimbursement on the Access to Care of Medicaid Enrollees: A Community Perspective,” Medical Care and Research Review 62, no. 6(2005), available at http://mcr.sagepub.com/content/62/6/676.abstract ↩︎
- D. Polsky, M. Richards, S. Basseyn, D.Wissoker, G. Kenney, S. Zuckerman, and K. Rhodes, “Appointment Availability after Increases in Medicaid Payments for Primary Care,” New England Journal of Medicine, February 5, 2015, accessed at: http://www.nejm.org/doi/full/10.1056/NEJMsa1413299 ↩︎
- Douglas, Director, California Department of Health Care Services v. Independent Living Center of Southern California, Inc., et al., available at http://www.supremecourt.gov/opinions/11pdf/09-958.pdf ↩︎
- S. Rosenbaum, Medicaid Payment Rate Lawsuits: Evolving Court Views Mean Uncertain Future for Medi-Cal, California Health Care Foundation, October 2009, available at http://www.chcf.org/publications/2009/10/medicaid-payment-rate-lawsuits-evolving-court-views-mean-uncertain-future-for-medical ↩︎
- 42 U.S.C. §1396a(a)(30)(A). ↩︎
- Medicaid and Children’s Health Insurance Program (CHIP) Programs; Medicaid Managed Care, CHIP Delivered in Managed Care, Medicaid and CHIP Comprehensive Quality Strategies, and Revisions Related to Third Party Liability: Proposed Rules, Federal Register, Vol. 80, No. 104, June 1, 2015, https://www.federalregister.gov/articles/2015/06/01/2015-12965/medicaid-and-childrens-health-insurance-program-chip-programs-medicaid-managed-care-chip-delivered ↩︎
- Medi-Cal at a Crossroads: What Enrollees Say about the Program, California HealthCare Foundation, May 2012, available at http://www.chcf.org/publications/2012/05/medical-crossroads-what-enrollees-say ↩︎
- Monitoring Access to Care for MediCal Enrollees in a Time of Change: CHCF Sacramento Briefing, October 16, 2014, California HealthCare Foundation, accessed at: http://www.chcf.org/events/2014/briefing-medical-access ↩︎
- Centers for Disease Control and Prevention, National Center for Health Statistics, “Acceptance of New Patients With Public and Private Insurance by Office-based Physicians: United States, 2013,” NCHS Data Brief, No. 195, March 2015; accessed at http://www.cdc.gov/nchs/data/databriefs/db195.pdf ↩︎
- J. Coffman, D. Hulett, M. Fix, and A. Bindman, Physician Participation in Medi-Cal: Ready for the Enrollment Boom? California HealthCare Foundation, August 2014, available at http://www.chcf.org/publications/2014/08/physician-participation-medical ↩︎
- California Department of Health Care Services: Improved Monitoring of Medi-Cal Managed Care Health Plans Is Necessary to Better Ensure Access to Care, Report 2014-134, California State Auditor, June 2015, available at http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/PDF%20P/PDF%20PhysicianParticipationMediCalEnrollmentBoom.pdf ↩︎
- Frequency of Threshold Language Speakers in the Medi-Cal Population by County for December 2013,” Medi-Cal Statistical Brief, California Department of Health Care Services Research and Analytic Studies Division, , “May 2014, available at http://www.dhcs.ca.gov/dataandstats/statistics/Documents/RASB_Issue_Brief_Annual_Threshold_Language_Report.pdf ↩︎
- G. Sánchez, T. Nevarez, W. Schink, and D. Hayes-Bautista, “Latino Physicians in the United States, 1980–2010: A Thirty-Year Overview From the Censuses,” Academic Medicine 90:7, July 2015, available at: http://journals.lww.com/academicmedicine/Citation/2015/07000/Latino_Physicians_in_the_United_States,_1980_2010_.20.aspx ↩︎
- On the Frontier: Medi-Cal Brings Managed Care to California’s Counties, California Healthcare Foundation, March 2015, available a http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/PDF%20F/PDF%20FrontierMediCalMgdCareRural.pdf ↩︎
- C. Graham, E. Kurtovich, S. Taube, and R. Arguello, Transitioning Beneficiaries with Complex Care Needs to Medicaid Managed Care: Insights from California, Kaiser Commission on Medicaid and the Uninsured, July 2013, available at https://modern.kff.org/search/?s=Transitioning+Beneficiaries+with+Complex+Care+Needs+to+Medicaid+Managed+Care:+Insights+from+California ↩︎
- D. Gorn, “Medi-Cal Transition ‘Lessons Learned,’” California Healthline, October 24, 2013, available at http://www.californiahealthline.org/capitol-desk/2013/10/lessons-learned-from-medical-transitions ↩︎
- Extended Continuity of Care for SPDs Transitioning to Mandatory Managed Care, News Release, Department of Health Care Services, November 4, 2011, available at http://files.medi-cal.ca.gov/pubsdoco/newsroom/newsroom_20066.asp ↩︎
- C. Graham, E. Kurtovich, S. Taube and R. Arguello, op. cit. ↩︎
- Available at http://www.calduals.org/enrollment-information/hra-data ↩︎
- J. Paradise and M. Musumeci, Proposed Rule on Medicaid Managed Care: A Summary of Major Provisions, Kaiser Commission on Medicaid and the Uninsured, July 23, 2015, available at https://modern.kff.org/medicaid/issue-brief/proposed-rule-on-medicaid-managed-care-a-summary-of-major-provisions/ ↩︎
- California Hospital Association comment letter to the Centers for Medicare & Medicaid Services, available at http://www.regulations.gov/#!documentDetail;D=CMS-2015-0068-0570 ↩︎
- Medi-Cal 2020 Waiver Resources, California Department of Health Care Services, available at http://www.dhcs.ca.gov/provgovpart/Pages/medi-cal-2020-waiver.aspx ↩︎