How Quickly are States Connecting Applicants to Medicaid and CHIP Coverage?
Application Processing Time
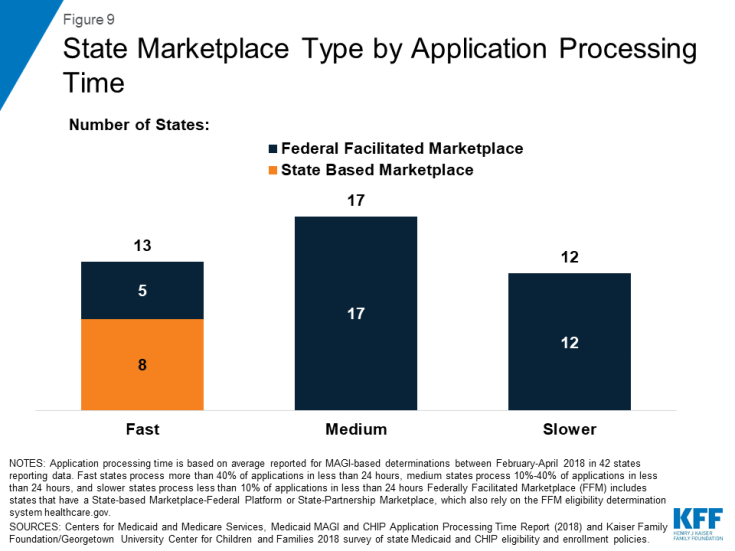
The CMS report shows that, among the 42 states reporting data for February to April 2018, the average share of applications processed in less than 7 days was 53%, including an average of 34% processed in less than 24 hours (Figure 2).1 On average, states processed 14% of applications in over 45 days, beyond the timeframe specified under federal rules. Application processing time varied widely across states (Appendix Table 1).
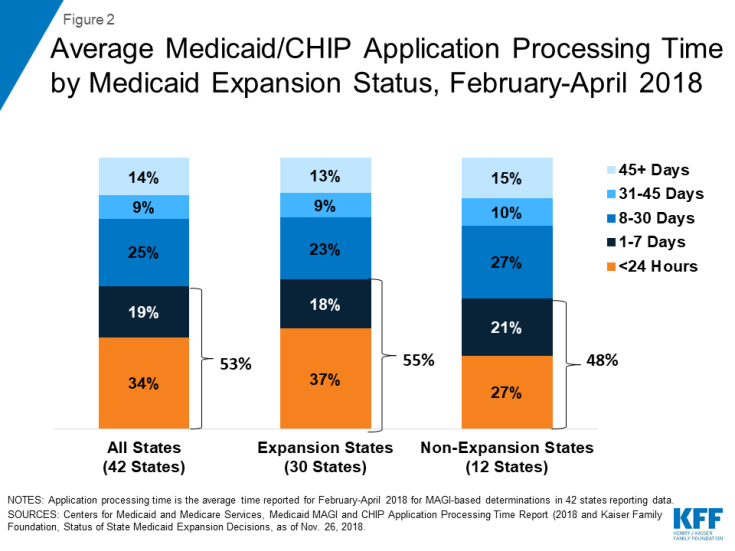
Figure 2: Average Medicaid/CHIP Application Processing Time by Medicaid Expansion Status, February-April 2018
On average, states that adopted the ACA Medicaid expansion reported faster application processing times compared to non-expansion states (Figure 2). Among the 30 expansion states reporting data, the average share of applications processed in less than 7 days was 55%, including an average of 37% processed in less than 24 hours. In the 12 non-expansion states reporting data, the average share of applications processed in less than 7 days was 48%, including an average of 27% processed in less than 24 hours.
Eligibility and Enrollment Policies and Processes
We classified states as having fast, medium, or slower application processing times based on the average share of applications processed within less than 24 hours between February and April 2018 (Figure 3). There were 13 fast states that processed more than 40% of applications in less than 24 hours, 17 medium states that processed 10%-40% of applications in less than 24 hours, and 12 slower states that processed less than 10% of applications in less than 24 hours. We then used data from the 2018 Kaiser Family Foundation national survey of Medicaid and CHIP eligibility and enrollment policies to examine selected eligibility and enrollment policies by states’ application processing time (Appendix Table 2).
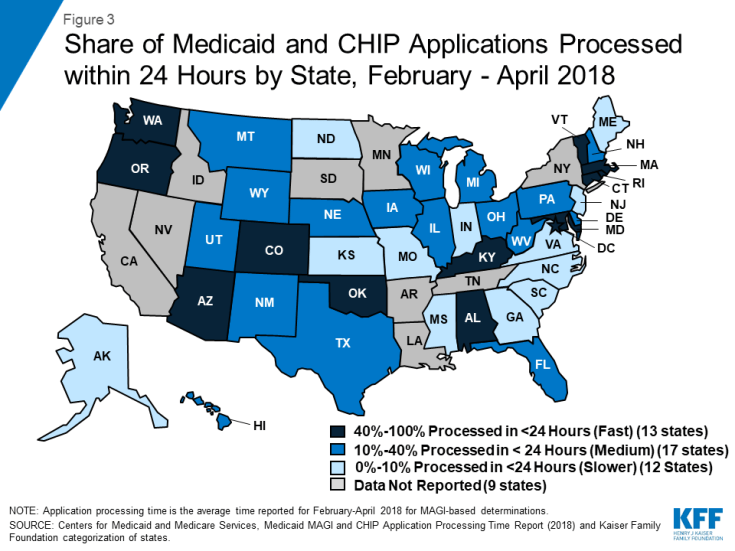
Figure 3: Share of Medicaid and CHIP Applications Processed within 24 Hours by State, February – April 2018
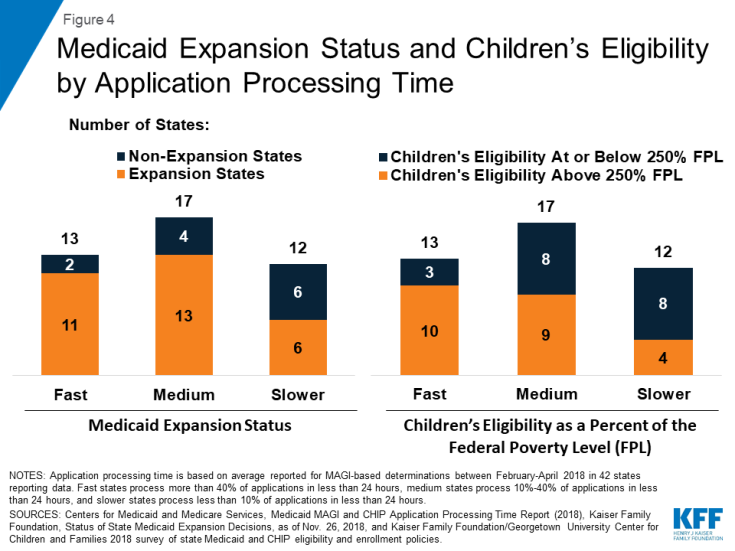
States that had fast or medium application processing times generally had broader eligibility than slower states. The majority of states with fast or medium application processing times have adopted the ACA Medicaid expansion to adults and expanded children’s Medicaid/CHIP eligibility to above 250% FPL (Figure 4). In contrast, among the 12 slower states, only half (6) have adopted the Medicaid expansion, and four have expanded children’s eligibility to above 250% FPL.
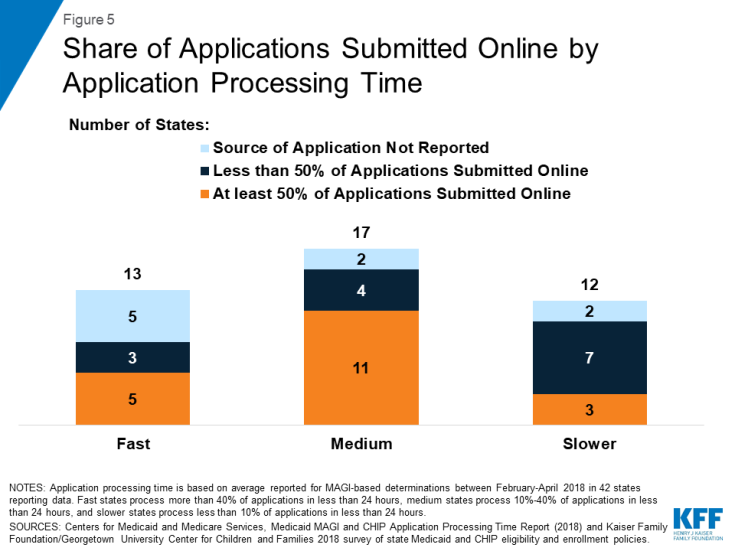
The majority of states with fast or medium application processing times reported receiving at least half of their applications online among those reporting data on mode of application (Figure 5). In the ten slower states reporting data on mode of application, three indicated that they receive more than half of applications online.
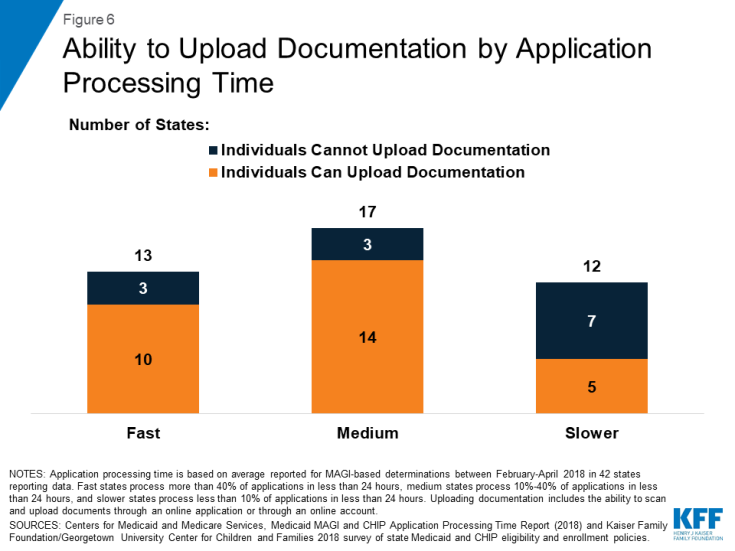
Most states with fast and medium application processing times allow individuals to upload required documents electronically as part of the online application or through an online account (Figure 6). Among the 12 slower states, 5 provide options for individuals to upload documentation electronically.
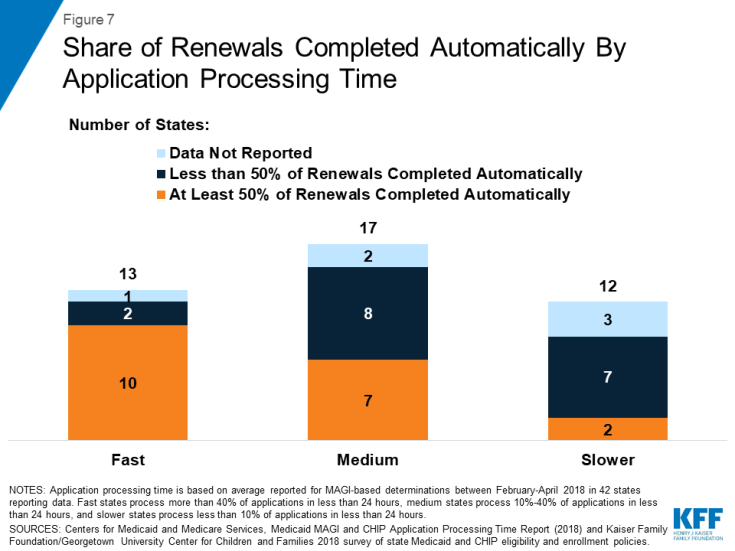
States with faster application processing times also were more likely to report completing most renewals automatically. Most states that had fast application processing time reported completing at least half of their renewals automatically (Figure 7). Less than half of states with medium processing time who reported data on automated renewals reported that they complete the majority of their renewals automatically, and only 2 of the 9 slower states that reported data on automated renewals reported completing more than half of renewals automatically.
Few states with fast application processing times had their MAGI Medicaid eligibility determination system integrated with non-MAGI groups or non-health programs, and most had a state-based Marketplace (SBM) (Figures 8 and 9). A larger share of states with medium and slower application processing times had their MAGI Medicaid eligibility systems integrated with non-MAGI groups and/or non-health programs, and all of these states rely on the Federally-Facilitated Marketplace (FFM, healthcare.gov) for eligibility determinations. This variation reflects differing approaches states took to upgrade processes and systems in response to the ACA. Prior to the ACA, states’ eligibility systems generally included all Medicaid groups and most included non-health programs, such as Temporary Assistance for Needy Families (TANF) and Supplemental Nutrition Assistance Program (SNAP).2 The ACA required states to use a new MAGI-based financial methodology to determine Medicaid eligibility for pregnant women, children, parents, and expansion adults, to apply streamlined eligibility and enrollment processes to MAGI groups, and to align and coordinate MAGI eligibility determinations and enrollment with the Marketplaces. States continue to apply their pre-ACA financial eligibility methodologies to non-MAGI groups (seniors and individuals eligible based on a disability) and have the option to apply some of the streamlined processes to non-MAGI groups. To implement the ACA policies, some states separated MAGI eligibility determinations from non-MAGI groups and non-health programs, often integrating them into newly built SBM systems. Others did not separate MAGI groups from other groups or programs when they upgraded their systems. Over the past few years, a number of states have reintegrated non-MAGI groups and non-health programs into their upgraded systems, and states continue to focus on reintegration as they refine their systems.3
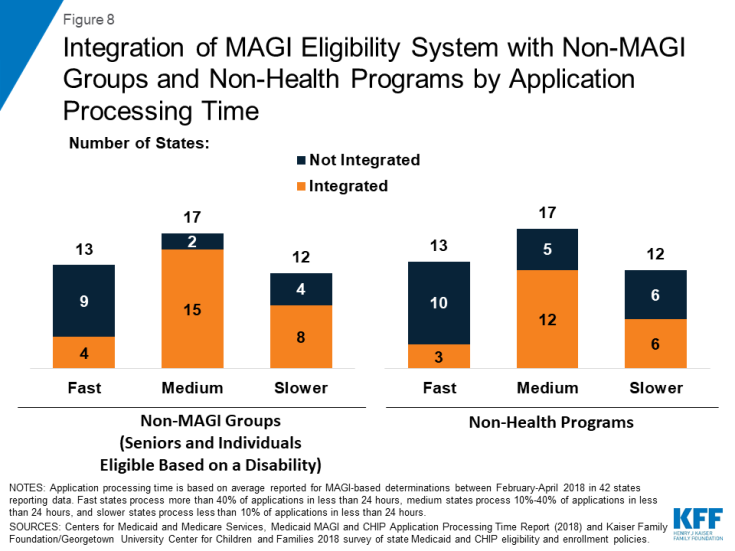
Figure 8: Integration of MAGI Eligibility System with Non-MAGI Groups and Non-Health Programs by Application Processing Time
Conclusion
In November 2018, CMS released new state data on MAGI Medicaid and CHIP application processing time. These data reflect continued progress in reporting of performance indicators that CMS established in 2013 to facilitate data-driven program management and improvement. The data show that, across the 42 states reporting data for February to April 2018, on average, over half (53%) of applications were processed within 7 days, including over a third (34%) processed in less than 24 hours.
There was significant variation across states in how quickly they process applications. States with faster application processing generally had broader eligibility compared to those with slower application processing. They also were more likely to receive the majority of their applications online and allow individuals to upload documentation electronically, which may facilitate faster application processing. Further, consistent with their ability to process applications quickly, they also were more likely to process the majority of renewals automatically, likely reflecting effective electronic data matching capabilities. States with faster application processing times were less likely than states with medium or slower application processing times to have their MAGI Medicaid eligibility systems integrated with non-MAGI groups (seniors and individuals eligible based on a disability) or non-health programs. This variation reflects states’ differing approaches to upgrade systems and processes in response to the ACA eligibility determination and enrollment policies, which vary for MAGI and non-MAGI groups. A number of states plan to reintegrate non-MAGI groups and non-health programs into their upgraded systems in the future, which may contribute to improvements in processing of eligibility determinations for other groups and programs and facilitate access to services for individuals.4
The ability for states to make real-time eligibility determinations, as demonstrated by these new data, illustrates the significant progress states have made in streamlining and automating enrollment processes under the ACA. Through the ACA’s streamlined policies and state efforts, the Medicaid enrollment and renewal experience has moved from a paper-based, manual process that could take days and weeks in some states to a modernized, technology-driven approach that can happen in real-time through electronic data matches to verify eligibility criteria.5 These changes facilitate individuals’ ability to access and maintain coverage and provide opportunities for states to realize administrative efficiencies and increase accuracy of determinations and renewals. However, there remains significant variation across states in application processing time, and continued opportunities for improvement to ensure states complete all MAGI eligibility determinations within 45 days, as required under federal rules. Recent waivers in some states to add eligibility and enrollment restrictions, including work reporting requirements, could reverse the progress achieved in streamlining enrollment, resulting in additional barriers to coverage and coverage losses.