Coverage of Preventive Services for Adults in Medicaid
Alexandra Gates, Usha Ranji, and Laura Snyder
Published:
Executive Summary
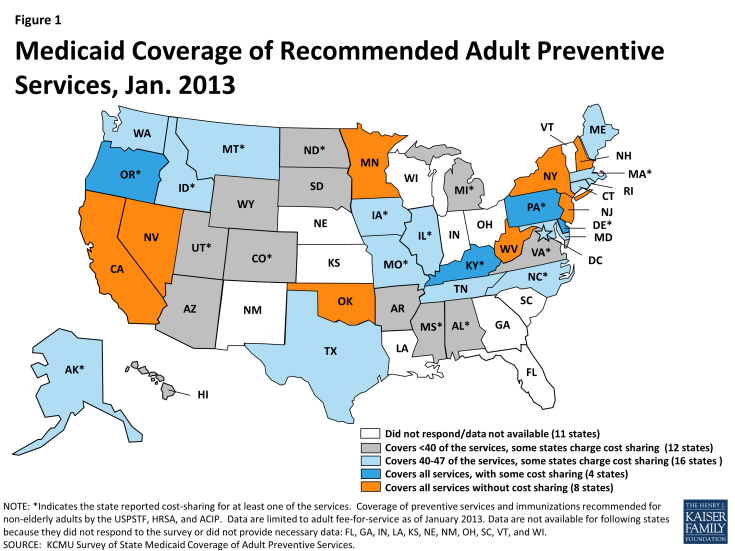
- While all of the individual preventive services were covered by most (28) state Medicaid programs in 2013, many states charged cost sharing for at least some of the services. Eight states (Figure 1) reported covering all 47 of the preventive services in this survey without cost sharing (California, Minnesota, Nevada, New Hampshire, New Jersey, New York, Oklahoma, and West Virginia).
- Several more states are close to qualifying for the higher matching rate. Four states cover all of the services but charge cost sharing for at least one of the services. Another 16 states cover at least 40 of the services but may charge cost sharing for some.
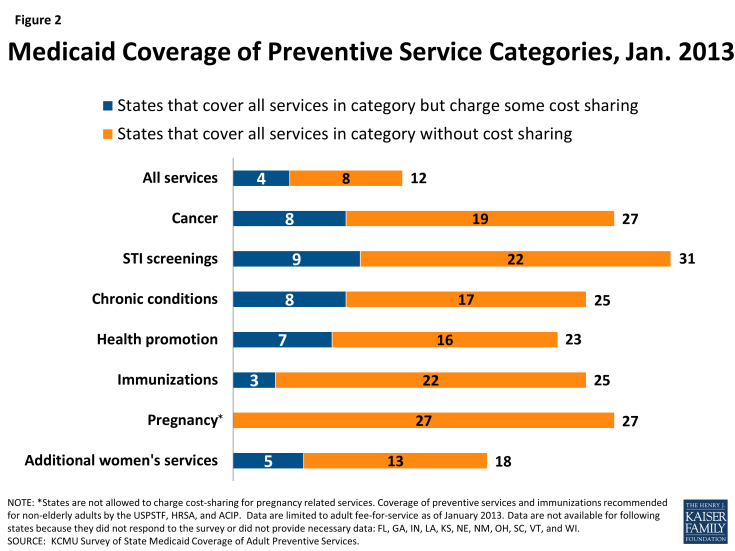
- More than half of the responding states reported they cover all STI counseling services and immunizations without cost sharing. Most also cover all pregnancy-related services, which are not subject to cost sharing. The majority of states reported covering all of the services in the other categories subject to the enhanced match (cancer screenings, health promotion, chronic conditions), but several states were charging cost sharing for at least one service (Figure 2).
- Each individual preventive service was covered by at least half and in many cases two-thirds of reporting states.
Introduction
Preventive Services and the Affordable Care Act (ACA)
One of the goals of the ACA was to expand access to preventive services. One of the first requirements of the ACA to be implemented was to require virtually all private health plans to cover recommended preventive services without cost sharing beginning September 2010.3 Medicare also eliminated cost sharing requirements for all recommended preventive services starting January 1, 2013.4
Under Medicaid, states must cover preventive services for children, while coverage of preventive services for adults in Medicaid has historically been considered optional. Additionally, states have the option of instituting cost sharing for selected beneficiaries and selected services. Given their limited incomes and greater health care needs, federal rules limit the amount of cost-sharing states can charge Medicaid enrollees to help protect them from high out-of-pocket costs and facilitate their access to needed care. States are prohibited from charging any cost sharing for pregnant women as well as children and adults with incomes below the poverty level.
Box 1: Preventive Services for AdultsThe preventive services that are subject to the enhanced federal match for Medicaid are those that are recommended for adults by two entities:
|
One of the pillars of the ACA is the incentive for states to expand eligibility for Medicaid to cover many currently uninsured individuals. In states that expand eligibility (as of October 2014, 27 states and the District of Columbia have expanded), the benefits package for most adults in the new Medicaid expansion group is known as the “Alternative Benefit Plan” (ABP). Under the ABP, states must cover preventive services for adults without cost sharing, but this is not required for the group of adults enrolled in or eligible for traditional Medicaid prior to the ACA’s expansion of the program. However, in order to incentivize states to cover preventive services without cost sharing in traditional Medicaid, Section 4106 of the ACA added an enhanced matching rate of one percentage point to the state’s Federal Medical Assistance Percentage (FMAP) for preventive services if the state covers without cost sharing all of the preventive services recommended by the United States Preventive Services Task Force (USPSTF) and the Advisory Committee on Immunization Practices (ACIP) (Box 1).
In addition, Section 2713 of the ACA authorized the development of an additional set of preventive services for women, which were recommended by the Institute of Medicine (IOM) and subsequently adopted by the federal Health Resources and Services Administration (HRSA). These services must be covered without cost sharing by all new private plans. While these services are not included as part of the requirements for the Medicaid enhanced match for preventive services, they overlap with many of Medicaid’s benefits categories and were recommended as important to fill in gaps in preventive services for women.
This brief highlights data from a survey of state fee-for-service Medicaid programs conducted by the Kaiser Commission on Medicaid and the Uninsured (KCMU) on coverage and cost sharing for 47 preventive services recommended by the USPSTF, ACIP, and HRSA for non-elderly adults as of January 1, 2013.6,7 In total, 39 states and the District of Columbia replied to the survey. Findings are summarized in the next section for coverage of cancer screenings, counseling on sexually transmitted infections, chronic conditions, health promotion, immunizations, pregnancy, and women’s health.
Key Findings
Survey Findings
The Kaiser Commission on Medicaid and the Uninsured conducted a survey of Medicaid programs in all 50 states and the District of Columbia on coverage of and cost sharing for preventive services. Thirty-nine states and the District of Columbia replied to the survey. States were asked whether they covered 40 services recommended by the USPSTF and ACIP as well as seven additional services recommended for women by HRSA. States were also asked whether they charge cost sharing for services, except for pregnancy-related services.
Cancer Screenings (Table 1)
TABLE 1: CANCER-RELATED SERVICES (as of January 2013)
Great strides in early detection and advances in treatment options have improved overall cancer survival rates over many decades. The USPSTF recommends three different services related to breast cancer as well as screening tests for cervical and colorectal cancers.
Breast Cancer Mammography, Cervical Cancer, and Colorectal Cancer Screenings
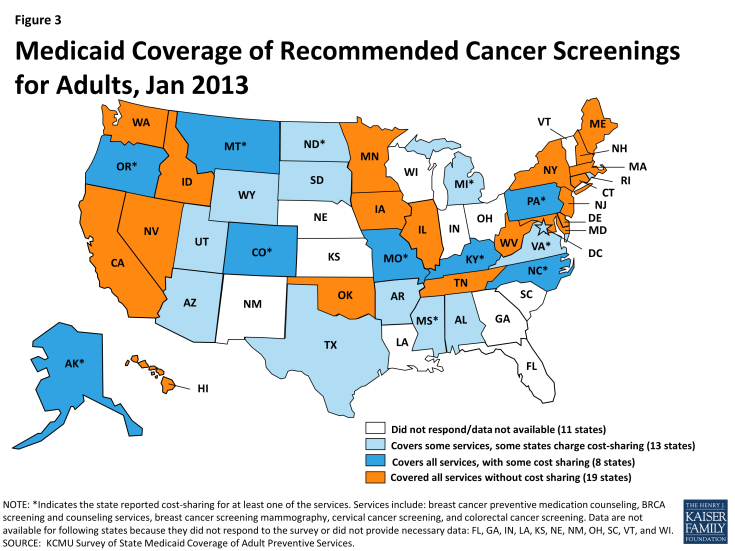
In total, 19 states cover all of the cancer-related services without cost sharing. Virtually all states responding to the survey indicated that they cover mammograms, cervical cancer screenings, and colorectal cancer screenings as recommended by the USPSTF. Arkansas reported that it does not cover both mammography and colorectal cancer screening, and Michigan noted that it does not cover screening for colorectal cancer. Only a handful of states reported cost-sharing for these services (8 states for colorectal cancer screenings, and 7 states for breast cancer mammography and cervical cancer screenings.)
Some states noted mammograms and cervical cancer screenings were at least in part covered through an optional eligibility pathway adopted by all states under the Breast and Cervical Cancer Prevention and Treatment Act. This option allows states to extend Medicaid coverage for cancer treatment to uninsured women diagnosed with breast or cervical cancer through a federal screening program; states receive a higher matching rate for services reimbursed under this program equivalent to the CHIP matching rate.1 A few states also noted coverage of these services under the family planning benefit, which is reimbursed at a 90 percent matching rate.
Breast Cancer Preventive Medication Counseling, BRCA Screening and Counseling
Coverage for two other services recommended by the USPSTF – breast cancer preventive medication counseling and BRCA screening, are not as commonly covered as the cancer screening tests discussed above. These services are recommended only for women who are deemed at high risk of breast cancer or those with a family history of deleterious mutations of select genes. Twenty-eight states cover both of these services; an additional 7 states cover one of these services but not the other. Ten states charge copays for one or both of these services (Figure 3).
Sexually-Transmitted Infection (STI) Screenings and Counseling (Table 2)
TABLE 2: SEXUALLY-TRANSMITTED INFECTION (STI) SCREENINGS (January 2013)
There are 20 million new sexually-transmitted infections (STIs) every year.2 Undetected and untreated STIs can increase a person’s risk for HIV and can lead to other adverse health consequences, such as infertility. According to the Centers for Disease Control and Prevention (CDC), less than half of people who should be screened for STIs receive recommended screening services.
Chlamydia, Gonorrhea, and Syphilis Screenings and STI Counseling
Almost all states participating in this survey reported covering screening tests for Chlamydia, Gonorrhea, and Syphilis as recommended by the USPSTF. Eight states reported that at least one of these STI screenings was subject to cost-sharing. Fewer states cover counseling about STIs as recommended by the USPSTF, though 32 states did report covering this service. Seven states indicated that they charge cost-sharing for STI counseling services. In total, 31 states covered all the STI screenings and counseling services; 22 of these states do so without charging cost-sharing (Figure 4).
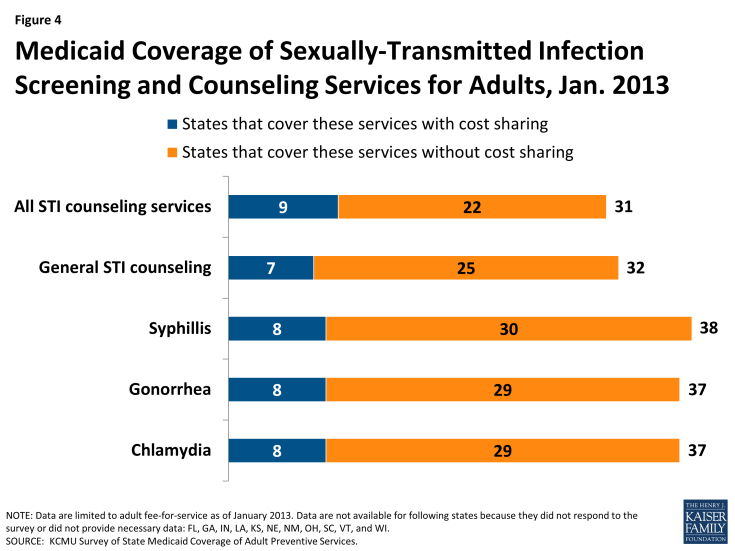
Figure 4: Medicaid Coverage of Sexually-Transmitted Infection Screening and Counseling Services for Adults, Jan. 2013
Some states noted some of these services are at least partially covered as family planning services. Family planning is a mandatory benefit for states; however the services covered under this benefit as well as limitations on those services vary across states, though states cannot charge cost-sharing for these services. States receive a 90 percent federal match on services covered under this benefit. Family planning services are not considered to be a preventive service for purposes of receiving the 1% increase in FMAP.
For non-elderly adults, states were surveyed regarding the coverage of two forms of HIV screenings: HIV for high risk populations and routine HIV screenings for adults. These survey results are reported in more detail on the Kaiser Family Foundation’s website at State Medicaid Coverage of Routine HIV Screening.3
Preventive Services Related to Chronic Conditions (Table 3)
TABLE 3: CHRONIC CONDITION-RELATED SERVICES (January 2013)
Chronic conditions afflict millions of women and men with Medicaid. Nearly one in ten low-income, non-elderly adult Medicaid beneficiaries have been diagnosed with diabetes, more than two in ten with chronic obstructive pulmonary disease, nearly three in ten with heart disease, and over one-third have been diagnosed with a mental health condition.4 Research has shown that increases in the use of preventive services, particularly screenings and treatment related to cardiovascular disease, can lead to the prevention of a significant number of deaths per year.5
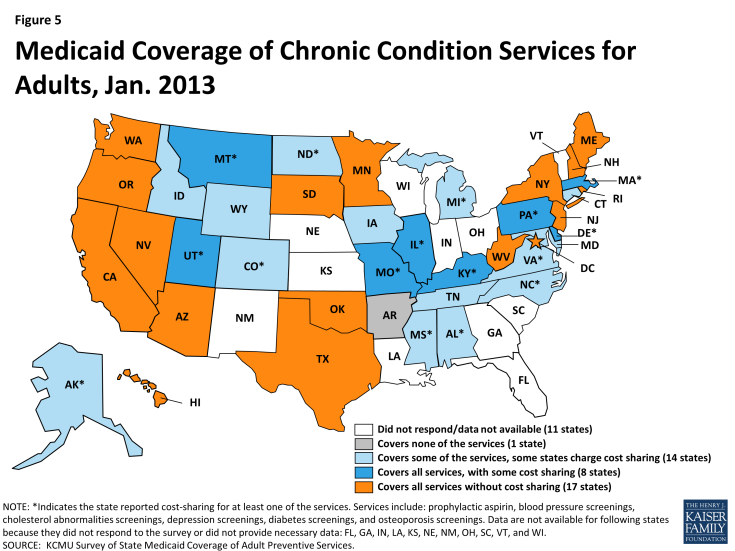
Prophylactic Aspirin, Blood Pressure, Cholesterol, Depression, Diabetes, and Osteoporosis Screenings
Overall, 25 states reported covering all of the services in this category; 17 without cost-sharing (Figure 5). Nearly all states reported covering blood pressure screenings and screenings for cholesterol abnormalities (38 states each). Fewer states reported covering prophylactic aspirin (31 states) despite research highlighting in particular its effectiveness in reducing the number of deaths from cardiovascular disease and its potential to yield significant medical savings.6 Copays were also most prevalent for this service compared to others in this category. Additionally, most states reported coverage of diabetes screenings (37 states) and osteoporosis screenings (35 states).
There is a high prevalence of diagnosed mental health conditions among Medicaid beneficiaries. The only preventive service specific to mental health in this survey was depression screening, which is covered by most states; 26 of the 34 states that cover this service do not charge cost-sharing.
Health Promotion (Table 4)
TABLE 4: HEALTH PROMOTION SERVICES (as of January 2013)
The category of health promotion includes a number of services aimed at promoting healthy behaviors that help prevent chronic illnesses. This includes screening for obesity and counseling on a number of behavioral issues such as diet and nutrition, tobacco use, and alcohol use.
Alcohol Misuse, Healthy Diet, Obesity Screening and Counseling, Tobacco Use Counseling, Folic Acid Supplementation
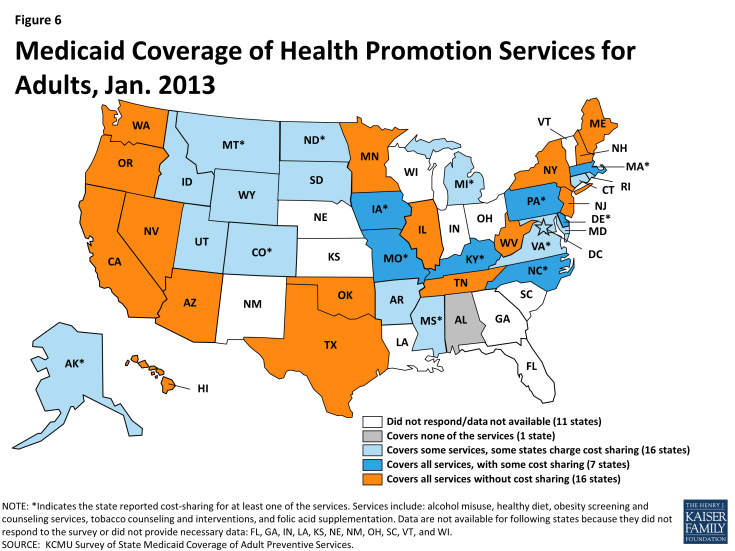
Twenty-three states covered all of the recommended preventive services that fall under this category; 16 states did so without cost-sharing (Figure 6). One state reported they do not cover any of these preventive services for adults (Alabama).
Nearly every state that covered healthy diet counseling services also covered obesity screening and counseling; the same 7 states also reported cost-sharing for both of these services.7 The obesity-related services are particularly important given the alarming high obesity rates in the United States and obesity’s link to many chronic conditions such as coronary heart disease, stroke, diabetes, and cancer.8
The most commonly covered service was tobacco use counseling and interventions (34 states) with 28 of these states doing so without cost-sharing. Research has highlighted the potential of tobacco use counseling and interventions to yield cost-savings and have large health impacts.9 Most of the surveyed states also cover counseling on alcohol misuse. Thirty-three states reported covering this service and 25 of them do not charge cost-sharing.
The USPSTF also recommends that women of childbearing capability take a daily supplement of folic acid to prevent certain birth defects. Thirty-one states reported covering this service and 21 of them do so without cost-sharing.
Immunizations (Tables 5A and 5B)
TABLE 5A: IMMUNIZATIONS RECOMMENDED IF OTHER RISK FACTORS ARE PRESENT (as of January 2013)
TABLE 5B: IMMUNIZATIONS RECOMMENDED FOR ALL PERSONS MEETING AGE AND GENDER REQUIREMENTS WHO LACK EVIDENCE OF IMMUNITY (as of January 2013)
There are ten immunizations recommended for adults by the Advisory Committee on Immunization Practices (ACIP). Six of the immunizations (Td booster/Tdap, MMR, Influenza, Varicella, Zoster and HPV) are recommended for all individuals who meet select age and gender criteria and who show no sign of immunity. Four (Hepatitis A, Hepatitis B, Meningococcal, and Pneumococcal) are recommended for those when additional risk factors are present.
Td booster/Tdap, MMR, Influenza, Varicella, Zoster, HPV, Hepatitis A and B, Meningococcal, and Pneumococcal
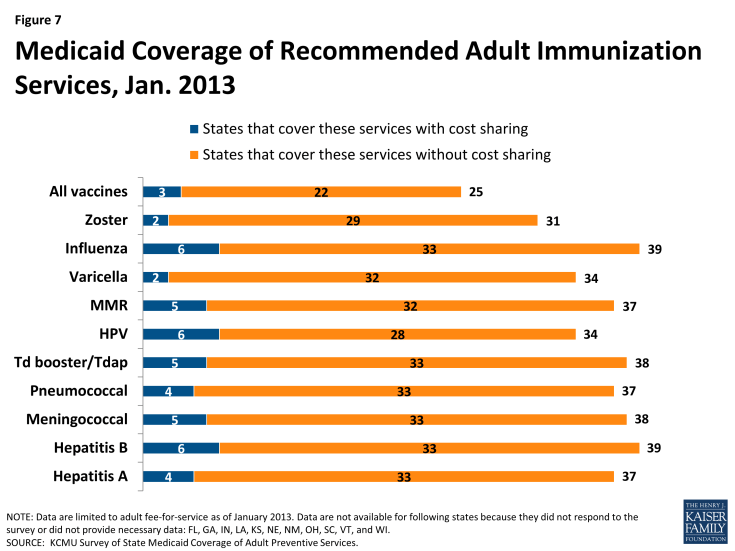
In total, 22 states reported covering all the recommended immunizations without cost-sharing (Figure 7). While 25 states indicated that they covered all of the recommended immunizations for non-elderly adults, some charged cost sharing. A number of other states reported coverage of the immunizations, but for a narrower age range than is recommended (i.e. for those 18 years and younger).
The most commonly covered immunizations were for Influenza and Hepatitis B (39 states). Both immunizations for MMR and Td booster/Tdap were covered for non-elderly adults by most states (37 and 38 states, respectively). However, fewer states cover Varicella (34 states) and Zoster (31 states). Another less commonly covered immunization was HPV; 34 states covered this immunization for women age 26 and under, and some of these 34 states reported covering the immunization for males as well.
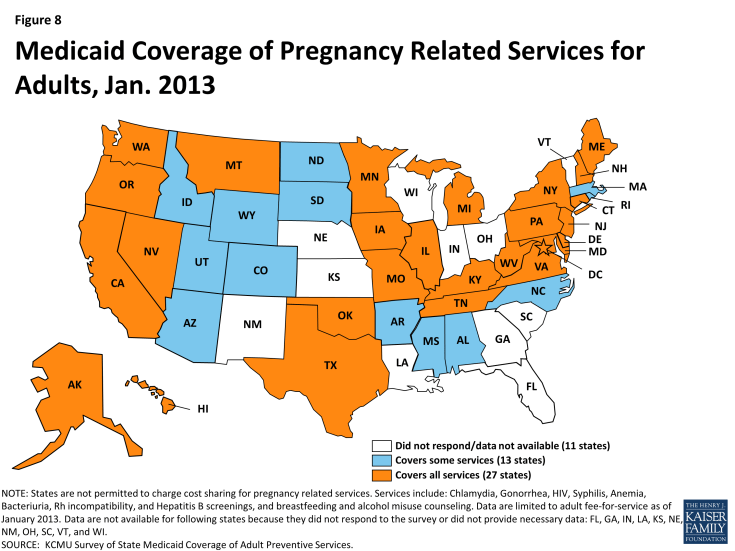
Pregnancy-Related Preventive Services
Approximately half of all births in the U.S. are paid for by Medicaid, making it the single largest payor for maternity care.10 Responses to the survey showed that preventive services recommended by the USPSTF for pregnant women were well-covered under state Medicaid programs in January 2013. Because pregnancy-related services are exempted from cost-sharing, states were not asked about cost-sharing for these services. (Figure 8).
STI and HIV Screenings (Table 6A)
TABLE 6A: SEXUALLY-TRANSMITTED INFECTION (STI) SCREENINGS FOR PREGNANT WOMEN (January 2013)
All states responding to the survey reported covering STI screenings for Chlamydia, Gonorrhea and Syphilis, which matches data reported on STI screenings covered for non-elderly adults in an earlier section. All states reported covering HIV screening for pregnant women as well.
Hepatitis B, Anemia, Bacteriuria, Rh Incompatibility Screenings, Breast Feeding Counseling, and Alcohol Misuse Counseling (Table 6B)
TABLE 6B: PREGNANCY-RELATED SCREENINGS AND COUNSELING SERVICES (as of January 2013)
All states responding to the survey reported covering screenings for Hepatitis B, as well as Rh incompatibility at both the first prenatal visit and again at 24-28 gestational weeks. All but two states also covered bacteriuria and anemia screenings. While not as common, the majority of states also cover breastfeeding counseling (29 states) and alcohol misuse counseling (36 states).
Women’s Preventive Services Recommended by the Health Resources and Services Administration
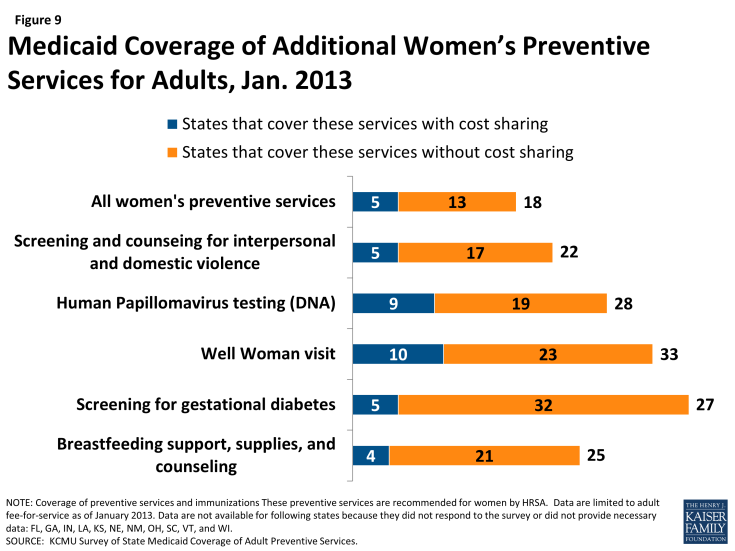
In addition to the preventive services recommended by the USPSTF and ACIP, Section 2713 of the ACA called for the formation of a committee to study and recommend whether any additional preventive services for women should be covered by private insurance plans. A committee of the IOM recommended eight additional preventive services for women11 and these recommendations were subsequently adopted by HRSA.12 As a result, all new private plans must cover these services without cost sharing. However, the additional women’s preventive services are not included as part of the Medicaid enhanced match for preventive services. Nonetheless, we surveyed states about Medicaid coverage of these services and found that all states covered most or some of the additional services. Of the 39 states and DC that responded, 18 covered all of these services and 13 of these states do not charge cost sharing for any of the services (Figure 9).
Screening for Gestational Diabetes and Breastfeeding Support, Supplies, and Counseling (Table 7A)13
TABLE 7A: ADDITIONAL WOMEN’S SERVICES
Most states (32) cover screening for gestational diabetes in pregnant women without cost sharing. Coverage for breastfeeding supports is not as common, with only 21 states reporting they cover these supports without cost sharing. While the USPSTF has recommended breastfeeding counseling prior to the passage of the ACA, the recommendation from HRSA is more expansive as it recommends coverage of counseling as well as supplies, in particular breast pumps.
Well Woman Visit, Human Papillomavirus DNA Testing, and Screening and Counseling for Interpersonal and Domestic Violence (Table 7B)
TABLE 7B: WOMEN’S PREVENTIVE SERVICES
HRSA also recommends coverage for at least one annual well woman visit, DNA testing for HPV, and screening and counseling for interpersonal and domestic violence. More than half of states cover well woman visits (33 states) and HPV testing (28 states), but that is not the case for interpersonal and domestic violence screening (22 states). However, many states charge cost sharing for these services and overall, of the 20 states that report covering all three of these services, 15 states cover them without cost-sharing.
Summary
The ACA provides a number of opportunities to improve access to and quality of care for many adults currently in Medicaid programs and those that are newly eligible since January 1, 2014. Medicaid coverage of preventive services for adults has historically been considered optional, meaning states can elect whether to cover preventive services in their Medicaid programs for adults. Furthermore, states are permitted to charge cost sharing for some beneficiaries, in the low-income population that Medicaid serves, where even nominal charges can pose a barrier to obtaining services.14
To date, at least eight states have taken up the ACA incentive for an enhanced match for preventive services. While all of the individual preventive services were covered by most state Medicaid programs in 2013, many states charged cost sharing for at least some of the services. Overall, 12 states reported covering all of the services included in the survey; eight of them did so without cost-sharing. Another 16 states reported covering at least 40 of the recommended services. In general, there was more variation in cost-sharing policies; 10 states reported cost-sharing for at least ten of the services.
While the ACA requires states to cover preventive services without cost sharing for newly eligible Medicaid populations in the Alternative Benefit Plans (ABPs), coverage of preventive services is provided at state option for those eligible for Medicaid prior to the ACA’s coverage expansion. As these plans are developed, additional states could align the benefits in their traditional Medicaid programs with the ABPs, and thus expand coverage of preventive services without cost sharing to previously eligible populations as well through amendments to their state Medicaid plans. This would reduce differences in benefits between different groups of Medicaid beneficiaries and would also extend coverage for preventive services to a broader group of individuals on the program.
Methodology
The data in this report reflect results from a survey fielded April through June 2013 that asked states about coverage and related cost-sharing for those preventive services recommended for non-elderly adults by the USPSTF (services that received a grade “A” or “B”,) some services under review by USPSTF at the time of the survey, some services recommended by HRSA and immunizations recommended by the ACIP; 47 services in total were included in the survey, which are detailed in Appendix A. These data do not reflect coverage for children or those over the age of 65 in Medicaid programs. Data are reported for 39 states and the District of Columbia that responded to the survey; data are not reported for the 11 states that did not respond or did not provide complete data: Florida, Georgia, Indiana, Kansas, Louisiana, Nebraska, New Mexico, Ohio, South Carolina, Vermont, and Wisconsin.
The survey instrument (a copy of which is provided in Appendix B) asked states if they had submitted or planned to submit a state plan amendment to receive the enhanced match for covering all the recommended services without cost sharing; if a state responded that they in fact did, they were assumed to have covered all preventive services with no cost-sharing asked about in the survey. All of the states that reported that they either submitted or planned to submit a SPA at the time of the survey have been approved (CA, NH, NJ, and NY) except for LA. While LA reported plans to submit a SPA, to date, there is no SPA submission posted for this state and documentation from the state’s website indicates that they do not cover at least some of the preventive services asked about in this survey. Therefore, data are not reported for LA. Some states did not respond to all questions; these cases are noted as “NR” in the appendix tables.
Coverage
The survey asked if the state Medicaid program covered any of the recommended preventive services. Many states responded with service-specific caveats, most notably that service was covered only if medically necessary or that the service was covered but only as part of an office visit and not as a distinct service. For purposes of this report, states reporting such caveats were counted as covering these services.
Cost-sharing
This survey asked states to report if they charged cost-sharing for the recommended preventive services. States were asked to include cost-sharing that applied to 1) the service when billed separately from the related office or clinic visit and 2) the visit if the preventive services was the primary purpose of the visit and the services and visit are not billed separately.
Appendices
Appendix A: ACA Section 4106 increase in FMAP for Coverage of Preventive Services in Medicaid
In order to incentivize states to cover preventive services without cost sharing in traditional Medicaid, Section 4106 of the ACA added an enhanced matching rate of one percentage point to the state’s Federal Medical Assistance Percentage (FMAP) for preventive services if the state covers without cost sharing all of the preventive services recommended by USPSTF and ACIP (Table A1).
To receive the enhanced match, states must cover all of these services without charging cost-sharing for any and file a State Plan Amendment (SPA) to their Medicaid plan. As of July 2014, eight (8) states had submitted preventive services SPAs: Four states had filed for SPAs at the time the survey was conducted in Spring 2013: California, New Hampshire, New Jersey, New York. Since the survey was fielded, an additional four states have obtained SPAs: Hawaii, Kentucky, Nevada, Ohio.
The incentive became effective January 1, 2013, and there is no time limit for states to submit a SPA for preventive services coverage. This option is available to all states, regardless of whether they implemented the Medicaid coverage expansion or not. On February 1, 2013, CMS issued a letter to State Medicaid Directors (SMD# 13-002) which provided details to states on the criteria for submitting a preventive services SPA.1 Specific requirements of the policy outlined in the letter include:
- States must cover all the recommended preventive services and their administration without cost sharing
- The FMAP increase applies only to the preventive services
- States must ensure they have correct codes and modifiers for providers to be able to match services rendered to the USPSTF and ACIP recommendations
- States should have financial monitoring procedures to ensure accuracy in claiming enhanced rate
- If preventive service overlaps with other enhanced reimbursement rates (e.g. temporary increase for primary care services), the 1% FMAP enhancement for preventive services is available for base payment rate from July 1, 2009
- Coverage without cost sharing must be applied to those in fee-for-service and managed care
- To claim the enhanced rate in managed care, states make estimates prospectively based on historical data from managed care plans to the extent possible
- States should have capacity to add/amend services as USPSTF and ACIP add new recommendations or change existing ones
- For 2013, the incentive only applies to services provided by physicians but as of January 1, 2014, will apply to services provide by other licensed practitioners
| Table A1: PREVENTIVE SERVICES DEFINITIONS | |
| Cancer-Related Services (Table 1) | |
| Breast cancer preventive medication counseling | Clinicians discuss chemoprevention with women at high risk for breast cancer and low risk for adverse effects of chemoprevention. |
| Breast cancer mammography* | Screening mammography for women, with or without clinical breast examination, every 1-2 years for women aged 40 and older. |
| BRCA screening and counseling | Genetic counseling and evaluation for BRCA testing for women whose family history is associated with an increased risk for deleterious mutations in BRCA1 or BRCA2 genes. |
| Cervical cancer screening | For women who have been sexually active and have a cervix. |
| Colorectal cancer screening | Using fecal occult blood testing, sigmoidoscopy, or colonoscopy starting at age 50 through 75. |
| STI screenings (Table 2) | |
| Chlamydial infection screening | For sexually active women age 24 and younger and older women who are at increased risk. |
| Gonorrhea screening | For all sexually active women, if they are at increased risk. |
| HIV screening | For all adolescents and adults at increased risk for HIV infection. |
| Syphilis screening | For those at increased risk. |
| STI counseling | High-intensity behavioral counseling to prevent STIs for sexually-active adolescents and adults at risk. |
| Chronic Condition-Related Services (Table 3) | |
| Prophylactic aspirin | For men age 45-79 years and women age 55-79 years, if potential benefit outweighs potential harm. |
| Blood pressure screening | For adults aged 18 and older. |
| Cholesterol abnormalities screening | Men aged 35+ and women aged 45+, and those younger at increased risk of coronary heart disease. |
| Depression screening | Staff-assisted supports to assure accurate diagnosis, effective treatment and follow-up. |
| Diabetes screening | Type 2 diabetes in asymptomatic adults with sustained blood pressure above 135/80 mm Hg. |
| Osteoporosis screening | Routine screening for women aged 65+, age 60 for women at increased risk of such fractures. |
| Health Promotion (Table 4) | |
| Healthy diet counseling | Intensive behavioral dietary counseling, delivered by primary care clinicians or specialists, for those with hyperlipidemia and other risk factors for cardiovascular and diet-related chronic disease. |
| Obesity screening and counseling | Screen all adults for obesity, offer intensive counseling and behavioral interventions to promote sustained weight loss for obese adults. |
| Tobacco use counseling and interventions | Ask all adults about tobacco use and provide tobacco cessation interventions. |
| Alcohol Misuse Counseling | Screening and behavioral counseling interventions in primary care settings. |
| Folic acid supplementation | A daily supplement of 0.4 to 0.8 mg of folic acid for women planning or capable of pregnancy. |
| Immunizations (Tables 5A and 5B) | |
| Tetanus-Diphtheria (Td)booster and Tetanus-Diphtheria-Pertussis (T-dap) | 1 Td Booster every 10 years and a one-time dose of Tdap for those under age 64. |
| Human Papilloma Virus | 3 doses for females age 26 and under. |
| Measles, Mumps, and Rubella | 1 or 2 doses for those 19-49; 1 dose for those 50 and older if other risk factors are present. |
| Varicella | 2 doses for those 19-49; 2 doses for those 50 and older if other risk factors are present. |
| Influenza | 1 annual dose for those 19-49 if other risk factors are present; 1 annual dose for those 50+. |
| Pneumococcal | 1 or 2 doses for those 19-64 if other risk factors are present; 1 dose for those 65 and older. |
| Hepatitis A | 2 doses if other risk factors are present. |
| Hepatitis B | 3 doses if other risk factors are present. |
| Meningococcal | 1 or more doses if other risk factors are present. |
| Zoster | For those 60 and older. |
| Pregnancy-Related Services (Tables 6A and 6B) | |
| Chlamydial infection screening | For all pregnant women age 24 and under and for older pregnant women at increased risk. |
| Gonorrhea screening | For all sexually active women if they are at increased risk. |
| Hepatitis B screening | For pregnant women at their first prenatal visit. |
| Syphilis screening | For all pregnant women. |
| Alcohol misuse counseling | Screening and behavioral counseling interventions to reduce misuse in primary care settings. |
| Anemia screening | For iron deficiency anemia in asymptomatic pregnant women. |
| Bacteriuria screening | For asymptomatic bacteriuria with urine culture at 12 to 16 weeks gestation. |
| Breastfeeding counseling | Interventions during pregnancy and after birth to promote and support breastfeeding. |
| Rh incompatibility screening at first visit | Rh (D) blood typing and antibody testing for all pregnant women during first pregnancy-related visit; repeat for all unsensitized Rh(D) negative women at 24-48 wks unless biological father is Rh(D) negative. |
| NOTES: *HHS uses the 2002 recommendation on breast cancer screening. Survey is based on recommendations from the USPSTF related the ACA provision – http://www.uspreventiveservicestaskforce.org/uspstf/uspsabrecs.htm and the Advisory Committee on Immunization Practices recommendations for adults in 2013 –http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5901a5.htm. | |
| SOURCE: KCMU Survey of State Medicaid Coverage of Adult Preventive Services, 2013. | |
In addition to the services recommended by USPSTF and ACIP, Section 2713 of the ACA authorized the development of an additional set of preventive services for women, to be covered by private insurance plans. A committee of the Institute of Medicine (IOM) developed a set of recommendations for 8 preventive services for women, and these recommendations were subsequently adopted by the federal Health Resources and Services Administration (HRSA), which means that these services must be covered without cost sharing by all new private plans. These services (Table A2) are not included as part of the requirements for the Medicaid enhanced match for preventive services, but they overlap with many of Medicaid’s benefits categories and thus were included in this state-level survey.
| Table A2: PREVENTIVE SERVICES DEFINITIONS | |
| Additional Preventive Services (Tables 7A and 7B) | |
| Routine HIV Screening for Adults | HIV screening for adolescents and adults ages 15-65. Younger adolescents and older adults at increased risk should also be screened. |
| HIV Screening for Pregnant Women | Screening for all pregnant women, including those who present in labor whose HIV status is unknown. |
| Gestational Diabetes | In pregnant women between 24 and 28 weeks of gestation and at the first prenatal visit for pregnant women identified to be at high risk for diabetes. |
| Well Woman Visit | Well-women preventive care visit annually for adult women to obtain the recommended preventive services that are age and developmentally appropriate, including preconception and prenatal care. |
| Breastfeeding support, supplies, and counseling | Comprehensive lactation support and counseling, by a trained provider during pregnancy and/or in the postpartum period, and costs for renting breastfeeding equipment. |
| Human papillomavirus testing (DNA) | High-risk human papillomavirus DNA testing in women with normal cytology results. Screening should begin at 30 years of age and should occur nomore frequently than every 3 years. |
| Screening and counseling for interpersonal and domestic violence | Annual screening and counseling for interpersonal and domestic violence for all women. |
| NOTES: HIV screening services were included in the survey and are discussed in a separate report: https://www.kff.org/hivaids/fact-sheet/state-medicaid-coverage-of-routine-hiv-screening/. Recommendations for all other services in this table are from HRSA Women’s Preventive Services. | |
| SOURCE: KCMU Survey of State Medicaid Coverage of Adult Preventive Services, 2013. | |
Appendix B: Survey Instrument
Kaiser Commission on Medicaid and the Uninsured: Preventive Services Survey
This survey is intended to provide information that is helpful to Medicaid programs as well as the broader policy community about the role Medicaid in the provision of preventive services. Given that preventive services for children are covered under the Early Periodic Screening, Diagnosis, and Treatment (EPSDT) benefit for children, this survey is designed to gather information on preventive services coverage in Medicaid programs for nonelderly adults. This survey was first conducted two years ago by Health Management Associates as part of the biannual update of the Kaiser Commission on Medicaid and the Uninsured Medicaid Benefits Database. The survey report is on the Kaiser Family Foundation web site at: http://www.kff.org/medicaid/8359.cfm.
The revised instrument takes into account the guidance released in the February 1, 2013 State Medicaid Director letter on the option newly available to states under the ACA (Section 4106), effective January 1, 2013, to receive an enhanced federal matching rate for clinical preventive services and immunizations for nonelderly adults if they provide all of these services without cost-sharing. Specifically, states that cover all preventive services rated Grade A or B by the United States Preventive Services Task Force (USPSTF) and immunizations recommended by the Advisory Committee on Immunization Practices (ACIP) without cost-sharing will receive a one percentage point increase in the federal matching rate for those services.
The CMS guidance cited above specifies that the one percentage point increase applies to preventive services and immunizations currently matched at:2
- the regular matching rate for states and the District of Columbia (without regard to the temporary enhanced match for specified primary care codes under ACA section 1202); or
- the enhanced matching rate under the Breast and Cervical Cancer Treatment Program.
The one percentage point increase does not apply to preventive services currently matched at other enhanced matching rates, most notably family planning services. In order for states to collect this one percentage point increase in the federal matching rate, states must submit a state plan amendment (SPA) to CMS and report such expenditures on a separate line of their CMS-64 forms.
The following suggestions may be helpful as you and your staff complete this survey:
- If your state has already submitted or is about to submit a SPA under this provision, please check “Yes” on the first question (provide an effective date if possible) and skip to Section III.
- Responses can be entered in any shaded area.
- To move around the form, you can use the tab key to move forward, shift-tab to move backward, or click any shaded area.
- To make an X in a check box, tab to the box and left-click on the mouse, or hit the space bar. Clicking the mouse or hitting the space bar a second time will remove a check. You can tab past the box if a check is not required.
- Text of any length can be entered in a text box. To start a new line within a text box, hold down the shift key and press return.
Appendix B: Survey Instrument
Endnotes
Executive Summary
The survey instrument was developed based on recommendations from the USPSTF related the ACA provision - http://www.uspreventiveservicestaskforce.org/uspstf/uspsabrecs.htm and the Advisory Committee on Immunization Practices recommendations for adults in 2010 -http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5901a5.htm.
Eight of these services (see Appendices 8A and 8B) were either recommended by HRSA or under review by USPSTF at the time of the survey following the Institute of Medicine’s (IOM) release of a report commissioned by the US Department of Health and Human Services (HHS) stating that there is a gap in preventive services covered by insurance companies for women. For more information please see Women's Preventive Services Guidelines and Clinical Preventive Services for Women: Closing the Gaps.
The HRSA women’s preventive services are not required for states to receive the enhanced match, but were included in the survey because they have been recommended as important to fill in gaps in preventive care for women and overlap with many of Medicaid’s benefits categories.
Introduction
KCMU/Urban Institute estimates based on data from FY 2010 MSIS and CMS-64. MSIS FY 2009 data were used for CO, MO, NC, and WV, but adjusted to 2009 CMS-64.
KCMU (2013). What Difference Does Medicaid Make? https://www.kff.org/wp-content/uploads/2013/05/8440-what-difference-does-medicaid-make2.pdf
Preventive Services Covered by Private Health Plans under the Affordable Care Act. Kaiser Family Foundation. https://www.kff.org/health-reform/fact-sheet/preventive-services-covered-by-private-health-plans/
CMS. (2013). http://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-Releases/2013-Press-Releases-Items/2013-12-17.html
The survey instrument was developed based on recommendations from the USPSTF related the ACA provision - http://www.uspreventiveservicestaskforce.org/uspstf/uspsabrecs.htm and the Advisory Committee on Immunization Practices recommendations for adults in 2010 - http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5901a5.htm.
The survey instrument was developed based on recommendations from the USPSTF related the ACA provision - http://www.uspreventiveservicestaskforce.org/uspstf/uspsabrecs.htm and the Advisory Committee on Immunization Practices recommendations for adults in 2010 -http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5901a5.htm.
Eight of these services (see Appendices 8A and 8B) were either recommended by HRSA or under review by USPSTF at the time of the survey following the Institute of Medicine’s (IOM) release of a report commissioned by the US Department of Health and Human Services (HHS) stating that there is a gap in preventive services covered by insurance companies for women. For more information please see Women's Preventive Services Guidelines and Clinical Preventive Services for Women: Closing the Gaps.
Key Findings
Survey Findings
Timothy Westmoreland, Director, Centers for Medicare and Medicaid Services, State Health Official Letter, January 4, 2001, http://downloads.cms.gov/cmsgov/archived-downloads/SMDL/downloads/sho010401.pdf
CDC. (2013). Incidence, Prevalence, and Cost of Sexually Transmitted Infections in the United States.
The survey findings reported here reflect whether a state covers HIV screenings for adults at increased risk for HIV infection and routine HIV screening for adults. For more information HIV screenings – see the following brief: State Medicaid Coverage of Routine HIV Screening. Kaiser Family Foundation, February 2014. https://www.kff.org/hivaids/fact-sheet/state-medicaid-coverage-of-routine-hiv-screening/
The Role of Medicaid for Adults with Chronic Illnesses. Kaiser Commission on Medicaid and the Uninsured. https://www.kff.org/wp-content/uploads/2013/01/8383.pdf
Farley, Thomas A. et al. “Deaths Preventable in the U.S. by Improvements in the Use of Clinic Preventive Services.” American Journal of Preventive Medicine, Vol. 38 no. 6, 2010. http://download.journals.elsevierhealth.com/pdfs/journals/0749-3797/PIIS0749379710002072.pdf.
Maciosek, Michael V. et al. "Greater Use of Preventive Services in U.S. Health Care Could Save Lives at Little or No Cost," Health Affairs, Vol. 29 no. 9, September 2010. http://content.healthaffairs.org/content/29/9/1656.full.pdf.
Twenty-eight states covered both healthy diet counseling and obesity screening and counseling services; Alaska reported coverage for obesity screening and counseling but not healthy diet counseling. The 7 states that charged cost-sharing for these services were IA, KY, MO, MT, ND, PA, and VA. Additionally, AK reported charging cost-sharing for obesity screening and counseling.
Cynthia L. Ogden, Margaret D. Caroll, et al. Prevalence of Childhood and Adult Obesity in the United States, 2011-2012. Journal of the American Medical Association (February 26, 2014,) http://jama.jamanetwork.com/article.aspx?articleid=1832542.
CDC. 2000. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr4916a1.htm
Guttmacher Institute. (2013). Public Costs from Unintended Pregnancies and the Role of Public Insurance Programs in Paying for Pregnancy and Infant Care.
IOM. (2011). Clinical Preventive Services for Women: Closing the Gaps.
HRSA. (2014). Women's Preventive Services Guidelines.
Hawaii did not provide a response for screening for gestational diabetes, contraceptive methods and counseling, and well woman visit.
KCMU, Premiums and Cost-Sharing in Medicaid: A Review of Research Findings, February 2013.
Appendices
CMS. (2013). http://www.medicaid.gov/Federal-Policy-Guidance/downloads/SMD-13-002.pdf
The guidance states that the one percentage point increase also applies to the enhanced federal match rate for those newly eligible for Medicaid coverage due to the Medicaid expansion. Since the federal match rate cannot exceed 100 percent, the one percentage point increase will not apply to this match rate until January 1, 2017, when the federal match for the newly eligible will first drop below 100 percent.