Almost One in Four Adult Workers is Vulnerable to Severe Illness from COVID-19
As states and employers continue to reopen businesses and public offices, important decisions are being made about how to keep workers safe from becoming infected with coronavirus at work or on their commutes to and from their homes. In addition, outbreaks of coronavirus at some businesses, such as food processing facilities and long-term care facilities, highlight the risks faced by essential workers who have continued to work outside the home. Safety considerations will be particularly important for those workers at greater risk of becoming seriously ill if they become infected with coronavirus. This caution applies to older workers in general, as well as to younger workers with certain medical conditions that put them at higher risk of serious illness if they become infected.
We use the National Health Information Survey (NHIS) to look at how many adult workers1 are at increased risk of severe illness if infected with coronavirus, based on risk factors identified by the Centers for Disease Control and Prevention (CDC). These risk factors include having diabetes, chronic obstructive pulmonary disease (COPD), heart disease, a body mass index (BMI) above 40, moderate to severe asthma, and a functional limitation due to cancer. All workers 65 and older also are considered at higher risk. The approach is similar to our prior work identifying at-risk adults and is described in more detail in the Methods.
Who are the At-Risk Workers?
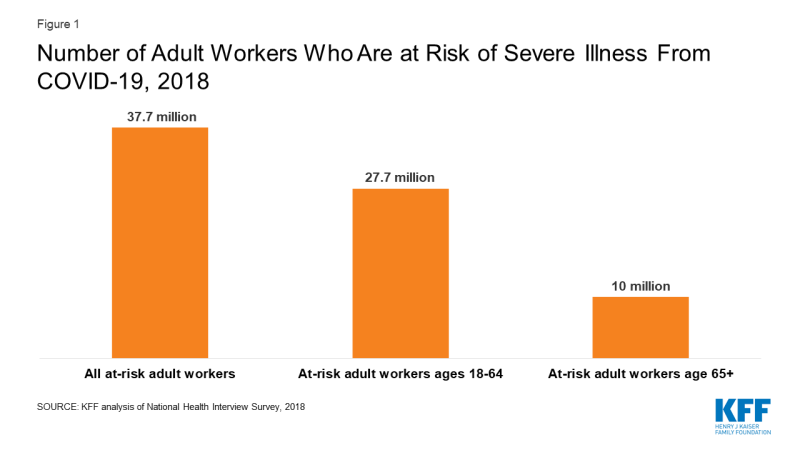
We find that over 90 million adults are at greater risk for severe illness from COVID-19 due to underlying health conditions or age. Of these at-risk adults, we estimate that about 37.7 million were employed at a job or business in the prior year, including 10 million people age 65 and older (19.5% of adults age 65 and older, all of whom are considered at greater risk) and 27.7 million non-elderly adults (Figure 1). These at-risk workers comprise 24% of all adult workers.
Among non-elderly adult workers, at-risk workers are older on average than non-elderly workers who are not at risk (average age of 45 versus 40), reflecting the fact that risk status chronic conditions or poor health increases with age. One-half of at-risk non-elderly adult workers are women, which is higher than the percentage (46%) of non-elderly adult workers who are not at risk.
Large shares of at-risk workers — 86% of non-elderly adult at risk workers and 61% of age 65 and older at-risk workers — work full-time (at least 35 hours per week). They have substantial connection to work and may face economic difficulties remaining absent from their jobs even if safety is a question.
The average annual earnings of non-elderly adult at-risk workers was $48,400 in 2018, somewhat lower than the average annual earnings for non-elderly adults workers who were not at risk ($51,900). The median annual earnings was $40,000 for both at-risk and not-at-risk adult non-elderly workers. One-quarter of non-elderly adult at-risk workers had annual earnings of less than $21,100.
The average annual earnings of workers age 65 and older was $49,100 in 2018; median annual earnings were $37,000. One-quarter of workers age 65 and older had annual earnings of less than $17,300.
The importance of at-risk workers’ earnings to themselves and to their families may put added pressure on them to continue to work or return to work even if their safety may be compromised. Not surprisingly, among both non-elderly at-risk workers and workers age 65 and older who live alone, earnings on average account for a very large share of their total annual incomes: 94% among non-elderly at-risk workers and 72% among older at-risk workers in 2018. For those living with others, the at-risk worker’s earnings on average comprised a substantial share of family income. Among non-elderly at-risk workers, their earnings accounted for 57% of family income in families of two or three and 50% in larger families. Among workers age 65 and older who live with others, the older worker’s earnings on average comprised 48% of family income.
Discussion
Most people, including at-risk workers, cannot afford to stay away from work for long periods of time. Some people at risk have likely continued to go to work outside their homes due to the nature of their jobs, perhaps as essential workers. Others may have been accommodated by remote work, which has taken hold to a remarkable degree but is not available to all workers. Some have lost their jobs or may be at risk of losing them. As more workplaces reopen there will be increasing pressures for all workers, including those at higher risk, to return to jobs or seek new jobs outside of their homes. This will raise issue both for employees concerned about their safety and for employers concerned about how to keep these workers safe.
In addition to at-risk people who are workers themselves, there are millions more at-risk adults who themselves are not workers but who live with workers. This indirect exposure could be just as serious of a risk as going to work themselves. We estimate that an additional 12 million at-risk adults who are not workers themselves live with at least one full-time worker. This includes 6.5 million people age 65 and older and about 5.5 million at risk non-elderly adults. This is a conservative estimate because additional non-working at-risk adults live with people who work part time or who are in and out of the work force. The safety of these family members will need to be part of the considerations for employees and employers as businesses continue to refine safety protocols and others reopen their workplaces.
State and local governments and employers themselves are wrestling with how to reopen businesses in the safest ways possible, with risks particularly high for workers who have pre-existing that make them more vulnerable to severe illness from COVID-19. Employers, workers, and governments may need to consider flexible and creative approaches to balance safety and business needs, but with such large number of workers meeting vulnerability criteria, there will be a continuing tension between the economic pressures facing families and businesses and the health and safety of millions of people.
Methods
This analysis uses data from the 2018 National Health Interview Survey (NHIS) to look at the share of workers who would be at increased risk of becoming seriously ill if they become infected with COVID-19. The analysis is similar to our previous [work], where we used the Behavioral Risk Factor Surveillance Survey (BRFSS) to estimate the number of adults who would be at increased risk if they were infected with coronavirus. In that study, we found that about 21% of non-elderly adults have one more of five risk factors that the Centers for Disease Control and Prevention (CDC) have identified as increased risk factors for those infected with coronavirus. The factors we were able to analyze were having diabetes, chronic obstructive pulmonary disease (COPD), heart disease, a body mass index (BMI) above 40, and asthma. In addition, the CDC criteria consider all people over age 65 to be at increased risk. In this brief we use similar information from the 2018 National Health Interview Survey (NHIS) to look at the share and characteristics of adults with these risk factors who are in the workforce.
We use NHIS rather than BRFSS for this analysis because it has more information about the earnings, income and family characteristics of the at-risk population, providing a fuller picture of the economic circumstances of these workers. The sample adult file in NHIS contains information about all of the same health conditions that we used in the previous study, plus the person file has information that allows us to include people who report being functionally limited due to cancer; CDC includes people with compromised immune systems, such as people undergoing treatment for cancer, as being at higher risk of serious illness if infected with coronavirus. With NHIS we find that 22% of non-elderly adults have one or more risk factors for becoming seriously ill with COVID-19, essentially the same share as we calculated under BRFSS. Including those with a functional limitation due to cancer accounts for less than one-half percentage point of this estimate. We note that one downside of using NHIS is that state-level analysis is not possible.
As with BRFSS study, the analysis identifies non-elderly people with one or more risk factors, but in two steps. One pass excludes asthma and the other includes it, and we use only a portion (62%) of the people whose only risk factor is asthma. Unlike our BRFSS analysis, here we incorporate the proportion by assigning risk status to 62% of those whose only risk factor is asthma. The assignment is done by sampling from the asthma risk only group in a way that increases the likelihood of selection with age. (See Zein et al.)
The purpose of the analysis is to look at people who may have difficult avoiding or delaying work if their safety may be compromised; we therefore attempted to focus the analysis on those with a significant amount of work, which we defined as workers who earned $5,000 or more at a job or business during the previous year. This threshold includes 94% of non-elderly adults and 88% of people age 65 and older with any work in the previous year.
We imputed full-time or part-time status for some observations with missing values. NHIS provides a file that multiply imputes family income, earnings and work status for survey respondents. This results in cases in which employment status and earnings are imputed for people who did not otherwise report being employed. Although NHIS contains several questions about hours worked (either in the previous period or usually), these questions do not contain information for respondents who were imputed to be workers and to have earnings. We imputed part-time/full-time status based on their annual earnings, separately for workers under age 65 and those 65 and older. More specifically, for cases where we had information on earnings and hours worked, we calculated the relative proportions of part-time and full-time workers in several earnings groups. We then randomly imputed yes or no for full-time status for the missing cases, using the probabilities associated with their income levels.
We calculated the share of earnings to family income, segmented by family size. For this analysis, we wanted to calculate the ratio for each worker in order to determine the importance of that worker’s earnings to the family. Doing this can create issues in cases where earnings are larger than family income, which can result in very high ratios of earnings to income, which inflate the overall average. To limit the impact of these situations, we capped the ratio associated with any worker to 1 (a worker’s earnings can account for 100 percent of family income but not more than that). A second issue is that the family incomes for some workers with significant earnings can be very low or even zero. This was the case for a small number of observations of at-risk workers (between 6 and 12 unweighted cases had earnings of $5000 or more and family income of less than $1,000. We excluded those cases when we calculated the ratios.
Endnotes
A person is considered to be a worker if they were employed at a job or business in the previous year and had at least $5,000 in annual earnings.