Tennessee’s Money Follows the Person Demonstration: Supporting Rebalancing in a Managed Long-Term Services and Supports Model
MFP in Tennessee’s Capitated MLTSS Program
Through CHOICES, Tennessee provides its Medicaid MCOs with a fully blended capitation payment to cover all of the physical, behavioral health, and LTSS (including both NFs and HCBS for NF level of care (LOC) eligible individuals) needed by beneficiaries. CHOICES beneficiaries are assigned to one of three groups:
- CHOICES Group 1 includes individuals who meet a NF LOC and receive institutional care;
- CHOICES Group 2 includes seniors (age 65 and older) and adults (age 21 and older) with physical disabilities who meet a NF LOC and receive HCBS; and
- CHOICES Group 3 includes seniors and adults with physical disabilities who qualify for TennCare as Supplemental Security Income recipients, who do not meet a NF LOC, but who, in the absence of HCBS, are at risk of NF placement.1
While there is an enrollment target (which functions as a cap) for CHOICES beneficiaries who receive Medicaid HCBS, Tennessee has been able (except for a brief period while awaiting approval from the Centers for Medicare and Medicaid Services to increase the target) to keep pace with the need, eliminate a waiting list for HCBS, and significantly expand the number of beneficiaries receiving HCBS as well as the percentage of beneficiaries receiving LTSS in home and community-based settings versus institutional settings. Further, pursuant to the terms and conditions of the state’s Section 1115 demonstration waiver implementing CHOICES, beneficiaries transitioning from a NF receive HCBS even if the CHOICES HCBS enrollment target has been reached, as do certain CHOICES beneficiaries who would be at risk of NF placement absent the provision of HCBS.
To enroll in MFP, beneficiaries must reside in a NF for at least 90 days prior to transitioning to a community-based setting. Upon transition, Tennessee seniors and adults with physical disabilities who continue to require a NF LOC are simultaneously enrolled in MFP and CHOICES Group 2 to receive HCBS. (Beneficiaries who transition from a NF into the CHOICES at-risk Group 3 receive HCBS but are ineligible for MFP as they no longer require a NF LOC.)
MCO Financial Incentives for Nursing Facility to Community Transitions
Capitated Payments
Tennessee’s CHOICES MCOs receive the same blended monthly capitated payment for all beneficiaries who meet a NF LOC (CHOICES Groups 1 and 2), regardless of whether those beneficiaries reside in NFs or receive HCBS. This rate is based on the historical mix of NF and HCBS used by the population enrolled and also takes into account some projected change in the service mix over time (as MCOs focus on serving more beneficiaries in the community when appropriate). Since, in most situations, the cost of institutional care is significantly higher than that of supporting a beneficiary in a community setting, MCOs have a strong financial incentive to minimize the time that Medicaid beneficiaries spend in NFs and to help those who can do so return to the community and remain there for as long as possible, even if they continue to meet an institutional LOC. Capitation payments for beneficiaries considered at risk of NF placement without the provision of HCBS (CHOICES Group 3) reflect the relatively lower cost associated with serving individuals who do not need an institutional LOC.
MFP Bonus Payments
To further prioritize institution-to-community transitions for MFP-eligible beneficiaries, Tennessee also provides specific financial incentives to MCOs for meeting certain MFP benchmarks (Text Box 2), which are detailed in the MCO contracts and listed below in Text Box 3.2 As a result, state officials believe that MCOs are more focused on reaching transition goals and note that MCOs have developed “transition teams” that concentrate on increasing MFP enrollment. These teams work along with state MFP staff to ensure that NF residents who desire to transition to the community can do so and in as timely a manner as possible.
| Text Box 2: State MFP Benchmarks |
|
| Text Box 3: MFP Incentive Payments to CHOICES MCOs |
|
MFP Outreach and Enrollment
CHOICES MCO care coordinators are responsible for regularly assessing NF residents’ interest in and potential for transitioning to the community. The MCO care coordinators are nurses and social workers, many of whom have experience working in hospitals, managed care systems and Section 1915(c) HCBS waivers. Once a CHOICES NF resident is identified as a potential candidate for community transition (based on his/her desire to receive HCBS and ability to transition), the MCO care coordinator assesses whether the member is a candidate for transition to the community, and if so, whether the member is also an MFP-eligible individual. The MFP eligibility criteria include: (1) residing in an institutional setting for at least 90 days, (2) transitioning into an MFP qualified residence, and (3) signing an attestation stating a willingness to participate in MFP. If the transitioning member does not meet all three of the above criteria, they would not qualify to enroll in MFP but would still transition into Group 2 with CHOICES services without simultaneous enrollment in MFP. Outreach efforts are focused on helping beneficiaries understand Tennessee’s MFP demonstration and why the program is valuable for LTSS system change within the state. Referrals to Tennessee’s MFP program come from a variety of sources, including beneficiaries themselves, family members, the Minimum Data Set 3.0 Section Q process,3 and NF staff.
MFP Care Coordination and Services
Transition and Care Planning
Once a beneficiary is identified for MFP, she works with a CHOICES MCO care coordinator to develop a transition plan that includes needs and risk assessments, a care plan, and a home safety check. MCOs must develop a risk agreement as part of the person-centered care planning process for all CHOICES HCBS beneficiaries, including MFP participants. This includes identifying the potential risks of receiving LTSS in a home and community-based (rather than institutional) setting; determining the potential consequences of the risks; developing and implementing strategies to mitigate the risks; and documenting and supporting the beneficiary’s informed decision to accept a reasonable degree of risk in living more independently in the community. Beneficiaries can receive HCBS so long as their needs can be safely met in a community setting at a cost that does not exceed institutional care.
The care plan takes into account a beneficiary’s physical and behavioral health needs, unpaid natural supports (e.g., a family caregiver), and other personal health care-related circumstances and details the type and amount of HCBS to be provided to ensure that the beneficiary’s needs are met in the community. During the transition planning period, CHOICES/MFP beneficiaries who need assistance in securing housing work with MCO care coordinators and the MFP housing specialist to complete housing searches or make connections with community-based housing providers. Prior to a beneficiary’s transition to the community, the MCO care coordinator assists the member as needed to ensure that essential household items (such as kitchen appliances, linens, etc.) are in place or purchased, necessary home modifications are completed, and utilities are set up. MCOs are permitted to offer a transition allowance of up to $2,000 in order to help a member who needs assistance in securing these items.
Prior to the member’s transition, the CHOICES MCO care coordinator will conduct an on-site evaluation of the physical residence and meet with the member’s family or other caregiver (as applicable). After the member transitions, CHOICES MCO care coordinators must visit the member face-to-face within 24 hours after transition if the member will live alone or call within 24 hours and visit face-to-face within seven days if the member will be living with family or in a Community-Based Residential Alternative (CBRA). After the initial 90 days of community living, the MCO care coordinator is required to have at least monthly contacts and quarterly face-to-face visits with each beneficiary. During these contacts, the MCO care coordinator assesses the beneficiary’s care quality, quality of life, and living environment. These regular assessments continue after the 365-day MFP participation period ends, through the CHOICES program.
Services
The HCBS benefit package is the same regardless of whether CHOICES beneficiaries also participate in MFP. In designing the MFP services package, Tennessee wanted to avoid any care disruptions for CHOICES/MFP beneficiaries at the end of their 365-day MFP participation period; after MFP, beneficiaries remain enrolled in CHOICES and continue to have access to the same array of HCBS as they did while they were MFP participants. The following is a selected list of HCBS available in the CHOICES program:
- Adult day care services
- Assistive technology
- Attendant care services
- Community-Based Residential Alternatives
- Home-delivered meals
- In-home respite care
- Inpatient respite care
- Minor home modifications
- Personal care services
- Personal emergency response systems
Beneficiary Self-Direction of Services
Nearly all MFP programs nationwide promote beneficiaries’ self-direction of services. Tennessee offers self- direction (called “consumer direction” in Tennessee) for CHOICES beneficiaries, including those enrolled in MFP. The self-direct program follows an employer authority model, allowing CHOICES beneficiaries to direct and manage certain aspects of the provision of services, including, primarily, the opportunity to recruit, hire, and supervise direct service workers. Prior to CHOICES, there were no options for seniors and adults with physical disabilities to self-direct their services in Tennessee. Now, about 8.5 percent of the CHOICES HCBS population is enrolled in the self-direction model. Self-direction program participation is lower among CHOICES members enrolled in MFP (3.2%) than in the CHOICES program as a whole, but Tennessee has seen an increase in MFP beneficiaries choosing to self-direct services since 2012. The state hopes to continue to increase the utilization of self-direction among CHOICES/MFP participants as well as traditional CHOICES HCBS participants; there is an MFP benchmark in place in to track progress in this area.
Service Delivery and Back-Up Plans
Under CHOICES, delivery of HCBS is monitored at the beneficiary-level on an ongoing basis through the use of an electronic visit verification system, which MCOs are required to maintain. This system requires direct care workers to log in at the beginning of each visit, and if a worker does not arrive as scheduled, an alert is generated to the provider agency as well as the MCO, with both entities obligated to take immediate action to resolve the potential gap in care.
Another key feature of Tennessee’s CHOICES program includes access to a 24-hour back-up assistance to prevent a lapse in the provision of essential medical and supportive services or other circumstances that could negatively affect a beneficiary’s health or welfare. There is an oversight process in place to ensure that the back-up strategy is working as intended. In addition to specifying the services and supports that he/she will receive, the beneficiary’s care plan includes a daily care schedule. The care coordinator develops the care plan in conjunction with each member, and then the MCOs create authorizations based on the approved schedule in the care plan. Each CHOICES beneficiary’s care plan also includes a back-up plan that describes specifically how the beneficiary’s service and support needs will be met if a direct care worker does not arrive as scheduled to ensure the beneficiary’s continued health and safety. The back-up plan includes the names and telephone numbers of persons and/or agencies to contact as well as the services and supports provided by each. The MCO care coordinator is responsible for ensuring that all individuals included in the back-up plan are willing and able to fulfill their assigned roles and responsibilities. For beneficiaries who self-direct their services, the Fiscal Employer Agency (FEA) is responsible for helping the member develop the initial back-up plan. The MCO care coordinator is responsible for assessing the adequacy of the beneficiary’s back-up plan, and for helping the member update the plan as needed on an ongoing basis. If the back-up plan is deemed inadequate, the MCO care coordinator is responsible for following up with the beneficiary and the FEA until all concerns have been addressed.
MCOs are also required to provide access to a call center, 24 hours a day, 7 days a week, to assist beneficiaries in accessing needed medical, behavioral health, and LTSS. The MCO call center is staffed with nurses who triage urgent care and emergency calls and facilitate the transfer of calls to the care coordinators. In addition, MCOs are required to designate a staff member to work with the state Medicaid program’s managed care call center staff for immediate resolution of service issues. The state Medicaid managed care call center also operates 24 hours a day, 7 days a week to help beneficiaries navigate service delivery issues and/or the appeals process.
MFP Staffing and Key Partnerships
Three full-time MFP staff members – a project manager, a data specialist, and a housing specialist – manage Tennessee’s MFP program in conjunction with other state LTSS Division leadership. Each staff member provides technical assistance to the CHOICES MCOs, and the state communicates with MCO care coordination team leaders on a weekly basis at minimum. Tennessee’s MFP project director oversees strategic development and regulatory compliance efforts. The data specialist manages the MFP database that is used primarily to track a potential MFP candidate’s movement through the enrollment process. Data collection is accomplished via an online LTSS eligibility/enrollment workflow management system, and MFP enrollment and expenditure data is fully integrated into the State’s Medicaid Management Information System. The housing specialist is charged with improving communication and coordination between MCOs and affordable housing resources across the state. For example, the housing specialist holds monthly phone calls with MCO staff to discuss complex transition cases and provide guidance on available options that best meet MFP participants’ needs. Key partnerships with Tennessee’s MFP program include:
Area Agencies on Aging and Disability (AAADs): Tennessee’s Medicaid program contracts with the state’s nine AAADs, which function as regional Single Points of Entry (SPOE) into the state Medicaid LTSS system and facilitate eligibility and enrollment. In addition to providing information about the CHOICES program, AAADs explain enrollment processes, including financial and categorical eligibility criteria, conduct individual functional assessments, and facilitate submission of Medicaid applications to both the state Medicaid LTSS Division for LOC determinations and the state Department of Human Services for financial eligibility determinations.4 In addition to their role as regional SPOEs, AAADs conduct the MFP Quality of Life (QoL) surveys (described below). AAADs were chosen to administer the QoL surveys because of their long-standing experience in working with Medicaid beneficiaries who receive HCBS.
Memphis Center for Independent Living (MCIL): In an effort to enhance MFP beneficiaries’ transition experience, Tennessee contracts with MCIL for statewide peer-to-peer training of individuals who will transition from NFs to HCBS. These peer volunteers, who are people with disabilities who have either transitioned from an institutional setting or live independently in the community, provide information about the Medicaid program, the Americans with Disabilities Act, and subsidized housing. In addition, peers help MFP candidates develop skills such as self-advocacy, personal budgeting, and, for individuals participating in self-direction, direct support staff management.
Tennessee Housing Development Agency (THDA): TennCare collaborated with Tennessee’s housing finance agency, the Tennessee Housing Development Agency (THDA), to create a pilot project that will provide a “bridge” rental subsidy from the time that the beneficiary leaves an institution until a permanent rental subsidy can be secured. Pilot program participants will have access to CHOICES care coordinators as they explore more permanent subsidized housing options, and the pilot will be funded through both the THDA Housing Trust Fund and the state’s MFP rebalancing funds.
MFP Housing Steering Committee: The MFP Housing Steering Committee works to expand access to community-based housing for individuals with LTSS needs. This housing committee is comprised of representatives from TennCare CHOICES MCOs, AAADs, low-income housing finance groups, low-income housing builders, public housing authorities, and beneficiary advocates. Committee members meet in-person on a quarterly basis, and the MFP housing specialist contacts committee members individually or as a group by phone or e-mail for guidance and resources as needed. For example, the MFP housing specialist has utilized the expertise of individual members when issues arose with individual CHOICES beneficiaries, such as assistance with identification of housing resources in specific geographic areas. Additionally, MFP staff have worked with the steering committee to address barriers and program details related to starting the THDA supportive housing pilot discussed above and sought input in structuring the first TennCare Housing Conference in October 2013. This conference brought together low-income housing providers and TennCare CHOICES MCOs, with the goals of joint education and troubleshooting barriers associated with obtaining affordable accessible housing for beneficiaries transitioning from institutional settings.
LTC Ombudsman Program: Tennessee’s LTC Ombudsman Program is operated by the state Commission on Aging and Disability. District LTC Ombudsmen and a statewide network of volunteer Ombudsmen assist residents of NFs or CBRAs with questions and concerns about services and play a critical role in facilitating large scale transitions, including transitions to community-based settings following the closure of an institution. Ombudsmen, in addition to assisting LTSS beneficiaries in understanding and exercising their rights and responsibilities, also advocate on behalf of LTSS beneficiaries residing in institutions or CBRAs.
Quality and Evaluation
Surveys and Performance Measures
As required by the MFP grant, Tennessee administers the QoL surveyto consenting beneficiaries at three specific timeframes: approximately 10 days prior to discharge from the institution, 11 months post-discharge and 24 months post-discharge. The QoL survey measures MFP participant’s perceptions and feelings across several domains, including life satisfaction, quality of care, and community life. Current contact information for each beneficiary is tracked through the state Medicaid program’s IT system, which has been customized to capture beneficiary-specific demographic information. MCOs have access to this system and must update beneficiary demographic information within two business days of notification of change.
The quality strategy for CHOICES is part of the integrated quality management strategyfor the entire TennCare program, and includes:
- Uniform measures of system performance;
- Detailed reporting requirements;
- Ongoing audit and monitoring processes;
- Measures to immediately detect and resolve problems, including gaps in care (e.g., Electronic Visit Verification);
- Independent review by an External Quality Review Organization and the Tennessee Department of Commerce and Insurance;
- A key focus on member perceptions of quality, including a modified QoL survey for LTSS members beyond MFP participants; and
- Advocacy for members across MLTSS system.
Certain LTSS performance measures were carried forward from Section 1915(c) HCBS waiver assurances and sub-assurances, including areas such as LOC (e.g., initial and annual LOC evaluations), care plan (e.g., freedom of choice, timely development and initiation of services, annual review, missed and late visits), qualified providers (e.g., credentialing and re-credentialing), health and welfare (e.g., timely reporting, investigation of critical incidents, member education regarding how to report abuse/neglect), and participant rights (e.g., notice of right to appeal any adverse action). Now that Tennessee provides HCBS to seniors and adults with physical disabilities through a Section 1115 exclusively, the state continues to monitor these areas and strives to ensure prompt remediation of individual findings and to promote systemic improvements in the MLTSS delivery system. All MCOs are required to maintain National Committee on Quality Assurance accreditation, and other performance measures will be added as new standardized MLTSS program measures are developed.
Critical Incident Reporting
CHOICES MCOs are responsible for developing and implementing a critical incident reporting and management system for incidents that occur in HCBS settings, including:
- Unexpected death of a CHOICES beneficiary;
- Suspected physical or mental abuse of a CHOICES beneficiary;
- Theft or financial exploitation of a CHOICES beneficiary; and
- Severe injury sustained by a CHOICES beneficiary.
MCOs must review, track, and analyze critical incident reports to identify and address potential and actual care quality and/or health and safety issues. Specifically, MCOs must review the number and types of incidents and findings from investigations; identify trends, patterns, and opportunities for improvement; and develop and implement strategies to reduce the occurrence of incidents and improve the quality of HCBS.
MCO-contracted HCBS providers are required to report critical beneficiary incidents, and, along with MCO care coordinators, are contractually obligated to take necessary steps to prevent further harm to beneficiaries and to respond to any emergency needs. For beneficiaries who elect to self-direct services, the MCO care coordinator is responsible for conducting investigations and working with the beneficiary and the FEA to take necessary steps to respond to critical incidents.
MCOs submit a quarterly CHOICES HCBS Critical Incidents Report to the Tennessee state Medicaid agency, which provides information, by month, about specified measures pertaining to MCOs’ management of critical incidents. State staff review incident management data and also conduct critical incident audits to ensure timely and appropriate remediation of individual issues. Additionally, they identify potential opportunities for systemic improvements and work with MCOs to address individual beneficiary or broader systemic concerns.
Institutional to Community Transition Progress in Tennessee
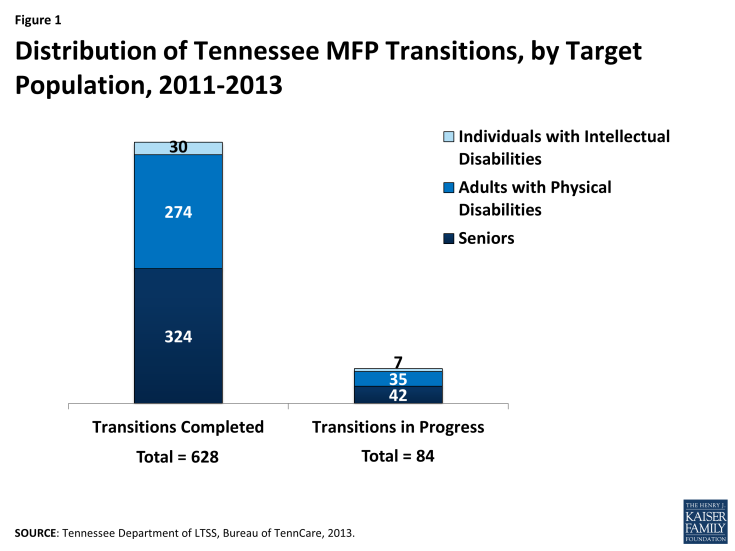
From the implementation of Tennessee’s MFP program on October 1, 2011 through June 30, 2013, 628 beneficiaries transitioned to the community through MFP. Of those, 598 were seniors and adults with physical disabilities simultaneously enrolled in the CHOICES MLTSS program (the remaining 30 beneficiaries simultaneously enrolled in MFP and a fee-for-service HCBS waiver for people with ID. As of June 30, 2013, another 77 NF residents were in the process of transitioning to the community via MFP as CHOICES participants (Figure 1). In comparison, during that same time period, 1,069 beneficiaries transitioned home through CHOICES, without enrolling in MFP.
Table 1 shows the total number of transitions by population group in Tennessee’s MFP program. Seniors and adults with physical disabilities are the target groups most likely to transition as MFP participants as the number of persons with ID residing in institutions is significantly less. While the average age of a Tennessee MFP participant is 65 years old, beneficiaries of all ages – from age 21 to 101 – have transitioned to community-based care under Tennessee’s MFP program. One MFP participant, a person with ID, had been institutionalized for 60+ years.5
| Table 1. Cumulative Tennessee MFP Transitions by Population, as of June 30, 2013 | ||||
| Total | Seniors | Persons with Physical Disabilities | Persons with Intellectual Disabilities | |
| Cumulative Transitions Completed | 628 | 324 | 274 | 30 |
| Transitions in Progress | 84 | 42 | 35 | 7 |
| Rate of Reinstitutionalization | 10 | 7 | 3 | 0 |
| Average Age of MFP Participants | 65 | 77 | 53 | 51 |
| Average Number of Days to Transition to Community | 31 | 26 | 32 | 83 |
| Housing Option Most Likely to Transition To | Home owned or leased by beneficiary or family member | Home owned or leased by beneficiary or family member | Home owned or leased by beneficiary or family member | Supported Living Home |
| SOURCE: Bureau of TennCare, Division of LTSS, June 2013. | ||||
The entire transition process for Tennessee MFP participants – from initiation in the NF to the date of relocation to the community– took 31 days on average to complete (the national average is 3.5 months6) with significant variation by target population. On average, persons with ID (who are not served through CHOICES MLTSS in Tennessee) were in the pre-transition stage for 83 days, while seniors transitioned in 26 days. MFP participants with ID most frequently transitioned to CBRA settings, while CHOICES/MFP participants primarily transitioned to a house owned or leased a family member.
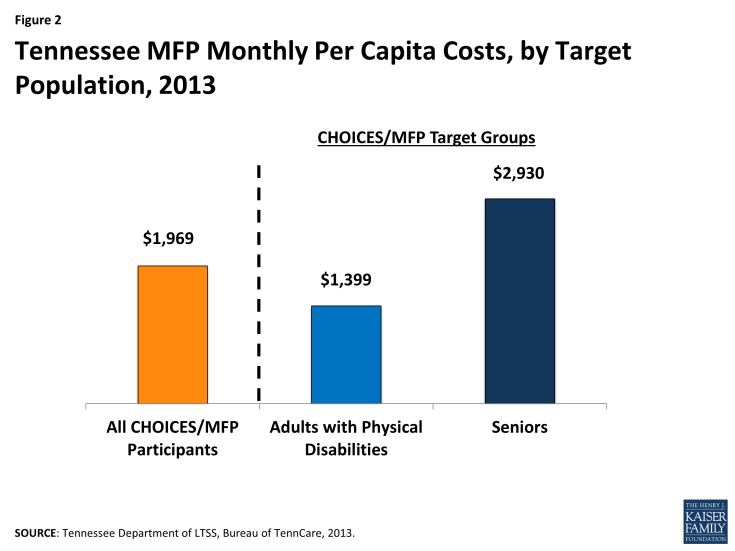
On average, it costs the state $1,969 per month to serve a CHOICES/MFP participant in the community (Figure 2).7 MFP participants who are seniors are less expensive to serve in the community than adults with physical disabilities ($1,399 and $2,930 per month, respectively). Across all CHOICES/MFP target populations, the average monthly HCBS expenditures are higher than those for non-MFP HCBS beneficiary populations and lower than those for Medicaid LTSS beneficiaries served in institutional settings (e.g., $3,710 per month to serve individuals in NFs).
The average reinstitutionalization rate of MFP participants in Tennessee, including persons with ID, was about 10 percent. Reinstitutionalization is defined as returning to a NF, hospital, or Intermediate Care Facility for Individuals with Intellectual Disabilities, regardless of length of stay, during the beneficiary’s MFP participation year. Nationally, states reported an average reinstitutionalization rate of 11 percent across all MFP populations.8
In 2011 and 2012, Tennessee achieved its MFP transition benchmarks; as of August 2013, MCOs reported being behind on their state-set annual transition goals for 2013. Some of this lag can be attributed to the fact that on July 1, 2012, Tennessee changed its Medicaid NF LOC criteria to target NF services to beneficiaries with higher acuity care needs, while continuing to make HCBS more broadly available to beneficiaries who do not meet the new more stringent LOC standards (i.e., Group 3 beneficiaries). As a result, the state has diverted nearly 20 percent of all NF applicants to more cost-effective and integrated community-based care.
In order to improve transition rates and meet its 2013 MFP transition benchmark, Tennessee is pursuing additional strategies to better support the remaining higher acuity NF population during transition and in the community. Examples of these strategies include the following:
- Developing a set of “best practices” that includes the most effective MCO staffing models such as transition teams, data-driven methods of MFP candidate identification, and use of natural and community-based supports, other outside resources, and community partners to improve MFP transition successes. These best practices were disseminated to all MCOs for use in developing their internal processes and enrollment strategies;
- Statewide peer-to-peer trainingfor beneficiaries transitioning from NFs to community-based settings and who wish to support other candidates in transition (described above);
- Ongoing technical assistance provided by the state to the MCOs to help identify the strategies and practices that are proving to be successful in identifying and facilitating MFP transitions; and
- Ongoing development of community-based services and supports and alternative residential settings.
LOOKING AHEAD
Given the state’s NF LOC eligibility criteria and an emphasis on NF diversion by providing HCBS to beneficiaries identified as at risk of NF placement, Tennessee expects a decline in the number of beneficiaries who transition from NFs to the community via MFP in 2014. As a result of these initiatives, Medicaid beneficiaries being served in NFs have higher acuity of care needs and the challenges associated with supporting the higher acuity individuals in the community are greater. To improve transitions, Tennessee is currently looking at a variety of options, including expanding community housing options that cost-effectively serve NF residents who desire to transition to the community.
Tennessee has integrated its MFP program into its existing Medicaid LTSS system, including CHOICES, the capitated MLTSS program for seniors and adults with physical disabilities. Together, these two Medicaid LTSS rebalancing efforts, MFP and CHOICES, are succeeding in placing more beneficiaries in home and community-based settings. In just under three years, the percentage of seniors and adults with physical disabilities receiving HCBS in Tennessee grew from 17 percent in 2010 to 40 percent as of August 31, 2013. This shift in care setting reflects Tennessee’s progress in meeting its community integration obligations under the U.S. Supreme Court’s 1999 Olmstead decision and beneficiaries’ preference for needing and receiving community-based care. Specifically, MFP has assisted in the paradigm shift within MCOs and the way they approach transitions. As a result of MFP, MCOs have changed staffing models, hired housing specialists, and developed care coordinator performance goals related to transitioning individuals from an institutional setting into MFP.
The lack of affordable, accessible housing options remains a challenge for MFP participants and for NF residents who desire to transition to the community and so Tennessee’s MFP program has focused on developing community housing options through its partnership with the state housing finance agency. Further, state officials maintain that the allowance of federal Medicaid matching funds for institutional room and board but not community housing assistance perpetuates the institutional bias in the Medicaid LTSS system and impedes MFP states’ efforts to transition individuals to the community.
The performance of Tennessee’s overall MFP program as well as that of CHOICES MCOs will continue to be monitored over time, with program adjustments as needed to ensure that the state continues to achieve its rebalancing goals. Looking ahead, the CHOICES program and MFP will continue to work together to support the transitions of seniors and adults with physical disabilities from institutions to the most integrated community setting in which they can be served.
This Kaiser Commission on Medicaid and the Uninsured brief was prepared by Molly O’Malley Watts with Watts Health Policy Consulting and Erica L. Reaves and MaryBeth Musumeci from the Kaiser Family Foundation. Special thanks to Catherine Lemaire Lozier, Rachel Turner, Michelle Morse Jernigan, and Patti Killingsworth of the Tennessee Division of LTSS, Bureau of TennCare who contributed to the content and review of this case study.