Racial Disparities in COVID-19: Key Findings from Available Data and Analysis
Summary
Over the course of the COVID-19 pandemic, there has been a growing focus on its disproportionate impacts on people of color, particularly as availability of data to understand racial disparities has increased. This brief summarizes key findings from data and analyses examining COVID-19 related cases, deaths, hospitalizations, and testing by race and ethnicity as of early August 2020 to provide increased insight into these disparities. Key findings include the following:
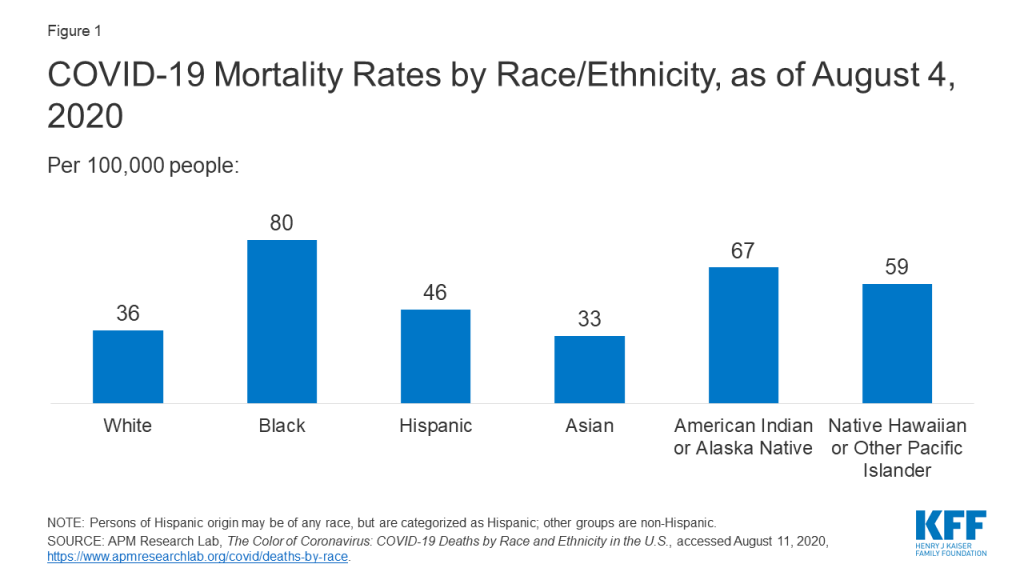
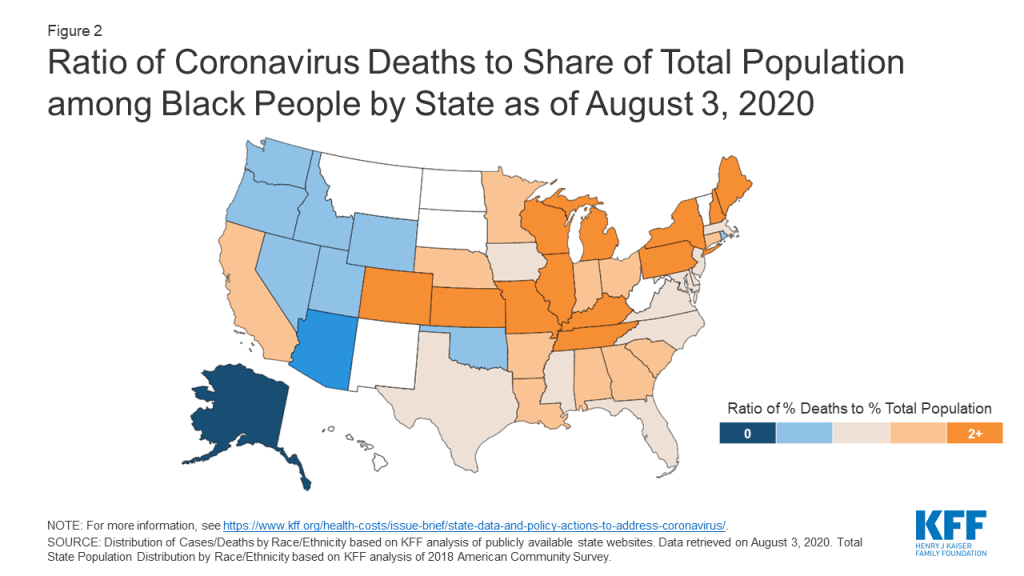
Multiple analyses of available federal, state, and local data show that people of color are experiencing a disproportionate burden of COVID-19 cases and deaths. They show particularly large disparities in cases and deaths for Black and American Indian and Alaska Native (AIAN) people and widespread disparities in cases among Hispanic people compared to their White counterparts. For example, KFF analysis of state reported data showed that, as of August 3, 2020, Black individuals accounted for more cases and deaths relative to their share of the population in 30 of 49 states reporting cases and 34 of 44 states reporting deaths. Other analysis of state-reported data finds that, as of August 4, the COVID-19 related death rate among Black people was over twice as high as the rate for White people, while the mortality rate for AIAN people was nearly two times that of White people. Data also reveal disparities for Asian and Native Hawaiian and Pacific Islander (NHOPI) individuals in certain areas and show a sharp, recent rise in mortality rates for NHOPI and Hispanic people. Analyses further find that disparities in COVID-19 related deaths persist across age groups and that people of color experience more deaths among younger people relative to White individuals. There is limited data and research to understand of impacts for subgroups, such as immigrants, who may be at increased risk.
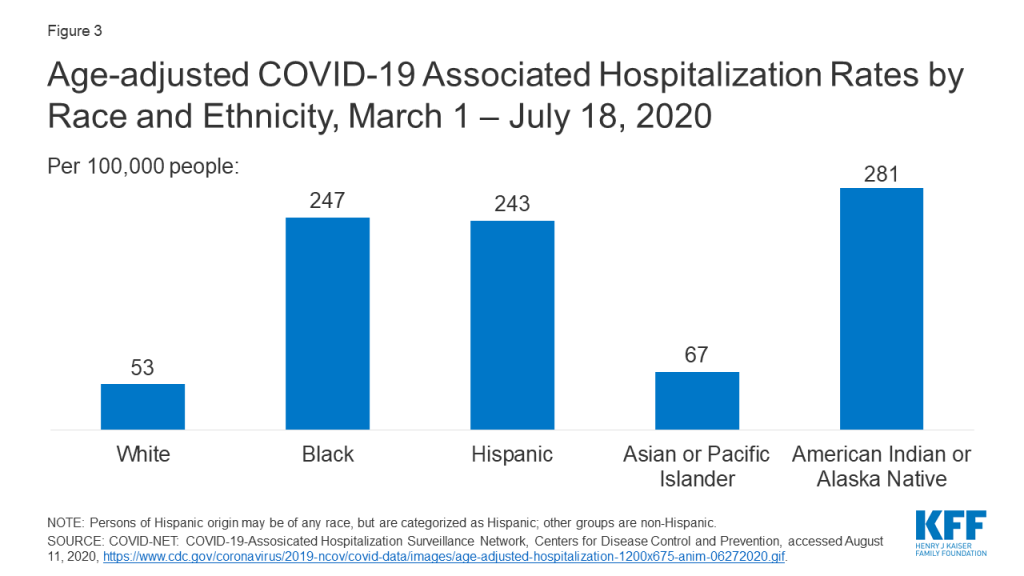
Data show that Black, Hispanic, and AIAN people are at increased risk of hospitalization due to COVID-19. For example, data from Coronavirus Disease 2019-Associated Hospitalization Surveillance Network (COVID-NET) show that, from March through July 18, 2020, age-adjusted hospitalization rates due to COVID-19 for Black, Hispanic, and AIAN people were roughly five times higher than that of White people. Several studies using health system data also point to a higher risk of hospitalization for Black and Hispanic patients. Reflecting these higher hospitalization rates, analyses show that people of color make up a disproportionate share of COVID-19 hospitalizations relative to their share of the population or total hospital visits.
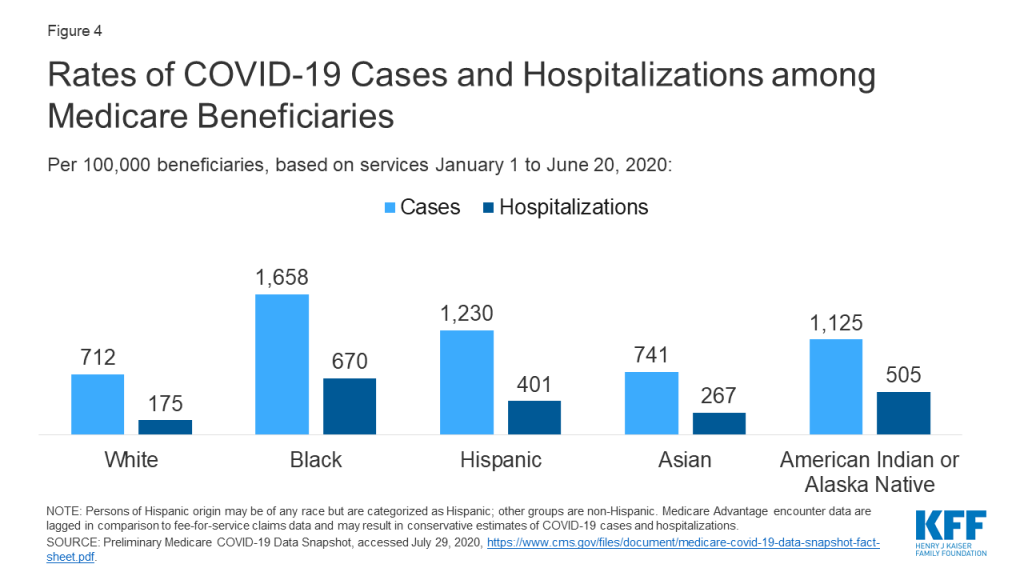
Studies find racial/ethnic disparities in COVID-19 among Medicare beneficiaries, nursing home facilities, pregnant women, and children. Preliminary Medicare COVID-19 data show that Black, Hispanic, and AIAN Medicare beneficiaries had higher rates of infection and hospitalization compared to White beneficiaries. Analysis finds that nursing homes where a higher share of residents are people of color are more likely to report a COVID-19 case. Studies also find disproportionate shares of infection among Hispanic and Black pregnant women and a higher risk of hospitalization among Black and Hispanic children.
Data to understand variation in testing by race/ethnicity remains very limited but suggest people of color may face increased barriers to testing. Very few states report testing data by race/ethnicity. Data on testing within community health centers analyzed by KFF show that people of color represented more than half of all people tested (57%) and confirmed cases (56%) at health centers, and that Hispanic patients made up a higher share of positive tests compared to their share of total tested patients. Analyses suggest that testing sites in and near predominantly Black and Hispanic neighborhoods are likely to face greater demand than those near predominantly White areas, which could contribute to longer wait times, and the share of people of color in an area is associated with an increase in travel time to a testing site. One study also found that, in New York City, more tests were performed in neighborhoods with a higher share of White residents, while the highest shares of positive tests were in neighborhoods with more people of color and lower socioeconomic measures. Reporting on testing site locations in Texas suggests that testing sites are disproportionately located in areas with larger shares of White residents.
Together, these data show that people of color are bearing a disproportionate burden of COVID-19 cases, deaths, and hospitalizations and that they may face increased barriers to access testing. Other analyses also suggest that the COVID-19 pandemic is taking a larger economic toll on people of color. These disparities in COVID-19 reflect and compound longstanding underlying social, economic, and health inequities that stem from structural and systemic barriers across sectors, including racism and discrimination. For example, prior to the pandemic, people of color had higher rates of health conditions, were more likely to be uninsured and face barriers to accessing health care, and were more likely to have lower incomes and face financial challenges. These underlying disparities put people of color at increased risk for exposure to the virus, experiencing serious illness if they are infected, and facing barriers to accessing testing and treatment.
The health and economic impacts of COVID-19 could further widen racial disparities at a time when there is a growing focus on and call for racial justice and health equity. Overall, the findings highlight the importance of considering how COVID-19 relief and response efforts will address inequities, including in decisions related to distribution of treatments and vaccines once they become available. Prioritizing equity will be key for addressing the current gaps in COVID-19 and health care more broadly and preventing widening of disparities in the future.
Issue Brief
Data on COVID-19 by Race/Ethnicity
At the outset of the COVID-19 pandemic, limited data were available on cases, hospitalization, deaths, and testing disaggregated by race/ethnicity, constraining the ability to understand its effects across communities and to target response and relief efforts. Availability of this data has increased over time and, along with it, there has been a growing body of analyses examining race-associated differences in the impacts of the virus. As of August 2020, nearly all states were reporting COVID-19 related cases and/or deaths by race and/or ethnicity. Following early state reporting of these data, the Centers for Disease Control and Prevention (CDC) began reporting hospitalizations, cases, and deaths by race/ethnicity, and the Centers for Medicare and Medicaid Services (CMS) and Health Resources and Services Administration (HRSA) began reporting limited data. (See Appendix A for a list of federal sources of COVID-19 data by race/ethnicity). Beyond these state and federal data sources, health systems and health insurers may also collect data, but these data typically are not publicly accessible.
While data have improved over time, they continue to have significant gaps and limitations. For example, some states only report either cases or deaths, states use different race/ethnicity categories, states vary in which racial/ethnic groups for which they report data, and some states have high shares of cases with unknown race/ethnicity. The federally reported data provide more standardized race/ethnicity categorizations but still have limitations, including high shares of cases with unknown race/ethnicity as well as lack of state-level data for some measures and inconsistencies that limit comparability of data across states. The federal data on hospitalizations represent a subset of 250 acute care hospitals in 14 states that are part of the Coronavirus Disease 2019-Associated Hospitalization Surveillance Network (COVID-NET). As of early August, data on testing by race/ethnicity remain very limited, with only six states reporting testing by race/ethnicity. In addition, because people of color may be at greater risk for exposure due to their jobs or living circumstances, data on testing rates alone cannot necessarily identify disparities. Data are available for tests conducted at community health centers, which primarily serve low-income patients and communities of color, though the data are not representative of a state’s population and are based on rapid response surveys.
Key Findings on COVID-19 by Race/Ethnicity
Below is a summary of key findings from data and analyses that examine reported COVID-19 cases, deaths, hospitalizations, and testing by race and ethnicity available as of early August 2020.1 (See Appendix B for a list of analysis referenced in this brief.) To collect relevant analyses, we conducted keyword searches of websites for government, research, and policy organizations that publish health-related research; media; and PubMed. While we tried to be comprehensive in our inclusion of studies and findings on this topic, it is possible that we omitted some relevant studies or findings. Moreover, because work in this area is continually developing and growing, research that is more recent may be available that this summary does not reflect.
Cases and Deaths
Multiple analyses of available federal, state, and local data show that people of color are experiencing a disproportionate burden of COVID-19 cases and deaths. They show particularly large disparities in cases and deaths for Black and AIAN people and widespread disparities in cases among Hispanic people compared to their White counterparts. Data also reveal disparities for Asian and NHOPI individuals in certain areas and show a sharp recent rise in mortality rates for NHOPI and Hispanic people. There is limited data and research to understand of impacts for subgroups, such as immigrants, who may be at increased risk.
- People of color are experiencing significantly higher rates of infections and deaths compared to White individuals. For example, analysis of state-reported data finds that, as of August 4, COVID-19 related death rates among Black people were over twice as high as the rate for White people, while the mortality rate for AIAN people was nearly two times that of White people (Figure 1). These data also show a sharp recent rise in mortality rates for NHOPI and Hispanic people. Reporting based on county-level data found that Black and Hispanic people are nearly three times as likely to contract COVID-19 and nearly two times as likely to die from COVID-19. It also found several areas where AIAN individuals were significantly more likely to be infected compared to White people as well as some higher risk of infection among Asian people. Other data show that, in states with large numbers of NHOPI people, they have higher infection rates compared to other racial and ethnic groups, and that Asian people are experiencing a higher case fatality rate than average in a number of areas across the country. Further, a study using data from a health system in the Baltimore-Washington DC region found that Hispanics had a higher infection rate compared to other groups.
- Disparities for Black and Hispanic people are widespread across the country. For example, KFF analysis of state reported data showed that, as of August 3, 2020, Black individuals accounted for more cases and deaths relative to their share of the population in 30 of 49 states reporting cases and 34 of 44 states reporting deaths (Figure 2). Hispanic people made up a higher share of cases and deaths compared to their share of the total population in 35 of 45 states reporting cases and 10 of 44 states reporting deaths. County-level data also suggest that disparities in infection rates for Black and Hispanic people are widespread across counties. The state and county-level data also point to stark disparities for AIAN and Asian people but in a more limited number of areas.
- County-level analysis finds that cases and deaths are concentrated in areas with higher shares of Black and Hispanic residents. One study of nationwide county-level data found that higher shares of Black people living in a county are associated with increased shares of COVID-19 cases and deaths in the county, as well as a positive correlation between the share of Asian residents and the county infection and mortality rate. Other analysis finds that, as of April, 97% of disproportionately Black counties (with a greater share of Black residents compared to the U.S. average) reported a case and 49% reported a death versus 81% and 28%, respectively, for other counties. These disparities persisted after adjusting for county-level characteristics such as percent of the population older than 65, unemployment, health insurance coverage status, comorbidities, days since first case of diagnosis, and urbanicity. Overall, the roughly 20% of U.S. counties that are disproportionately Black accounted for 52% of COVID-19 diagnoses and 58% of deaths nationally during the first several months of the U.S. epidemic. In addition, another analysis finds that, as of August 3, 8 of the 20 counties with the highest level of deaths per capita are predominantly Black, and three of the five counties with the highest per capita death rates are predominantly Black. Similarly, a study of ten major metropolitan areas found that counties with larger shares of Latino residents have disproportionate shares of cases. Additional work finds that, among both counties with higher median county-level income and lower median county-level income, higher shares of people of color were associated with higher rates of infection and death compared to counties that have higher shares of White residents (>81%).
Disparities in COVID-19 deaths for people of color persist across age groups, and people of color experience more deaths among younger people relative to White individuals. Researchers examining federally reported data find increased risk of death due to COVID-19 among Black, Hispanic, AIAN, and Asian and Pacific Islander people as compared to their White counterparts across age groups, with particularly large disparities among younger adults age 25-54. The study also found that Black and Hispanic populations lost more years of total potential life due to COVID-19 compared to the White population, even though the White population is three to four times larger. Other analysis finds that disparities in deaths widen for all groups of color after adjusting for age. CDC analysis of data for roughly 11,000 COVID-19 deaths in 16 public health jurisdictions found that over one in three (35%) deaths among Hispanic people and 30% of deaths among people of color were among those under age 65, compared to 13% of deaths among White people. Additionally, the median age of individuals dying from COVID-19 was 9 to 10 years younger among people of color.
Hospitalizations
Black and Hispanic people have higher hospitalization rates compared to their White counterparts. Data from COVID-NET show that, from March 1 through July 18, age-adjusted hospitalization rates due to COVID-19 for Black, Hispanic, and AIAN people were each roughly 5 times higher than that of White people (Figure 3). Another analysis of patients at a large hospital system in Boston who tested positive for COVID-19 found that a higher proportion of Hispanic patients were hospitalized compared to Black or White patients, particularly among those under age 60. In contrast, a study of patients tested at a health system in the Baltimore-Washington DC found a higher positivity rate among Latino patients but a lower hospital admission rate among Latino patients who tested positive. Latino patients who were hospitalized were younger, more likely to be male, and had fewer comorbidities compared to White or Black patients. Studies using data from an academic health system in Atlanta, Georgia, a large health system in California, and a health system in Chicago all find that Black patients are at higher risk for hospitalization. Reflecting these higher rates, several studies also found that people of color make up a disproportionate share of COVID-19 hospitalizations relative to their share of the population or total hospital visits. For example, earlier data from COVID-NET based on 580 hospitalizations as of March 2020 show that Black people accounted for more hospitalized COVID-19 patients compared to their share of the population in the area studied (33% vs. 18%). A study using data from a large health system in Louisiana found that Black people accounted for over three-quarters of patients who were hospitalized with COVID-19 (77%) and over 71% of in-hospital deaths, compared to just 31% of the total patient population.
Disparities among Specific Populations
Studies also find racial/ethnic disparities in COVID-19 cases and/or deaths among Medicare beneficiaries, nursing facilities, pregnant women, and children.
- Preliminary Medicare claims and encounter data based on services from January 1 through June 20, 2020 show higher rates of infection and hospitalization due to COVID-19 among Black, Hispanic, and AIAN Medicare beneficiaries compared to White beneficiaries (Figure 4).
- Analysis of nursing home facilities found that having a greater share of Black residents was associated with increased probability of having a COVID-19 case. Other reporting also has found that nursing homes where a higher share of residents are people of color are more likely to report a COVID-19 case.
- One study found that Hispanic and Black pregnant women accounted for a disproportionate share of confirmed cases relative to their share of women who gave birth in 2019 (46% vs. 24% and 22% vs 15%, respectively).
- CDC analysis of COVID-19 hospitalization data from 14 states found that, although the overall COVID-19 associated hospitalization rate for children is low, hospitalization rates for Hispanic and Black children were nearly eight times and five times higher than the rate for White children, respectively. Early data from a COVID-19 clinic in Chicago also suggest that Black children are at higher risk of infection. Similarly, a study of children tested at a pediatric community-based free testing site found that Black and Hispanic children had higher rates of infection, that these differences persisted after controlling for age, sex, and median family income, and that positivity rates among Hispanic children increased over time.
Testing
Data to understand variation in testing by race/ethnicity remains very limited. Very few states (5 as of July 2020) report testing data by race/ethnicity. Data on testing within community health centers show that people of color represented more than half of all people tested (57%) and confirmed cases (56%) at health centers, and that Hispanic patients made up a higher share of positive tests compared to their share of total tested patients. Reporting on testing site locations suggests that testing sites in and near predominantly Black and Hispanic neighborhoods are likely to face greater demand than those near predominantly White areas, which could contribute to longer wait times. Other research finds that the share of people of color in an area is associated with an increase in travel time to a testing site. Similarly, analysis of data from New York City found that more tests were performed in neighborhoods with higher shares of White residents, but that the highest proportion of positive tests were in neighborhoods with more people of color and lower socioeconomic measures. Reporting on testing site locations in Texas found that in four of the six largest cities testing sites are disproportionately located in census tracts where the share of White residents is greater than the city median.
Looking ahead
Together, these data show that people of color are bearing a disproportionate burden of COVID-19 cases, deaths, and hospitalizations and that they may face increased barriers to access testing. Other analyses also suggest that the COVID-19 pandemic is taking a larger economic toll on people of color. These disparities in COVID-19 reflect and compound longstanding underlying social, economic, and health inequities that stem from structural and systemic barriers across sectors, including racism and discrimination. Researchers across the studies suggest that these underlying disparities put people of color at increased risk for exposure to the virus, experiencing serious illness if they are infected, and facing barriers to accessing testing and treatment. For example, their living and employment situations make it more difficult to social distance, as they are more likely to work in jobs that cannot be done at home, more likely to use public transportation, and more likely to live in larger households. Variation in access to testing, delays in seeking care due to lack of insurance and other access barriers, as well as higher rates of underlying health conditions may contribute to more serious illness among individuals if they are infected and individuals being in more serious condition when they do seek care, which could contribute to higher rates of hospitalization and death.
While these data and analysis provide important insights into the disparate impacts of COVID-19, there remain significant data gaps and limitations that point to the importance of continued efforts to increase the availability of COVID-19 data by race and ethnicity. Data on testing may grow as, under the CARES Act and guidance from HHS, all laboratories or other facilities performing COVID-19 testing must report data to HHS and “make every reasonable effort” to collect and report demographic data, including race/ethnicity, starting August 1. However, continued efforts will be required to provide for timely, complete, and comparable data that allow for better understanding of COVID-19 impacts overall and particularly for smaller population groups, such as AIAN and NHOPI individuals as well as among ethnic groups. These data are key for understanding impacts across communities, guiding response and relief efforts, and providing for equitable access to treatments and vaccines as they are developed.
The health and economic impacts of COVID-19 could further widen racial/ethnic disparities at a time when there is a growing focus on and call for racial justice and health equity. Overall, the findings highlight the importance of considering how COVID-19 relief and response efforts will address inequities, including in decisions related to distribution of treatments and vaccines once they become available. Prioritizing equity will be key for addressing the current gaps in COVID-19 and health care more broadly and preventing widening of disparities in the future.
Appendix
Appendix A
| Table 1: Federal Data Sources on COVID-19 and Race/Ethnicity | |||
| Source | Title | Description | Level |
| Public Data from the Federal Government | |||
| CDC | CDC COVID Data Tracker | Provides information on cases and deaths by race/ethnicity. Race/ethnicity data can also be stratified by age group (updated daily). | National |
| CDC | Provisional Death Counts for Coronavirus Disease (COVID-19) | Contains multiple data sets from the National Vital Statistics System’s COVID-19 Surveillance Data Files, including provisional death counts by race/ethnicity and deaths involving coronavirus by race/ethnicity and age (race data updated weekly). | State and National |
| CDC | COVID-NET: COVID-19 Laboratory-Confirmed Hospitalizations | Summary of COVID-19 hospitalizations. In addition to race/ethnicity, figures are stratified by multiple demographic characteristics (updated biweekly). | National |
| CMS | Preliminary Medicare COVID-19 Data Snapshot | Counts of Medicare beneficiaries of COVID-19 cases and hospitalizations by several measures, including race/ethnicity at the national level (updated monthly). | State and National |
| HRSA | Health Center COVID-19 Survey | Rapid response survey of community health centers on a range of issues related to COVID-19, included testing data by race/ethnicity (updated weekly). | State and National |
Appendix B: References
KFF (Kaiser Family Foundation), State Data and Policy Actions to Address Coronavirus, COVID-19 Confirmed Cases and Deaths by Race/Ethnicity as of August 3, 2020, accessed August 11, 2020, https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/.
The COVID Tracking Project, The COVID Racial Data Tracker, accessed August 11, 2020, https://covidtracking.com/race.
APM Research Lab, The Color of Coronavirus: COVID-19 Deaths by Race and Ethnicity in the U.S., (August 5, 2020), accessed August 11, 2020, https://www.apmresearchlab.org/covid/deaths-by-race.
The COVID Tracking Project, The COVID Racial Data Tracker, accessed August 11, 2020, https://covidtracking.com/race.
KFF (Kaiser Family Foundation), State Data and Policy Actions to Address Coronavirus, COVID-19 Confirmed Cases and Deaths by Race/Ethnicity as of August 3, 2020, accessed August 11, 2020, available at https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/.
L. Kim, M. Whitaker. A. O’Halloran, et al., “Hospitalization Rates and Characteristics of Children Aged <18 Years Hospitalized with Laboratory-Confirmed COVID-19 — COVID-NET, 14 States, March 1–July 25, 2020,” Morbidity and Mortality Weekly Report ePub 7 (August 2020), available at https://www.cdc.gov/mmwr/volumes/69/wr/mm6932e3.htm?s#F2_down.
Monika K. Goyal, et al, “Racial/Ethnic and Socioeconomic Disparities of SARS-CoV-2 Infection Among Children, Pediatrics, Vol 16, Issue 2 (August 2020), accessed August 11, 2020, available at https://pediatrics.aappublications.org/content/early/2020/08/03/peds.2020-009951.
Centers for Disease Control and Prevention, Age-adjusted COVID-19-associated hospitalization rates by race and ethnicity, accessed August 11, 2020, https://www.cdc.gov/coronavirus/2019-ncov/covid-data/images/July-28_Race_Ethnicity_COVIDNet.jpg.
Centers for Medicare & Medicaid Services, Preliminary Medicare COVID-19 Data Snapshot, accessed August 11, 2020, https://www.cms.gov/research-statistics-data-systems/preliminary-medicare-covid-19-data-snapshot.
Samrachana Adhikari, Nicholas P. Pantaleo, and Justin M. Feldman, “Assessment of Community-Level Disparities in Coronavirus Disease 2019 (COVID-19) Infections and Deaths in Large Metropolitan Areas, Jama Network Open (July 28, 2020), accessed August 11, 2020, available at https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2768723.
Carlos E. Rodriguez-Diaz et al., “Risk for COVID-19 infection and death among Latinos in the United States: Examining heterogeneity in transmission dynamics”, Annals of Epidemiology (July 23, 2020), accessed August 11, 2020, available at https://www.sciencedirect.com/science/article/pii/S1047279720302672#figs1.
Soo Rin Kim et al., “Which Cities Have The Biggest Racial Gaps In COVID-19 Testing Access?” FiveThirtyEight, July 22, 2020, https://fivethirtyeight.com/features/white-neighborhoods-have-more-access-to-covid-19-testing-sites/.
J.M. Wortham, J.T. Lee, S. Althomsons et al., “Characteristics of Persons Who Died with COVID-19 — United States, February 12–May 18, 2020”, Morbidity and Mortality Weekly Report 69, no. 28 (July 17, 2020), accessed August 11, 2020, available at https://www.cdc.gov/mmwr/volumes/69/wr/mm6928e1.htm.
Brandon W. Yan et al., “Asian Americans Facing High COVID-19 Case Fatality”, Health Affairs (July 13, 2020), https://www.healthaffairs.org/do/10.1377/hblog20200708.894552/full/.
Heather E. Hsu et al., “Race/Ethnicity, Underlying Medical Conditions, Homelessness, and Hospitalization Status of Adult Patients with COVID-19 at an Urban Safety-Net Medical Center – Boston, Massachusetts, 2020”, Morbidity and Mortality Weekly Report 69 no. 27 (July 10, 2020), available at https://pubmed.ncbi.nlm.nih.gov/32644981/.
Ayodeji Adegunsoye, I. Bauer Ventura , and V.M. Liarski, “Association of Black Race with Outcomes in COVID-19 Disease: A Retrospective Cohort Study”, Annals of the American Thoracic Society (July 9, 2020), available at https://www.atsjournals.org/doi/abs/10.1513/AnnalsATS.202006-583RL.
Richard A. Oppel Jr. et al., “The Fullest Look Yet at the Racial Inequity of Coronavirus”, The New York Times, July 5, 2020, accessed August 11, 2020, https://www.nytimes.com/interactive/2020/07/05/us/coronavirus-latinos-african-americans-cdc-data.html.
David R. Holgrave et al., “Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York State”, Annals of Epidemiology 48 (June 29, 2020), available at https://doi.org/10.1016/j.annepidem.2020.06.010.
Marie E. Killerby et al. “Characteristics Associated with Hospitalization Among Patients with COVID-19 — Metropolitan Atlanta, Georgia, March–April 2020”, Morbidity and Mortality Weekly Report 69, no. 25 (June 26, 2020), available at https://www.cdc.gov/mmwr/volumes/69/wr/mm6925e1.htm.
Sascha Ellington et al., “Characteristics of Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status — United States, January 22–June 7, 2020”, Morbidity and Mortality Weekly Report 69 no. 25 (June 26, 2020): 769–775, available at https://www.cdc.gov/mmwr/volumes/69/wr/mm6925a1.htm.
Eboni G. Pricey-Haywood et al., “Hospitalization and Mortality among Black Patients and White Patients with Covid-19”, New England Journal of Medicine 382, no. 26 (June 25, 2020), available at https://www.nejm.org/doi/full/10.1056/NEJMsa2011686.
Wil Libermann-Cribbin et al., “Disparities in COVID-19 Testing and Positivity in New York City”, American Journal of Preventive Medicine (June 25, 2020), available at 10.1016/j.amepre.2020.06.005.
Diego A. Martinez et al., “SARS-CoV-2 Positivity Rate for Latinos in the Baltimore–Washington, DC Region”, Journal of the American Medical Association 324 no. 4 (June 13, 2020), available at 10.1001/jama.2020.11374.
Bassett MT, Chen JT and Krieger N, “The Unequal toll of COVID-19 Mortality by Age in the United States: Quantifying Racial/Ethnic Disparities”, Working Paper Series 19, no.3 (June 12, 2020), Harvard Center for Population and Development Studies, available at https://cdn1.sph.harvard.edu/wp-content/uploads/sites/1266/2020/06/20_Bassett-Chen-Krieger_COVID-19_plus_age_working-paper_0612_Vol-19_No-3_with-cover.pdf.
Hannah R. Abrams et al., “Characteristics of U.S. Nursing Homes with COVID ‐19 Cases”, Journal of the American Geriatrics Society, (June 2, 2020), available at https://doi.org/10.1111/jgs.16661.
Sindhura Bandi, M.Z. Nevid, M. Mahdavinia, “African American children are at higher risk of COVID‐19 infection”, Pediatric Allergy and Immunology (May 29, 2020), available at https://doi.org/10.1111/pai.13298.
Sean McMinn et al. “In Large Texas Cities, Access To Coronavirus Testing May Depend On Where You Live”, NPR, May 27, 2020, accessed August 11, 2020, https://www.npr.org/sections/health-shots/2020/05/27/862215848/across-texas-black-and-hispanic-neighborhoods-have-fewer-coronavirus-testing-sit.
Kristen M.J. Azar et al., “Disparities In Outcomes Among COVID-19 Patients In A Large Health Care System In California”, Health Affairs 39, no. 7 (May 21, 2020), accessed August 11, 2020, available at https://www.healthaffairs.org/doi/10.1377/hlthaff.2020.00598.
Robert Gebeloff et al., “The Striking Racial Divide in How Covid-19 Has Hit Nursing Homes”, The New York Times, May 21, 2020, accessed July 8, 2020, https://www.nytimes.com/article/coronavirus-nursing-homes-racial-disparity.html.
Uma V Mahajan and Margaret Larkins-Pettigrew, “Racial demographics and COVID-19 confirmed cases and deaths: a correlational analysis of 2886 US counties”, Journal of Public Health (May 21, 2020), available at 10.1093/pubmed/fdaa070.
Bradley Corallo and Jennifer Tolbert, Impact of Coronavirus on Community Health Centers, (Washington, DC, KFF, May 20, 2020), accessed August 11, 2020, available at https://www.kff.org/coronavirus-covid-19/issue-brief/impact-of-coronavirus-on-community-health-centers/
Benjamin Rader et al., “Geographic access to United States SARS-CoV-2 testing sites highlights healthcare disparities and may bias transmission estimates”, Journal of Travel Medicine (May 15, 2020), available at https://doi.org/10.1093/jtm/taaa076.
Gregorio A. Millett et al., “Assessing Differential Impacts of COVID-19 on Black Communities”, Annals of Epidemiology 47 (May 14, 2020), available at https://doi.org/10.1016/j.annepidem.2020.05.003.
Joseph Keawe‘aimoku Kaholokula et al., “COVID-19 Special Column: COVID-19 Hits Native Hawaiian and Pacific Islander Communities the Hardest”, Hawai’i Journal of Health & Social Welfare, 29 no. 5 (May 1, 2020), available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7226312/#.
Shikha Garg et al. “Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 — COVID-NET, 14 States, March 1–30, 2020”, Morbidity and Mortality Weekly Report 69, no. 15 (April 17, 2020), available at https://www.cdc.gov/mmwr/volumes/69/wr/mm6915e3.htm.
Endnotes
- Studies that estimated cases or deaths were excluded. ↩︎