Factors Affecting States’ Ability to Respond to Federal Medicaid Cuts and Caps: Which States Are Most At Risk?
In 2017, Congress has been debating legislation, the American Health Care Act (AHCA), which would end the enhanced federal matching funds for the Affordable Care Act (ACA) Medicaid expansion and fundamentally alter the structure and financing of the Medicaid program. Specifically, it would cap and significantly reduce the amount of federal funding provided to states for Medicaid through a per capita cap or block grant. The Congressional Budget Office estimated that the AHCA as passed by the House would reduce federal Medicaid spending by $834 billion from 2017-2026 and reduce enrollment by 14 million by 2026 compared to projections in current law. The proposed Trump Administration budget for FY 2018 would have deeper Medicaid reductions.
The cap on federal funding would lock-in current state spending patterns that reflect historic Medicaid policy choices. Today, Medicaid is a state and federal partnership where the federal government sets core requirements for Medicaid and states administer the program; financing for Medicaid is shared by states and the federal government with no caps. Due to flexibility in the current law, states historically have made different Medicaid decisions related to coverage, scope of benefits, reimbursement rates and delivery system models. In response to a funding cap, each state would need to make budget decisions to fill in gaps in federal funding (through taxes or other budget cuts) or to restrict Medicaid programs.
All states could face challenges responding to federal Medicaid cuts and caps to varying degrees, but states with certain characteristics are more at risk. This analysis examines 30 factors in five groups that could be high risk factors affecting states’ ability to respond to federal Medicaid cuts and caps and identifies states ranked in the top five for each factor as high risk (ES-1). This analysis shows that more than 6 in 10 states rank in the top five for multiple risk factors. Eleven states rank in the top five for five or more risk factors (Alabama, Arizona, Florida, Georgia, Kentucky, Louisiana, Mississippi, New Mexico, South Carolina, Texas, and West Virginia).
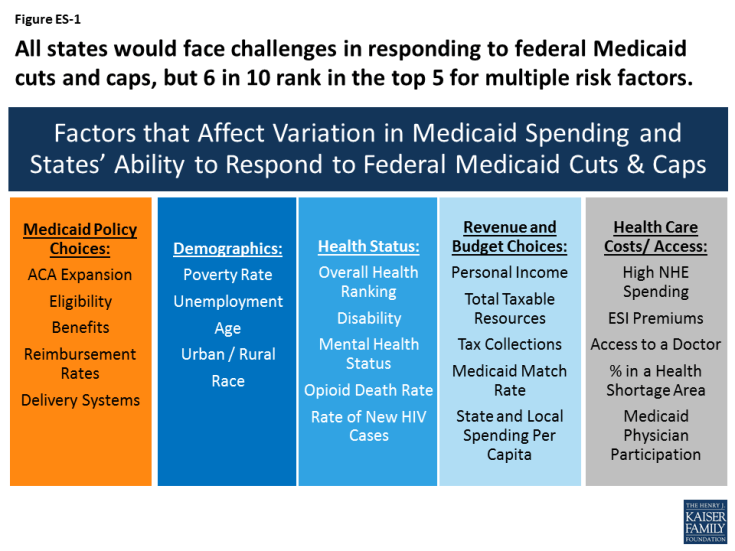
Figure ES-1: All states would face challenges in responding to federal Medicaid cuts and caps, but 6 in 10 rank in the top 5 for multiple risk factors.
States that adopted the Medicaid expansion have experienced gains in coverage and financing that are at risk under proposals like the AHCA that would end the enhanced federal match for the expansion. However, states that have not adopted the expansion would lose the option to access enhanced federal matching dollars for coverage in the future.
- Arkansas, Kentucky, Nevada and Oregon are among states that rank in the top five for multiple risk factors tied to the end of enhanced funding for expansion (i.e. large coverage gains, a high share of expansion enrollees, and a high share of expansion funding relative to the total). In total numbers, California, New York, Pennsylvania, Ohio and Illinois account for the largest number of enrollees in the expansion group (54%) and California, New York, Ohio, Michigan and Illinois account for the highest levels of federal expansion funding (52%).
- Non-expansion states would lose the future option to provide coverage to poor uninsured adults with enhanced federal dollars. Florida, Georgia and Texas have the largest number of uninsured residents who fall into the coverage gap (i.e. not eligible for Medicaid but have incomes below poverty so are not eligible for tax credits in the Marketplace) and the highest overall uninsured rates.
States with limited Medicaid programs and other challenging characteristics such as poor demographic indicators, poor health status, high cost health care markets and low state fiscal capacity could face more challenges in responding to per capita cap or block grant policies. States with limited Medicaid benefits or low provider reimbursement rates have less room to make further restrictions in benefits or to lower rates in response to reductions in federal financing. For these states, trade-offs within Medicaid would be difficult. States with an aging population, high levels of disability, a high share of people in health professional shortage areas or low per capita income may have higher demand for Medicaid services, but less capacity (especially with limited federal financing) to address those issues. In addition, because financing caps lock states into historic Medicaid decisions, states with limited programs and other risk factors will have a harder time adapting to future changes such as increased costs or changing demographics. One example of an emerging health issue is the opioid epidemic. Medicaid plays a central role in the nation’s effort to address the opioid epidemic through coverage of people struggling with opioid addiction and financing for states, limited funding could impede efforts to address this as well as other future health issues.
The findings below show states that rank in the top five for multiple risk factors within each of the five categories (beyond expansion):
- Medicaid Policy Choices: Alabama, Hawaii, Mississippi and Missouri have more than one restrictive Medicaid policies that would make it more challenging for them to implement additional program reductions (i.e. low eligibility levels, limited benefits, low provider reimbursement, high managed care penetration and/or a lower share of community based long-term care services).
- Demographics: Alaska, District of Columbia, Louisiana, New Mexico and Wyoming each have multiple demographic characteristics that indicate higher needs for Medicaid (i.e. high poverty, high unemployment, faster expected growth in the 85 year old population, high share of the population in rural areas, and / or high share of the population that is non-white).
- Health Status: Alabama, Arkansas, Louisiana, Mississippi and West Virginia have populations with multiple high health needs (i.e. overall poor health status, high share reporting a disability, high share reporting poor mental health, high opioid death rate and/or high rate of new HIV cases). Ohio, New Hampshire and West Virginia reported the highest opioid related drug overdoses at over 24 people in every 100,000.
- Revenue and Budget Choices: Alabama, Arizona, Idaho, Mississippi, New Mexico, South Carolina, Tennessee and West Virginia have multiple tax capacity challenges (i.e. low personal income, low total taxable resources, low tax effort or share of taxes relative to personal income, high Medicaid match rates, and/or low state and local spending per capita).
- Health Care Costs/Access: Alaska, Alabama, Florida, Louisiana, Massachusetts, Mississippi and New York have high cost health care markets and access challenges (i.e. high national health expenditures per capita, high employer sponsored insurance premiums, high share or people not seeking care due to cost, high share of the population in a shortage area and/or lower Medicaid physician participation).
While all states have risk factors to varying degrees, this analysis shows that more than 6 in 10 states rank in the top five for multiple risk factors. Eleven states rank in the top five for five or more risk factors (Alabama, Arizona, Florida, Georgia, Kentucky, Louisiana, Mississippi, New Mexico, South Carolina, Texas, and West Virginia). States that have multiple risk factors could face even more challenges making Medicaid program cuts or filling gaps in federal funding. Looking ahead, limiting the growth in federal Medicaid spending could force states to make difficult choices in their current programs and could also limit states ability to afford new drug therapies or other medical advances, adapt to changing demographics or make future investments to improve delivery systems or address broader health status issues in the future.
Tables with state-level data for each of the 30 risk factors considered in the analysis are included at the end of the report. Sources for data included in the tables and described in the report can be found in the appendix.
