Biden Wants to Partner with Health Centers to Promote More Equitable Access to COVID-19 Vaccines
Bradley Corallo and Jennifer Tolbert
Published:
As part of the Biden administration’s plans to speed up COVID-19 vaccinations, they are looking to form a new partnership with community health centers, known for providing health care to some of the hardest-to-reach populations. The national strategy from the White House plans to use health centers as key distribution points for the vaccine as well as providers for managing the longer-term effects of COVID in their communities, such as symptoms of long COVID. It also aims to engage health centers in vaccine distribution to improve access to vaccines in communities of color, which, to date, appear to be receiving vaccinations at disproportionately low rates, although race/ethnicity data on vaccinations are still limited. Biden’s national strategy also proposes that health centers should be able to directly access vaccine supply and encourages states and jurisdictions to engage health centers in local vaccine distribution plans.
Community health centers are a national network of safety net primary care providers that served nearly 30 million patients in 2019 who are disproportionately low-income, persons of color, uninsured, or publicly insured – groups that have been especially hard hit by the pandemic. Health centers are already playing a significant role in state and local responses to the pandemic – for example, virtually all (99%) health centers are providing tests, and some are even utilizing mobile clinics to take testing and medical services into hard-to-reach communities, such as agricultural worker housing, meatpacking facilities, American Indian reservations, and homeless encampments. Once vaccinations are further scaled up, health centers will likely deploy mobile clinics, help staff mass vaccination sites, and provide onsite and pharmacy-based vaccinations as described in the Biden plan.
However, there are a number of potential issues that could keep health centers from vaccinating at full capacity.
In a weekly federal survey, health centers are reporting that the greatest challenges in deploying the vaccine are supply and staffing needed to administer the vaccine (Figure 1). While vaccine supply is expected to increase in the coming months as manufacturing increases and new vaccines become available, staffing issues may be difficult to solve. Health centers have historically faced staffing challenges, and although layoffs at health centers have been relatively limited during the pandemic, some health center staff are experiencing burnout and the ramifications of becoming infected with the coronavirus.
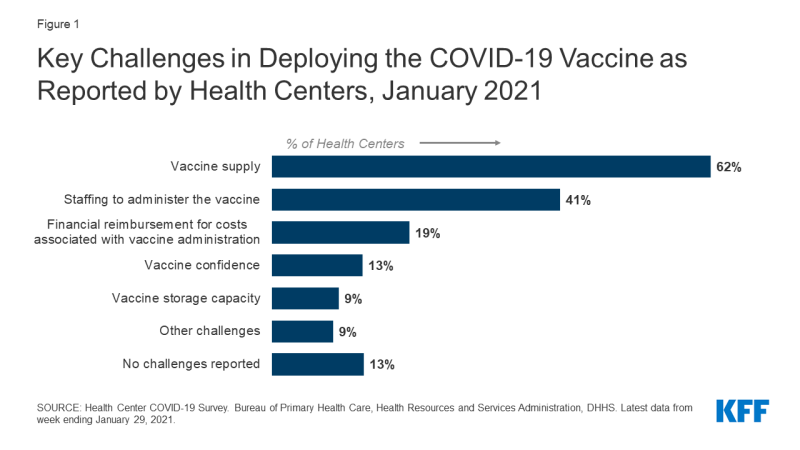
Figure 1: Key Challenges in Deploying the COVID-19 Vaccine as Reported by Health Centers, January 2021
Even after vaccine supply challenges are addressed, ongoing financial pressures may hinder health centers’ vaccination efforts. Health centers are still recovering from steep declines in patient revenues during the pandemic while operating costs have increased due to purchasing testing supplies, personal protective equipment, and operating telehealth programs. It is also possible that delayed reimbursement for administering the COVID-19 vaccine could slow health centers’ vaccination capacity. For example, Medicare plans to reimburse health centers similarly to flu vaccinations (based on reasonable cost) and pay for COVID-19 vaccinations after a health center files an annual cost report at the end of their accounting year – which could take until 2022 in some cases. Although only 10% of patients were Medicare beneficiaries in 2019, the number of Medicare patients varies widely across communities and is generally higher in rural health centers (14% of patients compared to 8% in urban health centers in 2019). Overall, assisting with state vaccination efforts that currently target adults over age 65 means that health centers could serve more Medicare beneficiaries than normal, particularly if they are required by state and local partnerships to reach beyond their patient populations and vaccinate older residents in their communities. Biden’s plan calls for increased federal funding for health centers to support this expanded role, although it is unclear if that funding will pass in a narrowly divided Congress and, if so, how quickly health centers can access funds.
There are considerable challenges for health centers to carry out vaccinations at their fullest capacity. Biden’s proposal to give health centers direct access to vaccine supply and receive new federal funding could, if implemented, help address these significant barriers and promote more equitable access to vaccinations in the hardest-to-reach communities.
