
The independent source for health policy research, polling, and news.
Nearly a Quarter of People Who Say They Were Disenrolled from Medicaid During the Unwinding Are Now Uninsured
Over Half Who Were Disenrolled Say They Put Off Needed Medical Care While Trying to Renew Medicaid
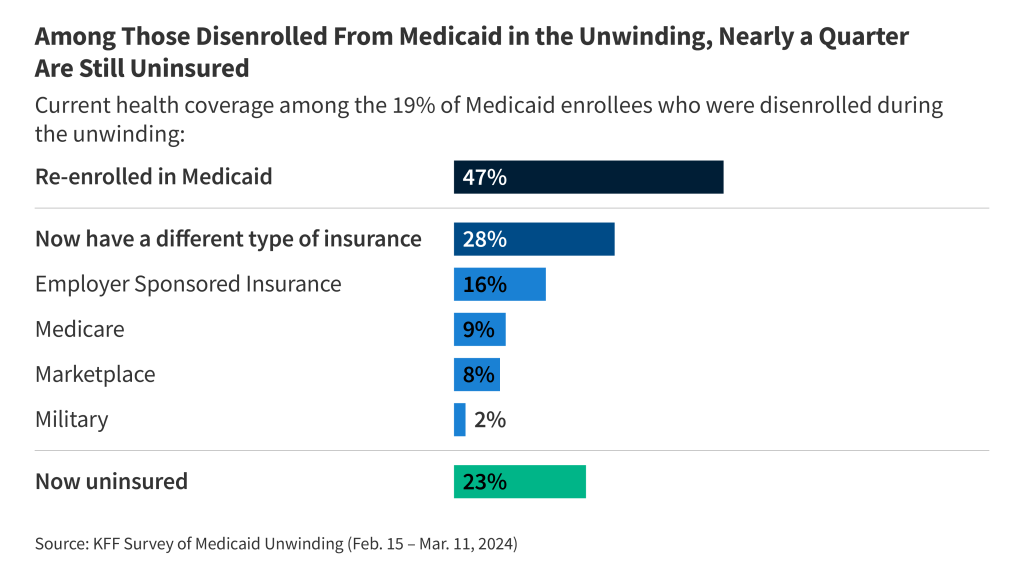
Nearly a quarter (23%) of adults who say they were disenrolled from Medicaid since early 2023 report being uninsured now, finds a new KFF national survey examining how the unwinding affected enrollees.
Overall, 19% of adults who had Medicaid prior to the start of unwinding say they were disenrolled at some point in the past year. Of this group, a large majority (70%) were left at least temporarily uninsured, while 30% already had another form of health coverage in place.
About half (47%) of those disenrolled say they subsequently re-enrolled in Medicaid, and more than a quarter (28%) now have another form of coverage—either through an employer, Medicare, the Affordable Care Act’s marketplace or health care for members of the military.
The survey examines adults who had Medicaid coverage in early 2023, just before states resumed eligibility checks and disenrollments after pandemic-era protections ended. Medicaid enrollees can be disenrolled for several reasons, including because they are no longer eligible or because they did not complete the renewal process due to paperwork issues, a late submission or other reasons.
About a third (35%) who tried to renew their coverage describe the process as difficult, and nearly half (48%) describe it as at least somewhat stressful. A majority (56%) of those disenrolled say they skipped or delayed care or prescriptions while attempting to renew their Medicaid coverage.
Among all adults who had Medicaid prior to the start of the unwinding, the vast majority (83%) retained their coverage or re-enrolled, while 8% are now uninsured and another 8% have other health insurance. The share who are now uninsured is larger in states that have not expanded Medicaid (17%) than in states that have (6%).
Across the United States, about 1 in 3 Medicaid enrollees have not yet completed their renewal process. KFF analysis shows considerable variation by state policies, which could affect the percent who have retained Medicaid, found other coverage or been left uninsured by the end of the unwinding.
Other findings from the survey include:
- At least three-quarters of those enrollees who now have other insurance or are uninsured say they are worried about affording the cost of health care services (76% and 78%, respectively), while fewer than half (47%) of enrollees who still have Medicaid express this concern. Among those who are now uninsured, more than half (54%) have not gotten another form of health insurance because of the cost.
- Two-thirds (64%) of adults who had Medicaid coverage prior to the start of unwinding took action to renew it. Among those who tried to re-enroll, 58% experienced at least one problem during the process, most commonly long phone wait times (44%).
- About 3 in 10 say gathering and submitting documents (29%) and figuring out what documents were needed to complete enrollment (28%) were very or somewhat difficult.
- Adults living in states that have not expanded Medicaid are more likely than those in expansion states to say they were asked to provide proof of residency when renewing their coverage.
- About a quarter (28%) of enrollees got help with their Medicaid renewal process during the unwinding, while an additional 17% wanted assistance but did not get it.
- About three-quarters (77%) of adults who were enrolled prior to the start of unwinding rate their experience with Medicaid as “excellent” (34%) or “good” (43%). About one in four give Medicaid a negative rating of either “fair” (19%) or “poor” (4%).
About the Medicaid Unwinding and KFF’s Survey
During the COVID-19 pandemic, states kept people continuously enrolled in Medicaid in exchange for enhanced federal funding. With the end of continuous enrollment on March 31, 2023, states are required to complete an eligibility renewal for all Medicaid and CHIP enrollees—a process commonly referred to as “unwinding.” KFF tracking shows that 20.1 million people (21%) have been disenrolled from Medicaid and 43.6 million people (46%) have had their coverage renewed since the unwinding began.
Designed and analyzed by public opinion researchers at KFF, the survey was conducted between February 15 and March 11, 2024, online and by telephone, among a representative sample of 1,227 U.S. adults who had Medicaid coverage in early 2023—prior to the start of unwinding on April 1st. Interviews were conducted in English and in Spanish. The margin of sampling error is plus or minus 4 percentage points. The report describes U.S. adults’ experiences with Medicaid renewals, disenrollments and coverage transitions or losses during the unwinding.