The independent source for health policy research, polling, and news.
Beneficiaries Who Switch to Medicare Advantage Have Lower Medicare Spending and Use Fewer Services – In the Prior Year – Than Those Who Stay in Traditional Medicare
Current Medicare Advantage Payment System May Overestimate Expected Costs for Plans
Medicare Advantage plans gain beneficiaries from traditional Medicare who have lower average spending and use fewer health services than similar beneficiaries who choose to remain in traditional Medicare, according to a new KFF analysis.
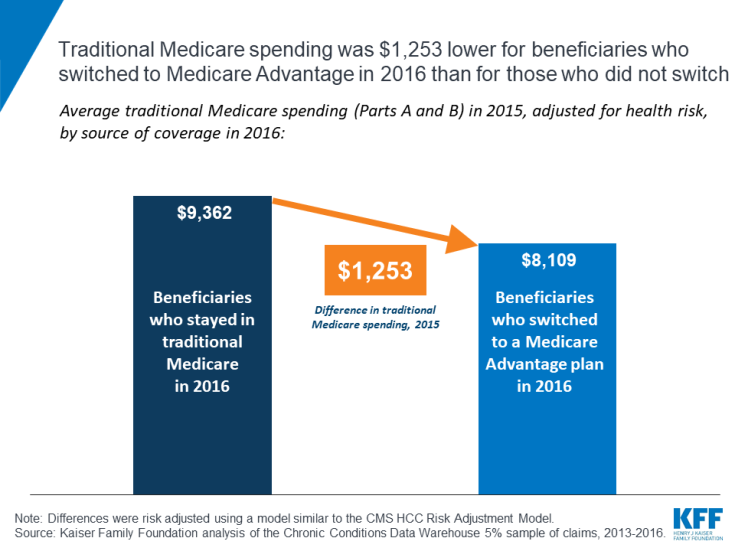
The analysis finds that people who switched from traditional Medicare to Medicare Advantage in 2016 had health spending in 2015 that was $1,253 less, on average, than the average spending for beneficiaries who remained in traditional Medicare (after adjusting for health risk).
The pattern held true even among beneficiaries with specific health conditions, including asthma, breast or prostate cancer and diabetes. For instance, among beneficiaries with diabetes who were in traditional Medicare in 2015, those who switched to Medicare Advantage in 2016 had Medicare spending in 2015 that was $1,072 lower, on average, than similar beneficiaries with diabetes who stayed in traditional Medicare (after adjusting for health risk).
The findings raise questions about whether Medicare Advantage plans tend to attract healthier and lower-cost beneficiaries and whether lower rates of service use among Medicare Advantage enrollees is attributable to care management or self-selection. Most notably, the study findings suggest that the current method of setting payments to Medicare Advantage plans based on spending for people in traditional Medicare may systematically overestimate expected costs of Medicare Advantage enrollees. Adjusting payments to reflect Medicare Advantage enrollees’ prior use of health services could potentially lower total Medicare spending by billions of dollars annually.
Setting payments to more accurately reflect expected costs would have major implications for Medicare spending, as Medicare Advantage plans cover 20 million people, about a third of all Medicare beneficiaries, and enrollment is expected to climb to over 30 million people within the next decade.