During Pandemic, Higher Premature Excess Deaths in U.S. Compared to Peer Countries Partly Driven by Racial Disparities
A new brief from the Peterson-Kaiser Health System Tracker looks at how the pandemic affected the excess mortality rate in 2020 and estimates how many potential years of life were lost. “Excess deaths” represent the number of deaths beyond what is expected in a typical year. “Premature” excess death measure accounts for age at excess death to estimate potential years of life lost up to age 75 over a typical year, using the OECD methodology. Overall, the U.S. had more than 500,000 excess deaths in 2020 compared to prior years, losing an estimated 3.6 million potential years of life.
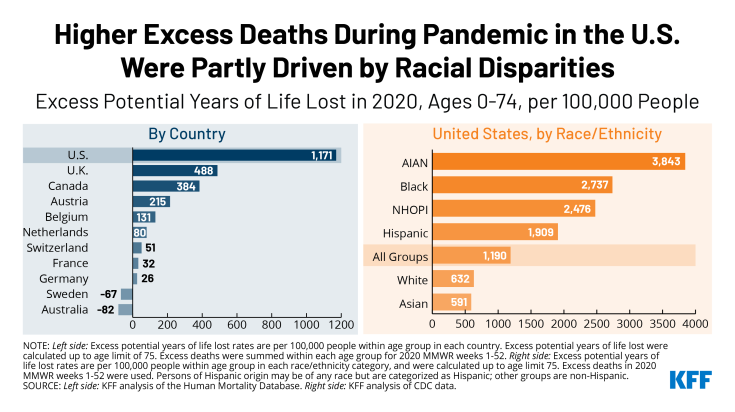
Relative to similarly wealthy countries, the U.S. had the highest overall premature excess mortality rate in 2020 with 1,171 excess potential years of life lost per 100,000 people (compared to an average of 126 excess potential years of life lost per 100,000 people in comparable countries). Among excess deaths in 2020, the average person lost 14 years of life in the U.S. compared to an average of 8 years in peer countries before the age of 75.
The higher premature excess death rate in the U.S. compared to peer nations was driven in part due to racial disparities. People of color under age 75 were more likely to have died in the U.S. during the pandemic in 2020 than white non-elderly individuals, as shown in the chart below. Among people under the age of 75, American Indian and Alaska Native, Black, Native Hawaiian and Other Pacific Islander, and Hispanic people had over 3 times the premature excess death rate in the U.S. in 2020 than the rate among White and Asian people. Of the potential years of life lost in the U.S., 30% were among Black people and another 31% were among Hispanic people, disproportionate to their share of the U.S. population.
The higher premature excess mortality rate among people of color in the U.S., and in the U.S. as a whole compared to similar countries, is likely due in part to higher COVID-19 risk factor rates and broader racial inequities. For more data and discussion of the gaps in premature excess mortality within the U.S. and among peer countries, please visit the Peterson-Kaiser Health System Tracker.