 How Many Employers Could Be Affected by the High-Cost Plan Tax
Issue Brief
How Many Employers Could Be Affected by the High-Cost Plan Tax
Issue Brief
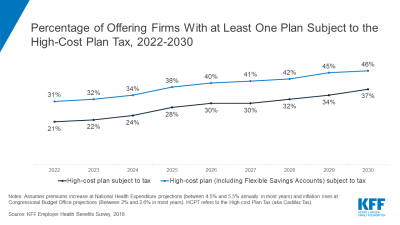
The high cost plan tax (HCPT) sometimes referred to as the Cadillac tax, is an excise tax on the cost of employer health benefit exceeding certain threshold. The HCPT provides a powerful incentive to control health plans costs over time, whether through efficiency gains or shifts in costs to workers. While many employers do not expect that the tax will take effect in 2022, others are already amending their health programs in anticipation. We estimate if the tax takes effect in 2022, 21% will be subject to the tax, increasing to 37% by 2030 unless firms reduce costs. Larger shares would be affected when counting workers’ voluntary contributions to Flexible Spending Accounts (FSAs)