The Trump Administration’s Final Rule on Section 1557 Non-Discrimination Regulations Under the ACA and Current Status
| Key Findings |
On June 19, 2020, the Trump Administration issued final regulations implementing Section 1557 of the Affordable Care Act. Section 1557 prohibits discrimination based on race, color, national origin, sex, age, and disability in health programs and activities receiving federal financial assistance. Notably, it is the first federal civil rights law to prohibit discrimination in health care based on sex. The final rule, issued in the midst of the ongoing COVID-19 pandemic, significantly narrows the scope of a rule issued in 2016 by the Obama Administration by:
Just after the Administration published the final rule, the Supreme Court ruled that sex discrimination includes sexual orientation and gender identity in the employment context. Based on that decision, two federal courts issued nationwide preliminary injunctions blocking parts of the final rule: NY and DC courts blocked provisions excluding sex stereotyping from the definition of sex discrimination, and the DC court also blocked the religious freedom exemption. The NY court is now considering whether to block other provisions of the rule, and other lawsuits are pending. |
Introduction
On June 19, 2020, the Department of Health and Human Services (HHS) finalized revised regulations implementing Section 1557 of the Affordable Care Act (ACA),1 which prohibits discrimination in health care based on race, color, national origin, sex, age, and disability in health programs and activities receiving federal financial assistance.2 The final rule (which mirrors a proposed rule issued by HHS in June of last year3) is a significant departure from the Obama Administration regulations issued in 2016. Specifically, the final rule eliminates nondiscrimination protections based on gender identity, as well as specific health insurance coverage protections for transgender individuals, adopts blanket abortion and religious freedom exemptions for health care providers, reduces protections for those with limited English proficiency, and limits the activities and entities covered, among other provisions. It also eliminates prohibitions on discrimination based on gender identity and sexual orientation in ten other federal regulations outside Section 1557.
The changes were scheduled to take effect on August 18, 2020, but a Supreme Court ruling in Bostock v Clayton County, Georgia,4 issued just days after the final regulation was released, found that discrimination based on sex encompasses sexual orientation and gender identity in the context of employment. Based on that decision, two federal courts have issued nationwide preliminary injunctions blocking the Administration from implementing parts of the final rule. A NY court blocked the implementation of provisions excluding sex stereotyping from the definition of sex discrimination.5 After the plaintiffs requested clarification about the scope of the preliminary injunction order, the court directed the plaintiffs to submit a list of provisions of the 2020 rule, beyond the definition of sex discrimination, that should be stayed in light of the Supreme Court’s Bostock decision for the court’s consideration.6 The DC court blocked the implementation of provisions excluding sex stereotyping from the definition of sex discrimination as well as provisions incorporating a blanket religious freedom exemption from claims of sex discrimination.7 Several other legal challenges to the rule are also pending.8
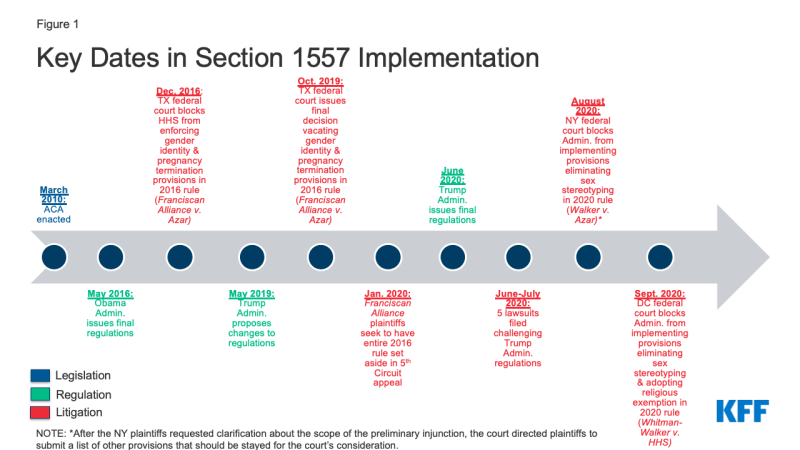
This issue brief summarizes HHS’s final rule and provides a side-by-side comparison to the Obama Administration 2016 rule (Table 1). It also examines HHS’s changes to other regulations, separate from Section 1557 (Table 2). Finally, it assesses the current status of the final rule in light of the recent Supreme Court ruling and subsequent legal challenges (Table 3). Figure 1 presents a timeline of key dates in Section 1557 implementation, including the development and revision of regulations and subsequent legal challenges. A more expansive timeline is contained in Table 4.
Background and HHS’s Rationale for Changes
Section 1557 incorporates protections from existing civil rights laws. These include Title VI of the Civil Rights Act of 1964 (race, color, and national origin), Title IX of the Education Amendments of 1972 (sex), the Age Discrimination Act of 1975, and Section 504 of the Rehabilitation Act of 1973 (disability). Notably, Section 1557 is the first federal civil rights law to prohibit discrimination on the basis of sex in health care. Section 1557’s protections took effect when the ACA was enacted on March 23, 2010. Implementing regulations issued by HHS under the Obama Administration became effective on July 18, 2016.9
The provisions of the 2016 rule that included gender identity and termination of pregnancy in the definition of sex discrimination were vacated by a federal trial court in Franciscan Alliance v. Azar. This case was brought in August 2016 by a group of religiously affiliated health care providers and states, led by Texas.10 In December 2016, a Texas federal district court issued a nationwide preliminary injunction preventing HHS from enforcing the challenged provisions while the case was pending. In October 2019, the court issued a final decision finding violations of the Administrative Procedures Act and the Religious Freedom Restoration Act and vacating the 2016 regulation’s inclusion of gender identity and termination of pregnancy in the definition of sex discrimination as exceeding the authority delegated to HHS by Congress. Specifically, the court found that HHS should have limited its regulatory definition of sex discrimination to a binary definition encompassing biological differences between males and females. The court also found that HHS should have incorporated Title IX’s blanket abortion and religious exemptions into its Section 1557 regulations. In January 2020, the religiously affiliated health care providers appealed to the 5th Circuit Court of Appeals, seeking to have the entire Obama Administration rule vacated. The case is now being briefed and will proceed at the same time as the various lawsuits challenging the Trump Administration’s final regulations (described below).
In contrast to the Franciscan Alliance case, other federal courts have granted relief to private individuals alleging Section 1557 discrimination claims based on gender identity. These courts relied on the text of Section 1557 as enacted in statute, not the contested regulation. For example, a federal district court permanently enjoined the Wisconsin Medicaid program’s categorical exclusion of gender affirming services from coverage, relying on the statute as enacted by Congress.11 Another federal district court case was brought on behalf of a transgender boy, who committed suicide after experiencing “extreme distress” from hospital staff repeatedly referring to him as a girl while he was admitted for psychiatric inpatient care.12 That court allowed a claim for emotional distress damages to proceed, finding that Section 1557’s statutory language prohibiting sex-based discrimination includes discrimination based on gender identity.13
In issuing its June 2020 final rule, HHS under the Trump Administration stated that its changes were needed to “address legal concerns,” relieve costs and regulatory burden, and reduce confusion, because it now views the regulations as inconsistent with or duplicative of other civil rights provisions.14 In support of its changes, HHS cited the Franciscan Alliance decision, though HHS’s changes to the regulations go beyond the issues raised in that case. In addition to gender identity and termination of pregnancy, HHS’s revised Section 1557 regulations substantially change, or in some cases entirely eliminate, existing provisions related to health insurance benefit design; language access; notices, grievance procedures, and enforcement; and which entities are covered (Table 1). Beyond the Section 1557 regulations, HHS removes prohibitions on discrimination based on gender identity and sexual orientation in ten other Medicaid, private insurance, and education program regulations (Table 2). It also adds abortion and religious exemptions to existing regulations that prohibit sex discrimination in education programs under Title IX.
Key Changes in the Trump Administration’s Final Rule
Sex Discrimination
Gender Identity
In the final rule, HHS eliminates entirely Section 1557’s regulatory definition of sex discrimination, as defined by the 2016 rule to include gender identity and sex stereotyping. The preamble notes that, while HHS “declines to replace it with a new regulatory definition. …the final rule reverts to, and relies upon, the plain meaning of the term [sex] in the statute” which in “its original and ordinary public meaning refers to the biological binary of male and female that human beings share with other mammals.”15 HHS also eliminates the definition of gender identity, which previously included gender expression and transgender status. In addition, it removes specific provisions that required covered entities to treat individuals consistent with their gender identity. Neither the 2020 final rule nor the 2016 rule recognizes discrimination on the basis of sexual orientation alone as a prohibited form of sex-based discrimination.16
Removing gender identity and sex stereotyping from the definition of prohibited sex-based discrimination could allow health care providers to refuse to serve individuals who are transgender or who do not conform to traditional sex stereotypes. For example, a health care provider could refuse to treat a patient for a cold or a broken arm based on the patient’s gender identity or refuse to accept a transgender individual in favor of a person who is not transgender when accepting new patients.17 The resulting inability to access needed health care services could exacerbate health disparities experienced by LGBTQ people, such as higher rates of depression and suicide attempts, higher risk of HIV/AIDS, higher use of tobacco and drugs, and higher risk of breast cancer.18 As noted above, two federal district courts in NY and DC have issued nationwide preliminary injunctions blocking the Administration from implementing the provisions of the final rule excluding sex stereotyping from the definition of sex discrimination, and the NY court is now considering whether additional provisions of the final rule should be stayed in light of Bostock. Because the Franciscan Alliance court previously vacated the 2016 rule’s inclusion of gender identity from the definition of sex discrimination, other federal district courts could not subsequently restore the prior regulatory provision. However, given the Supreme Court’s recent Bostock decision (discussed below), further litigation is likely to address the inclusion of gender identity as part of prohibited sex discrimination under Section 1557.
The final rule no longer explicitly prohibits covered entities from denying or limiting services that are ordinarily or exclusively available to one sex or gender when those services are sought by an individual of a different sex or gender. In contrast, the 2016 regulation prohibited differential coverage of services based on the fact that an individual’s sex assigned at birth, gender identity, or gender in a medical or health plan record differs from the one to which such services are ordinarily or exclusively available. For instance, under the previous regulation, health plans could not deny medically necessary treatment for ovarian cancer in a transgender man based on his gender identity.19 Commenters responding to the Administration’s draft rule issued in 2019 worried that the rule ”would allow or encourage providers to deny basic healthcare to individuals who identify as transgender.”20 While HHS noted that ”all people should be treated with dignity and respect, regardless of their characteristics including their gender identity, and they should be given every protection afforded by the Constitution and the laws passed by Congress,”21 the rule does not extend such protections to transgender people.
The final rule also eliminates the provision that prohibits a health plan from categorically or automatically excluding or limiting coverage for health services related to gender transition. Under the final rule, it appears an issuer could deny coverage for a hysterectomy that a provider determines is medically necessary to treat a patient’s gender dysphoria, even though hysterectomies are covered in other circumstances.22 Despite evidence to the contrary, as cited in the preamble to the Obama Administration’s 2016 rule,23 HHS now argues that there is a lack of consensus on care for transgender people and explicitly states, “a medical provider may rightly judge a hysterectomy due to the presence of malignant tumors to be different in kind from the removal of properly functioning and healthy reproductive tissue for psychological reasons, even if the instruments used are identical.”24 This is in contrast to the 2016 regulation which stated that such categorical exclusions are outdated and do not reflect current standards of care.25
Changes to Regulations Beyond Section 1557: Gender Identity and Sexual Orientation
Beyond the Section 1557 regulations, HHS also eliminates explicit nondiscrimination protections related to gender identity and sexual orientation in ten other existing regulations. HHS characterizes these changes as “limited conforming amendments.”26 These regulations include those that govern Medicaid managed care entities, state Medicaid programs, PACE organizations, group and individual health insurance issuers, Marketplaces, qualified health plan issuers, agents and brokers that assist with Marketplace applications and enrollment, and education programs that receive federal financial assistance. In the past, these regulations, some of which had been in place for several years, provided explicit protections against discrimination based on sexual orientation and gender identity. Without these protections, Medicaid managed care entities could discriminate against LGBTQ beneficiaries in policies authorizing covered services, and PACE organizations could refuse to serve someone based on their sexual orientation, for example.27
Abortion and religious exemptions
The final Section 1557 rule allows health care providers and other covered entities to invoke blanket abortion and religious objection exemptions from the regulations’ general prohibition on sex discrimination.28 The regulation incorporates provisions from Title IX that exempt covered entities from complying with the general prohibition against sex discrimination if doing so (1) involves providing or paying for abortion29 or (2) would be inconsistent with the organization’s religious tenants.30 The regulation also exempts entities from having to comply with the Section 1557 regulations if doing so would violate a specific list of existing, as well as any future, federal abortion and religious exemption laws.31 Additionally, as noted above, HHS eliminates the 2016 regulatory definition of sex-based discrimination, which had included discrimination on the basis of pregnancy, false pregnancy, termination of pregnancy, or recovery therefrom, and childbirth or related medical conditions.32 Commenters noted that the regulation might open the door to discrimination based on abortion history.33 “Commenters also identified a variety of other women’s healthcare services related to pregnancy that may be implicated, including prenatal and postpartum services, tubal ligations, and birth control (both as a contraceptive and when used to treat other medical conditions). . . [and] infertility treatments including in vitro fertilization ….”34 In its response, HHS ”decline[d] to speculate on particular hypotheticals related to the termination of pregnancy and will proceed on the specific facts and circumstances of each case that may arise.”35
This change means that people seeking abortion or other health care services that violate a provider’s religious beliefs may be denied, delayed, or discouraged from seeking necessary care, placing them at risk of serious or life-threatening results in emergencies and other circumstances where the individual’s choice of health care provider is limited.36 The Obama Administration regulation provided that covered entities did not have to comply with Section 1557’s prohibition of discrimination on the basis of sex if doing so would have violated existing federal abortion and religious exemption laws, but it did not include a blanket religious exemption.37 When the Obama Administration issued Section 1557 regulations in 2016, HHS rejected incorporating Title IX’s blanket religious exemption because Title IX is limited to educational institutions, which it concluded are significantly different from the health care context.38 While students and parents typically have a choice about whether to select a religiously affiliated educational institution, individuals’ choice of health care provider may be limited, especially in rural areas, locations where hospitals are run by religious institutions, or emergencies.39 In 2016, HHS explained that it instead would rely on the Religious Freedom Restoration Act to make individual case-by-base determinations about “whether a particular application of Section 1557 substantially burdened a covered entity’s exercise of religion, and if so, whether there were less restrictive alternatives available.”40 This meant that, under the Obama Administration regulation, there may have been some instances in which a provider’s religious beliefs would have exempted it from providing services, but other instances, based on the facts of a particular case, in which an individual was entitled to receive services despite a provider’s religious objection. As noted above, the DC federal district court issued a nationwide preliminary injunction blocking the implementation of the Trump Administration provisions incorporating a blanket religious freedom exemption from claims of sex discrimination.
Non-Discrimination in Health Coverage
In addition to the specific gender identity provisions discussed above, HHS also eliminates the entire regulation prohibiting discrimination in health insurance issuance, coverage, cost-sharing, marketing, and benefit design. Under the 2016 regulations, covered entities were prohibited from taking the following actions on the basis of race, color, national origin, sex, age, or disability:
- Denying, canceling, limiting, or refusing to issue or renew a health insurance policy;
- Denying or limiting coverage of a health insurance claim;
- Imposing additional cost sharing or other limitations or restrictions on coverage; or
- Using discriminatory marketing practices or insurance benefit designs.
Without these provisions, health plans could, for example, cover inpatient treatment for eating disorders for men but not women or cover bariatric surgery for adults except those with certain developmental disabilities.41 Other benefit designs that might be discriminatory include placing all or most prescription drugs used to treat a specific condition on a health plan’s highest cost formulary tier, applying age limits to services that have been found to be clinically effective at all ages, or requiring prior authorization or step therapy for all or most medications in drug classes such as protease inhibitors for HIV or immune suppressants regardless of medical evidence.42 Other ACA provisions regarding guaranteed issue continue to apply.
Language Access
In the final rule, HHS reduces the standards governing access to language assistance services, including oral interpretation and written translation, for individuals with limited English proficiency (LEP). Specifically, HHS replaces the requirement in the 2016 regulation for covered entities to take reasonable steps to provide meaningful access to “each individual with LEP eligible to be served or likely to be encountered”43 with a requirement to provide meaningful access to ”limited English proficient individuals” generally. Language access protections are required to prevent discrimination based on national origin. HHS notes that commenters expressed concerns that this change would weaken nondiscrimination requirements and result in some LEP individuals being unable to access health care; many commenters further indicated that lack of understanding in a medical setting could cause harm and possibly death to patients with LEP.44 In response, HHS indicated that the 2016 standard was a stringent requirement that could be interpreted to require an entity to provide language assistance services to every LEP individual with which it comes in contact. It says that by adopting this revised language, it is applying the same standard to both health and human service programs within the department and that it conforms to existing LEP guidance.45
HHS also replaces the test to determine when covered entities must provide language access services with one that removes the emphasis on the importance of the communication to the specific individual. Under the 2016 regulation, the test to determine whether an entity is in compliance with requirements to provide meaningful access to LEP individuals gave “substantial weight” to the nature and importance of the health program or activity and the communication at issue to the specific individual. Under the final rule, HHS applies a different test that balances a variety of factors to determine when language assistance services are required, including the overall number of LEP individuals eligible to be served or likely to be encountered, the frequency with which any LEP individuals come into contact with the covered program or activity, and the costs involved. HHS also eliminates the provision that allows HHS to consider whether the covered entity has an effective written language access plan when assessing compliance with requirements to provide meaningful access. In addition, HHS eliminates remote video interpreting standards and instead includes standards only for remote audio interpreting services. Some commenters expressed concerns that the revised test to assess compliance with providing meaningful access to LEP individuals places too much of an emphasis on costs and is too broad, lacks clarity, and does not ensure that translation and other language services are available under important medical circumstances, In response, HHS notes that the revised test is consistent with existing LEP guidance and intended to strike a balance between ensuring access by LEP individuals while not imposing undue burdens on small businesses, small local governments, or small nonprofits.46
HHS eliminates requirements that non-discrimination notices (discussed further below) must include the availability of language assistance services and taglines in the top 15 languages spoken by LEP individuals in the state. Some commenters stated that the removal of the notice and tagline provisions will result in LEP individuals having less knowledge of available language assistance and will be more likely to rely on informal sources of assistance through family members.47 HHS responded that the rule maintains the requirement that covered entities provide a notice of discrimination and taglines whenever necessary to ensure meaningful access, and that it is only removing the requirement that all significant communications contain taglines. It also says that this requirement caused significant unanticipated expenses and indicates it has determined that the financial burden on covered entities was not justified by the protections or benefits it provided to LEP individuals.48
Notice and Enforcement
The final rule eliminates all of the previous Section 1557 nondiscrimination notice and grievance procedure requirements. Covered entities with at least 15 employees no longer must adopt a grievance procedure or designate at least one employee to coordinate its Section 1557 responsibilities. Covered entities also no longer must provide notice of their nondiscrimination policies in significant communications (such as handbooks and outreach publications), physical locations where the entity interacts with the public, and on their website homepage. HHS notes that the regulations implementing Title VI, Title IX, the Age Act and Section 504 “already contain notice provisions” and concluded that creating a single notice standard in the Section 1557 regulation “has led to an unjustifiable burden and understandable confusion.”49
HHS projects that all of its proposed Section 1557 changes will result in approximately $2.9 billion in undiscounted cost savings over the first five years after implementation, primarily from eliminating the notice and tagline requirements.50 HHS says that its original cost projections for the notice and tagline requirements did not account for approximately $585 million in additional average annual costs over the next five years.51
Although HHS eliminated provisions that recognize the right of private individuals and entities to file lawsuits in federal court to challenge alleged violations of Section 1557, HHS states that it no longer intends to take a position about whether the statute in fact provides such a right. Instead, HHS says that “[t]o the extent that Section 1557 permits private rights of action, plaintiffs can assert claims under Section 1557 itself rather than under the Department’s Section 1557 regulation.”52 This leaves the right to sue under Section 1557 for courts to decide. For example, in the cases cited above, individuals filed lawsuits in federal court alleging that the Wisconsin Medicaid program’s categorical exclusion of gender affirming services from coverage and California hospital staff’s repeated mis-gendering of a transgender boy who was admitted for inpatient psychiatric care and subsequently committed suicide were unlawful discrimination, relying on the statute as enacted by Congress. HHS also eliminated the regulation that provides that money damages are available to compensate those injured by violations of Section 1557. Instead, HHS will rely on the enforcement provisions of the underlying civil rights statutes, Title VI, Title IX, the Age Act, or Section 504, when determining when money damages are available for a violation of Section 1557.53
Scope of Applicability
Covered Entities Receiving Federal Financial Assistance
The final rule narrows the scope of the regulations to cover only the specific programs and activities that receive federal funding, and not all operations, of health insurers that are not principally engaged in the business of providing health care. The prior rule applied Section 1557’s non-discrimination protections broadly to health programs and activities, defining them to include all operations of an entity receiving federal financial assistance that is principally engaged in the provision or administration of health-related services or health-related insurance coverage. For example, all health plans offered by an issuer that participated in a Marketplace were subject to Section 1557.54 Under the final rule, if this issuer is not principally engaged in the business of providing health care (as opposed to health insurance), only its Marketplace plans are covered and any plans it offers outside the Marketplace are not subject to Section 1557. The change also means that the regulations do not apply to short term limited duration insurance, employer-sponsored group health plans, self-insured church plans, the Federal Employees Health Benefits Program, or non-Federal governmental plans, so long as coverage is offered by an entity that is not principally engaged in the business of providing healthcare and does not receive Federal financial assistance.55 In support of this change, HHS states that the “‘business of providing . . . health care’ differs substantially from the business of providing health insurance coverage (or other health coverage) for such health care.”56 The end result is to reduce the number and type of entities required to comply with Section 1557’s non-discrimination protections. The final rule continues to apply to health care providers, such as physicians’ practices, hospitals, nursing homes, and organ procurement centers that receive federal funds such as Medicare (excluding Part B57) or Medicaid payments; health-related education and research programs; state Medicaid, CHIP, and public health agencies; and state-based Marketplaces.58
HHS programs and activities
HHS also applies the regulations only to health programs and activities that it administers under ACA Title I (Marketplaces), instead of all HHS-administered programs and activities. Health programs and activities conducted by HHS outside ACA Title I include other CMS programs and activities, the Health Services Research Administration (such as clinics operated by the National Health Service Corps), the Centers for Disease Control, the Indian Health Services (including IHS tribal hospitals), and the Substance Abuse and Mental Health Services Administration.59 Under the prior regulation, these programs were subject to the Section 1557 regulations.
discrimination based on association
The final rule eliminates the prohibition against discrimination based on an individual’s association or relationship with someone else based on that other person’s race, color, national origin, sex, age, or disability. These grounds for discrimination were recognized by the former Section 1557 regulations. Examples of discrimination based on association that were recognized by the prior regulations include a doctor refusing to see a white patient because the patient has a biracial child or a health plan issuer excluding a provider from its network because the provider’s patients are primarily LEP individuals.60 A hearing parent who is required by a hospital to interpret for her deaf child would no longer be able to pursue a discrimination claim based on association under the Section 1557 regulations.61
Disability Discrimination
Although HHS requested public comment on whether some of Section 1557’s disability discrimination provisions should be changed, it did not adopt many changes in this area. Specifically, HHS did not exempt entities with less than 15 employees from the requirement to provide auxiliary aids and services to ensure effective communication with people with disabilities nor did HHS create an undue hardship exemption from the provision requiring covered entities to make reasonable modifications in policies, practices, and procedures to avoid disability-based discrimination. Instead, HHS notes that the entities would not be required to comply with either of these provisions if they can demonstrate that doing so would result in a fundamental alternation of their services, programs, or activities or an undue financial or administrative burden, consistent with the ADA regulations.62 HHS also did not create additional exemptions for covered entities subject to the architectural standards applicable to public buildings, especially with regard to multi-story building elevator and TTY requirements, noting that the ”great majority” of entities already are subject to these standards.63 HHS did finalize a change to the definition of auxiliary aids and services by eliminating ”acquisition or modification of equipment and devices; and other similar services and actions” from the list of examples.64
The Supreme Court’s Bostock Decision and Legal Challenges to the Final Rule
Just after the Administration published its final rule in June 2020, the Supreme Court decided Bostock v. Clayton County, Georgia, a sex-based employment discrimination case with implications for Section 1557. In Bostock, the Court found that Title VII of the Civil Rights Act of 1964 protects employees against discrimination because of their sexual orientation or gender identity. In the preamble to the Section 1557 final rule, the Trump Administration acknowledged the Bostock decision, which was still pending at that time. Specifically, the Administration said that it “continues to expect that a holding by the U.S. Supreme Court on the meaning of ‘on the basis of sex’ under Title VII will likely have ramifications for the definition of ‘on the basis of sex’ under Title IX [as] Title VII case law has often informed Title IX case law.”65 However, HHS also noted that the “binary biological character of sex (which is ultimately grounded in genetics) takes on special importance in the health care context” and asserted that “[t]hose implications might not be fully addressed by future Title VII rulings even if courts were to deem the categories of sexual orientation or gender identity to be encompassed by the prohibition on sex discrimination in Title VII.”66 Rather than revisiting its revised Section 1557 rule in light of Bostock after the Court issued its decision, the Administration argued that Bostock’s “holding was limited to Title VII” and the case‘s “applicability to contexts outside of employment discrimination is a question for future courts to decide.”
Relying in part on Bostock, two federal district courts have issued nationwide preliminary injunctions preventing the Administration from implementing parts of the Section 1557 final rule. On August 17, 2020, the day before the final rule was to take effect, the Eastern District of New York blocked the Administration from implementing provisions excluding sex stereotyping from definition of sex discrimination in Walker v. Azar, a case brought by two transgender women of color. On September 2, 2020, the DC federal district court blocked the Administration from implementing provisions excluding sex stereotyping from the definition of sex discrimination as well as from incorporating a blanket religious exemption from sex discrimination claims in Whitman-Walker Clinic v. HHS, a case brought by health care and social service providers who serve LGBTQ people and LEP people. While the plaintiffs in both the NY and DC cases also sought to have gender identity restored to the Section 1557 rule’s definition of sex discrimination, both courts concluded that they lacked authority to do so because the Franciscan Alliance court previously vacated the inclusion of gender identity from the 2016 regulations.67 The preliminary injunctions issued by the NY and DC courts block implementation of the 2020 regulations, reverting back to the 2016 regulations, which as a result of Franciscan Alliance no longer include gender identity in the definition of sex discrimination. After the NY plaintiffs requested clarification about the scope of the preliminary injunction order, the court directed the plaintiffs to submit a list of provisions of the 2020 rule, beyond the definition of sex discrimination, that should be stayed in light of Bostock for the court’s consideration.
Given the Bostock decision, it is likely that further litigation will address whether gender identity should be restored to Section 1557’s definition of sex discrimination. As the DC court noted when issuing its preliminary injunction, the Supreme Court in Bostock “expressly assumed that ‘sex’ [in Title VII] ‘refer[red] only to biological distinctions between male and female.”68 Notably, the Supreme Court went on to conclude that “it is impossible to discriminate against a person for being homosexual or transgender without discriminating against that individual based on sex.”69 The DC acknowledged that other federal courts, both pre- and post-Bostock have concluded that sex discrimination under Title IX includes gender identity, and “Bostock, at the very least, has significant implications for the meaning of Title IX’s prohibition on sex discrimination.”70 Consequently, for purposes of deciding whether the Trump Administration’s changes to Section 1557’s regulatory definition of sex discrimination violated the Administrative Procedures Act, the DC court concluded that “it was arbitrary and capricious for HHS to eliminate the 2016 Rule’s explication of that prohibition without even acknowledging — let alone considering — the Supreme Court’s reasoning or holding” in Bostock.71
The remaining provisions of the Trump Administration’s final rule remain in effect. The DC court denied the Whitman-Walker plaintiffs’ request to apply the preliminary injunction to other parts of the final rule, including (1) the elimination of the prohibition on categorical coverage exclusions for gender-affirming care, (2) the elimination of notice and tagline requirements, (3) the restriction of the rule’s scope to apply only to HHS-administered programs and activities under ACA Title I, and not all HHS programs and activities, (4) the exclusion of certain activities of health insurance issuers not principally engaged in the business of providing health care from the final rule, and (5) provisions regarding the appropriate legal standard to be applied to Section 1557 claims.
Other cases challenging the Trump Administration’s Section 1557 final rule are pending. A transgender man and health and social service providers serving LGBTQ and LEP people filed a case in Massachusetts federal district court (Boston Alliance of Gay, Lesbian, Bisexual & Transgender Youth v. HHS), and a group of 23 states led by New York filed a case in the Southern District of New York (NY v. HHS). The plaintiffs in NY v. HHS have filed a motion for partial summary judgement, seeking to have the entire 2020 rule vacated. In another case brought by the state of Washington (WA v. HHS), the Western District of Washington denied a preliminary injunction, finding that the state did not have standing to bring a lawsuit challenging the final rule because it had not established that it was injured. Subsequently, the state voluntarily dismissed the case without prejudice. Table 3 summarizes the current litigation challenging the final rule.
Looking Ahead
The final rule, issued in the midst of the ongoing COVID-19 pandemic, substantially narrows, and in many cases entirely eliminates, the prior regulations’ existing nondiscrimination protections in meaningful ways. Section 1557 sought to standardize the protections and processes that prohibit discrimination in health care for all protected populations. Section 1557 also recognizes intersectional discrimination that affects people who belong to multiple protected classes; for example, discrimination against an African-American woman could be discrimination on the basis of both race and sex.72 While HHS maintains that it “is committed to ensuring the civil rights of all individuals who access or seek to access health programs or activities of covered entities,”73 the final rule substantially scales back non-discrimination protections.
The Supreme Court’s Bostock decision has significant implications for the final rule’s elimination of protections based on gender identity and sexual orientation, with two federal district courts blocking the Administration from implementing parts of the rule. Nationwide preliminary injunctions issued by federal district courts in NY and DC prevent the Administration from implementing provisions removing sex stereotyping from the rule’s definition of sex discrimination, and the NY court is now considering whether to expand its preliminary injunction to block additional provisions of the rule in light of Bostock. The DC court’s preliminary injunction also prevents the Administration from implementing the provision adopting a blanket religious exemption from sex discrimination claims. In another case, the state of NY is asking another NY federal district court to grant its motion for partial summary judgment, vacating the entire 2020 rule. The final outcome of these cases, other pending challenges to the Trump Administration’s final rule, and the pending Franciscan Alliance case challenging the 2016 rule will continue to shape the Section 1557 regulations.
Moreover, the final rule, while reshaping the regulatory protections, does not change the underlying statutory protections of Section 1557 as enacted by Congress. As noted above, some federal courts have recognized claims of discrimination and awarded relief under Section 1557 based on the statute itself and may continue to do so, regardless of regulatory changes. While the HHS Office for Civil Rights’ enforcement of Section 1557 is substantially narrowed under the rule, in terms of the scope of covered entities and the type of claims constituting prohibited discrimination, federal courts could continue to apply Section 1557’s statutory protections more broadly and provide relief to individuals experiencing discrimination in the health care context. Finally, regardless of the outcome of these challenges, the final rule does not prohibit states from outlawing health care discrimination on the basis of gender identity, sexual orientation, or other grounds beyond those recognized under federal law,74 as several states already have done.75
This work was supported in part by the Elton John AIDS Foundation. We value our funders. KFF maintains full editorial control over all of its policy analysis, polling, and journalism activities.