Access to Care for the Insured and Remaining Uninsured: A Look at California During Year One of ACA Implementation
Usual Sources of Care
Adults who gained coverage are more likely to be linked to care than those who remained uninsured. Newly insured adults were more likely than those who remained uninsured in fall 2014 to have a usual source of care, or a place to go when they are sick or need advice about their health (not counting the emergency room); they were also more likely to have a regular doctor at their usual source of care. Previously insured adults were also more likely than the uninsured to have a regular site of care and regular provider. These findings hold across coverage type. Having a usual source of care or regular doctor is an indicator of being linked to the health care system and having regular access to services. These patterns reinforce a large body of research that finds that gaining coverage is associated with improved access to care. However, results also indicate that the newly insured are less likely than the previously insured to have a usual source of care or regular doctor. This finding may indicate that newly insured adults are still navigating the health care system and are not as settled into regular care as their previously insured counterparts. Compared to 2013, there was no change in the share of Medi-Cal enrollees who reported having a usual source of care or regular doctor, while uninsured adults in 2014 were less likely than those in 2013 to say they have a usual source of care (but not a regular doctor).1
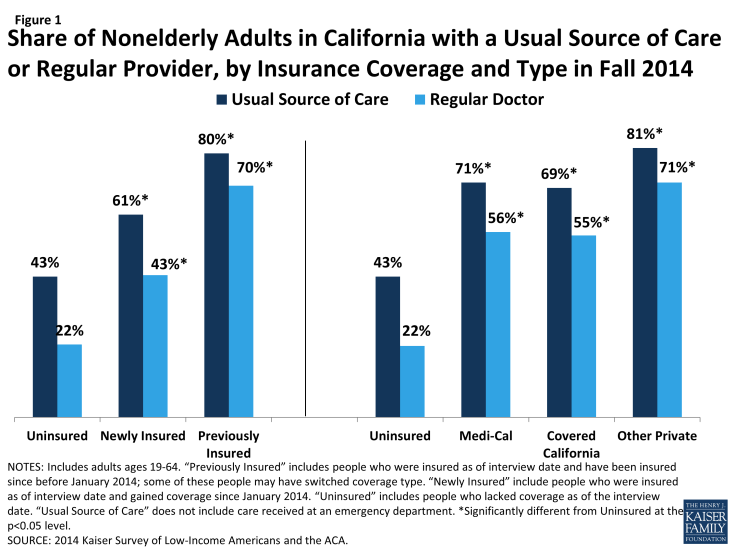
Figure 1: Access to Care for the Insured and Remaining Uninsured: A Look at California During Year One of ACA Implementation
Newly insured adults were more likely to change where they usually go for care than their previously insured counterparts. Nearly a fifth (19%) of newly insured adults who have a usual source of care reported that they changed the place they usually go for care since gaining their coverage. Uninsured adults in 2014 were not significantly more likely to say they changed their usual source of care compared to uninsured adults in 2013, and there were no significant differences between the rates of uninsured and newly insured adults changing their usual source of care in 2014. However, newly insured adults in 2014 were more likely than previously insured adults to change their usual source of care. Most newly insured adults who changed their site of care reported that it was due to their insurance, a significantly higher rate than the previously insured. There were no significant differences in the likelihood of Medi-Cal or Covered California enrollees changing their usual source of care, and Medi-Cal enrollees in 2014 were no more likely than those in 2013 to say they changed where they usually go for care.
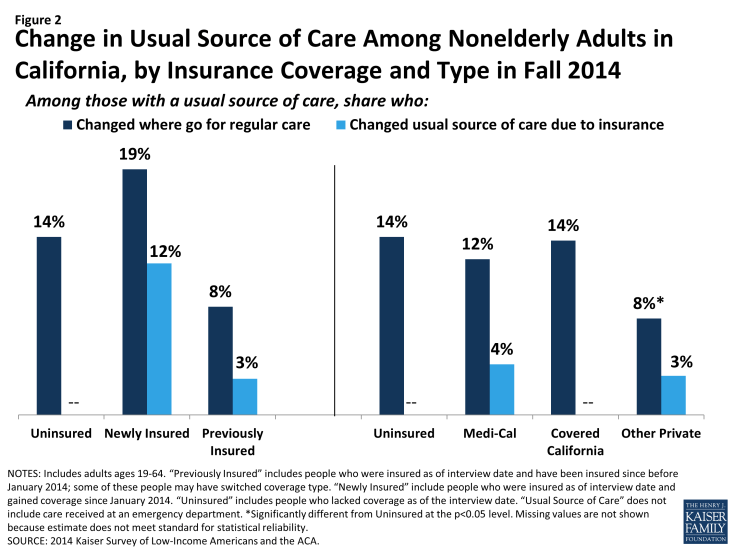
Figure 2: Change in Usual Source of Care Among Nonelderly Adults in California, by Insurance Coverage and Type in Fall 2014
Clinics remain an important source of care for both the uninsured and the newly insured. Both uninsured and newly insured adults with a usual source of care are most likely to use a clinic or health center for that care. In contrast, previously insured adults were most likely to use a doctor’s office or HMO as their usual source of care. Historically, clinics and health centers were crucial “safety net” providers for uninsured people, and the share of uninsured adults using clinics as their usual source of care was unchanged since 2013. Though some of the newly insured have changed their source of care, many continue to rely on these providers. According to policy experts from county health systems, this pattern may reflect lack of understanding of new health care options among the newly insured. Alternatively, it could reflect community health centers’ efforts to retain patients after helping them enroll in health coverage.
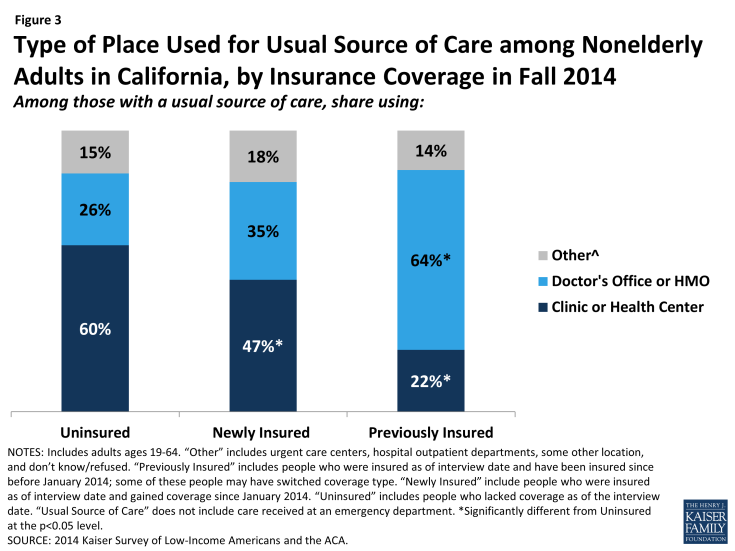
Figure 3: Type of Place Used for Usual Source of Care among Nonelderly Adults in California, by Insurance Coverage in Fall 2014
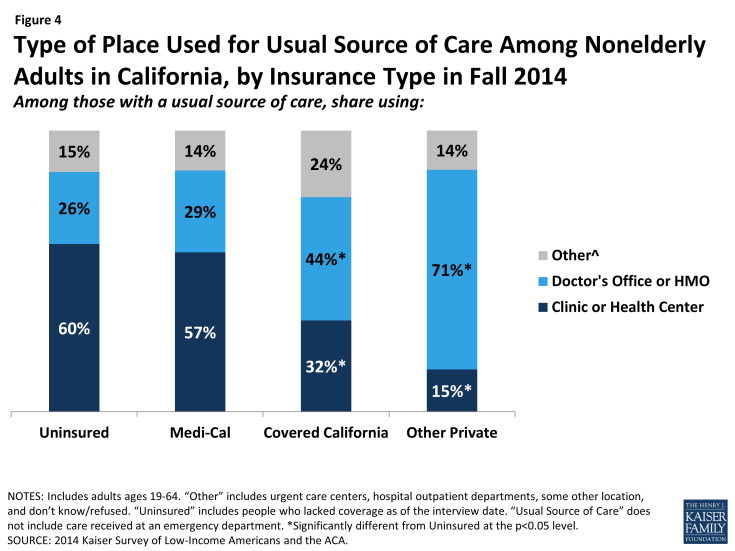
Figure 4: Type of Place Used for Usual Source of Care Among Nonelderly Adults in California, by Insurance Type in Fall 2014
Comparing site of care by type of coverage reveals that those enrolled in Covered California (44%) or other private coverage (71%) were more likely than Medi-Cal enrollees (29%) to choose a doctor’s office as their usual source of care, with adults with other private coverage most likely to do so. Medi-Cal enrollees were most likely to use clinics or health centers for their usual care (57%). This pattern is in line with pre-ACA patterns, which showed that a plurality of adults with Medi-Cal used clinics or health centers for their regular care.2 Comparing the 2013 and 2014 surveys indicates that a significantly larger share of Medi-Cal adults with a usual source of care is relying on clinics. This change could indicate that, as uninsured adults gain Medi-Cal coverage, they still use the clinics and health centers that they relied on when they were uninsured.
Uninsured adults are most likely to choose their site of care based on affordability, whereas newly insured adults are most likely to choose based on convenience. In the past, many uninsured adults reported that they chose their usual source of care because it was affordable, a pattern that is also seen among adults who were uninsured in 2014. More than a third (37%) of uninsured adults say they use their usual source of care because it is affordable, a share not significantly different than the uninsured in 2013 reported. In contrast, adults who gained coverage in 2014 were more likely to say they chose their usual source of care because it was convenient (40%). Previously insured adults were most likely to choose their site of care because their preferred provider is there (37%). As the newly insured establish relationships with a regular doctor at their usual source of care, it is possible that they too will begin to seek out routine care at a place where their preferred doctor is available.
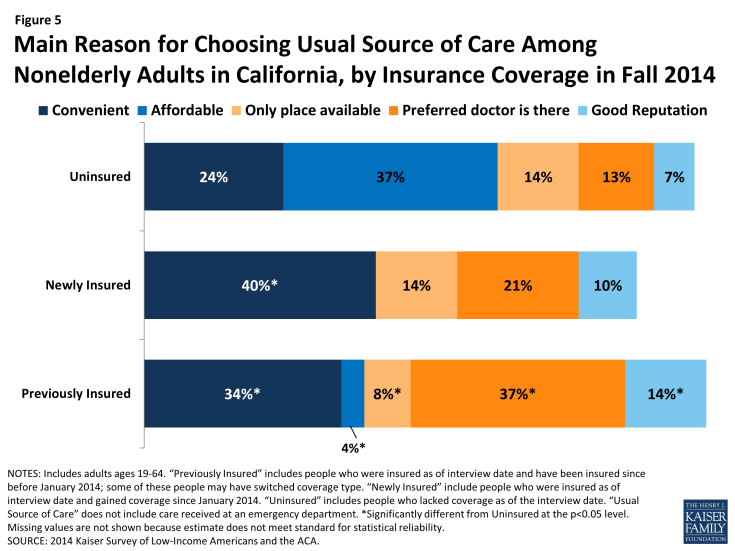
Figure 5: Main Reason for Choosing Usual Source of Care Among Nonelderly Adults in California, by Insurance Coverage in Fall 2014
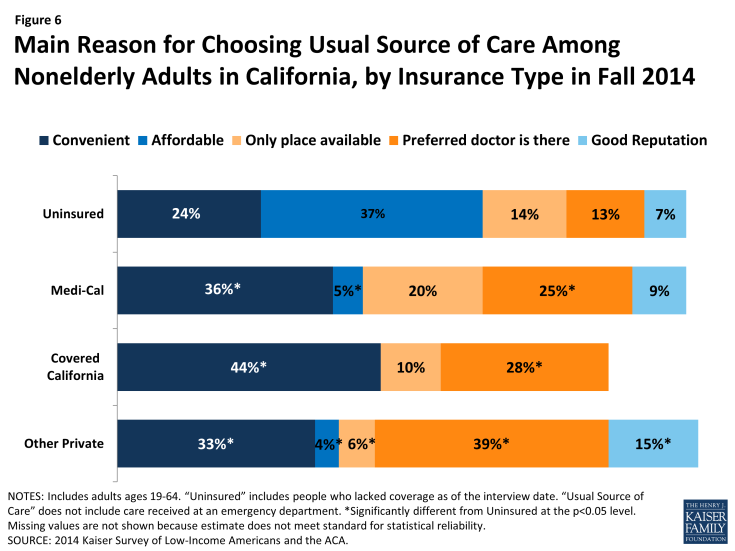
Figure 6: Main Reason for Choosing Usual Source of Care Among Nonelderly Adults in California, by Insurance Type in Fall 2014
Looking at reason for choosing site of care by coverage, Medi-Cal enrollees were more likely than those in Covered California and other private insurance to report choosing their usual source of care because it was the only place available. Ten percent of Covered California enrollees reported choosing their usual source of care because it was the only place available, compared with 20% of Medi-Cal enrollees and 6% of those with other private insurance. Though Medi-Cal managed care plans are held to state standards of network adequacy and patient access, experts report that low reimbursement rates make contracting with providers difficult, especially in rural areas. There was no change from 2013 to 2014 in the share of Medicaid enrollees who reported they chose their usual source of care because it is the only place available. According to a state Medicaid expert, long-standing federal and state standards of network adequacy have required managed care plans to grow their network to meet demand in the past and will continue to do so as needed.
Uninsured adults and newly insured adults report greater difficulty than previously insured adults in traveling to their regular site of care. Among adults with a usual source of care, most report that it is “very easy” or “somewhat easy” to travel there. However, there was no significant difference in the share of newly insured and uninsured adults who reported ease in traveling to care, while previously insured adults were more likely than uninsured to report ease of traveling to care. Within types of coverage, adults with Covered California and other private coverage were more likely than the uninsured to say it was easy to travel to care. These patterns may reflect the need for the uninsured to find a source of care that is affordable, which may require farther travel. In addition, those with private coverage were also more likely than those with Medi-Cal to report ease of travel to their USC. Taken together, these findings also suggest that the difference may be due to lower provider density in areas where those with the lowest incomes live or the need for lower-income people to rely more heavily on public transit than their own vehicle. There was no change from 2013 to 2014 in the share of uninsured or Medi-Cal enrollees reporting difficulty traveling to their usual source of care.
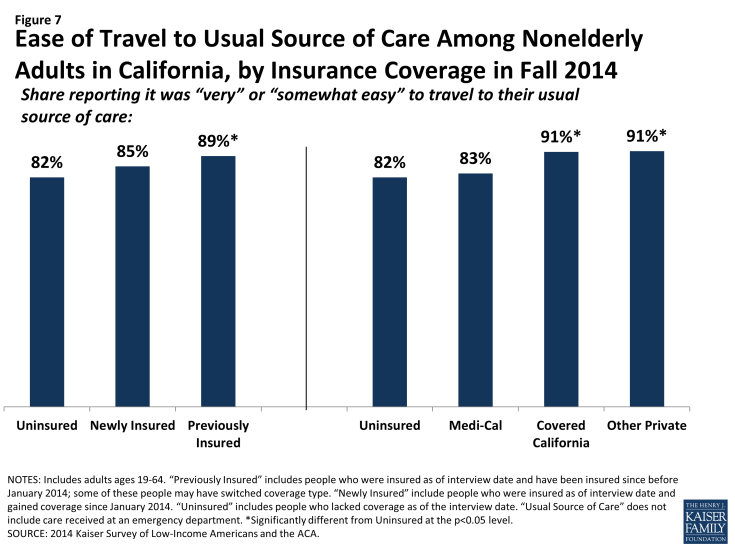
Figure 7: Ease of Travel to Usual Source of Care Among Nonelderly Adults in California, by Insurance Coverage in Fall 2014
Translating Coverage to Care
Mirroring patterns for being linked to care, adults with insurance coverage were more likely than the uninsured to have used medical services or received preventive care. More than half (58%) of adults who gained coverage in 2014 said that they used at least one medical service since gaining their coverage, and nearly half (47%) had received a preventive visit or check-up. These rates were significantly higher than those the uninsured reported for 2014 but were lower than the previously insured reported for 2014. There were no differences in the share of adults reporting visits by coverage type, with the exception of adults with other private coverage being more likely than adults with Medi-Cal to have a preventive visit. Again, these findings are not unexpected given the large body of research showing that people without insurance coverage are less likely to use care, including preventive care. Compared to 2013, Medi-Cal beneficiaries were less likely to report using care but no more or less likely to report using preventive care. Among uninsured adults, there were no changes in utilization rates between 2013 and 2014.
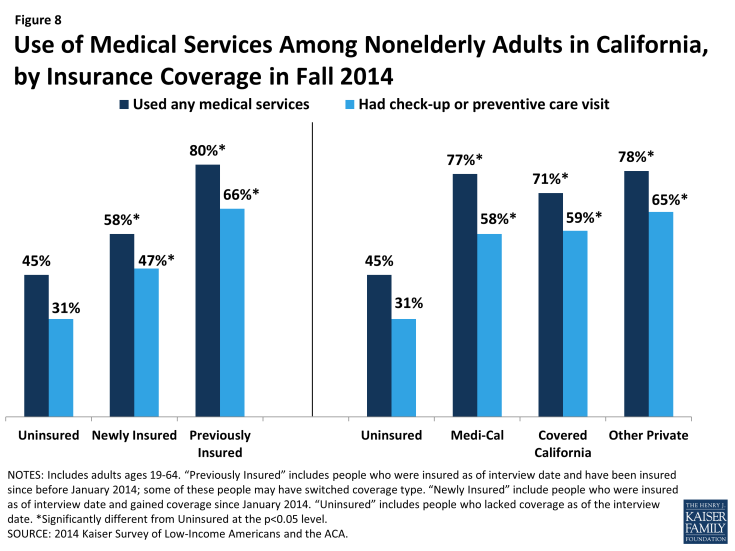
Figure 8: Use of Medical Services Among Nonelderly Adults in California, by Insurance Coverage in Fall 2014
Still reflecting some unmet need, many newly insured adults reported postponing or delaying needed services. More than a third of newly insured adults (35%) reported that they postponed or went without needed care since gaining their coverage, the same share as the uninsured and a higher share than the previously insured. Similar patterns were seen for the shares reporting that they never received this care or that postponing care had negative consequences such as a condition worsening, loss of time at work or school, or substantial stress. When comparing these outcomes by type of coverage, similar patterns persist, though Covered California enrollees were less likely than uninsured adults or adults in Medi-Cal to say that they never received the care they needed or that postponing care led them to miss work or school. Notably, Medi-Cal enrollees were more likely than uninsured adults to report postponing needed care; this outcome may be due to Medi-Cal enrollees’ poorer health status and the greater frequency with which they may need complex services. People with a large number of complex needs may be more likely to encounter access barriers for some services than those with more limited needs. Compared to 2013, Medi-Cal enrollees in 2014 were no more likely to say they postponed care and were less likely to say that their condition worsened or their stress increased as a result of postponing care. The high rates of unmet need among the uninsured corroborate existing evidence that this group goes without needed care due to cost, though the uninsured in 2014 were less likely to postpone care than the uninsured in 2013. Among those who do have coverage, postponing care could be related to several factors, including difficulty finding a provider, problems navigating the health system and health insurance networks, misunderstanding of how to use coverage and when to seek care, or concerns about out-of-pocket costs.
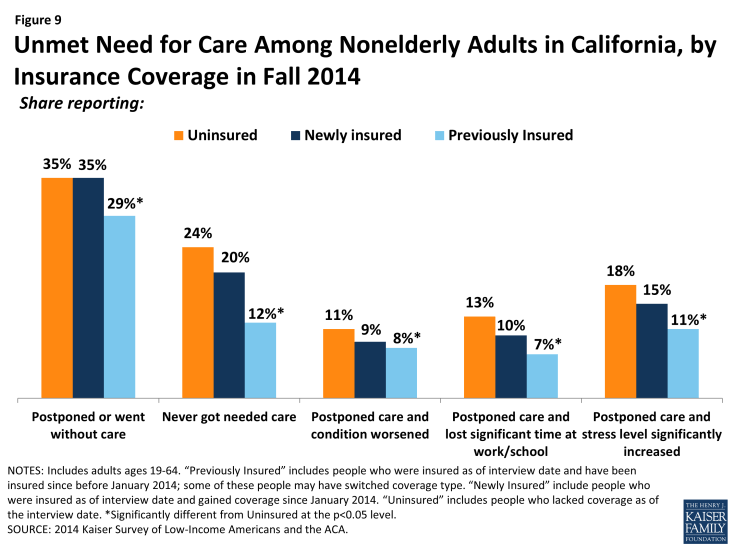
Figure 9: Unmet Need for Care Among Nonelderly Adults in California, by Insurance Coverage in Fall 2014
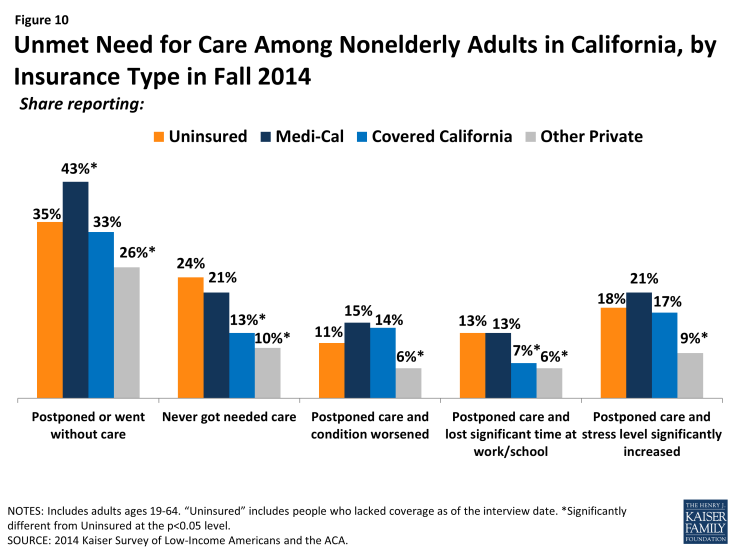
Figure 10: Unmet Need for Care Among Nonelderly Adults in California, by Insurance Type in Fall 2014
Though most adults did not report problems getting appointments, some insured adults say a provider would not take them as a patient due to coverage. Though a very small share (7%) of newly insured or previously insured (4%) adults reported this problem, both these groups were more likely than the uninsured to say a provider would not accept them as a patient due to coverage. The low rates of these problems among the uninsured (2%) likely reflect this group’s lower propensity to seek care, as detailed elsewhere, although uninsured adults in 2014 were more likely than those in 2013 to say they were told a provider would not take them as a patient. There were no significant differences in the share reporting not being taken as a new patient for any reason or reporting having to wait longer than they thought reasonable for an appointment. However, when examined by type of coverage, differences do emerge, with adults in Covered California or Medi-Cal being more likely to report being told that a provider would not take them as a patient than adults with other private coverage. Medi-Cal enrollees in 2014 were no more likely to say a provider would not take them as a patient than those in 2013. Like the forces underlying choice of usual source of care, these issues may reflect continuing problems with network adequacy, despite the existence of state standards for network adequacy and patient access.
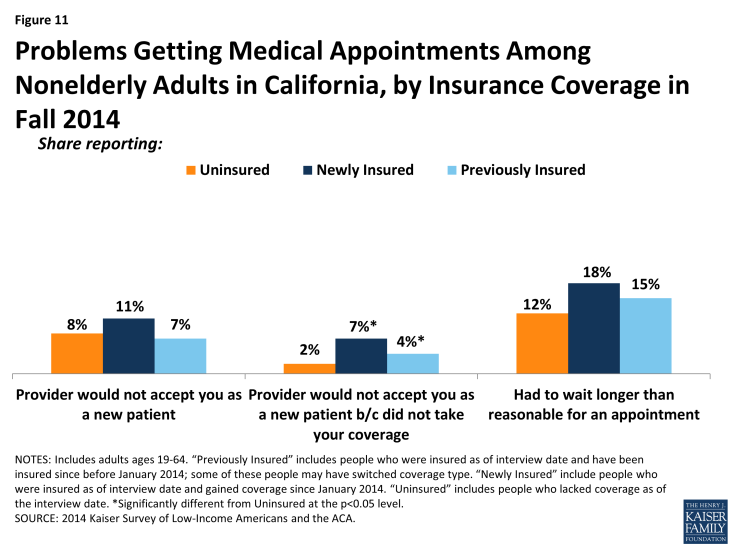
Figure 11: Problems Getting Medical Appointments Among Nonelderly Adults in California, by Insurance Coverage in Fall 2014
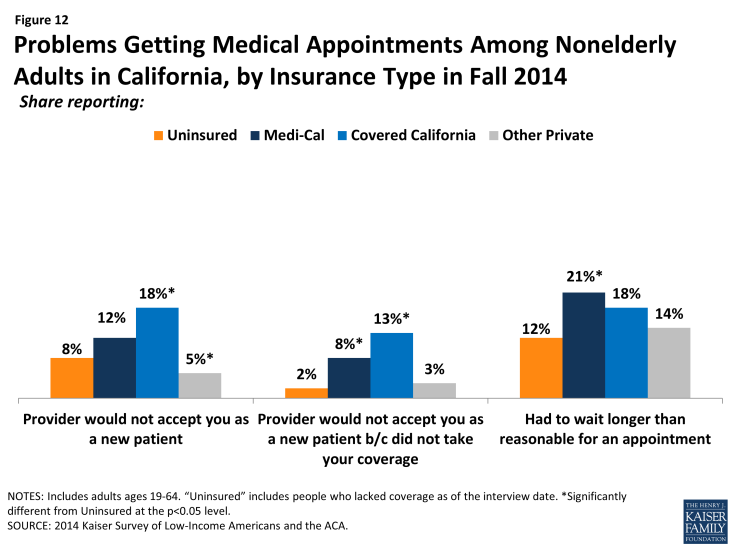
Figure 12: Problems Getting Medical Appointments Among Nonelderly Adults in California, by Insurance Type in Fall 2014
Provider Communication and Health Literacy
Among adults who received care, most adults across coverage types report effective communication with their providers about their care. Once people get into care, health literacy—or “patients’ ability to obtain, process, and understand the basic health information and services they need to make appropriate health decisions”3—plays an important role in how that care affects health outcomes. Health literacy depends on a range of factors related to patients (e.g., engagement in care), providers (e.g., how the information is communicated), service setting (e.g., the length of time of the interaction), and the nature of the visit (e.g., the complexity of health information). Survey results reveal that both previously insured and newly insured both reported understanding their test results or how to take their medication either “always” or “most of the time” that they saw a provider in higher proportions than the uninsured. However, on outcomes of getting all the information you wanted from the provider or feeling encouraged to ask questions, the newly insured were no more likely than the uninsured to report experiencing these always or most of the time. Comparing results by coverage type reveals few differences, though Medi-Cal enrollees were less likely than adults with other private coverage to report getting all the information they wanted or feeling encouraged to ask questions. A statewide analysis of consumer ratings of doctor communication for all health plans found that Medi-Cal managed care plans received a “poor” rating relative to national benchmarks and thresholds, but ratings varied greatly across plans.4 This pattern may stem from income differences between the groups, since low-income Californians are less likely than higher-income Californians to give high ratings of communication with their provider, patient satisfaction, or patient engagement.5 Gaps in patient-satisfaction and engagement stem from low-income Californians reporting lower rates of feeling connected to the health care system or to seeing the same provider over time.6
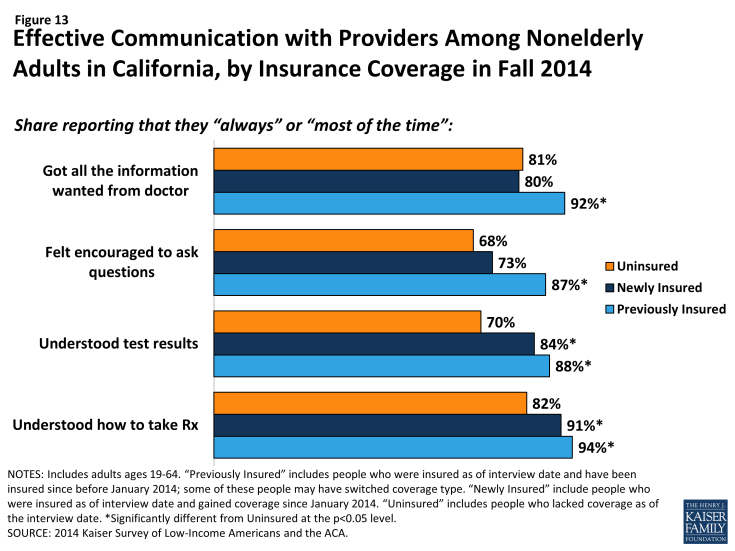
Figure 13: Effective Communication with Providers Among Nonelderly Adults in California, by Insurance Coverage in Fall 2014
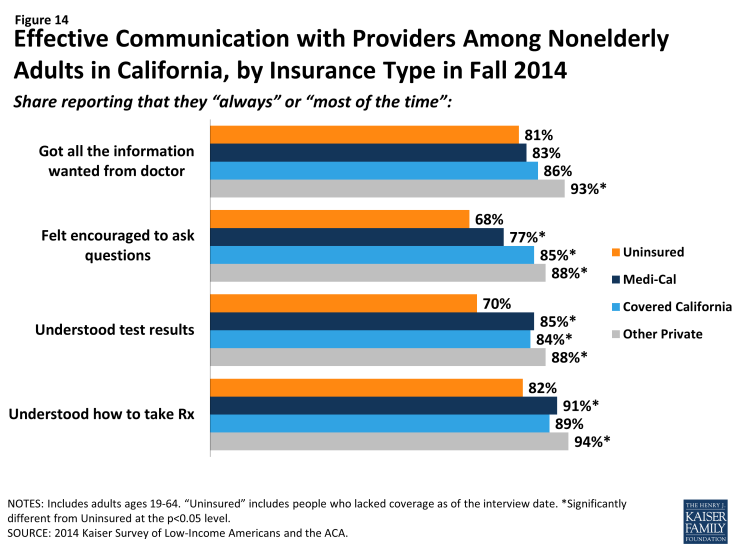
Figure 14: Effective Communication with Providers Among Nonelderly Adults in California, by Insurance Type in Fall 2014
Policy Implications
Clinics and health centers remain core providers for the uninsured and will require ongoing support to serve this population. Though uninsured adults are less likely than insured to have a usual source of care, those that do are most likely to name a clinic or health center (versus doctor’s office, HMO, or other location). Many clinics offer services at greatly reduced cost or on a sliding scale relative to income, which makes them affordable options for the uninsured. Indeed, most uninsured adults said they chose their site of care based on affordability. California safety net providers are likely to play an ongoing, core role in serving the uninsured. However, experts note that these providers are also adapting to meet the changing health care environment in California, including becoming “providers of choice” to retain patients as they gain coverage and expanding primary care capacity to meet demand.
While some uninsured are able to navigate the system when they need care, most are not and face serious consequences as a result. Some uninsured people report that they receive regular care, preventive services, and can access care when they need to, but these individuals are the exception: survey results repeatedly indicate inferior access to care for people who lack insurance coverage compared to those who have coverage. In addition, the uninsured face negative financial consequences of having to pay out-of-pocket for care. Experts noted that access to care for the uninsured varies by region within the state. Some areas, particularly rural areas, have provider shortages for both insured and uninsured people. In addition, while some counties provide services to undocumented individuals, not all do, and those that do vary greatly in the scope of these services. Some local initiatives aim to address access barriers among the uninsured by providing insurance or insurance-like coverage, rather than just direct services, for low-income uninsured people. For example, Healthy San Francisco and My Health LA (MHLA) provide limited coverage for uninsured residents of San Francisco or LA county, respectively, regardless of immigration status. Programs such as these could increase access to health services for California’s uninsured and underinsured and could serve as models for other localities. Since people will continue to lack coverage under the ACA, planned efforts to deliver services to those who lack coverage when they need them may be necessary.
While gains in coverage have resulted in greater access to care for the newly insured, some newly insured adults still report access barriers. These barriers could be related to several factors, including difficulty finding a provider, problems navigating the health system and health insurance networks, misunderstanding of how to use coverage and when to seek care, or concerns about out-of-pocket costs. In discussing barriers to care among the newly insured, experts in the state frequently mentioned issues related to network adequacy. In Medi-Cal, low reimbursement rates have made it difficult to contract with providers in some cases, and the state is monitoring networks closely. In Covered California, experts noted that some plans established narrow networks to contain costs and added that some provider directories were inaccurate. Advocates in the state have pushed for legislation to address these issues, and in January 2015, the state issued an emergency regulation to address network issues in Covered California.7 In addition, the state is focusing on continuing delivery system transformation in Medi-Cal to provide better coordinated care for people. Under the proposed Section 1115 waiver renewal, the state aims to undertake efforts to integrate behavioral/physical health, increase attention to social determinants of health, redesign systems for ambulatory care, and coordinate care for high-need populations, among other initiatives.8
