FAQs on Mental Health and Substance Use Disorder Coverage in Medicare
In light of the heightened attention to mental health needs and challenges that emerged during the COVID-19 pandemic, policymakers are focusing more attention on strategies to improve access to mental health and substance use disorder (SUD) services generally, and in Medicare specifically. Medicare currently covers mental health and substance use disorder services, including inpatient and outpatient services, and prescription drugs, but patient advocates and others have pushed to strengthen coverage and access to these services. To address concerns about barriers to mental health and substance use disorder care, Congress and the Biden Administration recently adopted changes to Medicare coverage that expand the types of providers that Medicare will reimburse for providing mental health and substance abuse disorder services; relax requirements related to telehealth mental health services; and clarify coverage of partial hospitalization services for mental health treatment.
These FAQs review Medicare coverage of mental health and substance use disorder treatment and cost-sharing requirements, and describe recent policy changes including mental health and substance use disorder provisions in the Consolidated Appropriations Act, 2023, which was enacted on December 29, 2022, and in the 2023 Medicare Physician Fee Schedule Final Rule.
What mental health benefits and substance use disorder benefits does Medicare cover and how much do Medicare beneficiaries pay for these benefits?
Medicare covers a range of mental health and substance use disorder services, both inpatient and outpatient, and Part D plans cover outpatient prescription drugs used to treat these conditions. Medicare Advantage plans are required to cover benefits covered under traditional Medicare and most also cover prescription drugs.
Most of these benefits are subject to cost sharing in both traditional Medicare and Medicare Advantage. Medicare Advantage plans may provide reduced cost sharing compared to traditional Medicare, though most people with traditional Medicare have some kind of supplemental coverage (e.g. Medicaid, employer-sponsored coverage and Medigap) that helps with Medicare cost sharing, though nearly six million people on Medicare do not. Out-of-pocket costs may differ between traditional Medicare and Medicare Advantage plans and vary from one Medicare Advantage plan to another.
Medicare Advantage plans can and do apply cost management tools to mental health and other services, such as prior authorization requirements and limited networks that can restrict beneficiary choice of in-network physicians. (See below section “How are mental health benefits and substance use disorder benefits covered under Medicare Advantage plans?” for more detail.)
Out-of-pocket costs for prescription drugs to treat mental health and other conditions also vary among Part D plans, including stand-alone plans that supplement traditional Medicare and Medicare Advantage plans that cover prescription drugs. Part D plans can also impose cost management tools, such as prior authorization, though they are required to cover all or substantially all drugs in six protected classes, including antidepressants and antipsychotics.
Inpatient Services
Medicare Part A covers inpatient care for beneficiaries who need mental health treatment in either a general hospital or a psychiatric hospital. For inpatient stays in a psychiatric hospital, Medicare coverage is limited to up to 190 days of hospital services in a lifetime.
Beneficiaries who are admitted to a hospital for inpatient mental health treatment are subject to the Medicare Part A deductible of $1,600 per benefit period in 2023. Part A also requires daily copayments for extended inpatient hospital stays. For extended hospital stays, beneficiaries pay a $400 copayment per day (days 61-90) and $800 per day for lifetime reserve days in 2023.
Outpatient Services
Medicare Part B covers one depression screening per year, a one-time “welcome to Medicare” visit, which includes a review of risk factors for depression, and an annual “wellness” visit, where beneficiaries can discuss their mental health status. Part B also covers individual and group psychotherapy with doctors or with certain other licensed professionals, depending on state rules, family counseling if the main purpose is to help with treatment, psychiatric evaluation, medication management, and partial hospitalization.
Partial hospitalization is a more structured program of individualized and multidisciplinary outpatient psychiatric treatments that is more intensive than outpatient treatment in a doctor’s or therapist’s office, and is an alternative to an inpatient stay. As part of the Consolidated Appropriations Act, 2023, beginning January 1, 2024, the definition of partial hospitalization under Medicare will be modified to clarify that it is for individuals who have a need for these services for a minimum of 20 hours per week, which must be confirmed by a physician once a month. Also beginning in 2024, Medicare will cover intensive outpatient services, which are the same as partial hospitalization services but only for beneficiaries who need these services for a minimum of 9 hours per week, which must be confirmed by a physician every other month.
Part B also covers outpatient services related to substance use disorders. These include opioid use disorder treatment services, such as medication, counseling, drug testing, and individual and group therapy. Medicare covers one alcohol misuse screening per year, and for beneficiaries determined to be misusing alcohol, four counseling sessions per year. Medicare also covers up to 8 tobacco cessation counseling sessions in a 12-month period, a change made by the Affordable Care Act.
Medicare also covers some telehealth services, including for mental health and substance use disorder services as well as non-mental health related services, on both a permanent basis and on a temporary basis as part of the COVID-19 public health emergency. Medicare Advantage plans also have additional flexibilities for providing telehealth benefits (See below sections “How has expanded telehealth coverage affected access to mental health benefits and substance use disorder benefits during the COVID-19 pandemic?”, “What Medicare-covered telehealth mental health and substance use disorder benefits have been extended beyond the public health emergency?” and “How are mental health benefits and substance use disorder benefits covered under Medicare Advantage plans?” for more detail).
For most outpatient services covered under Part B, a deductible of $226 deductible in 2023 applies, and 20 percent coinsurance that applies to most services, including physician visits. However, some specific Part B services have different cost-sharing amounts that depend in part on whether the provider accepts “assignment” (Table 1). Accepting assignment on all Medicare claims for all of a provider’s Medicare patients means that a provider agrees to accept Medicare’s fee schedule amounts as payment-in-full for all Medicare-covered services.
Prescription Drugs
The Medicare Part D program provides an outpatient prescription drug benefit to people on Medicare who enroll in private plans, including stand-alone prescription drug plans (PDPs) or Medicare Advantage prescription drug plans (MA-PDs). Medicare Part D prescription drug plans cover retail prescription drugs related to mental health and are required to cover all or substantially all antidepressants, antipsychotics, and anticonvulsants (such as benzodiazepines), as each is one of the six protected classes of drugs in Part D.
Part D plans are permitted to impose prior authorization and step therapy requirements for beneficiaries initiating therapy (i.e., new starts) for each of these protected drug classes. Coverage of other prescription drugs is based on an individual plan’s formulary, and depending on a plan’s formulary, beneficiaries can also be subject to prior authorization, step therapy, and quantity limits.
Medicare beneficiaries with Part D coverage face cost-sharing amounts for covered drugs and may pay an annual deductible ($505 in 2023) and a monthly premium. For example, most Part D enrollees pay less than $10 for generic drugs, but many pay $40-$100 (or coinsurance of 40%-50%) for brand-name drugs. Beneficiaries with low incomes and modest assets are eligible for assistance with Part D plan premiums and cost sharing. A majority of beneficiaries receiving the Part D low-income subsidy qualify for full benefits and pay no Part D premium or deductible and modest copayments of $1.45 for generic drugs and $4.30 for brand-name drugs in 2023.
Medicare also covers a more limited set of prescription drugs for mental health and substance use disorders under Part B, which are typically administered in outpatient settings such as physicians’ offices and hospital outpatient departments. These drugs are also subject to the Part B deductible and 20% cost sharing.
Which health providers can bill Medicare directly for mental health and substance use disorder services, and how much does Medicare pay for these services?
Medicare provides coverage and reimbursement for mental health services provided by psychiatrists or other doctors, clinical psychologists, clinical social workers, clinical nurse specialists, nurse practitioners, and physician assistants.
Additionally, beginning in 2023, Medicare allows licensed professional counselors, licensed marriage and family therapists, and other practitioners to provide mental health or substance use disorder services under the general supervision of the billing physician or non-physician practitioner, rather than under their direct supervision due to a change made in the 2023 Medicare Physician Fee Schedule Final Rule. (Prior to 2023, Medicare did not provide reimbursement for mental health services provided by licensed professional counselors and licensed marriage and family therapists, unless the service was provided under the direct supervision of a billing physician). In practice, this means that auxiliary staff such as licensed professional counselors and licensed marriage and family therapists do not need the continuous, direct physical presence of supervising physicians or non-physician practitioners to furnish these services and get reimbursement from Medicare.
Further, in changes adopted as part of the Consolidated Appropriations Act, 2023, beginning January 1, 2024, Medicare will directly reimburse marriage and family therapists as well as mental health counselors, such as certified or licensed clinical professional counselors, or professional counselors, for the provision of mental health services. (These types of providers are not currently allowed to bill Medicare to provide these services.)
Medicare fees vary by type of provider, according to the Medicare Physician Fee Schedule (Table 2).
Are psychiatrists accessible to Medicare beneficiaries?
The majority of physicians, both primary care and specialists, report taking new Medicare patients, similar to the share who take new privately insured patients. Psychiatrists, however, are less likely than other specialists to take new patients, whether covered by Medicare or private insurance. According to a KFF analysis, 60% of psychiatrists are accepting new Medicare patients, which is 21 percentage points lower than the share of physicians in general/family practice accepting new patients (81%).
In addition, psychiatrists are more likely than other specialists to “opt out” of Medicare altogether. Providers who opt out of Medicare do not participate in the Medicare program and instead enter into private contracts with their Medicare patients, allowing them to bill their Medicare patients any amount they determine is appropriate. Overall, 1% of all non-pediatric physicians have formally opted-out of the Medicare program, with opt-out rates highest among psychiatrists: 7.5% of psychiatrists opted out in 2022. Psychiatrists account for 42% of the 10,105 physicians opting out of Medicare in 2022.
The relatively high rate of psychiatrists not taking new Medicare patients, combined with relatively high opt out rates, could pose access issues for Medicare beneficiaries who need mental health services. The extent to which access problems may exist, including for other mental health provider types, is unknown. (For additional information on access to providers in Medicare Advantage plans, see “Provider Networks” in the section below: “How are mental health benefits and substance use disorder benefits covered under Medicare Advantage plans?”)
How has expanded telehealth coverage affected access to mental health benefits and substance use disorder benefits during the COVID-19 pandemic?
Prior to the COVID-19 pandemic, Medicare coverage of telehealth services was very limited. Before the COVID-19 public health emergency, telehealth services were generally available only to beneficiaries in rural areas originating from a health care setting, such as a clinic or doctor’s office. One exception, however, was for individuals diagnosed with a substance use disorder for the purposes of treatment of such disorder or co-occurring mental health disorder, where the geographic and originating site (i.e., the health care setting where the beneficiary is located) restrictions were lifted as of July 1, 2019, based on changes included in the SUPPORT Act.
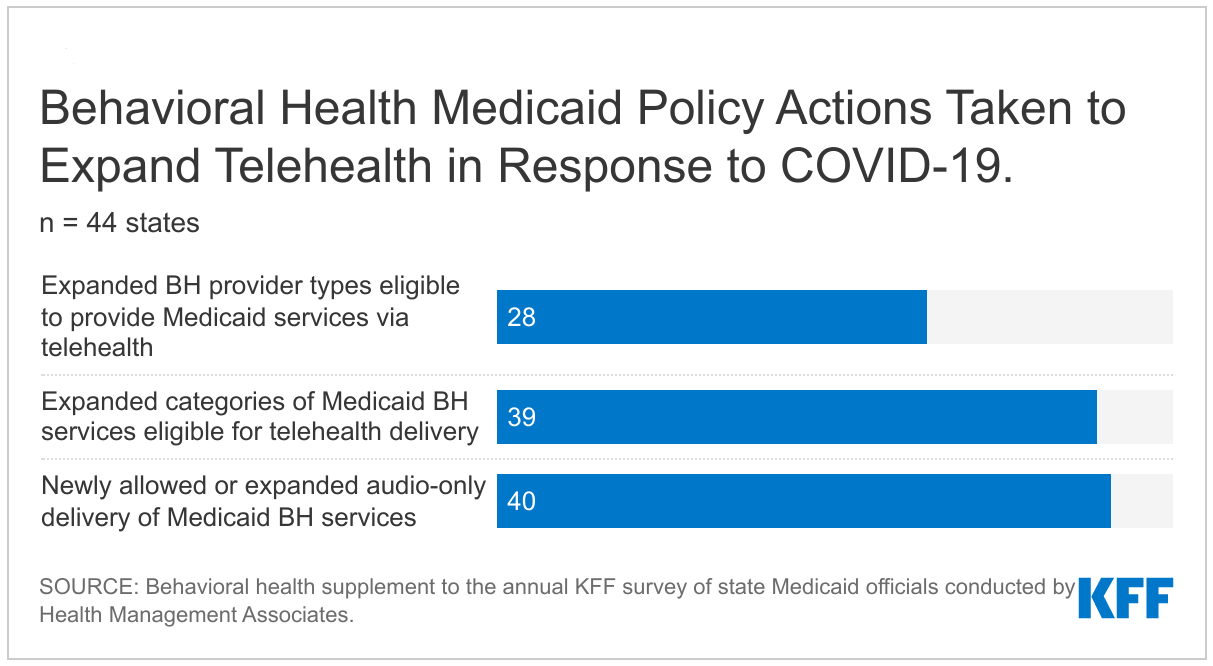
During the COVID-19 public health emergency and extended through December 31, 2024 (based on changes in the Consolidated Appropriations Act, 2023), beneficiaries in any geographic area can receive telehealth services, and can receive these services in their own home, rather than needing to travel to an originating site. During the first year of the pandemic, 28 million Medicare beneficiaries used telehealth services, a substantial increase from the 341,000 who used these services the prior year. Telehealth accounted for 43% of all behavioral health services during the first year of the pandemic, including individual therapy, group therapy, and substance use disorder treatment, but just 13% of all office visits.
Medicare covers telehealth services under Part B, so beneficiaries in traditional Medicare who use these services are subject to the Part B deductible of $226 in 2023 and 20% coinsurance. The HHS Office of Inspector General has provided flexibility for providers to reduce or waive cost sharing for telehealth visits during the COVID-19 public health emergency, although there are no publicly-available data to indicate the extent to which providers may have done so. Some Medicare Advantage plans reduced or waived cost sharing during the public health emergency, though these waivers are likely no longer in effect.
What Medicare-covered telehealth mental health and substance use disorder benefits have been extended beyond the public health emergency?
Medicare has made permanent some changes to telehealth coverage related to mental health services. Based on changes in the Consolidated Appropriations Act, 2021, as implemented under the 2022 Medicare Physician Fee Schedule Final Rule, Medicare has permanently removed geographic restrictions for telehealth mental health services and permanently allows beneficiaries to receive those services at home. Also under the 2022 Physician Fee Schedule final rule, Medicare now permanently covers audio-only visits for mental health and substance use disorder services when the beneficiary is not capable of, or does not consent to, the use of two-way, audio/video technology.
While Medicare does impose some in-person requirements in tandem with coverage of these mental health services through telehealth, these requirements have been delayed as part of the Consolidated Appropriations Act, 2023 until January 1, 2025. Once the requirements take effect, in order for a beneficiary to receive telehealth mental health services, there must be an in-person, non-telehealth service with a physician within six months prior to the initial telehealth service, and an in-person, non-telehealth visit must be furnished at least every 12 months for these services, though exceptions can be made due to beneficiaries’ circumstances. These requirements for periodic in-person visits (in conjunction with telehealth services) apply to treatment of mental health disorders other than treatment of a diagnosed substance use disorder.
How are mental health benefits and substance use disorder benefits covered under Medicare Advantage plans?
Medicare Advantage plans are required to cover all Medicare Part A and Part B services, but cost-sharing requirements for beneficiaries enrolled in Medicare Advantage vary across plans. Medicare Advantage plans can require provider referrals and impose prior authorization for Part A and B services, including mental health and substance use disorder services. Medicare Advantage plans typically have networks of providers, which can restrict beneficiary choice of in-network physicians and other providers, although plans must meet network adequacy requirements for the number of providers and facilities that are available to beneficiaries. Medicare Advantage plans also have different flexibilities for telehealth benefits than under traditional Medicare.
Cost Sharing for Medicare-Covered Mental Health Benefits
Medicare Advantage plans have the flexibility to modify cost sharing for most Part A and B services, subject to some limitations. For example, Medicare Advantage plans often charge daily copayments for inpatient hospital stays starting on day 1, in contrast to traditional Medicare, where there is a deductible and no copayments until day 60 of a hospital stay. Medicare Advantage enrollees can be expected to face varying costs for a hospital stay depending on the length of stay and their plan’s cost-sharing requirements.
Prior Authorization and Referrals
Medicare Advantage plans can require referrals and prior authorization for Part A and B services, including mental health and substance use disorder services. In 2022, virtually all enrollees (99%) are in plans that require prior authorization for some services, including for inpatient stays in a psychiatric hospital (94%), partial hospitalization (92%), opioid treatment program services (85%), mental health specialty services (therapy with other mental health providers besides psychiatrists; 85%), psychiatric services (therapy with a psychiatrist; 85%), and outpatient substance abuse services (83%) (Figure 1).
To address concerns related to the use of prior authorization in Medicare Advantage, CMS released a proposed rule in December 2022 that would institute an electronic prior authorization process in Medicare Advantage and increase the speed at which Medicare Advantage plans must respond to prior authorization requests, which would apply both to mental health and non-mental health related services.
Another proposed rule issued by CMS in December 2022 would clarify the coverage criteria Medicare Advantage plans can use when making prior authorization determinations, including that they follow traditional Medicare coverage guidelines when making medical necessity determinations, and require that a prior authorization approval remain valid for a full course of treatment, proposals which would apply to both mental health and non-mental health related services.
Provider Networks
Unlike in traditional Medicare, where Medicare beneficiaries can see any provider who accepts Medicare, beneficiaries enrolled in Medicare Advantage plans are limited to receiving care from providers in their network or must pay more to see out-of-network providers (in most cases). To ensure that enrollees have adequate access to providers, Medicare Advantage plans are required to meet network adequacy standards, which include a specified number of physicians and other providers, along with hospitals, within a particular driving time and distance of enrollees.
Currently, Medicare Advantage plans are required to meet network adequacy requirements for two mental health specialty types: psychiatry and inpatient psychiatric facility services. However, prior KFF analysis showed that access to psychiatrists has been more restricted than for any other physician specialty: on average, plans included less than one-quarter (23%) of the psychiatrists in a county, and more than one-third (36%) of the Medicare Advantage plans included less than 10 percent of the psychiatrists in their county. Data are not available on network inclusion of other types of mental health providers, such as clinical psychologists and clinical social workers.
CMS has proposed to add three new provider specialty types or categories to Medicare Advantage network adequacy requirements: (1) clinical psychology, (2) clinical social work, and (3) prescribers of medication for Opioid Use Disorder.
Telehealth
As of 2020, Medicare Advantage plans have been permitted to include costs associated with telehealth benefits (beyond what traditional Medicare covers) in their bids for basic benefits. The above-mentioned geographic and originating site limitations do not apply in Medicare Advantage plans, which have had flexibility to offer additional telehealth benefits outside of the public health emergency, including telehealth visits provided to enrollees in their own homes and services provided to beneficiaries residing outside of rural areas. In 2022, 98% of Medicare Advantage enrollees in individual plans had a telehealth benefit. During the first year of the COVID-19 pandemic, 49% of Medicare Advantage enrollees used telehealth services.
Do mental health and substance use disorder parity laws apply to Medicare?
Prior to 2010, Medicare beneficiaries paid a higher coinsurance rate (50%) for outpatient mental health services than for other outpatient services covered under Part B (20%). The Medicare Improvements for Patients and Providers Act of 2008 (MIPPA) phased in parity for cost sharing for all outpatient services covered under Part B between 2010 and 2014, so that as of 2014, cost sharing for outpatient mental health services is the same as for other Part B services.
Federal parity laws, including the Mental Health Parity Act of 1996 and the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA), do not apply to Medicare, however. The Mental Health Parity Act of 1996 requires parity in annual and aggregate lifetime dollar limits for mental health benefits and medical or surgical benefits in large groups plans, but not in Medicare. The Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA), which expanded on the 1996 law, extends parity to substance use disorder treatments and prevents certain health plans from making mental health and substance use disorder coverage more restrictive than medical or surgical benefits, but also does not apply to Medicare. In 2016, some of these parity rules were applied to Medicaid Managed Care Organizations (MCOs) but not to Medicare benefits that are provided by Medicaid MCOs to beneficiaries dually enrolled in Medicare and Medicaid.
Because MHPAEA does not apply to Medicare, some mental health benefits can be more restricted than other health services. Some stakeholders have asserted that this lack of parity is reflected in the lifetime limit of 190 days on inpatient hospitalizations in psychiatric hospitals, because Medicare does not have any other lifetime limits on comparable inpatient services.
What policy approaches have been proposed related to coverage of mental health benefits and substance use disorder benefits in Medicare?
As part of the President’s FY 2023 budget, the Biden Administration proposed a number of changes to enhance coverage of and access to mental health services, including but not limited to Medicare. These include, for example: applying the Mental Health Parity and Addiction Equity Act to Medicare, requiring Medicare to cover three behavioral health visits without cost sharing, and authorizing licensed professional counselors and marriage and family therapists to bill Medicare directly. As noted above, this last proposal was incorporated in the Consolidated Appropriations Act, 2023 and will go into effect January 1, 2024.
During the 117th Congress, policymakers in the House passed legislation to improve access to mental health services in Medicare by establishing an electronic prior authorization process in Medicare Advantage that would have provided real-time decisions on the status of a request, and would have applied both to mental health and non-mental health related services. A similar proposal was included in a CMS December 2022 proposed rule. Some lawmakers have also proposed to remove the 190-day lifetime limit on inpatient psychiatric hospital services under Medicare.
Because many of these proposals would increase access to mental health and substance use disorder treatment, there would likely be an increase in costs to the Medicare program. For example, eliminating the 190-day lifetime limit on psychiatric hospital services is estimated to increase Medicare Part A spending by $3 billion over 10 years, according to CBO. Other changes, such as requiring Medicare to cover three behavioral health visits without cost sharing is estimated to increase Part B spending by $1.4 billion over 10 years.