Medicare Advantage in 2023: Premiums, Out-of-Pocket Limits, Cost Sharing, Supplemental Benefits, Prior Authorization, and Star Ratings
People with Medicare have the option of receiving their Medicare benefits through the traditional Medicare program administered by the federal government or through a private Medicare Advantage plan, such as an HMO or PPO. In Medicare Advantage, the federal government contracts with private insurers to provide Medicare benefits to enrollees. Medicare pays insurers a set amount per enrollee per month, which varies depending on the county in which the plan is located, the health status of the plan’s enrollees, and the plan’s estimated costs of covering Medicare Part A and Part B services. The plans use these payments to pay for Medicare-covered services, and in most cases, also pay for additional benefits and reduced cost sharing. Plans are required to meet federal standards, including providing an out-of-pocket limit. Medicare Advantage plans are also permitted to limit provider networks, and may require prior authorization for certain services, subject to federal requirements.
This brief provides information about Medicare Advantage plans in 2023, including premiums, cost sharing, out-of-pocket limits, supplemental benefits, prior authorization, and star ratings, as well as trends over time. A companion analysis examines trends in Medicare Advantage enrollment.
Key highlights include:
- In 2023, more than 7 in 10 (73%) enrollees in individual Medicare Advantage plans with prescription drug coverage pay no premium other than the Medicare Part B premium, which is a big selling point for beneficiaries.
- Most Medicare Advantage enrollees have access to benefits that are not covered by traditional Medicare, such as vision, hearing and dental. Plans are able to offer extra benefits because they are paid $2,350 per enrollee, on average, above their estimated costs of providing Medicare-covered services (known as “the rebate”). The rebate has increased substantially in the last several years, more than doubling since 2018.
- Nearly all Medicare Advantage enrollees (99%) are in plans that require prior authorization for some services, which is generally not used in traditional Medicare. Medicare Advantage plans also have defined networks of providers, in contrast to traditional Medicare.
- Most Medicare Advantage enrollees are in plans with a quality rating of at least 4 out of 5 stars, explained in part by the fact that more than half (51%) of plans receive ratings at or above this threshold.
In 2023, more than 7 in 10 Medicare Advantage enrollees (73%) are in plans with no supplemental premium (other than the Part B premium)
In 2023, most people (73%) enrolled in individual Medicare Advantage plans with prescription drug coverage (MA-PDs) pay no premium other than the Medicare Part B premium ($164.90 in 2023) (Figure 1). The MA-PD premium includes both the cost of Medicare-covered Part A and Part B benefits and Part D prescription drug coverage. In 2023, 97% of Medicare Advantage enrollees in individual plans open for general enrollment are in plans that offer prescription drug coverage.
Altogether, including those who do not pay a premium, the average enrollment-weighted premium in 2023 is $15 per month, and averages $10 per month for just the Part D portion of covered benefits, substantially lower than the average premium of $40 for stand-alone prescription drug plan (PDP) premiums in 2023. Higher average PDP premiums compared to the MA-PD drug portion of premiums is due in part to the ability of MA-PD sponsors to use rebate dollars from Medicare payments to lower their Part D premiums. When a plan’s estimated costs for Medicare-covered services are below the maximum amount the federal government will pay private plans in an area (known as the benchmark), the plan retains a portion of the difference, known as the “rebate”. According to the Medicare Payment Advisory Commission (MedPAC), rebates average over $2,300 per enrollee in 2023.
For the remaining 27% of beneficiaries who are in plans with a MA-PD premium (5.1 million), the average premium is $57 per month, and averages $38 for the Part D portion of covered benefits – slightly lower than the $40 monthly PDP premium.
Premiums paid by Medicare Advantage enrollees have declined since 2015.
In 2023, the average enrollment weighted MA-PD premium, including among those who do not pay a premium, is $15 per month. However, average MA-PD premiums vary by plan type, ranging from $14 per month for HMOs to $17 per month for local PPOs and $46 per month for regional PPOs. Nearly 6 in 10 Medicare Advantage enrollees are in HMOs (58%), 40% are in local PPOs, and 2% are in regional PPOs in 2023.
Average MA-PD premiums have declined from $36 per month in 2015 to $15 per month in 2023. The reduction is driven in part by the decline in premiums for local PPOs and HMOs, that account for a rising share of enrollment over this time period.
Since 2015, a rising share of plans estimate that their cost of providing Medicare Part A and Part B services (the “bid”) is below the maximum amount that CMS will pay in the area where the plan operates (the “benchmark”). The difference between bids and benchmarks enables plans to offer coverage that typically includes extra benefits without charging an additional premium. As plan bids have declined, the rebate portion of plan payments has increased, and plans are allocating some of those rebate dollars to lower the part D portion of the MA-PD premium. This trend contributes to greater availability of zero-premium plans, which brings down average premiums.
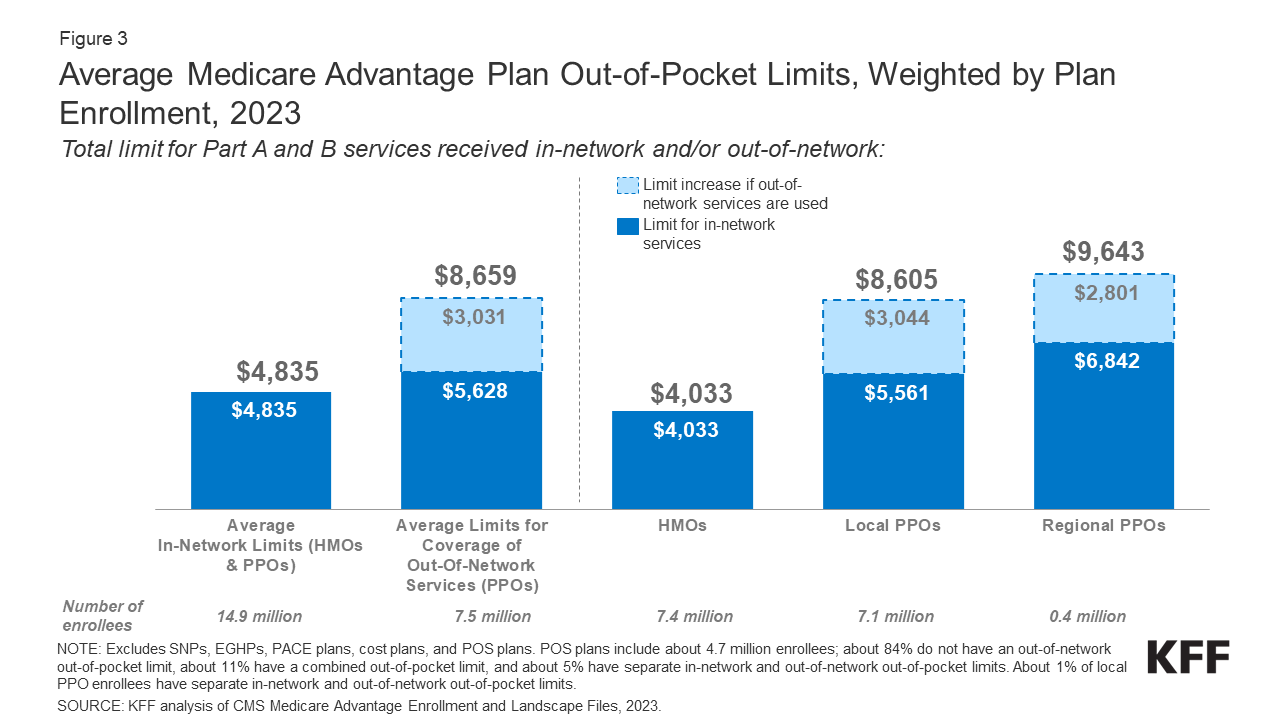
The average out-of-pocket limit for Medicare Advantage enrollees is $4,835 for in-network services and $8,659 for both in-network and out-of-network services (PPOs).
Since 2011, federal regulation has required Medicare Advantage plans to provide an out-of-pocket limit for services covered under Parts A and B. In contrast, traditional Medicare does not have an out-of-pocket limit for covered services.
In 2023, the out-of-pocket limit for Medicare Advantage plans may not exceed $8,300 for in-network services and $12,450 for in-network and out-of-network services combined. These out-of-pocket limits apply to Part A and B services only, and do not apply to Part D spending, for which there is a separate out-of-pocket threshold of $7,400 in 2023, above which enrollees pay 5% of costs. (The 5% coinsurance requirement for Part D enrollees in the catastrophic phase will be eliminated starting in 2024 as part of the Inflation Reduction Act). Whether a plan has only an in-network cap or a cap for in- and out-of-network services depends on the type of plan. HMOs generally only cover services provided by in-network providers, whereas PPOs also cover services delivered by out-of-network providers but charge enrollees higher cost sharing for this care. The size of Medicare Advantage provider networks for physicians and hospitals vary greatly both across counties and across plans in the same county.
In 2023, the weighted average out-of-pocket limit for Medicare Advantage enrollees is $4,835 for in-network services and $8,659 for in-network and out-of-network services combined. For enrollees in HMOs, the average out-of-pocket (in-network) limit is $4,033 (Figure 3). Enrollees in HMOs are generally responsible for 100% of costs incurred for out-of-network care. However, HMO point of sale (POS) plans allow out-of-network care for certain services, though it typically costs more than in-network coverage. For local and regional PPO enrollees, the average out-of-pocket limit for both in-network and out-of-network services is $8,605, and $9,643, respectively.
The average out-of-pocket limit for in-network services has generally trended down from 2017, and the average in-network limit decreased from $5,091 in 2021 to $4,835 in 2023. The average combined in- and out-of-network limit for PPOs decreased from $9,245 in 2022 to $8,659 in 2023.
Most Medicare Advantage enrollees, including enrollees in special needs plans, have access to some benefits not covered by traditional Medicare in 2023
Virtually all enrollees in individual Medicare Advantage plans (those generally available to Medicare beneficiaries) are in plans that provide access to eye exams and/or glasses (more than 99%), hearing exams and/or aids (99%), a fitness benefit (99%), telehealth services (98%), and dental care (98%) (Figure 4). Similarly, most enrollees in SNPs are in plans that provide access to these benefits. However, benefits such as Part B drug rebate are less common for enrollees in both individual plans (10%) and SNPs (7%). This analysis excludes employer-group health plans because employer plans do not submit bids, and available data on supplemental benefits may not be reflective of what employer plans actually offer.
Though these benefits are widely available, the scope of specific services varies. For example, a dental benefit may include preventive services only, such as cleanings or x-rays, or more comprehensive coverage, such as crowns or dentures. Plans also vary in terms of cost sharing for various services and limits on the number of services covered per year, many impose an annual dollar cap on the amount the plan will pay toward covered service, and some have networks of dental providers beneficiaries must choose from.
Enrollees in SNPs have greater access than other Medicare Advantage enrollees to transportation (91% vs 44%), meal benefits (86% vs 78%), bathroom safety devices (15% vs 10%), and in-home support services (31% vs 17%).
Compared to 2022, similar shares of enrollees in individual plans are in plans that offer eye exams and/or eyeglass, hearing exams and/or aids, fitness, telehealth, and dental care benefits. Somewhat larger shares are in plans in 2023 than 2022 that offer over-the-counter drug benefits (84% in 2022 vs 90% in 2023), meal benefits (71% in 2022 vs 78% in 2023), transportation (39% in 2022 versus 44% in 2023), and in-home support services (12% in 2022 vs 17% in 2023). The shares of enrollees in SNPs that offer coverage of dental services (96% in 2022 vs 88% in 2023) and over-the-counter benefits (96% in 2022 vs 84% in 2023) have decreased, while the share in plans that offer coverage of in-home support services (20% in 2022 vs 31% in 2023) has increased.
As of 2020, Medicare Advantage plans have been allowed to include telehealth benefits as part of the basic Medicare Part A and B benefit package – beyond what was allowed under traditional Medicare prior to the public health emergency. These benefits are considered “telehealth” in the figure above, even though their cost may not be covered by either rebates or supplemental premiums. Medicare Advantage plans may also offer supplemental telehealth benefits via remote access technologies and/or telemonitoring services, which can be used for those services that do not meet the requirements for coverage under traditional Medicare or the requirements for additional telehealth benefits (such as the requirement of being covered by Medicare Part B when provided in-person). The majority of enrollees in both individual plans and SNPs have access to remote access technologies (73% and 82%, respectively), similar to the shares in 2022, but just 4% of enrollees in individual plans and 2% of enrollees in SNPs have access to telemonitoring services.
Enrollees in SNPs are more likely to be in plans that offer Special Supplemental Benefits for the Chronically Ill (SSBCI) than other Medicare Advantage enrollees.
Beginning in 2020, Medicare Advantage plans have also been able to offer extra benefits that are not primarily health related for chronically ill beneficiaries, known as Special Supplemental Benefits for the Chronically Ill (SSBCI). The majority of individual and SNP Medicare Advantage enrollees are in plans that do not yet offer these benefits. Fewer than half of all SNP enrollees are in plans that offer some SSBCI. The share of Medicare Advantage enrollees who have access to SSBCI benefits is highest for food and produce (15.8% for individual plans and 41.4% for SNPs), general supports for living (e.g., housing, utilities) (11.7% in individual plans and 29.2% for SNPs), transportation for non-medical needs (10.7% for individual plans and 25.7% for SNPs), and social needs benefits (8.3% for individual plans and 16.7% for SNPs) (Figure 5).
Nearly all Medicare Advantage enrollees are in plans that require prior authorization for some services
Medicare Advantage plans can require enrollees to receive prior authorization before a service will be covered, and nearly all Medicare Advantage enrollees (99%) are in plans that require prior authorization for some services in 2023. Prior authorization is most often required for relatively expensive services, such as Part B drugs (99%), skilled nursing facility stays (99%), and inpatient hospital stays (acute: 98%; psychiatric: 93%), and is rarely required for preventive services (7%). Prior authorization is also required for the majority of enrollees for some extra benefits (in plans that offer these benefits), including comprehensive dental services, hearing and eye exams, and transportation. The number of enrollees in plans that require prior authorization for one or more services stayed around the same from 2022 to 2023. In contrast to Medicare Advantage plans, traditional Medicare does not generally require prior authorization for services and does not require step therapy for Part B drugs.
7 in 10 Medicare Advantage enrollees are in plans that have quality ratings of 4 or more stars
For many years, CMS has posted quality ratings of Medicare Advantage plans to provide beneficiaries with additional information about plans offered in their area. All plans are rated on a 1 to 5-star scale, with 1 star representing poor performance, 3 stars representing average performance, and 5 stars representing excellent performance. CMS assigns quality ratings at the contract level, rather than for each individual plan, meaning that each plan covered under the same contract receives the same quality rating; most contracts cover multiple plans. More than half (51%) of Medicare Advantage plans with a Prescription Drug Plan (MA-PDP) earned 4 stars or higher for their 2023 overall rating, with an average rating of 4.15 stars across all contracts.
In 2023, 7 in 10 (71%) Medicare Advantage enrollees are in plans with a rating of 4 or more stars, a decrease from 2022 (86%) (Figure 7). The decrease in the share of enrollees in plans with a rating of 4 or more stars is largely attributable to the expiration of measures in place during the COVID-19 Public Health Emergency. For example, for some measures, in 2022, if the rating on that measure was lower than the prior year, the ratings reverted back to the 2021 value to hold plans harmless. An additional 2 percent of enrollees are in plans that were not rated because they are in a plan that is too new or has too low enrollment to receive a rating. Plans with 4 or more stars and plans without ratings are eligible to receive bonus payments for each enrollee the following plan year. The star ratings displayed in the figure above are what beneficiaries saw when they chose a Medicare plan for 2023 and are different than what is used to determine bonus payments.
In recent years, MedPAC has raised concerns about the star rating system and quality bonus program, including that star ratings are reported at the contract rather than the plan level, and may not be a useful indicator of quality for beneficiaries because they include too many measures. Additionally, others have questioned whether these policies exacerbate racial disparities without leading to improvements to quality.
Discussion
In 2023, as in prior years, the majority of Medicare Advantage enrollees are in plans that do not charge a premium and provide some extra benefits and reduced patient cost-sharing. Virtually all Medicare Advantage enrollees are in plans that impose prior authorization requirements for multiple services. More than 7 in 10 Medicare Advantage enrollees (73%) are in plans that do not charge a premium (other than the Part B premium), with the remaining quarter paying an average premium of about $57 per month. More than 9 in 10 enrollees are in plans that also provide access to a variety of supplemental benefits, such as eye exams, dental and fitness benefits. Plans also vary in in terms of provider networks and prescription drug benefits, which are beyond the scope of this analysis, but are features people may consider as they make their decisions.
Plans are able to offer extra benefits, often at no additional cost to enrollees, because they receive an additional $2,350 per enrollee above their estimated costs of providing Medicare-covered services. This portion of plan payments, also called the rebate, has increased substantially in the last several years, more than doubling since 2018. Rebates have grown because plan bids for their costs to provide Medicare-covered services have declined, while benchmarks (the maximum amount CMS will pay plans) have remained well-above traditional Medicare spending (plans keep a portion of the difference between the benchmark and their bid, ranging from 50% to 70% depending on the plan’s quality score).
While data on Medicare Advantage plan availability and enrollment and plan offerings is robust, the same cannot be said about service utilization (especially for supplemental benefits) and out-of-pocket spending patterns, which allow assessment of how well the program is meeting its goals in terms of value and quality and help Medicare beneficiaries compare coverage options. Additionally, there is no publicly available data on how frequently supplemental benefits are used by enrollees or how much enrollees pay out-of-pocket for these services. As enrollment in Medicare Advantage and federal payments to private plans continue to grow, greater transparency and more robust information will become increasingly relevant for people with Medicare program oversight.
Nancy Ochieng, Jeannie Fuglesten Biniek, Meredith Freed, and Tricia Neuman are with KFF. Anthony Damico is an independent consultant
| Methods |
| This analysis uses data from the Centers for Medicare & Medicaid Services (CMS) Medicare Advantage Enrollment, Benefit and Landscape files for the respective year. Starting in 2022, KFF is using the Medicare Enrollment Dashboard for enrollment data, from March of each year.
In previous years, KFF had used the term Medicare Advantage to refer to Medicare Advantage plans as well as other types of private plans, including cost plans, PACE plans, and HCPPs. However, since 2022, KFF has excluded cost plans, PACE plans, HCPPs in addition to MMPs. We exclude these other plans as some may have different enrollment requirements than Medicare Advantage plans (e.g., may be available to beneficiaries with only Part B coverage) and in some cases, may be paid differently than Medicare Advantage plans. These exclusions are reflected in both current data as well as data displayed trending back to 2010. |