
The independent source for health policy research, polling, and news.
Proposed Work Requirements Could End Federal Medicaid Coverage for 1.7 Million People
Covering All 1.7 Million Would Require $10.3 Billion in Additional State Funds, Although it Would Be Up to States to Decide
A new KFF analysis finds that an estimated 1.7 million Medicaid enrollees could become ineligible for federal Medicaid under proposed work requirements and presents state-by-state projections, based on estimates of coverage loss from the Congressional Budget Office (CBO).
States could continue to provide Medicaid to those enrollees but would not receive federal matching funds for doing so. It is unclear if any states would choose to do that, though CBO estimated over half of enrollees would continue to be covered at the states’ expense. If states did choose to continue coverage for those individuals, states collectively could face $10.3 billion in new costs in 2024.
The work requirements were included in the Republican-backed debt ceiling legislation that passed the House of Representatives on April 26.
Five states would pay nearly half of the estimated $10.3 billion in new costs: California (326,000 enrollees at a cost of $1.6 billion), New York (186,000, $1.1 billion), Illinois (116,000, $692 million), Pennsylvania (83,000, $537 million) and Washington (72,000, $578 million).
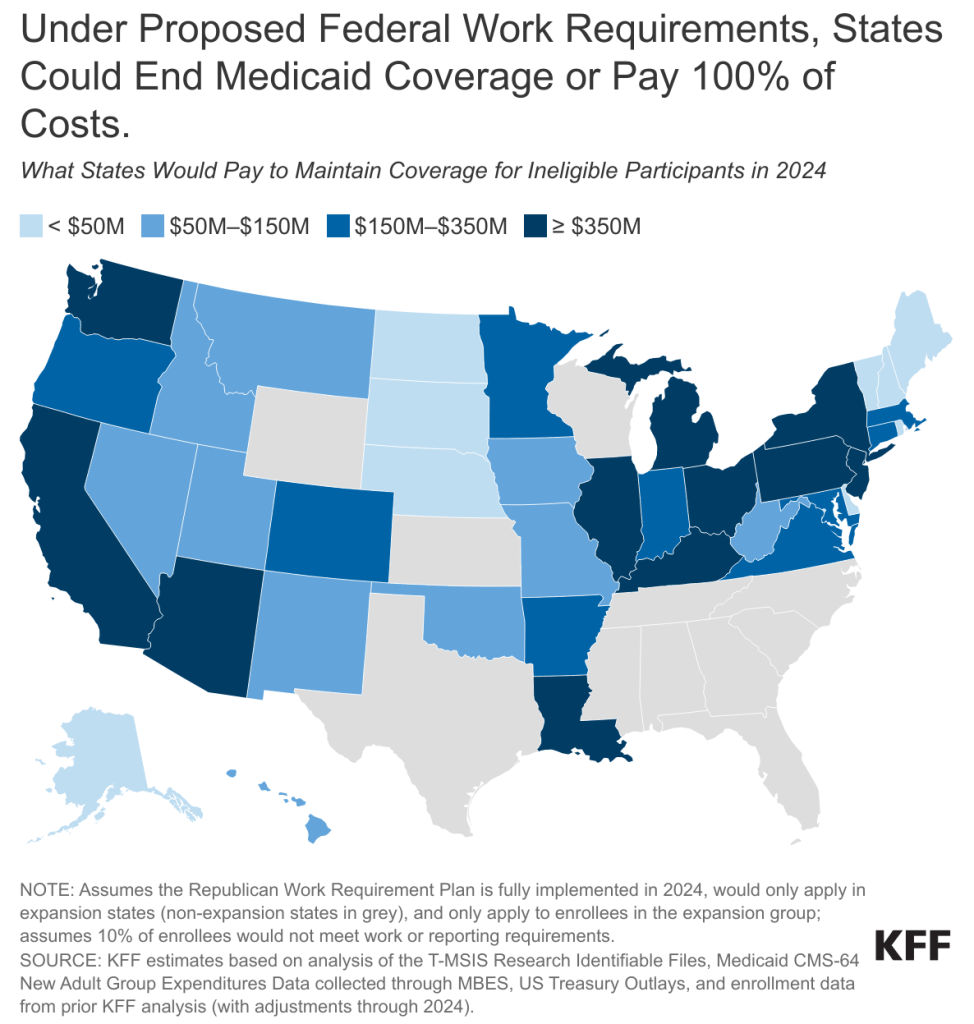
The CBO cost estimate included national estimates of coverage loss and changes in federal spending but did not include state-specific estimates or details about how individual states would respond or why. Our estimates assume a 10 percent rate of Medicaid eligibility loss across all states, based on the national estimate released from the Congressional Budget Office (CBO); this rate could be higher or lower and not uniform across states.
Our analysis, similar to estimates issued by the Department of Health and Human Services, assumes that under the work requirements passed last month by the GOP-controlled House, all enrollees who become ineligible would be in Medicaid expansion states (40 states plus Washington D.C.). The new cost to the states equals 90 percent of total spending for affected enrollees—reflecting the 90 percent of costs that the federal government pays for expansion enrollees who would remain eligible for Medicaid only through state-funded coverage.
If the federal work requirements were applied more broadly across Medicaid eligibility groups, many more people could potentially be subject to reporting requirements, such as parents and people who cannot work due to a disability. Although most of those people likely would qualify for an exemption, some could lose Medicaid eligibility because they are unable to comply with reporting requirements.
While the mandatory work requirements were included in the debt ceiling legislation that passed the House of Representatives, the bill is not expected to pass in the Senate. It is unclear whether work requirements —or similar policies—could end up being debated as negotiations over the debt ceiling continue, or as part of broader federal spending and policy debates.