Navigating Recovery: Health Care Financing and Delivery Systems in Puerto Rico and US Virgin Islands
Hurricane Maria hit on September 20th, less than two weeks after Hurricane Irma hit on September 6, 2017, causing significant physical damage to the infrastructure (including health care infrastructure) in Puerto Rico and the US Virgin Islands (USVI). These hurricanes left major challenges for residents and severe economic damage and health consequences in their wakes. The problems wrought by the storms exacerbate pre-existing fiscal and health challenges faced by these territories. One of the major financing issues for the territories is how to respond given the cap on federal Medicaid financing coupled with the end of the additional funding provided through the Affordable Care Act (ACA). This brief identifies key issues and short and long-term options for recovery in Puerto Rico and USVI drawn from research and from a November 30th roundtable discussion held at the Kaiser Family Foundation in Washington, DC with individuals representing a variety of perspectives on Medicaid policy, health insurance and care delivery systems, and disaster recovery. The roundtable discussion was focused on Medicaid’s role in Puerto Rico and USVI and as part of the hurricane recovery efforts.
Key challenges in Puerto Rico and USVI Pre-Hurricanes
The Territory Clause of the U.S. Constitution authorizes Congress to treat territories differently than states under federal laws and programs as long as there is a “rational basis” for the differential treatment. Federal law provides that residents of the territories are generally not required to pay federal tax; however, the territories have special rules regarding Medicaid, Medicare and SSI.1
Fiscal Challenges
Prior to the hurricanes, Puerto Rico and USVI had fiscal challenges. In Puerto Rico, 44% of the population has incomes below poverty and the unemployment rate is 14% (compared to 14% below poverty and 5% unemployment in the US). (Appendix Table 1). In response to the economic crisis in Puerto Rico, Congress passed the Puerto Rico Oversight, Management and Economic Stability Act (PROMESA) in June 2016 to allow Puerto Rico to restructure its debts. PROMESA created the Financial Oversight and Management Board (FOMB) that was required to approve a fiscal plan developed by the governor. Prior to the hurricane there was tension between the governor and the FOMB about the severity and implementation of austerity measures.2,3 Prior to the hurricanes, Congress approved $296 million in additional Medicaid funding for Puerto Rico as part of the Consolidated Appropriation Act of 2017. Before the hurricanes, there was an out flow of working people from Puerto Rico. Population peaked in 2004 at 3.8 million and has decreased annually since then (by 9.2% through 2015).4 In USVI, 22% of the population lives in poverty and the unemployment rate is 13%. Prior to the hurricanes, the local treasury had barely enough cash to keep the government funded for three days and debt had grown so large that Wall Street stopped lending it money.5
Health Challenges
Higher shares of the population in Puerto Rico have fair / poor health or other health conditions compared to other territories and the rest of the United States. Roughly one third of adults report fair or poor health in Puerto Rico (34%) a much higher share compared to the 50 states and DC (18%) and USVI (20%). The population in Puerto Rico has a higher share of heart attack/heart disease, diabetes, depression, disability, low-birthweight infants and a higher infant mortality rate than the US overall (or the USVI). (Appendix Table 1). The HIV death rate in Puerto Rico was nearly four times higher than that of the U.S. overall, and the number of people living with HIV in Puerto Rico in 2014 was estimated at 17,072, one of the highest rates of people living with HIV per 100,000 in the U.S.6 Puerto Rico has also seen outbreaks of mosquito-borne viral diseases over the last several years, including dengue, chikungunya, and Zika. The majority (84%) of all U.S. Zika cases were reported in Puerto Rico.7 Officials declared that the Zika epidemic was over in May 2017 due to declining cases, but with the new conditions, potential for further disease outbreaks exist. Compared to Puerto Rico, fewer adults report fair or poor health, depression and heart attack/ disease in USVI; however, the share of uninsured (30%) in USVI is much higher than in Puerto Rico (7%) and the rest of the United States (12%).
Infrastructure and Workforce Challenges
Prior to the hurricane, Puerto Rico suffered from poor health infrastructure, declining health care workforce and health indicators that lagged behind those in the rest of the United States. In 2015 alone, approximately 500 physicians left leaving the island with less than half the emergency physicians as well as other key specialists compared to the availability of these providers on the rest of the U.S.8 As a result, there are long wait times to access care and individuals are less likely to receive preventive care and screenings. The Health Resources and Services Administration (HRSA) has deemed 72 of Puerto Rico’s 78 municipalities as medically underserved areas.9 Prior to the hurricanes, USVI had two main hospitals—one on St. Croix and the other on St. Thomas built in the 1980s—and affiliated healthcare facilities. Patients with needs that cannot be served are transferred to Puerto Rico, or mainland US (Florida, New York, Atlanta and Washington DC primarily). The Department of Health (DOH) provides services on all three islands including Maternal and Child Health and Special Needs Programs, dental services, HIV/AIDS programs, long and short-term mental health and substance abuse services with funding from CDC and HRSA. Federally qualified health center (FQHC) on St. Thomas and on St. Croix, each provide a large volume of primary care, dental services, and obstetrical care.10 Because USVI consists of three islands, St. Croix, St. Thomas, and St. John) it is difficult to share health care resources and services need to be available on each island.
Health Financing and Medicaid Challenges
Unlike the 50 states and D.C., annual federal funding for Medicaid in the territories is subject to a statutory cap. Once federal funds are exhausted under each territory’s cap, the territory no longer receives federal financial support for its Medicaid program during that fiscal year. The territories receive a match rate that is fixed in statute, unlike the states where the statutory formula is adjusted annually based on a states’ relative per capita income. The ACA increased the traditional match rate from 50% to 55% for the territories (plus 2.2 percentage points for 2014 and 2015).11 The ACA also provided the territories with the expansion state match rate for non-disabled adults without children (87% in 2017).12 As territories, Puerto Rico and USVI do not receive Disproportionate Share Hospital (DSH) payments that are used in other states to provide supplemental payments to hospitals that service a high share of Medicaid and uninsured patients.
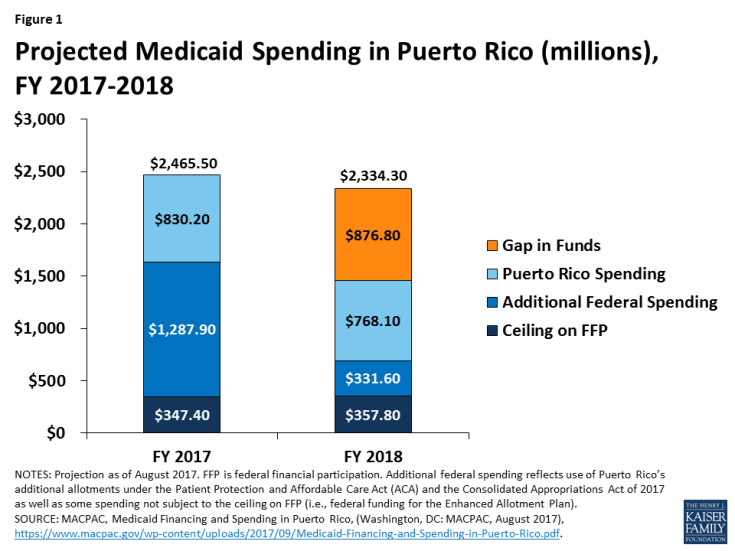
Additional funds totaling $7.3 billion were made available to be divided across all the territories under the ACA. The $7.3 billion consists of a $6.3 billion allotment available between July 2011 and September 2019 and another $1 million for funds in lieu of creating its own Marketplace.13 Of the total $7.3 billion, $6.3 billion was directed to Puerto Rico and about $300 million was directed to the USVI14. In Puerto Rico, ACA funding was the largest source of Medicaid spending (beyond the Medicaid allotment ceiling and spending by Puerto Rico). Based on projections from May 2017 (prior to the hurricanes), Puerto Rico expected to exhaust ACA funding in FY 2018 leaving a $877 million gap in funding (Figure 1).15 So, even before the hurricane, Medicaid financing was in peril. Prior to the hurricanes, estimates showed that as the current rate of spending, it was unlikely that USVI would exhaust ACA related funds before their expiration in September and December 2019.16
Funding for Medicare is limited in the territories, and individuals in the territories are not eligible for SSI benefits. Under federal law, individuals are not automatically enrolled in Medicare Part B. As a result, many fail to enroll, and are subject to a late-enrollment penalty. There are no Medicare Savings Programs (MSP) in the territories that help low-income individuals with some of the out-of-pocket costs for Medicare, so many cannot afford Medicare Part B. Cost-sharing assistance for Medicare enrollees in the territories is limited to individuals dually eligible for full Medicaid and Medicare benefits (not to partial duals in Medicare Savings Programs). In Puerto Rico, nearly all dual eligible are enrolled in Medicare Platino, a Medicare Advantage special needs plan that covers Medicare Part A and B services as well as outpatient prescription drugs. Residents of the territories are not eligible for the low-income subsidies (LIS) to help pay for Medicare Part D (prescription drugs). Instead, federal law provides a fixed amount of funding to each territory to provide Medicaid coverage of prescription drugs for low-income Medicare beneficiaries, provided under Section 1935(e) of the Social Security Act, and called the enhanced allotment program (EAP). Annual EAP funding is estimated to be significantly less than funding that would be received under the LIS.17
In addition, individuals in the territories are not eligible for Supplemental Security Income (SSI) benefits, but receive some aid through a grant (Aid to the Aged, Blind and Disabled, or AABD) program that requires matching funds from Puerto Rico. According to GAO, an estimated 300,000 to 350,000 individuals would receive benefits (compared to 34,000-38,000 under AABD), and the average monthly benefit would be around $540 (compared to $74-$77 under AABD); SSI payments to beneficiaries are estimated to be between $1.5 billion and $1.8 billion per year in federal funding with no local matching fund requirement (compared to the current $24-$26 million under AABD).18
What was the impact of the hurricanes in Puerto Rico & USVI?
Hurricanes Maria and Irma significantly damaged key transportation, communication, and electricity infrastructure in Puerto Rico and USVI that have exacerbated fiscal and health challenges that predated the storms. More than two months after the hurricanes, power, water, and cell service are not available to many in Puerto Rico and USVI. The ongoing power outage in Puerto Rico has been named the “largest blackout in American history”.19 Official estimates show that 64 people died as a result of the hurricane in Puerto Rico, but more recent analysis points to more than 1,000 hurricane related deaths 42 days after the storms.20 The public health challenges are immense in Puerto Rico, as well as USVI, including the potential for the spread of infectious diseases due to unsafe living conditions, difficulties accessing health care services and needed medications, increasing mortality from unaddressed health care needs, and widespread mental health issues. The hurricanes exacerbated the pre-hurricane trends in out migration of working age people and physicians. In testimony to Congress on November 14, 2017, the Governors of Puerto Rico and USVI estimated hurricane damages of up to $95 billion in Puerto Rico and $7.5 billion in USVI.21
Health care infrastructure was badly damaged by the hurricanes. In Puerto Rico, hospitals and other health care infrastructure suffered extensive damage from the storm. In the immediate aftermath of the hurricane Maria, most hospitals were left without electricity and with limited access to generators and the fuel needed to run them. More than two months after the storm, 4 in 10 hospitals and many dialysis centers are still running on generators rather than regular electric power. However, some at the roundtable noted that generators need maintenance and diesel and were not designed to be long-term power substitutes. Given the high burden of diabetes in Puerto Rico, dialysis centers are an important part of the health care system. Community health centers (CHCs) have also been affected by the storm. While nearly all of the 93 health center sites on the island were open as of November 17, almost half (47%) are operating with generators or still do not have power. As a result, some have been forced to limit hours of operation and services. For USVI, Governor Kenneth Mapp testified on November 14, 2017 that Hurricanes Irma and Maria completely devastated critical health care infrastructure, destroying two main hospitals and affiliated healthcare facilities leaving many residents without access to critical care and requiring dialysis patients to be flown to the states for care.22
The hurricanes puts further stress on Medicaid funding limits and has quickened the pace to exhaust available ACA funding. As noted above, before the hurricanes hit, Puerto Rico estimated that the ACA funding would be exhausted in FY 2018 leaving cliffs in federal funding when a greater response is needed. USVI reported that the hurricanes have resulted in an increase in demand for Medicaid as well as for reimbursement from states providing services to displaced Virgin Islands residents.23 The economic damage from the hurricanes has also made it difficult for Puerto Rico and USVI to meet the state matching requirements to draw down federal Medicaid dollars.
Navigating Recovery in Puerto Rico and US Virgin Islands
As policy makers debate legislation and implement strategies to address the short and long-term recovery needs in Puerto Rico and USVI, most of the public (63 percent) say they are closely following news about the recovery effort. An increasing share say that people in Puerto Rico are not yet getting needed help (70 percent up from 62 percent last month) although these views vary considerably by party. On this point, most Republicans (63 percent) feel the federal government is doing enough, while majorities of independents (59 percent) and Democrats (86 percent) feel it is not. In addition, the response to the crisis varies across Puerto Rico with more assistance and progress in urban centers compared to rural areas.
What Help Has Been Provided To Date?
To date, there has been legislative action to provide funding and administrative actions through FEMA and HHS.
Legislative Actions: To date, two aid packages have passed to provide hurricane relief totaling just over $50 million (this funding was for aid beyond Puerto Rico and USVI).24 On November 17, 2017 the White House asked Congress for an additional $44 billion for disaster relief from recent hurricanes, but also called for spending cuts to offset disaster costs.25 Puerto Rico has also requested legislation to address the cliff in Medicaid funding when the ACA related funds are exhausted. The bill passed by the House to reauthorize CHIP included $1 billion Medicaid funding for Puerto Rico and USVI, but has not been acted on in the Senate.
FEMA Actions: The Federal Emergency Management Agency (FEMA) along with federal and local partners, works to help prepare and respond to disasters. In Puerto Rico, following Hurricane Maria, FEMA has primarily been working to gain stability in five critical areas: delivering meals and water to communities in need, restoring power, maintaining a sound medical support structure, and protecting property against further damage from wind and rain.26 The US Army Corps of Engineers is posting daily progress reports measuring costs and personnel on the ground as well as statistics related to temporary roofing, emergency power, debris management, facilities assessment, and additional details about the power grid repair in Puerto Rico.27 On November 27, 2017 FEMA announced that activities in Puerto Rico will begin to transition from the response phase to recovery. These efforts will be led by different agencies across the federal government and will focus on housing, infrastructure systems, economic recovery, health and social services, natural and cultural resources and community planning and capacity building.28
HHS Actions: In October, the HHS Assistant for Preparedness and Response reported that federal partners were working with the Puerto Rico Department of Health and local hospitals to “save lives, stabilize the health care infrastructure, and restore health care services.”29 Activities have included efforts to dispatch medical equipment, supplies and personnel from our National Disaster Medical System and U.S. Public Health Service; in the first 30 days, HHS, along with the Departments of Defense (DoD) and Veterans Affairs (VA) collectively cared for over 8,700 patients in Puerto Rico.30 Federal teams are working with medical volunteers from New York hospitals – under an emergency medical assistance compact that is an agreement between Departments of Health in New York and Puerto Rico.31 In both Puerto Rico and USVI the federal government has activated the Emergency Prescription Assistance Program, which pays for prescription medications for people without health insurance who are affected by disasters.
What are the Limitations of Federal Financing?
Historically, territories have exceeded their allotted Medicaid funding ceilings each year. As noted above, the ACA funding has provided additional federal support for health coverage, but even before the hurricanes Puerto Rico and other territories were anticipating gaps in health spending as these funds are exhausted or expire. The hurricanes have increased demand for Medicaid but also made it difficult for Puerto Rico and USVI to fund their Medicaid matching share.
Financing caps may make it difficult to use Medicaid waivers to assist Puerto Rico and USVI. In other emergencies, the Administration has been able to grant Medicaid waivers to simplify and streamline enrollment processes, expand eligibility for coverage and provide funds for uncompensated care. Such actions were taken following Hurricanes Katrina and Rita, and in responding to the 9/11 crisis in New York and the water crisis in Flint, Michigan. Most recently, Texas received some waivers to provide a six-month extension of eligibility for those enrolled in Medicaid and CHIP in FEMA-declared disaster counties and Texas also waived co-payments for CHIP covered services from August 25 through November 30, 2017, including pharmacy, for CHIP members with a permanent address in one of the Hurricane Harvey FEMA-declared disaster counties.32 However, the block-grant financing structure of Medicaid in Puerto Rico does not allow for similar Medicaid response through waivers in Puerto Rico. So, there are limited ways in which Medicaid can be used through administrative actions to provide short-term assistance.
Other federal funding for DSH, Medicare and SSI is also restricted in the territories. Limited federal funds for hospital DSH payments, Medicare Part B and Part D financing and SSI benefits put further strain on the overall health care system. Addressing these issues could provide additional health care resources beyond changes in Medicaid financing caps and match rates.
Options to Address health care needs: Reflections from the RoundTable
Much of the November 30 roundtable discussion focused on identifying options to address short and longer-term health care needs in Puerto Rico and USVI. However, there was a strong recognition that it would be necessary to both address pre-existing fiscal debt challenges as well as economic damages related to the storms to secure a sustainable economic future in Puerto Rico and USVI. Building a strong health care system with adequate financing was identified as key for economic development on the islands.
- Provide economic and fiscal stability for Puerto Rico and USVI going forward. Short-term financing to address damages related to the storms is critical. However, this short-term funding will not address the underlying fiscal issues tied to the debt-burden that will be needed for longer-term stability. Improving economic stability is important to efforts to stem the flow of out migration and incentivize working people to remain or return to Puerto Rico. Although difficult, participants at the round table underscored the importance of focusing simultaneously on short-term as well as longer term financing relief. Strategies to address economic development are key in addressing long-term financing issues.
- Address Medicaid financing caps and matching requirements. The capped Medicaid financing structure and limit on federal matching funds contributes to broader financing problems in Puerto Rico and USVI and constrains better health care coverage and access. In the near-term, some participants at the roundtable noted that increased Medicaid financing, without a federal matching requirement (similar to emergency relief after Katrina) could provide support to Puerto Rico and USVI, while legislation to change the cap and match rate are longer-term issues. Overall health care funding efforts could also include support for disproportionate share payments, Medicare (Medicare Savings Programs and low-income subsidy funding) as well as funding for SSI.
- Provide support to promote health care delivery system improvements as well as improvements to health capacity (infrastructure and workforce). In the short-term, additional funding can be used to help finance community health centers and other local providers. Some at the roundtable supported changes in emergency response that would automatically trigger increased funding for clinics in disasters. More broadly, access to care and public health measures are lagging in both Puerto Rico and USVI. Changes to financing can help increase resources, but other changes such as a targeted focus on capacity (in terms of infrastructure and health care work force) are interconnected; it is difficult to attract providers without facilities to support their practice. Consideration of new models of care that may rely on electronic health records or tele-health may offer promise to improve health care systems and outcomes is important in plans to build capacity.
- Engage philanthropy and non-profits to work in conjunction with the federal and territory governments to make progress. Those experienced in disaster recovery noted the importance of a local foundation that can bring together governments, private sector, local communities and non-profits to help direct and organize relief and recovery efforts and to marshal funds from many sources. There may be a lot of paperwork to access federal funds. Ultimately, local leader should be working side-by-side with federal and other entities to help direct relief and recovery efforts.
Conclusion
The recent hurricanes brought light to the pre-existing economic and health issues in Puerto Rico and USVI. Fiscal and health challenges have been exacerbated over the years by differential treatment across many federal programs; however, the capped financing and limited federal match rate for Medicaid stand out as key contributors to both the fiscal crisis and a struggling health care system. The hurricanes resulted in widespread damage to the infrastructure (including health care infrastructure) as well as severe economic damage, health consequences and many deaths. Research and input from a roundtable discussion point to a number of options to address the short and longer-term needs of residents in Puerto Rico in USVI. Such options include: funding and support to provide economic and fiscal stability; options to address the Medicaid funding disparities (as well as Medicare and SSI); initiatives to support health capacity through infrastructure and workforce development efforts, and new opportunities to engage philanthropy and non-profits to work with the federal and territory governments to make progress toward recovery and stability.