
The independent source for health policy research, polling, and news.
What You Need to Know About Medicaid Managed Care, Amid the New Federal Rules
New federal rules released last week strengthen managed care access standards, including establishing national maximum wait times for routine primary care, OB/GYN, and behavioral health appointments
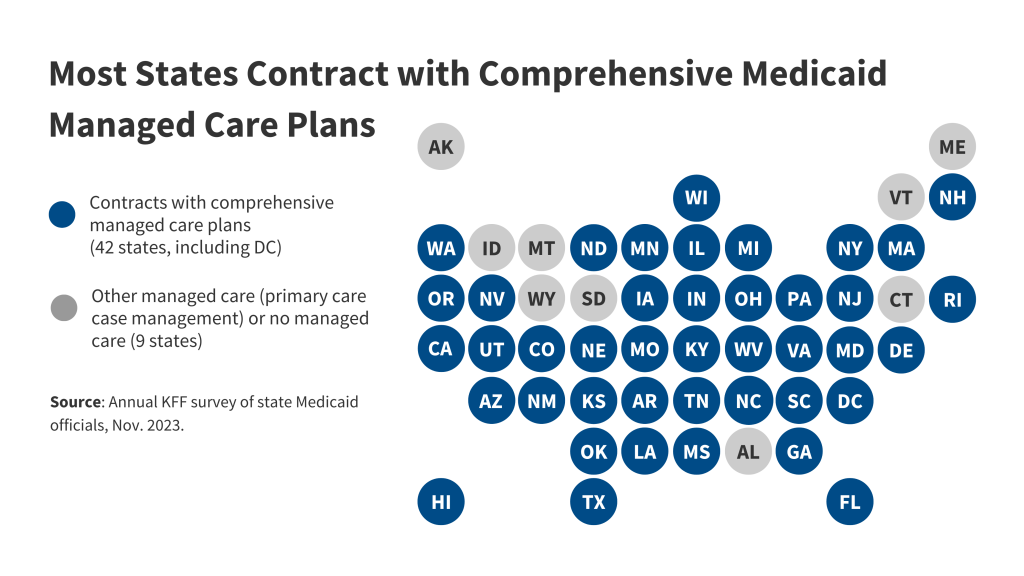
Managed care is the most common delivery system for Medicaid. Most states (42, including DC) use comprehensive managed care plans to provide care to at least some of their Medicaid enrollees, according to KFF’s updated explainer.
Roughly 3 out of 4 Medicaid enrollees receive care through managed care organizations and payments to these organizations account for over half of total Medicaid spending. Five publicly traded firms – Centene, UnitedHealth Group, Anthem (renamed “Elevance” in 2022), Molina, and Aetna/CVS – account for half of managed care enrollment.
Historically, states have had broad flexibility in defining and enforcing network adequacy standards for managed care organizations. Under the new federal rules, states will be required to monitor and enforce key standards for improving access to care.
The effects of these rule changes will be implemented over time and may have significant implications for states, plans and enrollees. Learn more about Medicaid managed care via our updated explainer: 10 Things to Know About Medicaid Managed Care.