
The independent source for health policy research, polling, and news.
Prescriptions to Treat Opioid Overdoses and Opioid Use Disorder Among Medicaid Enrollees Rose Sharply in the Years Leading Up to the Pandemic
Policymakers Are Increasing Access to Such Treatments Amid the Recent Surge in Overdose Deaths
State Medicaid programs saw a doubling of prescriptions for medications used to treat Opioid Use Disorder (OUD) or rapidly reverse opioid overdoses from 2016 to 2019, finds a new KFF analysis.
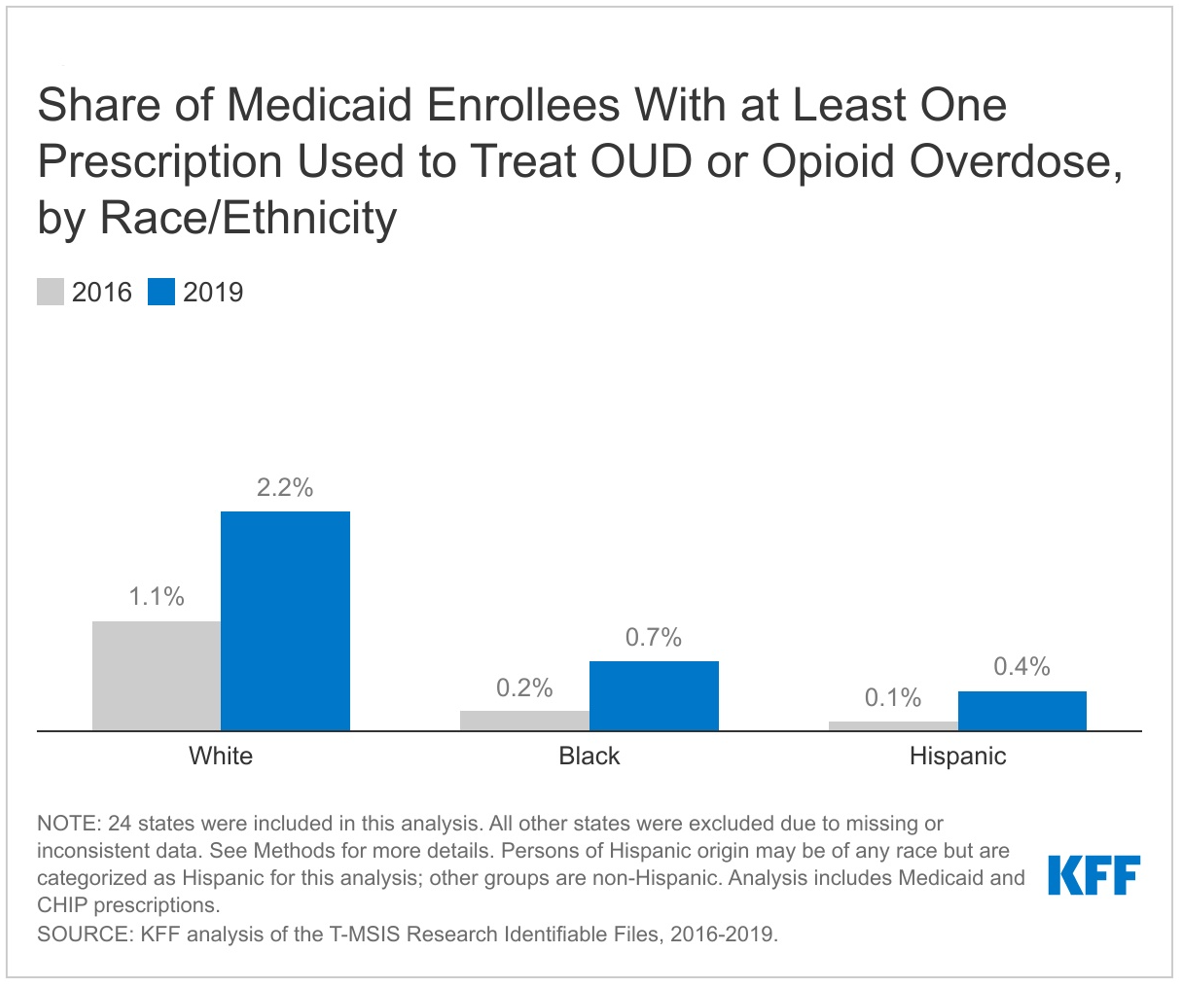
KFF analysts studied the latest available Medicaid claims data — detailed and comprehensive administrative data that can help answer questions and inform policy — and found that the share of enrollees who received at least one medication used to treat OUD or reverse opioid overdose doubled from 0.6 percent to 1.2 percent over the period. In raw numbers, such prescriptions rose from 3.5 million in 2016 to 7.1 million in 2019.
Compared to Black and Hispanic enrollees, White enrollees were more likely to receive at least one treatment prescription and saw the largest percentage point increase over the period, suggesting the presence of racial disparities in access to prescription medication to treat OUD or reverse opioid overdoses.
The prescribing patterns in Medicaid mirror national trends, as policymakers in Washington and in state capitals around the country have implemented policies to increase access to treatment for OUD and reduce overprescribing of opioid prescriptions for pain. A provision in the federal omnibus legislation enacted in December will expand the number of providers who are able to prescribe buprenorphine for treating OUD.
Despite efforts to address the epidemic, deaths due to substance use disorder (SUD) have risen sharply during the pandemic. Opioid overdose death rates increased by 38 percent from 2019 to 2020, with deaths involving illicitly manufactured synthetic opioids like fentanyl now driving the trend. The rise in deaths associated with drug overdose has disproportionately affected people of color.
Medicaid enrollees may be particularly impacted, as 21 percent have mild, moderate, or severe SUD, compared to 16 percent of commercially insured. In its role as a public program and the single largest payer of behavioral health services in the country, Medicaid is particularly well positioned to implement policy to improve the delivery, quality, and effectiveness of behavioral health services.
A second KFF analysis released today finds that 7.3 percent of Medicaid enrollees ages 12 to 64 had at least one clinically-identified SUD in 2019. Other data sources suggest that this may be an undercount because it is a measure of people who receive a diagnosis or prescription code that indicates the presence of a SUD. People with clinically-identified SUD were more likely to be male, White, over 25 years old, and qualify for Medicaid based on a disability or through Medicaid expansion.
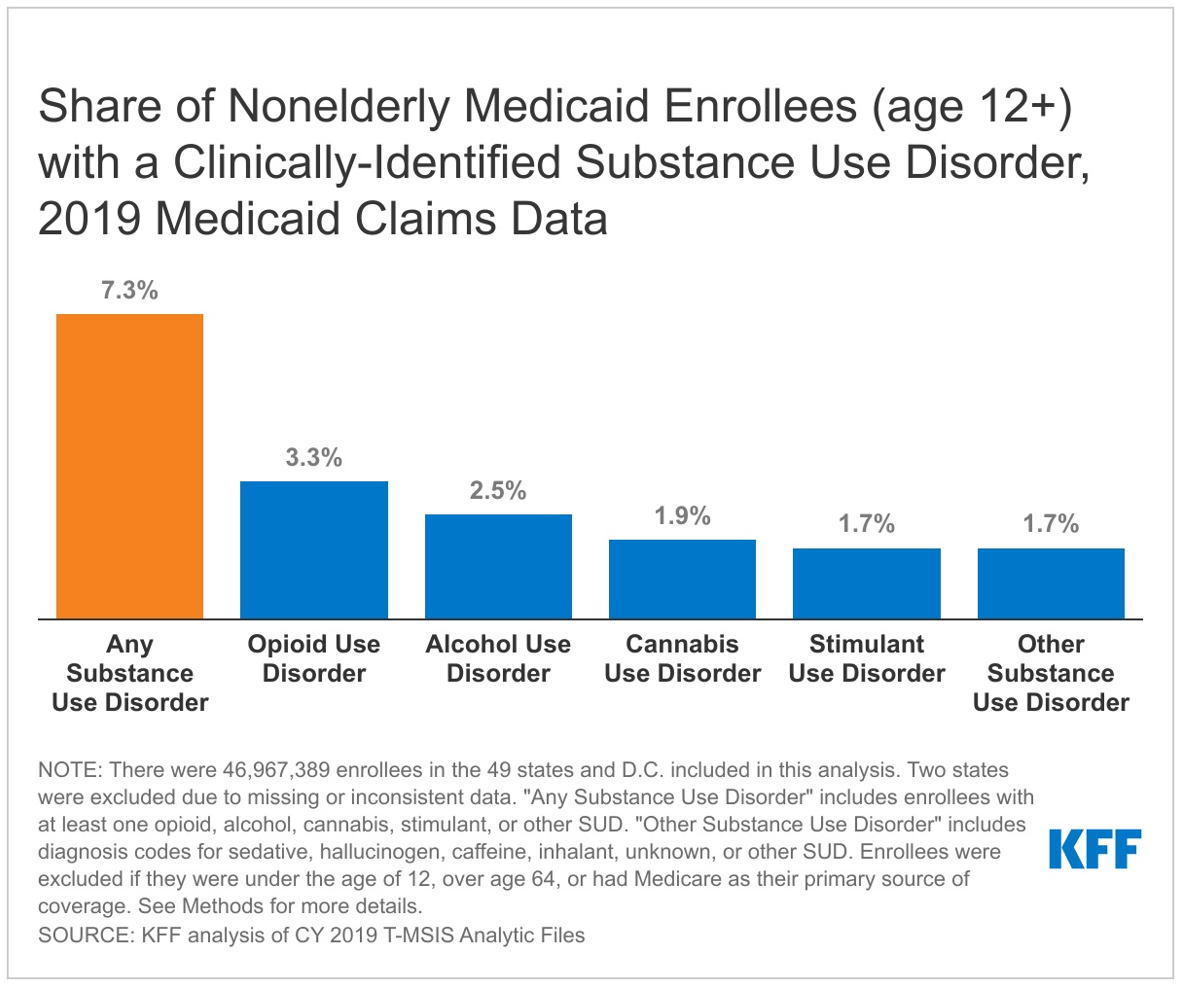
Rates of clinically-identified SUD vary widely across states, not only because of prevalence, but also because of other factors, such as provider screening behavior and variation in Medicaid coverage of SUD services.
Understanding characteristics of Medicaid enrollees with SUD and receiving OUD prescription treatment can help shed light on longstanding gaps in access to care including under-identification and undertreatment of SUD and inform policies to address issues.
For more data and analyses on Medicaid and substance use disorder, visit kff.org