
The independent source for health policy research, polling, and news.
As State Medicaid Programs Prepare to Resume Disenrollments, Many States Are Using a Range of Strategies to Make it Easier for People Who Remain Eligible to Retain Coverage, But in Others it Will be More Difficult
Annual 50-State Survey Looks at Medicaid Eligibility, Enrollment, and Renewal Policies
With pandemic-era protections for Medicaid enrollees set to expire this month, state Medicaid programs are gearing up to resume eligibility checks and disenrollments. But how the unwinding of the federal continuous enrollment provision affects enrollees and state budgets will vary according to states’ differing approaches and administrative capabilities, a new KFF survey finds.
The 21st annual KFF survey of state Medicaid and Children’s Health Insurance (CHIP) Program officials finds that many states are using an array of strategies to promote continuity of coverage, while other states have adopted policies that may make it harder for people who are still eligible to retain coverage. Staffing shortages and systems limitations could also affect whether eligible enrollees are able to remain enrolled.
The survey, conducted by KFF in collaboration with the Georgetown University Center for Children and Families, presents a snapshot of actions that states are taking to prepare for the unwinding of the provision that has paused Medicaid disenrollments since February 2020. It also highlights states’ Medicaid eligibility, enrollment, and renewal policies and procedures in place as of January 2023.
KFF has estimated that enrollment in Medicaid and CHIP will have grown by 23.3 million enrollees, to nearly 95 million, by the end of March when the continuous enrollment provision expires. Millions of beneficiaries are expected to be disenrolled over the next year, including some who are no longer eligible for Medicaid and others who still qualify but lose coverage due to administrative paperwork problems.
In the new survey, the one-third of states that were able to report projected coverage losses estimate that about 18 percent of Medicaid enrollees will be disenrolled after the continuous enrollment provision ends. The estimates range from seven percent to 33 percent of total enrollees and are consistent with other estimates that about 15 million people may lose Medicaid coverage over the coming year.
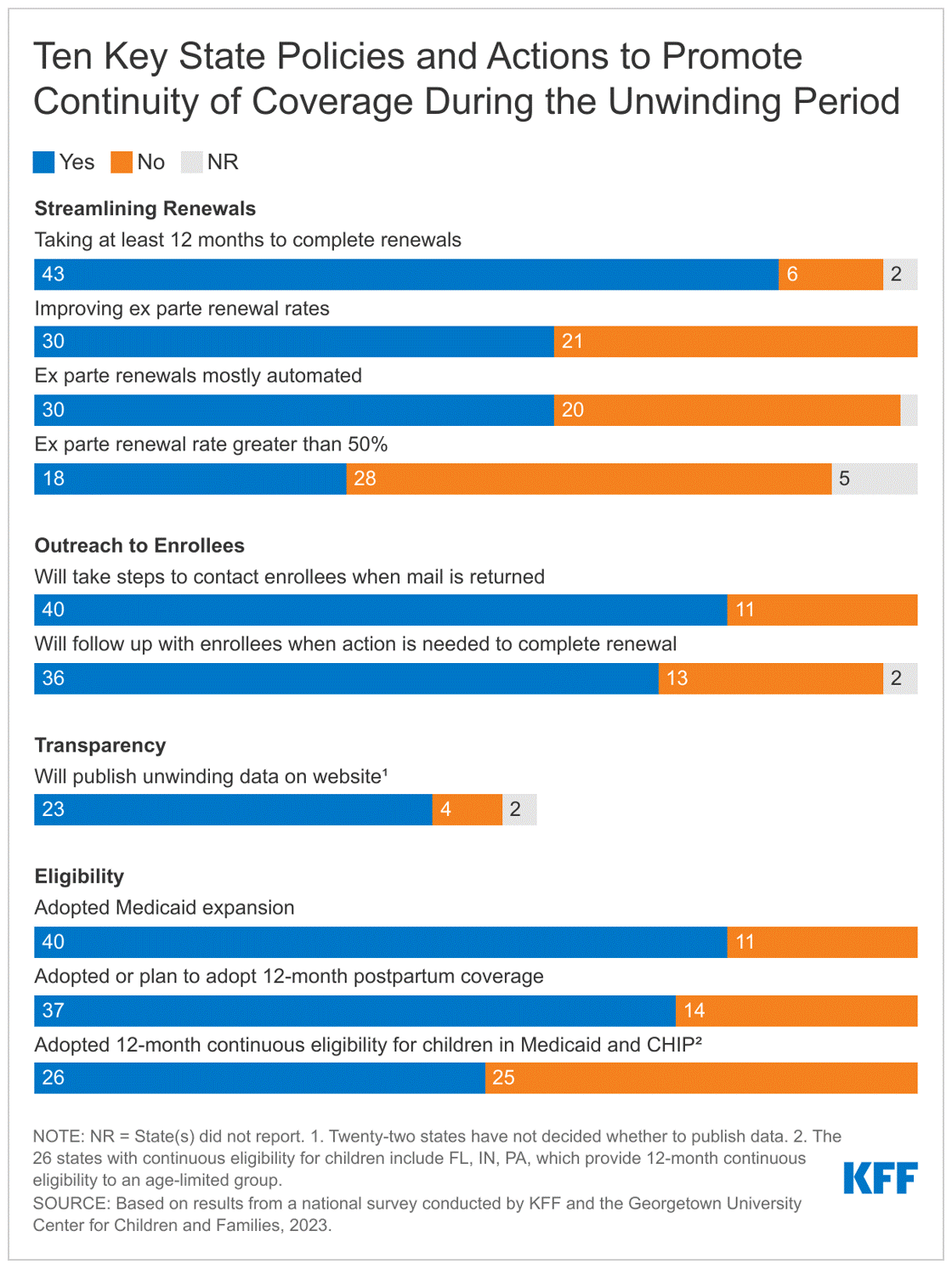
There is variation in the strategies states are adopting that could affect the amount of coverage losses, including:
- Taking 12-14 months to complete renewals following the end of the continuous enrollment provision (43 states). Taking more time can help prevent inappropriate terminations of those who are still eligible but could maintain enrollment of ineligible people for longer.
- Improving rates of renewals using ex parte processes that use reliable data sources — such as the Federal Data Services Hub and Supplemental Nutrition Assistance Program (SNAP) information — to verify ongoing eligibility, reducing the administrative burden on both states and enrollees (30 states).
- Contacting enrollees when renewal action is needed and following up with those who don’t respond (36 states). About half of the states (27) have been flagging individuals who may no longer be eligible or who did not respond to renewal requests.
- Adopting continuous eligibility policies for children, postpartum and for some adults that will help more people retain coverage during the unwinding. A total of 37 states have extended postpartum coverage to 12 months and 26 states provide 12-month continuous eligibility to some or all children in Medicaid and CHIP.
At the same time, some states have not adopted these strategies. Several states lack fully automated systems, processing some or most renewals manually (12 states) and others have ex parte renewal rates below 25 percent (11 states), which will increase the administrative burden on staff and enrollees. Even among states that adopt policies to promote continuity of coverage, implementation of policies and systems capacity will be key in how enrollees fare during the unwinding.
The challenge of processing an unprecedented volume of eligibility renewals and disenrollments comes at a time when most state Medicaid programs face significant staffing challenges. The survey finds that more than half of reporting states have staff vacancy rates greater than 10 percent for eligibility workers (16 of 26 reporting states) and slightly less than half for call center staff (13 of 28 reporting states).
These and other findings from the survey will be discussed today at a public web briefing. An archived video recording of the briefing will be available on kff.org later today.
The full survey report, “Medicaid and CHIP Eligibility and Enrollment Policies as States Prepare for the Unwinding of the Pandemic-Era Continuous Enrollment Provision,” includes state-level data about Medicaid and CHIP eligibility in every state. Also available are other recent KFF analyses related to the end of the continuous enrollment provision, including “Unwinding the Continuous Enrollment Provision: Perspectives from Current Medicaid Enrollees” and “Medicaid Enrollment Growth: Estimates by State and Eligibility Group Show Who may be at Risk as Continuous Enrollment Ends.