For decades, KFF polling has provided insights into national and state-level reproductive health care policy including multiple public opinion polls examining the experiences and attitudes of the general public as well as the group most impacted by such policies – women between the ages of 18 and 49. This latest KFF poll was fielded the week following the leak of a draft of the U.S. Supreme Court opinion on Dobbs v. Jackson Women’s Health Center. If the final ruling in the case resembles the leaked draft, the Court would overturn Roe v. Wade and end the constitutional right to abortion. This analysis examines the public’s attitudes and understanding of the future of reproductive health and abortion access in the U.S. and looks at the role abortion and a decision on Dobbs may play in the upcoming midterm elections this November.
Key Findings:
- Majorities of U.S. adults are aware of the leaked draft of the pending Supreme Court decision, and majorities across gender and partisanship say it is either “very likely” or “somewhat likely” the Supreme Court will be overturning Roe v. Wade this year. With this in mind, nearly two-thirds of adults do not want to see the decision overturned, and a large majority (74%) say abortion should be a personal choice and not something that is regulated by law.
- Among those who live in the 17 states1 where abortion is certain or very likely to be banned if Roe v. Wade is overturned, majorities are aware that getting an abortion would be much harder in their state as a result of such a decision. However, partisans differ on whether this increased difficulty is a good or a bad thing, with Republicans more likely to say it would be a “good thing” that abortion would be harder to access in their state and Democrats more likely to view it as a “bad thing.”
- Looking ahead to the role this decision could play in the anticipated Republican Wave in the midterm elections this November, most voters (57%) say a Supreme Court ruling overturning Roe v. Wade would not make a difference in their motivation to vote in the upcoming midterms and some (6%) say it would make them less motivated to vote. On the other hand, nearly four in ten voters (37%) say such a decision would make them more motivated to vote, including at least half of all Democratic voters (55%) and Democratic voters in states where abortion is likely or certain to be banned if Roe is overturned (51%). Majorities of Republican voters (73%) and Republican women voters (74%) say it would not make a difference in their motivation to vote.
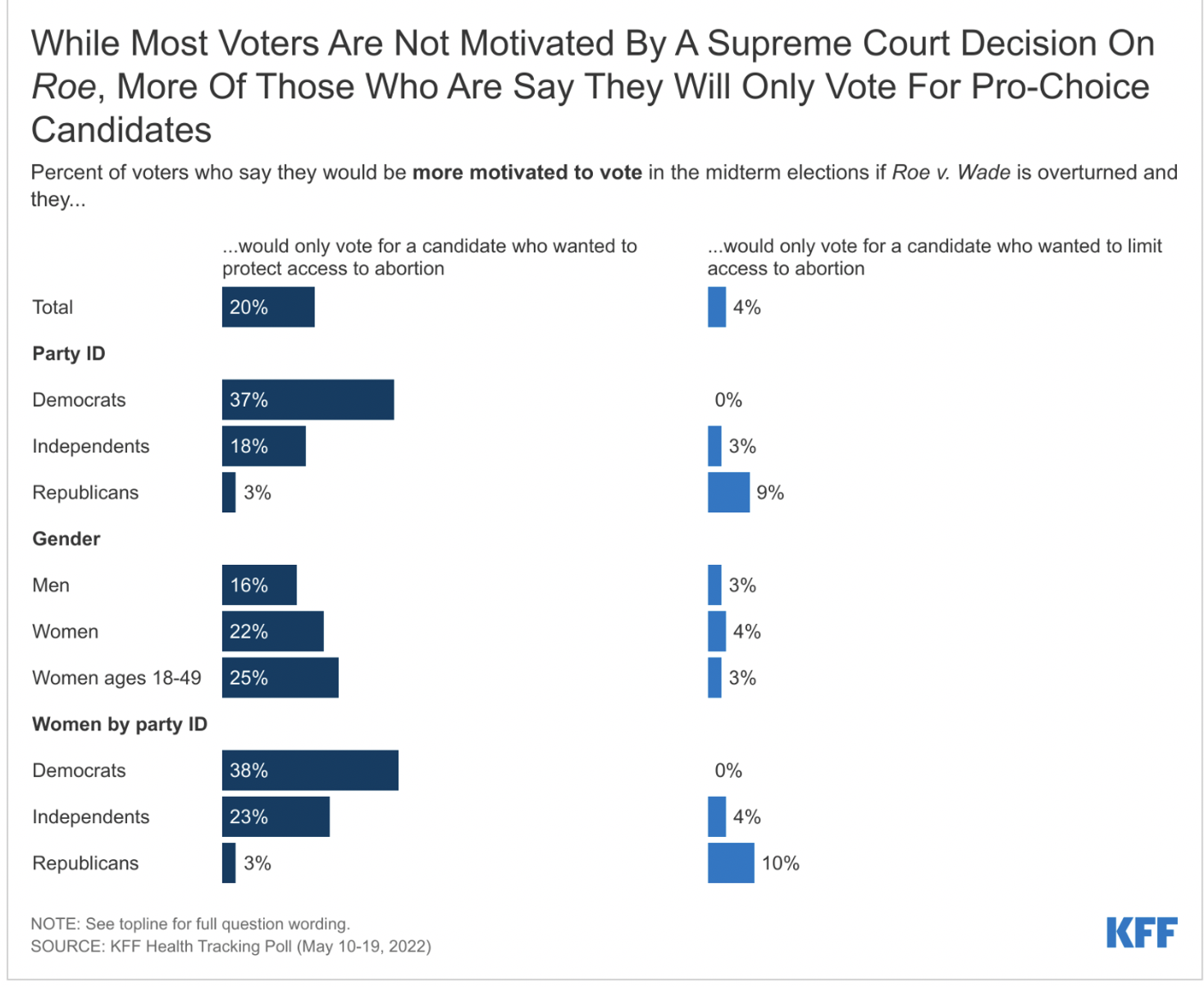
- While a Supreme Court ruling overturning Roe v. Wade doesn’t appear to motivate a majority of voters overall, there is a small share of voters (20%) who say they would be more motivated to vote and that they would only support a candidate who shares their view and wants to protect access to abortion. This includes nearly four in ten Democratic voters, Democratic women voters, and one-fourth of women voters ages 18-49. A smaller share of voters (4%) says they would be more motivated to vote by the Supreme Court decision, but in the opposite direction – to only support candidates who want to limit access to abortions.
- There is an age divide among voters who prefer candidates who want to protect abortion access, that crosses partisanship and gender lines, with voters under age 50, regardless of party identification and gender, more likely to prefer such candidates compared to their older counterparts. For example, while fewer than four in ten male voters ages 50 and over (37%) say they prefer a candidate who wants to protect abortion access, this rises to a majority (56%) of male voters ages 18-49. Most voters who prefer a candidate who wants to protect access to abortion say they would not vote for a candidate who disagreed with them on this issue (63%), compared to half of those who prefer a candidate who wants to limit access to abortion.
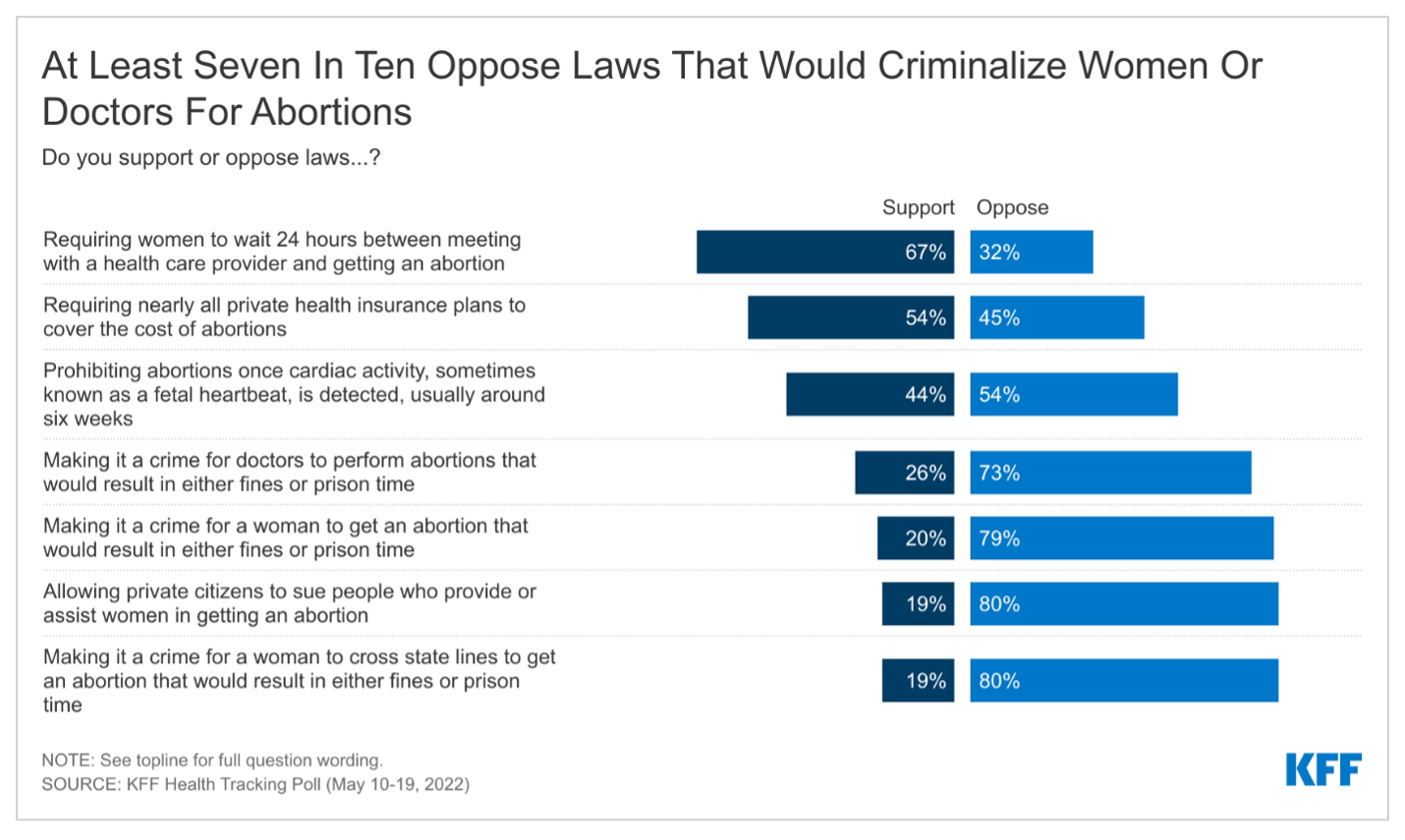
- If the Supreme Court overturns Roe v. Wade, states will set their own abortion policies without any federal constitutional standards. This poll finds there is some support for state restrictions on abortions, such as requiring women to wait 24 hours between a meeting with a health care provider and getting an abortion (67% support). However, majorities oppose other state laws, including at least three-fourths who oppose laws that would make it a crime for women to get an abortion (79%), allowing private citizens to sue people who provide or assist women in getting an abortion (80%), or making it a crime to cross state lines to obtain an abortion (80%).
- This KFF poll also finds that there are significant knowledge gaps on the prevalence and the overall safety of abortions. Additionally, a majority of adults (73%) and of women between ages 18-49 (60%) have not heard of mifepristone or medication abortion, the method in which most abortions occur in the U.S.
The Supreme Court Draft Opinion Leak
On May 2, 2022, Politico published a leaked draft opinion of the U.S. Supreme Court on Dobbs v. Jackson Women’s Health Center that would overturn the precedent set by Roe v. Wade and Planned Parenthood v. Casey, eliminating federal protections to the right to an abortion. The Supreme Court acknowledged the authenticity of the draft but stated, “it does not represent a decision by the Court or the final position of any member on the issues in the case.” If the draft opinion is indicative of the final opinion to be released later this month, the constitutional right to an abortion established by the 1973 case would be overturned and it would be again up to individual states to decide whether to restrict or uphold a right to abortion services. Unlike other cases regarding abortion rights since Roe v. Wade, the Dobbs case comes at a time when the ideological composition of the Supreme Court is conservative by a strong majority 6-3, and the case’s plaintiffs, the state of Mississippi, have asked, the Court to outright overturn Roe v. Wade.
Awareness of the Leaked Supreme Court Opinion Draft
Majorities of the U.S. public, across gender and partisanship, say they have heard at least some about the draft opinion that was leaked to the press, including more than one-third (37%) who say they have heard “a lot” about it. Notably, the group most likely to be impacted by this decision – women of reproductive age (ages 18 to 49)2 – report hearing the least about the leak, with a quarter (23%) saying they have heard “a lot” and nearly half saying they’ve heard “little” (24%) or “none at all” (23%).

There is some confusion among the public about what the leaked draft of the Supreme Court opinion portends for the current and future state of abortion access in the country. The poll, conducted immediately following the leak of the draft opinion, finds that while about two-thirds (64%) are aware Roe v. Wade remains the law of the land, a small share (3%) incorrectly believe it has already been overturned and another third (33%) are unsure. Women are more likely than men to say it has already been overturned or that they are not sure (40% v. 33%). Nearly half of women ages 18-49 either say it has already been overturned (6%) or they are not sure (40%).

Two-thirds of adults say it is either “very likely” (22%) or “somewhat likely” (42%) that the Supreme Court will overturn Roe this year. While few (6%) women ages 18-49 incorrectly believe Roe v. Wade has already been overturned, most say that it is “very likely” (12%) or “somewhat likely” (45%) that Roe will be overturned. About one-third (35%) of women ages 18-49 do not think this is likely to happen this year.
Supreme Court and Motivation in the Midterm Elections
If Roe v. Wade is overturned by the U.S. Supreme Court and the decision on abortion legislation is left to the states, the latest KFF polling finds a candidates’ positions on abortion could be a salient issue for a certain segment of Democratic-leaning voters but only motivates a small share of voters.
While a majority of voters (57%) say the Supreme Court overturning Roe v. Wade would not make a difference in their motivation to vote in the upcoming midterm and some (6%) say they would be less motivated, about four in ten voters (37%) say such a decision would make them more motivated to vote. As many election forecasters are projecting a Republican wave in the upcoming midterms, the poll finds the Supreme Court decision may motivate Democratic voters but fewer Republican or independent voters. More than half (55%) of Democratic voters say the Supreme Court decision will make them more motivated to vote. Majorities of Republican voters (73%), independent voters (62%), and Republican women voters (74%) say it would not make a difference to their motivation.

A majority of voters who are motivated by the Supreme Court decision are pro-choice (75%), younger (55% under age 50), half are Democrats (51%), and about four in ten are liberal (38%). Similar shares of Black voters (40%), Hispanic voters (37%), and White voters (35%) report a Supreme Court decision overturning Roe would make them more motivated to vote. In addition, about one in five voters who say they would be motivated by the Supreme Court decision are Republican (18%), want a candidate who will limit access to abortions (19%), are conservative (21%) and independent (22%).
How Candidates’ Stance On Abortion May Impact Voters
If the Supreme Court overturns Roe v. Wade, between now and the midterm elections, one would expect the issue will become more salient in the midterms with increased attention in campaign advertisements and candidate talking points.3 The KFF Tracking Poll finds this salience may play an important role in persuading a small share of voters.
About half (52%) of voters overall say they are more likely to vote for a candidate in the upcoming election who wants to protect access to abortion, about one-quarter (27%) are more likely to vote for a candidate who will limit access to abortion, and one in five voters say a candidate’s position on abortion does not matter to their vote. Eight in ten (79%) Democratic voters say that they are more likely to vote for a candidate in the upcoming election who wants to protect access to abortion, 9% prefer a candidate who wants to limit access to abortion, and 11% say a candidate’s position on abortion would make no difference to their vote. At least half of Republicans say they want to vote for someone who wants to limit access to abortion (56%), 15% prefer a candidate who wants to protect access to abortion, and a sizeable three in ten (29%) Republican voters say it does not make a difference to their vote. Half (54%) of independent voters prefer a candidate who wants to protect access to abortion while half are split between preferring a candidate who wants to limit abortion (24%) or that it does not matter to their vote (22%).

Across key demographics, groups that typically lean more Democratic consistently report they want a candidate who will protect access to abortions. For example, more than half of Black voters (58%) and Hispanic voters (52%) say they are more likely to vote for such a candidate. In addition, younger voters are more likely than their older counterparts to say they want a candidate who will protect access to abortion, with six in ten (59%) voters ages 18-49 saying they are more likely to vote for a candidate who wants to protect access to abortion, compared to less than half (44%) of voters ages 50 and older. This age divide on the issue of abortion is consistent with other studies and this poll finds the age divide exists across partisans and gender, with younger independents, Republicans and men being more likely than their older counterparts to say that they are more likely to vote for a candidate that wants to protect access to abortion.

While the Supreme Court overturning Roe v. Wade doesn't appear to motivate a majority of voters overall, there is a small share of voters (20%) who say they would be more motivated to vote, and they would only support a candidate who shares their view, and they want candidates to protect access to abortion. This includes nearly four in ten Democratic voters, Democratic women voters, and one-fourth of women voters ages 18-49. A smaller share of voters (4%) say they are more motivated to vote by the Supreme Court decision, but in the opposite direction - to support candidates who want to limit access to abortions.
In Their OWn Words, Voters Say What About Overturning Roe Motivates Their Vote
When asked to say in their own words what it is about a Supreme Court decision overturning Roe that would make them more motivated to vote, about one-fourth cite a need to protect women’s rights to choose, rights to privacy and bodily autonomy (23%), about one in five mention wanting legislation to codify the right to an abortion or to vote for people who will protect abortion rights (18%), and 8% say that Roe v. Wade is the law and should not be overturned. About one in ten (9%) say they are motivated by wanting legislators who will ban abortions or support overturning Roe v. Wade. Five percent of voters who are motivated by Roe say that it is about having their voices heard and wanting legislators who represent their beliefs.

In Their Own Words: What specifically about the Supreme Court ruling that could overturn Roe v. Wade would make you more motivated to vote?
Among those who prefer a candidate who will protect access to abortion:
“I feel very strongly that everyone should have access to abortion, and I would be even more inclined to use my right to vote to help myself and others who think alike.” -21 year-old Democratic woman, Kentucky
“Voting in politicians who will protect abortion rights in their state if the federal government won't do it themselves.” -25 year-old Democratic woman, Florida “I'm actually not a person to jump out and vote but, on this issue, if my vote would make a difference then I will vote.” -37 year-old independent woman, California
“Protecting access to health care will make me even more likely to vote in the midterms.” -47 year-old independent man, Arizona
“I'm moderate not conservative. Every choice of a woman has different circumstances. I feel they should not all be subject to one blanket law. Democrats are more open minded about that.” -48 year-old Democratic woman, Missouri
In Their Own Words: What specifically about the Supreme Court ruling that could overturn Roe v. Wade would make you more motivated to vote?
Among those who want a candidate who will limit access to abortion:
"Vote for people in my state that would restrict abortion.” -79 year-old Republican woman, Missouri
“We need more moral minded leaders voted in.” -73 year-old Republican woman, Tennessee
“It would stop some of the murder of the pre-born.” -82 year-old Republican woman, Texas
“I would not want to see abortions done unless under certain circumstances.” -48 year-old Republican woman, Florida
“Murder shouldn’t be legal.” -46 year-old independent man, Minnesota
Public’s Opinion on Overturning Roe v. Wade, State Restrictions
KFF polling has consistently found that a majority of the public do not want to see Roe v. Wade overturned and the latest KFF poll is no different. About two-thirds (64%) U.S. adults say they do not want to see the Supreme Court overturn Roe v. Wade, while one-third of adults say they would like to see the case overturned. Majorities across gender and racial and ethnic groups say they don’t want to see it overturned, but there are differences by partisanship. Six in ten (61%) Republicans want to see the law overturned while a large majority of Democrats (85%) and six in ten independents (62%) do not want the Supreme Court to overturn Roe.

Once again, saliency lies on the side of those who want to protect abortion rights. While a large majority of Democrats (70%) say they feel “very strongly” that Roe v. Wade should not be overturned, Republicans are not as coalesced, with the about half as many Republicans (37%) feel “very strongly” that it should be overturned. A further one-quarter (24%) of Republicans feel “somewhat strongly” that Roe should be overturned, and a similar share (22%) feels “somewhat strongly” that it should not be overturned.
The public has mixed feelings on the potential for the Supreme Court to overturn Roe v. Wade and allowing states to ban abortion, with about half of adults reporting that they would feel “sad” (53%) or “angry” (47%), and fewer saying they would feel “hopeful” (34%), “indifferent” (27%) or “enthusiastic” (22%) about this decision.
Partisans have very different emotional responses to the possibility of the Supreme Court overturning Roe v. Wade, with nearly three-fourths of Democrats reporting they would be “sad” (74%) or “angry” (72%), while more than half of Republicans saying they would feel “hopeful” (57%) and four in ten would be “enthusiastic” (41%).
While a majority of women report they would be “sad” (56%) or angry” (51%) if the Supreme Court overturned Roe, there are differences among women – and men – across age groups. Majorities of adults under age 50 – both men and women – say they would feel “sad” or “angry” if Roe were overturned while four in ten older men and women say they would feel “hopeful” if this occurred.
Most Say Abortion Should Be Personal Choice Rather Than Regulated, Some Support For Limited State Regulations
Despite divided views on the future of Roe v. Wade, the public is somewhat more aligned in believing that getting an abortion should be a personal choice rather than one regulated by the government. Three in four U.S. adults say generally, getting an abortion should be a personal choice (74%), while one in four say it should be something that is regulated by law. Large majorities of Democrats (90%) and independents (74%) say it should be a personal choice, while Republicans are split (52% saying it should be a personal choice and 48% say it should be regulated by law). Eight in ten (79%) women ages 18-49 say that getting an abortion should be a personal choice, including majorities across party; nine in ten (90%) Democratic women, eight in ten (80%) independent women and about six in ten (59%) Republican women ages 18-49 say this should be a personal choice.
Awareness Of State-Specific Abortion Legislation
Landscape of state-level abortion legislation in the U.S. if Roe v. Wade is overturned:
If Roe v. Wade is overturned, the availability and legality of abortion will vary from state to state, with many already preparing for the impending Supreme Court ruling and defining what a post-Roe world would look like in their states. Should the Court rule to overturn Roe v. Wade, abortion will likely become illegal immediately in 17 states that either already have laws that ban abortion that predate Roe v. Wade or have passed laws limiting abortion to the maximum extent permitted by federal law.4 Three states (GA, OH and SC) have 6 week bans that courts have temporarily blocked but could become effective soon after a decision overruling Roe v. Wade.
In contrast, 16 states and Washington, D.C., have explicit laws in place codifying the right to an abortion in their state. Many of these states have enacted new laws and are also considering bills to expand funding and access to people who live in states where abortion will be banned or restricted, as well as legal protections for clinicians and patients who obtain abortions.5
In the remaining states, the future of abortion access is less clear, and will likely depend on the political parties in office in the coming years.
Just over four in ten (45%) of those living in the 17 states with laws that would likely ban abortion immediately, known as trigger laws, or abortion bans still in place since before Roe v. Wade was decided in 1973, are aware that if Roe v. Wade is overturned, abortion will no longer be legal in their state, while four in ten (42%) are not sure, and 13% say it would continue to be legal. While a small majority (55%) of women ages 18-49 in these states are aware that abortion would immediately be banned in their state, nearly half are either not sure (33%) or incorrectly believe abortions would continue to be legal (12%).
Two-thirds (63%) of those living in states where the right to an abortion is explicitly protected are aware that abortion would continue to be legal if the case was overturned, while three in ten are unsure, and few (8%) think it would no longer be legal in their state.

Populations Most Affected by Abortion Bans
If Roe v. Wade is overturned and many states across the country move to ban or restrict abortion access, people of color, lower-income people, and younger people would be disproportionately impacted by the laws largely due to the high cost of travel to neighboring states. The states seeking to ban abortions are concentrated heavily in the South, which has large shares of Black and Hispanic adults, the Plains which has a large Indigenous population, and the Midwest. Despite a few states passing legislation that would protect out-of-state residents seeking abortions in their state, many people in these populations would still be unable to travel to neighboring states to access abortion, forcing them to either seek abortion services outside of recognized clinical care, or carry their pregnancy to term.
Large majorities of adults who reside in states with trigger laws or pre-Roe abortion bans know that for various groups of women, getting an abortion will prove more difficult in their state if Roe is overturned. In the states where the right to an abortion will be most vulnerable, eight in ten say that a Supreme Court decision overturning Roe v. Wade will make it harder for young women (82%), lower-income women (78%), Black and Hispanic women (76%), and the women in their life (77%) to get an abortion in their state.
While there is widespread awareness of the impacts on certain populations, partisans differ on their assessment of whether this is a “good thing” or a “bad thing,” with larger shares of Republicans saying it is a “good thing” that it would be harder for each of these groups to get an abortion in their state and larger shares of Democrats viewing it as a “bad thing.” Notably, at least one in five Republicans say that it would be a “bad thing” that it would be more difficult for these groups to obtain an abortion.
Among women of reproductive age in these states, about six in ten believe overturning Roe v. Wade would make abortion harder to access in their state and that this is a “bad thing”, while between two and three in ten say making abortion harder to access would be a “good thing.”
State Legislation On Abortion
The Supreme Court’s 1992 decision for Planned Parenthood v. Casey established the right of states to regulate abortion services before viability as long as the regulation does not place an “undue burden” on women seeking an abortion. “Undue burden” is shorthand for a state regulation that has been found to have the purpose or effect of placing a substantial obstacle in the path of a person seeking an abortion. Since the Casey decision in 1992, many states have enacted a wide range of restrictions such as counseling, ultrasound and waiting period requirements; parental notification and consent requirements, restrictions on insurance coverage for abortion, and regulations specific to facilities and clinicians providing abortions. If the Supreme Court overrules Roe v. Wade, states will be able to enact abortion regulations without having to pass the “undue burden” standard and states could pass restrictions that could effectively block abortion access without actually passing a ban on abortion.
Among the public, there is some support for certain state-level restrictions on women seeking abortions, but majorities of the U.S. public oppose criminalizing women, doctors, or people who assist those seeking abortion care. Waiting periods are a common regulation on abortion and 27 states have enacted waiting periods ranging from 18 to 72 hours after contacting the clinic. Two-thirds of the public (67%) support laws requiring women to wait 24 hours between meeting with a health care provider and getting an abortion. Gestational limits are another type of law that states have enacted to limit how far into a pregnancy an abortion can be performed. Recently, several states have passed laws banning abortions after the time in which fetal cardiac activity can be detected, around 6 weeks of pregnancy (which is often before a person knows they are pregnant). While many of these laws have been blocked, this type of ban on all but the earliest abortions is currently in effect in Texas. Forty-four percent of adults support laws prohibiting abortions “once a fetal heartbeat is detected, which is usually around six weeks” (44%), while 54% are opposed to these types of laws. While this is unchanged from a 2019 KFF poll, that poll found that when the public was told that six weeks is usually before many women know they are pregnant, opposition to this policy increased to six in ten.
Large majorities oppose making it a crime for doctors to perform abortions (73%) or for women to get abortions (79%). With the impending Supreme Court decision on Roe, some states have passed restrictions to ban abortions using civil enforcement and penalties. Oklahoma and Texas have laws in effect that allow private citizens to sue people who provide or abet women in getting an illegal abortion. Some state legislators have considered making it a crime to travel across state lines to obtain an abortion, but such a law is not currently in effect in any state. KFF polling finds that eight in ten oppose each of these types of laws. It is also worth noting that several states have taken action to uphold the right or expand access to abortion and also protect doctors practicing in their states from criminal or civil liabilities for performing abortions in their state.

There is also majority opposition to many of these state policies on abortion among those who reside in states where there are trigger laws or pre-Roe abortion bans. At least two-thirds of people living in these 17 states oppose criminalizing doctors for performing abortions (69%), making it a crime for women to cross state lines to get an abortion (76%), making it a crime for a woman to get an abortion (74%), or allowing private citizens to sue people who provide or assist in abortions (78%).
Partisans differ in their level of support for these state-level abortion policies. A majority of Republicans support a 24-hour waiting period (90%) and prohibiting abortions once there is cardiac activity (70%). However, less than half of Republicans now support making it a crime for doctors to perform abortions that would result in fines or prison time (47%, down from 58% in 2019), making it a crime for women to get an abortion (36%, down from 49% in 2019), allowing private citizens to sue people who provide or assist women in getting abortions (32%) or making it a crime for a woman to cross state lines to get an abortion (35%). Independents are also less likely than they were in 2019 to support laws that would criminalize doctors (25%, down from 34% in 2019). About one in five independents continue to support criminalizing women seeking an abortion (19% v. 23% in 2019).
With the exception of the law that requires women to wait 24 hours between meeting a health care provider and getting an abortion, fewer than half of Democrats and independents support these laws.
In states that have protected the right to an abortion, there is growing momentum to provide public funding to support their clinics to provide abortion care to out-of-state women who seek an abortion in their state. Among those who live in a state that has laws in place protecting the right to an abortion, majorities oppose (56%) using public funding to cover these costs. However, two-thirds (64%) would support a law that would require all employer provided health insurance plans to cover an abortion.

If abortion is banned in many states across the country, the costs associated with obtaining an abortion will increase for those who are able to travel out of state to obtain abortion services. Some employers have begun offering to cover travel expenses for employees who need to travel out of state to obtain an abortion. Asked if they would support or oppose employers paying the travel costs for an employee to travel out-of-state to obtain an abortion if abortion is not available where they reside, a slim majority (51%) of U.S. adults say they would support this and 47% oppose. Seven in ten (72%) Democrats support this, and nearly eight in ten (78%) Republicans oppose. Independents are divided, with about half saying they support (53%) or oppose (44%) this workplace benefit. Younger adults across gender are more likely than their older counterparts to support this benefit.
Gaps Remain in Public’s Knowledge About Abortion, Birth Control
This KFF poll examines what Americans know about abortion services and finds there are significant knowledge gaps on the prevalence and the overall safety of abortions.
How common are abortions? The number of abortions performed in the U.S. has been steadily decreasing over the last several decades, and reached a historic low in 2017, of 11.4 abortions per 1,000 women ages 15 to 44, although it increased slightly (by 2%) between 2017 and 2019. The decline in abortion rates is often attributed to greater affordability of contraception and increased use of highly effective long-acting reversible contraception such as IUDs and contraceptive implants. Still, using 2014 abortion rates, an estimated 1 in 4 reproductive-aged women (24%) will have had an abortion by age 45.
Does abortion cause breast cancer? No. The link between abortions and breast cancer has been refuted by The National Cancer Institute (NCI) and the American College of Obstetricians and Gynecologists (ACOG) but was used in misinformation campaigns from the 1970s until the early 2000s.
Does abortion cause infertility? No. A major study of the quality and safety of abortion by the National Academies of Science, Engineering, and Medicine found no association between abortion and secondary infertility. Only a minute fraction (0.23%) of legal abortions in a clinical setting in the U.S. have complications that could lead to infertility.
Is abortion safe? Yes. Abortion has fewer complications than many other common procedures, such as wisdom tooth removal (7%), tonsil removal (8-9%), appendix removal (13%), and childbirth (29%).
At what point in pregnancy do most abortions occur? The vast majority of abortions occur early in pregnancy; most (79%) occur at ≤9 weeks gestation, while almost all (93%) are performed at ≤13 weeks gestation (also referred to as the 1st trimester). Abortions later in pregnancy, at ≥21 weeks gestation, are rare, comprising only 1.2% of all abortions.
Two-thirds of U.S. adults (64%) say that they or someone they know has had an abortion, including at least six in ten Democrats, independents and Republicans, men, and women. Yet, about half of U.S. adults (49%) incorrectly say that less than 10% of women in the U.S. have had an abortion, when the actual share is closer to one-quarter. Men are more likely than women to underestimate the share of women who have had an abortion, with six in ten (56%) of men saying it is true that less than 10% of women have had an abortion.
A large majority of the public (87%) across partisan and age groups correctly says that it is false that a woman who has gotten an abortion has a higher risk of getting breast cancer. However, a small share (9%) of all adults, rising to 13% of Republicans, believe this to be true. Three quarters (72%) of U.S. adults correctly say that a woman who has gotten an abortion will not have a harder time getting pregnant again, while one-fourth (26%) say that this statement is true, rising to one-third of Republicans.
Many also do not know at what point in pregnancy most abortions occur. Majorities (65%) incorrectly say most abortions occur after eight weeks of pregnancy, while one-third (32%) correctly say most occur fewer than eight weeks into pregnancy. Few, however, believe that most abortions occur more than 20 weeks into pregnancy (2%).
How much does an abortion cost? Recent research finds that the median out-of-pocket cost of a first-trimester abortion is close to $600 for those who self-pay, not including costs that could be incurred to travel out of state or take time off from work.
Cost can be a barrier for women seeking abortion care, as many adults cannot afford the expense and not all health insurance plans cover abortion services. In fact, among women ages 18 to 49 who are insured, more than eight in ten (84%) say that they do not know if their insurance plan covers the cost of an abortion. Just 6% say that their insurance plan does cover the cost of an abortion, and one in ten say it does not. Most women of reproductive age do not know the cost of an abortion during the first trimester in the U.S. Just 14% correctly say that the cost out-of-pocket for a first-trimester abortion is between $500 and $700, while one-third (32%) are unsure of the cost, and many both over and underestimate the cost of this procedure.
Medication Abortion
While medication abortion now accounts for more than half of all abortions in the U.S., fewer than three in ten U.S. adults (27%) say they have heard of the medication abortion pill known as mifepristone, up slightly from 2019 (21%). Women ages 18-49 (40%) are twice as likely as women ages 50 and older (19%) and men (23%) to say they have heard of the medication abortion pill.
Of those who had heard of it, 63% (17% of total) correctly say that mifepristone can be effectively used to end a pregnancy up to the first 10 weeks. Few (12%) incorrectly say it is effective at any point during pregnancy. Six in ten of those who have heard of mifepristone (59%, 16% of total) know that a prescription is required to get medication abortion pills, while four in ten either incorrectly say it is available without a prescription (13%) or that they are unsure (28%).
Small Majorities Support requiring in-person appointments for Medication Abortion Prescriptions
Since the start of the COVID-19 pandemic, medical providers have been expanding their use of telehealth to consult with patients on issues that do not require in-person appointments. The expansion of telehealth has given some people access to health care when they otherwise would not be able to due to barriers to access, time, and distance required to travel to providers. The FDA no longer requires mifepristone to be dispensed in-person in a clinical setting, which has enabled people in many states to obtain the medications through the mail rather than having to go to a clinic or provider to receive the medication.
However, some states have explicitly banned the use of telehealth for abortion and others have instituted policies such as ultrasound requirements that necessitate the physical presence of the prescribing clinician, despite the FDA’s finding that the use of telehealth for medication abortion is safe.6 Among the 27% of U.S. adults who have heard of mifepristone, six in ten (16% of all adults) say they support the policy already in effect in 19 states that requires patients to have an in-person appointment to obtain a prescription for medication abortion pills, while 40% (11% of all adults) are opposed to such a requirement.
Some Confusion remains about difference between Emergency Contraceptive Pills and Medication Abortion
Some state lawmakers have discussed the possibility of placing additional restrictions or limits on the use of emergency contraceptive pills. Most U.S. adults (92%), have heard of emergency contraceptive pills, sometimes called the morning after pill or “Plan B,” similar to the share who had heard of it in 2019 and up from 85% in 2003, shortly after it was approved by the FDA. Yet some knowledge gaps remain when it comes to how the pills work. While most are aware that emergency contraceptive pills are not the same as the abortion pill (62%), and that some types are available over-the-counter without a doctor’s prescription (72%), a substantial share (73%) incorrectly think that emergency contraceptive pills can end a pregnancy in its early stages.