The Effects of Medicaid Expansion under the ACA: Studies from January 2014 to January 2020
Executive Summary
Another analysis that reviews studies published between February 2020 and March 2021 is available here. That more recent analysis also updates summary figures on coverage, access, and economic findings across the full body of research published between January 2014 and March 2021.
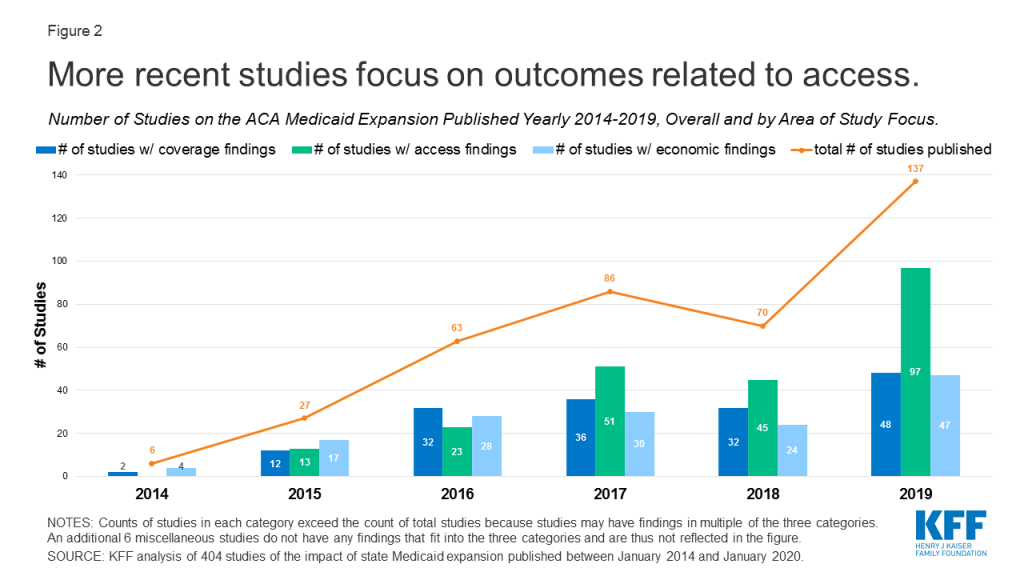
At the ten year mark since the passage of the Affordable Care Act (ACA), a substantial body of research has investigated effects of the Medicaid expansion on coverage; access to care and related measures (including utilization, quality of care and health outcomes, provider capacity, and affordability and financial security); and various economic measures. This issue brief summarizes findings from 404 studies (including 80 newly included since the last update of this analysis) of the impact of state Medicaid expansions under the ACA published beginning in January 2014 (when the coverage provisions of the ACA went into effect) and updates earlier versions of this brief with studies through January 2020.1
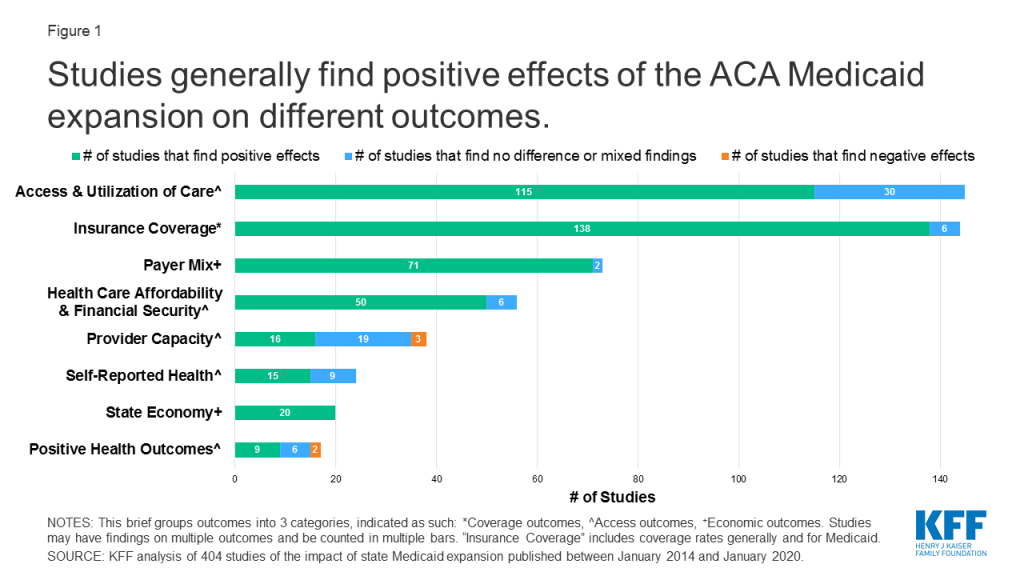
This brief groups outcomes into three broad categories: coverage, access, and economic measures. Research indicates that the expansion is linked to gains in coverage; improvements in access, financial security, and some measures of health status/outcomes; and economic benefits for states and providers (Figure 1).
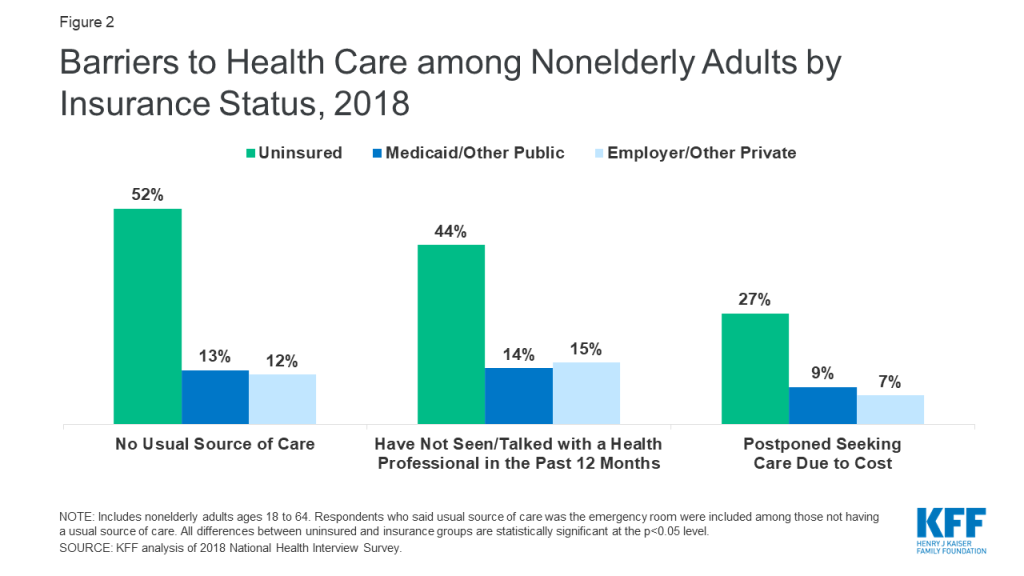
Studies included in this review may include multiple findings across multiple categories. For example, studies that point to increased coverage may also include findings related to access, outcomes, or economic metrics. While most early studies focused on expansion’s impact on coverage and economic measures, over time studies have increasingly focused on measures related to access to care (Figure 2).
Findings related to coverage, access, and economic measures are discussed in detail in the text of this brief and are also summarized below:
Coverage: Studies show that Medicaid expansion states experienced significant coverage gains and reductions in uninsured rates among the low-income population broadly and within specific vulnerable populations. States that implemented the expansion with a waiver have seen coverage gains, but some waiver provisions appear to compromise coverage.
Access to care and related measures: Most research demonstrates that Medicaid expansion has improved access to care, utilization of services, the affordability of care, and financial security among the low-income population. Studies show improved self-reported health following expansion and an association between expansion and certain positive health outcomes. A small subset of study findings showed no effects of expansion on certain specific measures within these access-related categories. Findings on expansion’s effect on provider capacity are mixed, with studies showing increases, decreases, or no effects on measures like appointment availability or wait times.
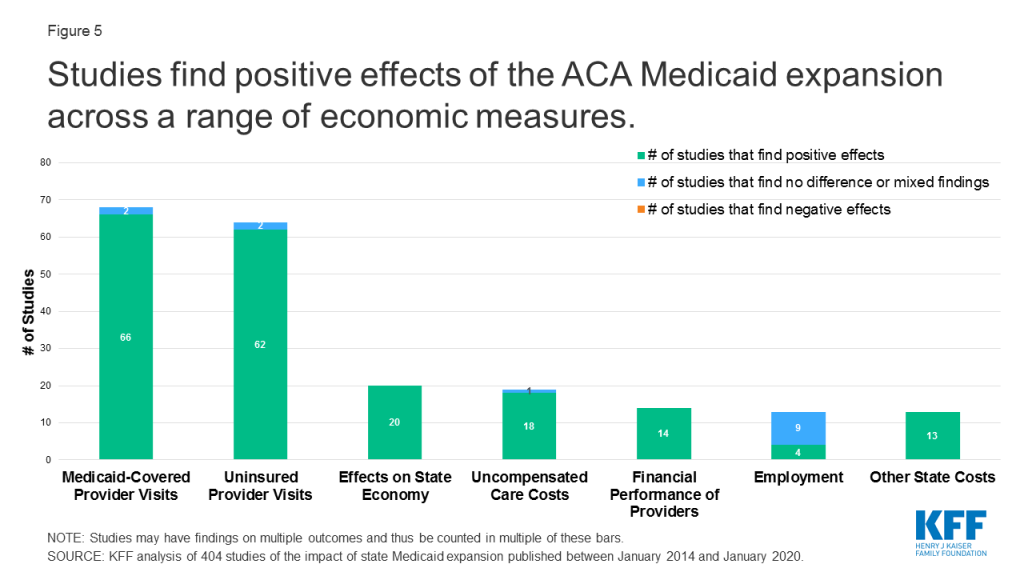
Economic measures: Analyses find effects of expansion on numerous economic outcomes, including state budget savings, revenue gains, and overall economic growth. Multiple studies suggest that expansion can result in state savings by offsetting state costs in other areas. The federal government covered 100% of the cost of the expansion in the early years of the ACA and will cover 90% beginning in 2020. There is limited research examining the fiscal effects of the Medicaid expansion at the federal level. Additional studies show that Medicaid expansions result in reductions in uncompensated care costs for hospitals and clinics, and a growing number of studies show an association between expansion and gains in employment as well as growth in the labor market (with a minority of studies showing neutral effects in this area).
More recent studies: Recently published studies newly included in this analysis from July 2019 through January 2020 support earlier findings while using the additional years of experience with expansion to deepen findings in many areas, including expansion’s effects on health outcomes, access to services and medications for behavioral health and other needs, providers’ financial stability, and employment. Some recent analyses that include outcomes beyond those typically examined in Medicaid expansion research show that expansion is associated with decreased mortality overall and for certain specific conditions; reductions in rates of food insecurity, poverty, and home evictions; and improvements in measures of self-reported health and healthy behaviors.
Looking back and looking ahead: Looking back on 10 years since the ACA has been enacted shows that the Medicaid expansion has expanded coverage and led to increases in access and utilization to health care services, improvements in financial security and positive net effects for state budgets and revenues. This analysis may help inform states still debating whether to adopt the expansion. Future studies will continue to examine the economic implications of the expansion as the state share of costs remains constant at 10 percent. A looming economic downturn will also test how the Medicaid expansion affects coverage and state budgets. Looking ahead, while additional states may expand eligibility under the ACA, the changing landscape of Medicaid demonstration activity could limit the reach of the Medicaid expansion as envisioned under the law. For example, the administration issued new guidance that would allow states to cover certain adults (including the expansion population) through new demonstrations with eligibility restrictions and not apply other Medicaid rules in exchange for capped financing. In addition, continued efforts from the administration to conduct intense oversight and change the rules on Medicaid enrollment and financing, as well as litigation efforts to repeal the entire ACA keep the law in the spotlight and highlight future challenges. The outcome of the next election could bring significant changes to the ACA, including the Medicaid expansion.
Methods
This literature review summarizes findings from 404 studies of the impact of state Medicaid expansions under the ACA published beginning in January 2014 (when the coverage provisions of the ACA went into effect). This version of the brief updates earlier versions and includes studies published through January 2020. It includes studies, analyses, and reports published by government, research, and policy organizations using data from 2014 or later and only includes studies that examine impacts of the Medicaid expansion in expansion states. This review excludes studies on impacts of ACA coverage expansions generally (not specific to Medicaid expansion alone), studies investigating potential effects of expansion in states that have not (or had not, at the time of the study) expanded Medicaid, and reports from advocacy organizations and media sources.
To collect relevant studies, we conducted keyword searches of PubMed and other academic health/social policy search engines as well as websites of government, research, and policy organizations that publish health policy-related research. We also used a snowballing technique of pulling additional studies from reference lists in previously pulled papers. While we tried to be as comprehensive as possible in our inclusion of studies and findings that meet our criteria, it is possible that we missed some relevant studies or findings. For each study, we read the final paper/report and summarized the population studied, data and methods used, and findings. In instances of conflicting findings within a study, or if a reviewer had questions about specific findings, multiple reviewers read and classified the study to characterize its findings. In the issue brief text, findings are broken out and reported separately in three broad categories: Medicaid expansion’s impact on coverage; access to care and related measures; and economic outcomes for the expansion states. Studies may be cited in multiple of these categories or in multiple places within a category. The Appendix at the end of the brief provides a list of citations for each of the included studies, grouped by the three categories of findings.
Report
Impacts on Coverage
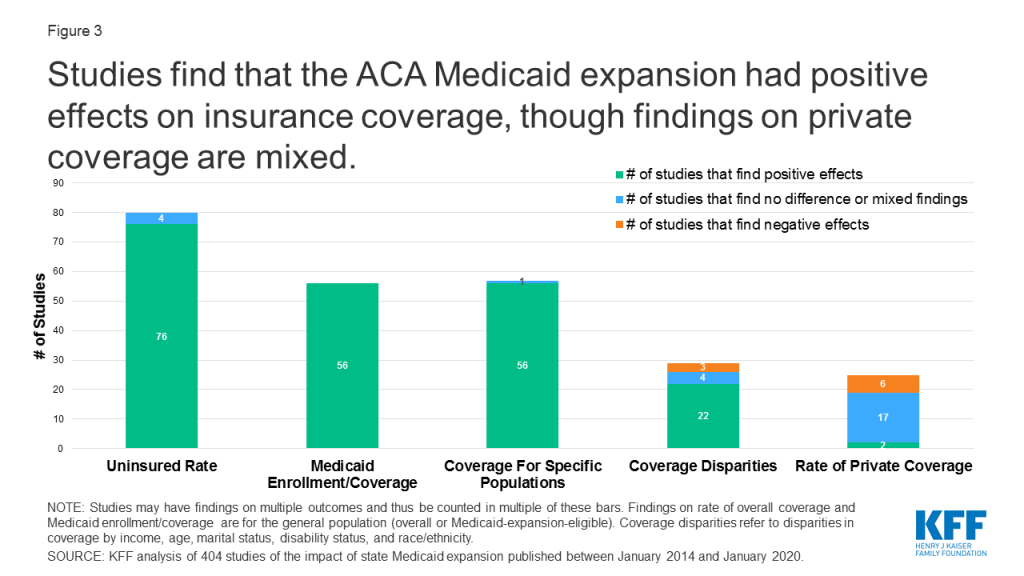
Studies find positive effects of Medicaid expansion on a range of outcomes related to insurance coverage (Figure 3). In addition to changes in uninsured rates and Medicaid coverage, both overall and for specific populations, studies also consider private coverage and waiver implications.
Uninsured Rate and Medicaid Coverage Changes
States expanding their Medicaid programs under the ACA have seen large increases in Medicaid enrollment. These broad coverage increases have been driven by enrollment of adults made newly eligible for Medicaid under expansion. Enrollment growth also occurred among both adults and children who were previously eligible for but not enrolled in Medicaid (known as the “woodwork” or “welcome mat” effect). Some, but not all, research finds evidence of reduced coverage churn in expansion compared to non-expansion states.2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61
Numerous analyses demonstrate that Medicaid expansion states experienced large reductions in uninsured rates that significantly exceed those in non-expansion states. The sharp declines in uninsured rates among the low-income population in expansion states are widely attributed to gains in Medicaid coverage. Declines began in 2014, and some studies showed that expansion-related enrollment growth in Medicaid and declines in uninsured rates in expansion states continued in 2015, 2016, and 2017 and that the gap between coverage rates in expansion and non-expansion states continued to widen in the years after 2014. Two studies found that despite a nationwide increase in uninsured rates from 2016 to 2017, uninsured rates remained stable in states that had expanded Medicaid and coverage losses were concentrated in non-expansion states.62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 101 102 103 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 121 122 123 124 125 126 127 128 129 130 131 132 133 134 135 136 137 138
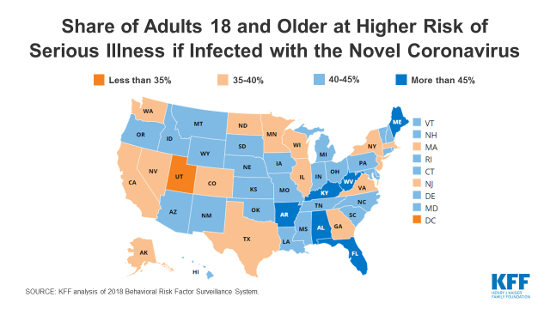
Several studies identified larger coverage gains in expansion versus non-expansion states for specific vulnerable populations. While the list of specific populations studied is long, studies include: individuals across the lifespan (children, young adults, women of reproductive age with and without children, and the near-elderly), lesbian, gay, and bisexual adults, the unemployed, low-income workers, justice-involved individuals, homeless individuals, noncitizens, people living in households with mixed immigration status, migrant and seasonal agricultural workers, and early retirees. Other populations that experienced coverage gains include those with specific medical conditions or needs such as prescription drug users, people with substance use disorders including opioid use disorders, people with HIV, people with disabilities, low-income adults who screened positive for depression, adults with diabetes, cancer patients/survivors, adults with a history of cardiovascular disease or two or more cardiovascular risk factors, and veterans.139 140 141 142 143 144 145 146 147 148 149 150 151 152 153 154 155 156 157 158 159 160 161 162 163 164 165 166 167 168 169 170 171 172 173 174 175 176 177 178 179 180 181 182 183 184 185 186 187 188 189 190 191 192 193 194 195
Most analyses that looked at rural/urban coverage changes find that Medicaid expansion has had a particularly large impact on Medicaid coverage or uninsured rates in rural areas. Studies have found that Medicaid expansion reduced or eliminated disparities in coverage between adults living in rural vs. urban areas. However, as noted below, research on coverage effects in rural versus urban areas was mixed.196 197 198 199
Studies show larger Medicaid coverage gains and reductions in uninsured rates in expansion states compared to non-expansion states occurred across most or all of the major racial/ethnic categories. Additional research also suggests that Medicaid expansion has helped to reduce disparities in coverage by income, age, marital status, disability status, and, in some studies, race/ethnicity.200 201 202 203 204 205 206 207 208 209 210 211 212 213 214 215 216 217 218 219 220 221 222 223 224
A minority of coverage studies show no effect or mixed results of expansion in certain areas. Many of these findings were included in studies that had additional findings related to coverage or disparity improvements and are also cited above. Some findings within three studies did not show greater coverage changes for rural areas. A limited number of studies found that expansion was not significantly associated with changes in the uninsured rate among certain specific groups, as Medicaid coverage gains in expansion states were offset larger private insurance gains in non-expansion states for these groups. Findings within four studies suggested that expansion was associated with an increase in coverage disparities (by gender in one study, by race/ethnicity in another, and by marital status among women in two others). In addition, one study showed no significant differences in churn rates among low-income adults between 2013 and 2015 based on the state’s expansion policy.225 226 227 228 229 230 231 232 233 234 235 236 237 238 239 240 241 242 243 244 245 246 247 248
Private Coverage and Waiver Implications
Some studies exploring the effects of Medicaid expansion on private insurance coverage found no evidence of Medicaid expansion coverage substituting for private coverage including employer-sponsored insurance, while other studies showed declines in private coverage associated with expansion overall or among certain specific population groups. These declines in private coverage may occur if individuals previously covered through employer-sponsored or self-pay insurance opt in to Medicaid given Medicaid’s typically lower out-of-pocket costs and more comprehensive benefit packages, or if employers alter their offering of coverage in response to the expansion of Medicaid. Private coverage changes in studies that include states that expanded later than January 2014 may also reflect people above 100% FPL transitioning from subsidized Marketplace coverage to Medicaid after their state adopts the expansion.249 250 251 252 253 254 255 256 257 258 259 260 261 262 263 264 265 266 267 268 269 270 271 272 273
States implementing the expansion with a waiver have seen similar or larger gains in coverage as states not using waivers, but research finds that some provisions in these waivers present barriers to coverage.
- Studies show that some states initially expanding Medicaid with Section 1115 waivers experienced coverage gains that were similar to gains in states implementing traditional Medicaid expansions. Research comparing Arkansas (which expanded through a premium assistance model) and Kentucky (which expanded through a traditional, non-waiver model) showed no significant differences in uninsured rate declines between 2013 and 2015 in the two states. An analysis of expansion waiver programs in Michigan and Indiana showed that both states experienced uninsured rate reductions between 2013 and 2015 that were higher than the average decrease among expansion states as well as large gains in Medicaid enrollment.274 275 276 277 278 279
- A growing body of research suggests that certain Section 1115 waiver provisions that target the expansion population have caused coverage losses or presented barriers to enrollment, particularly in Arkansas related to the implementation of a Medicaid work requirement and in Indiana related to the Healthy Indiana Plan (HIP) 2.0 monthly contribution requirements.280 ,281 ,282 283 284 285 286 287 288 289 290
Impacts on Access and Related Measures
Studies find positive effects of Medicaid expansion on a range of outcomes related to access (Figure 4). In addition to impacts on access to and utilization of care, studies consider the effect of expansion on quality of care, self-reported health, and health outcomes; provider capacity; and affordability and financial security.
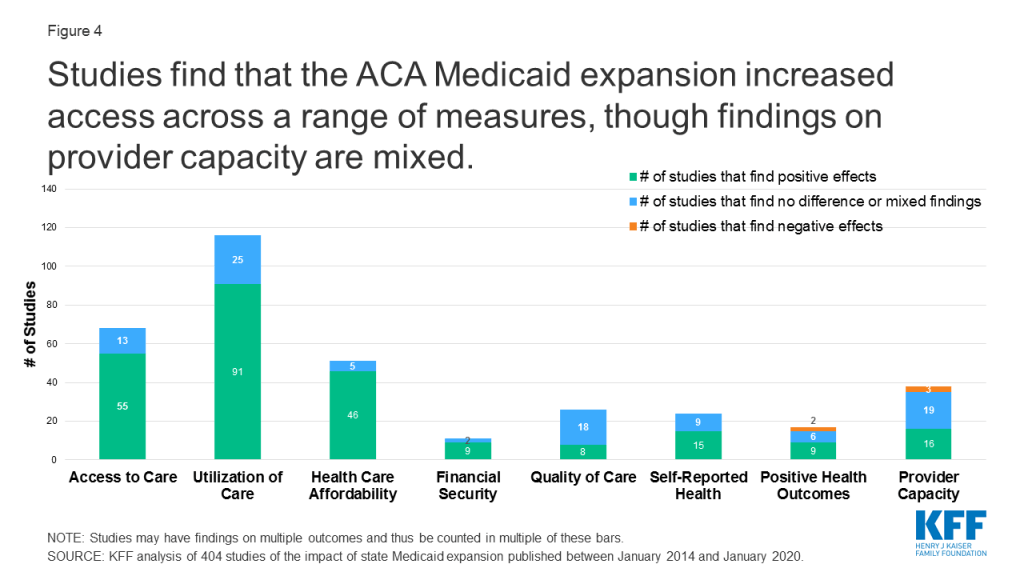
Access to Care and Utilization
Most research demonstrates that Medicaid expansion improves access to care and increases utilization of health care services among the low-income population. Many expansion studies point to improvements across a wide range of measures of access to care as well as utilization of a variety of medications and services. Some of this research also shows that improved access to care and utilization is leading to increases in diagnoses of a range of diseases and conditions and in the number of adults receiving consistent care for a chronic condition.291 292 293 294 295 296 297 298 299 300 301 302 303 304 305 306 307 308 309 310 311 312 313 314 315 316 317 318 319 320 321 322 323 324 325 326 327 328 329 330 331 332 333 334 335 336 337 338 339 340 341 342 343 344 345 346 347 348 349 350 351 352 353 354 355 356 357 358 359 360 361 362 363 364 365 366 367 368 369 370 371 372 373 374 375 376 377 378 379 380 381 382 383 384 385 386 387 388 389 390 391 392 393 394 395 396 397 398 399 400 401 402 403 404 405 406 407 408 409 410 411 412 413 414 415 416 417 418 419 420 421 422 423 424
For example:
- Cancer Diagnosis and Treatment. Multiple studies found that expansion was associated with significantly greater increases in overall or Medicaid-covered cancer diagnosis rates and/or early-stage diagnosis rates. Multiple studies found an association between expansion and increased access to and utilization of certain types of cancer surgery, with one study finding a decreased disparity in expansion states between Medicaid and privately-insured patients in the odds of undergoing surgery for certain types of cancer.425 426 427 428 429 430 431 432 433 434 435 436
- Transplants. Additional studies found a correlation between expansion and increased heart transplant listing rates for African American adults (both overall and among Medicaid enrollees) and increased lung transplant listings for nonelderly adults.437 438
- Smoking Cessation. Additional research found decreased cigarette and other nicotine product purchases and increased access, utilization, and Medicaid coverage of evidence-based smoking cessation medications post-expansion in expansion states relative to non-expansion states. For example, one recent study found that Medicaid expansion lead to a 24% increase in new use of smoking cessation medication.439 440 441 442 443 444
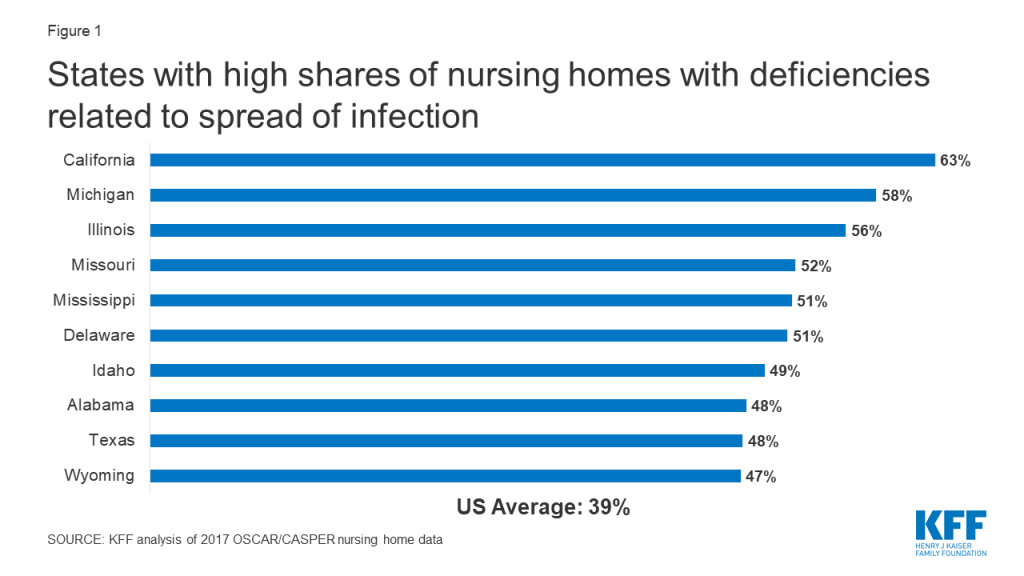
- Behavioral Health. Recent evidence demonstrates that Medicaid expansion states have seen improvements in access to medications and services for the treatment of behavioral health (mental health and substance use disorder (SUD)) conditions following expansion, with many national and multi-state studies showing greater improvements in expansion compared to non-expansion states. This evidence includes studies that have shown that Medicaid expansion is associated with increases in overall prescriptions for, Medicaid-covered prescriptions for, and Medicaid spending on medications to treat opioid use disorder and opioid overdose.445 446 447 448 449 450 451 452 453 454 455 456 457 458 459 460 461 462 463 464 465 466 467 468 469 470
- Medication Assisted Treatment (MAT) for Treatment of Opioid Use Disorder. Multiple studies have found increases in medication assisted treatment (MAT) drug prescriptions (either overall or Medicaid-covered prescriptions) associated with expansion. Some of these studies also found that in contrast, there was no increase in opioid prescribing rates (overall or Medicaid-covered) associated with expansion over the same period. One study found that expansion was associated with an 18% increase in aggregate opioid admissions to specialty treatment facilities, nearly all of which was driven by a 113% increase in admissions from Medicaid beneficiaries.471 472 473 474 475 476 477 478 479 480
Multiple recent studies have also found expansion to be associated with improvements in disparities by race/ethnicity, income, education level, insurance type, and employment status in measures of access to and utilization of care.481 482 483 484 485 486 487 488
Studies point to changes in patterns of emergency department (ED) utilization. Some studies point to declines in uninsured ED visits or visit rates and increases in Medicaid-covered ED visits or visit rates in expansion states compared to non-expansion states, compared to pre-expansion, or compared to other populations within expansion states. Studies show inconsistent findings about how Medicaid expansion has affected ED volume or frequency of visits overall or among specific populations (e.g., Medicaid enrollees or frequent ED users), with some studies showing increases, no change, or declines. Studies also showed decreased reliance on the ED as a usual source of care and a shift in ED use toward visits for higher acuity conditions among individual patients who gained expansion coverage, compared to those who remained uninsured in non-expansion states.489 490 491 492 493 494 495 496 497 498 499 500 501 502 503 504 505 506
In contrast with other studies’ findings on decreased reliance on the ED as a usual source of care, some recent studies suggest that Medicaid expansion may increase non-necessary use of certain health services. These services include hospitalization or specialty treatment for certain specific health conditions, including lupus, oral health conditions, and upper-extremity trauma. Authors explain that the non-necessary use of these services could be prevented by primary care and indicates the need for increased access to outpatient care for new enrollees.507 508 509 510
Evidence suggests that beneficiaries and other stakeholders lack understanding of some waiver provisions designed to change utilization or improve health outcomes. Multiple studies have demonstrated confusion among beneficiaries, providers, and advocates in expansion waiver states around the basic elements of the programs or requirements for participation, as well as beneficiary reports of barriers to completion of program activities (including internet access and transportation barriers). These challenges have resulted in increased costs to beneficiaries, beneficiaries being transitioned to more limited benefit packages, low program participation, or programs not operating as intended in other ways.511 512 513 514 515 516 517
Some study findings did not show that expansion significantly improved some measures of access, utilization, or disparities between population groups. Many of these findings were included in studies that also found related improvements in access, utilization, or disparities measures and are also cited above. Authors of some early studies using 2014 data note that changes in utilization may take more than one year to materialize. Consistent with this premise, a longer-term study found improvements in measures of access to care and financial strain in year two of the expansion that were not observed in the first year.518 519 520 521 522 523 524 525 526 527 528 529 530 531 532 533 534 535 536 537 538 539 540 541 542 543 544 545 546 547 548 549 550 551 552 553 554 555 556 557 558 559 560 561 562 563 564 565 566 567 568 569 570 571 572 573 574
Quality of Care, Self-Reported Health, and Health Outcomes
Several studies show an association between Medicaid expansion and improvements in quality of care. These include studies focused on the low-income population broadly, academic medical center or affiliated hospital patients, or community health center patients and look at outcomes including receipt of recommended screenings or recommended care for a particular condition.575 576 577 578 579 580 581 582
Additional studies show effects of expansion on measures of quality hospital care and outcomes. A few studies found that Medicaid expansion was associated with declines in hospital length of stay and in-hospital mortality as well as increases in hospital discharges to rehabilitation facilities, and one study found an association between expansion and declines in mechanical ventilation rates among patients hospitalized for various conditions. One recent study found that expansion was associated with decreased preventable hospitalizations, measured by reductions in annual ambulatory care-sensitive discharge rates and inpatient days. Additional analyses found that, contrary to past studies associating Medicaid insurance with longer hospital stays and higher in-hospital mortality, the shift in payer mix in expansion states (increase in Medicaid discharges and decrease in uninsured discharges) did not influence length of stay or in-hospital mortality for various types of patients.583 584 585 ,586 ,587 588 589 590 591 592 593 594 595
Multiple studies have found improvements in measures of self-reported health or positive health behaviors following Medicaid expansions. Studies found improvements in both measures of self-reported physical and mental health, as well as increases in healthy behaviors such as self-reported diabetes management. Additional research has documented provider reports of newly eligible adults showing improved health or receiving life-saving or life-changing treatments that they could not obtain prior to expansion.596 597 598 599 600 601 602 603 604 605 606 607 608 609 610 611 612
Studies have found an association between Medicaid expansion and improvements in certain measures of health outcomes. Studies in this area find an association between expansion and improvements in cardiac surgery patient outcomes and perforated appendix admission rates among hospitalized patients with acute appendicitis. One study did not find a significant association between expansion and differences in rates of low birth weight or preterm birth outcomes overall, but did find significant improvements in relative disparities for black infants compared with white infants in states that expanded vs. those that did not. Two studies found expansion was associated with increased odds of tobacco cessation (among adult CHC patients in one study and childless adults in the other).613 614 615 616 617 618
Additionally, a growing body of research has found an association between Medicaid expansion and mortality, either population-level rates overall, for particular populations, or associated with certain health conditions. A 2019 national study found that expansion was associated with a 0.132 percentage point decline in annual mortality among near-elderly adults driven largely by reductions in disease-related deaths, an effect that translates to about 19,200 deaths that were averted during the first four years of expansion (or 15,600 deaths in expansion states could have been averted in non-expansion states). A 2020 study found that expansion was associated with a 6% lower rate of opioid overdose deaths. Another study suggests that expansion may have contributed to infant mortality rate reductions, finding that the mean infant mortality rate rose slightly in non-expansion states between 2014 and 2016, compared to a decline in expansion states over that period (this effect was particularly pronounced among the African-American population). Studies also found reductions in cardiovascular mortality among middle-aged adults and in one-year mortality among end-stage renal disease patients initiating dialysis.619 620 621 622 623
Some studies did not find significant changes associated with expansion on certain measures of quality of care, self-reported health, or health outcomes.
- Some studies did not find an association between Medicaid expansion and quality outcomes; many of these studies focused on very narrow population groups and/or found a link between expansion and improvements in quality of care for some of the patient/population groups studied. One study found no significant association between Medicaid expansion and changes in quality of care delivered through Medicaid managed care plans. The authors suggest that this finding shows that the health system has generally been able to absorb new expansion enrollees without sacrificing care for existing enrollees.624 625 626 627 628 629 630 631 632 633 634
- Some studies on specific hospital patient groups found no significant changes associated with expansion in measures of hospital care and outcomes, including rates of emergent admission, admissions from clinic, diagnosis category at admission, admission severity, rapid discharges, lengthy hospitalizations, unplanned readmissions, discharges to rehabilitation facilities, or failure to rescue. One study found that expansion was associated with an increase in length of stay for adult trauma patients.635 636 637 638 639 640 641 642 643 644 645 646 647 648 649
- A small number of studies did not find significant changes in certain measures of self-reported health status, health outcomes including mortality, wellbeing, or healthy behaviors, or in disparities between certain population groups in these measures. One study found that although Medicaid expansion was associated with increased access to opioid pain-relievers, it was not significantly associated with any change in opioid deaths. Similarly, an earlier study found no evidence of expansion affecting drug-related overdoses or fatal alcohol poisonings. A third study found that although opioid overdose mortality rates increased more in expansion states, this difference was not caused by increased prescriptions. Given that it may take additional time for measurable changes in health to occur, researchers suggest that further work is needed to provide longer-term insight into expansion’s effects on self-reported health and health outcomes.650 651 652 653 654 655 656 657 658 659 660 661 662 663 664 665 666 667 668 669 670 671 672 673 674
Provider Capacity
Many studies conclude that providers have expanded capacity or participation in Medicaid following expansion and are meeting increased demands for care. Studies in this area include findings showing an association of expansion with increases in primary care appointment availability, the likelihood of accepting new patients with Medicaid among non-psychiatry specialist physicians, and Medicaid acceptance and market entry among select medication assisted treatment (MAT) providers. One study found improvements in receipt of checkups, care for chronic conditions, and quality of care even in areas with primary care shortages, suggesting that insurance expansions can have a positive impact even in areas with relative shortages. A survey of Medicaid managed care organizations found that over seven in ten plans operating in expansion states reported expanding their provider networks between January 2014 and December 2016 to serve the newly-eligible population.675 676 677 678 679 680 681 682 683 684 685 686 687 688 689 690 691 692 693 694 695 696 697 698 699 700 701
Some studies on measures of provider availability showed no changes associated with expansion. Authors note that findings of no changes may, in some cases, be viewed as favorable outcomes indicating that provider availability is not worsening in expansion states despite the increased demand for care associated with expansion. For example, despite concerns that expansion might worsen access for the already-insured, two studies found that expansion was not associated with decreased physician availability for Medicare patients.702 703 704 705 706 707 708 709 710 711 712 713 714 715
Other studies found expansion was linked to problems with provider availability. Some of these studies also had positive or insignificant findings related to provider capacity for certain populations or types of appointment with negative findings related to others. These include findings that Medicaid expansion was associated with longer wait times for appointments or increased difficulty obtaining appointments with specialists. Most of these studies use early data from 2014 and 2015.716 717 718 719 720 721 722 723 724 725 726 727
Affordability and Financial Security
Research suggests that Medicaid expansion improves the affordability of health care. Several studies show that people in expansion states have experienced reductions in unmet medical need because of cost, with national and multi-state studies showing those reductions were greater than reductions in non-expansion states. Research also suggests that Medicaid expansion results in significant reductions in out-of-pocket medical spending, and multiple studies found larger declines in trouble paying as well as worry about paying future medical bills among people in expansion states relative to non-expansion states. A recent study in Washington state found that among trauma patients, expansion was associated with a 12.4 percentage point decrease in estimated catastrophic healthcare expenditure risk. One study found that previously uninsured prescription drug users who gained Medicaid coverage in 2014 saw, on average, a $205 reduction in annual out-of-pocket spending in 2014. A January 2018 study that focused on the 100-138% FPL population in expansion and non-expansion states also found that Medicaid expansion coverage produced greater reductions than subsidized Marketplace coverage in average total out-of-pocket spending, average out-of-pocket premium spending, and average cost-sharing spending.728 729 730 731 732 733 734 735 736 737 738 739 740 741 742 743 744 745 746 747 748 749 750 751 752 753 754 755 756 757 758 759 760 761 762 763 764 765 766 767 768 769 770 771 772 773
- Studies have found that Medicaid expansion significantly reduced the percentage of people with medical debt, reduced the average size of medical debt, and reduced the probability of having one or more medical bills go to collections in the past 6 months.774 775 776 777 778 779 780 781 782 783 784
- A study in Ohio showed lower medical debt holding levels among continuously-enrolled expansion enrollees compared to those who unenrolled from expansion and those who had a coverage gap, suggesting that medical debt levels rose even after a relatively short time without Medicaid expansion coverage.785 786
Research also suggests an association between Medicaid expansion and improvements in broader measures of financial stability.787 788 789 790 791 792 793 794 795
For example:
- A study found that Medicaid expansion was associated with a 2.2 percentage point decrease in very low food security (which is characterized by actual reduction of food intake due to unaffordability) among low-income childless adults.796
- Two 2019 national studies looked at the association between Medicaid expansion and poverty rates. One found that expansion was associated with a reduction in the rate of poverty by just under 1 percentage point (or an estimated 690,000 fewer Americans living in poverty). The other found that Medicaid expansion was associated with a 1.7 percentage point reduction in the health-inclusive poverty measure (HIPM) poverty rate and a 0.9 percentage point reduction in the HIPM deep poverty rate that were significant across all demographic groups considered except single-parent households and were particularly substantial for vulnerable groups including children, the near-elderly (age 55-64), black people, Hispanics, and those who have not completed high school. The same study showed no significant change in the Census Bureau’s supplemental poverty measure (SPM).797 798
- Studies have found that Medicaid expansion significantly reduced the average number of collections, improved credit scores, reduced over limit credit card spending, reduced public records (such as evictions, bankruptcies, or wage garnishments), and reduced the probability of a new bankruptcy filing, among other improvements in measures of financial security. One 2019 study found that Medicaid expansion was associated with a 1.15 reduction in the rate of evictions per 1000 renter-occupied households and a 1.59 reduction in the rate of eviction filings.799 800 801 802 803 804
- A Michigan study found an association between expansion and improvements across a broad swath of financial measures.805
Multiple studies have found expansion to be associated with improvements in disparities by income or race/ethnicity in measures of affordability of care or financial security.806 807 808 809 810 811
Some study findings did not show significant effects of expansion on measures of affordability or financial security. Several of these studies did not identify statistically significant differences in changes in unmet medical need due to cost between expansion and non-expansion states, though authors note that some of these findings may have been affected by study design or data limitations. Other studies did not find changes associated with expansion in trouble or worry about paying medical bills. Two studies did not find improvements in disparities by race/ethnicity associated with expansion in measures of unmet care needs due to cost.812 813 814 815 816 817 818 819 820 821 822 823 824 825 826 827 828 829 830 831 832
Economic Effects
Studies find positive effects of Medicaid expansion on a range of economic measures (Figure 5). Economic effects of expansion include changes to payer mix and other impacts on hospitals and other providers; effects on state budgets and economies; Medicaid spending per enrollee; marketplace effects; and employment and labor market effects.
State Budgets and Economies
Analyses find effects of expansion on multiple state economic outcomes, including budget savings, revenue gains, and overall economic growth. These positive effects occurred despite Medicaid enrollment growth initially exceeding projections in many states and increases in total Medicaid spending, largely driven by increases in federal spending given the enhanced federal match rate for expansion population costs provided under the ACA (the federal share was 100% for 2014-2016). As of Summer 2019, most expansion states reported relying on general fund support to finance the state share of expansion costs, although some also use new or increased provider taxes/fees or savings accrued as a result of the expansion. While studies showed higher growth rates in total Medicaid spending (federal, state, and local) following initial expansion implementation in 2014 and 2015 compared to the previous few years, this growth rate slowed significantly beginning in 2016. There is limited research examining the fiscal effects at the federal level from the additional expenditures for the Medicaid expansion or the revenues to support that spending.833 834 835 836 837 838 839 840 841 842 843 844 845 846 847 848 849 850 851 852 853 854 855
- National research found that there were no significant increases in spending from state funds as a result of Medicaid expansion and no significant reductions in state spending on education, transportation, or other state programs as a result of expansion during FYs 2010-2015. During this period, the federal government paid for 100% of the cost expansion. State spending could rise as the federal matching for the expansion phases down to 90%.856
- Single-state studies in Louisiana and Montana showed that expansion resulted in large infusions of federal funds into the states’ economies and significant state savings. Louisiana studies showed increases in overall state and local tax receipts in 2017 and 2018. A study in Montana found positive financial effects for businesses due to infusion of federal dollars to fund health coverage for workers.857 858 859 860 861
Multiple studies suggest that Medicaid expansion resulted in state savings by offsetting state costs in other areas, including state costs related to behavioral health services and crime and the criminal justice system. For example, a study in Montana showed offsets for state SUD spending, a study in California showed reduced county safety-net spending, and a study in Michigan pointed to state savings for non-Medicaid health programs (including the state’s community mental health system, its Adult Benefit Waiver program, and spending on health care for prisoners), which, combined with increased tax revenue associated with expansion, resulted in net fiscal benefits expected through 2021. Limited research also indicates possible federal and state savings due to decreased SSI participation associated with expansion.862 863 864 865 866 867 868 869 870 871 872 873 874 875 876
Medicaid Spending Per Enrollee
Studies have found lower Medicaid spending per enrollee for the new ACA adult eligibility group compared to traditional Medicaid enrollees (including seniors and people with disabilities in some studies and excluding those populations in others) and that per enrollee costs for newly eligible adults have declined over time since initial implementation of the expansion.877 878 879 880 881 882 883 884
- One analysis found that in 2014, among those states reporting both spending and enrollment data, spending per enrollee for the new adult group was much lower than spending per enrollee for traditional Medicaid enrollees. Similarly, an analysis of 2012-2014 data from expansion states found that average monthly expenditures for newly eligible Medicaid enrollees were $180, 21% less than the $228 average for previously eligible enrollees.885 886
- A June 2017 study showed that per enrollee Medicaid spending declined in expansion states(-5.1%) but increased in non-expansion states (5.1%) between 2013 and 2014. Researchers attributed these trends to the ACA Medicaid expansion, which increased the share of relatively less expensive enrollees in the Medicaid beneficiary population mix in expansion states.887
Marketplace Effects
Studies suggest that Medicaid expansion supports the ACA Marketplaces and may help to lower Marketplace premiums. Two national studies showed that Marketplace premiums were significantly lower in expansion compared to non-expansion states, with estimates ranging from 7% lower in 2015 to 11-12% lower in a later study that looked at 2015-2018 data. Another study found that the state average plan liability risk score was higher in non-expansion than expansion states in 2015 (higher risk scores are associated with sicker state risk pools and likely translate to higher premiums). A study in Arkansas showed that the “private option” expansion has helped to boost the number of carriers offering Marketplace plans statewide, generated a younger and relatively healthy risk pool in the Marketplace, and contributed to a 2% drop in the average rate of Marketplace premiums between 2014 and 2015. A study of New Hampshire’s Premium Assistance Program (PAP) population (Medicaid expansion population enrolled in the Marketplace), however, showed higher medical costs for the PAP population compared to other Marketplace enrollees.888 889 890 891 892
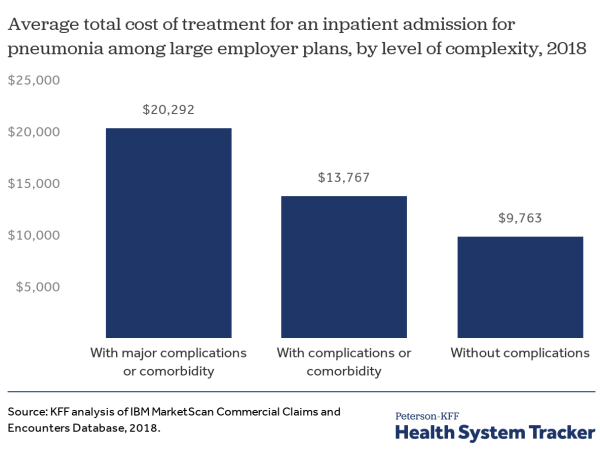
Impacts on Hospitals and Other Providers
Research shows that Medicaid expansions result in reductions in uninsured hospital, clinic, or other provider visits and uncompensated care costs, whereas providers in non-expansion states have experienced little or no decline in uninsured visits and uncompensated care. One study suggested that Medicaid expansion cut every dollar that a hospital in an expansion state spent on uncompensated care by 41 cents between 2013 and 2015, corresponding to a reduction in uncompensated care costs across all expansion states of $6.2 billion over that period.893 894 895 896 897 898 899 900 901 902 903 904 905 906 907 908 909 910 911 912 913 914 915 916 917 918 919 920 921 922 923 924 925 926 927 928 929 930 931 932 933 934 935 936 937 938 939 940 941 942 943 944 945 946 947 948 949 950 951 952 953 954 955 956 957 958 959 960 961 962 963 964 965 966 967 968 969 970 971 972 973 974 975 976
- Some studies point to changes in payer mix within emergency departments (EDs), specifically. Multiple studies found significant declines in uninsured ED visits and increases in Medicaid-covered ED visits following expansion implementation. In addition, one study found that expansion was associated with a 6.3% increase in ED physician reimbursement per visit in states that newly expanded coverage for adults from 0% to 138% FPL compared to non-expansion states.977 978 979 980 981 982 983 984 985 986 987 988 989 990
- Multiple studies found an association between expansion and significant increases in Medicaid coverage of patients/treatment at specialty substance use disorder (SUD) treatment facilities or treatment programs, with two studies also showing associated decreases in the probability that patients at these facilities were uninsured. An additional study found large shifts in sources of payment for SUD treatment among justice-involved individuals following Medicaid expansion in 2014, with significant increases in those reporting Medicaid as the source of payment.991 992 993 994 995
- Numerous recent studies found an association between expansion and payer mix (decreases in uninsured patients and increases in Medicaid patients) among patients hospitalized for certain specific conditions, including a range of cardiovascular conditions and operations; diabetes-related conditions; traumatic injury; and cancer surgery. Another analysis found expansion was associated with increases in Medicaid patient admissions for five of the eight types of cancer included in the study. Additional studies found that expansion was associated with increases in the proportion of transplant listings (for lung, liver, and pre-emptive kidney transplants, especially among racial and ethnic minorities) with Medicaid coverage, as well as increases in the proportion of received pre-emptive kidney transplantations that were covered by Medicaid. Two additional studies also found an increase in the chances of enrolling in Medicaid during post-liver transplant care. A study using birth certificate data found that expansion was associated with an increased proportion of deliveries covered by Medicaid, which was offset by a decrease in the proportion covered by private insurers or other payers but no change in the proportion of women who were uninsured.996 997 998 999 1000 1001 1002 1003 1004 1005 1006 1007 1008 1009 1010 1011 1012 1013 1014 1015 1016 1017 1018
- Studies found that expansion’s impact on payer mix and uncompensated care varied by the type and location of hospital. Two studies found larger decreases in uncompensated care and increases in Medicaid revenue among hospitals that treat a disproportionate share of low-income patients (DSH hospitals) compared to those that do not. A third study found no significant association of Medicaid expansion with changes in charge-to-cost ratio for certain surgical procedures in safety net hospitals vs. non-safety net hospitals, suggesting that safety net hospitals did not increase charges to private payers in response to expansion-related payer mix changes. A fourth study found that Medicaid expansion was significantly associated with increased Medicaid-covered discharges for rural hospitals but not for urban hospitals, but that urban hospitals saw significant reductions in uncompensated care costs while rural hospitals did not.1019 1020 1021 1022
Additional studies demonstrate that Medicaid expansion has significantly improved operating margins and financial performances for hospitals, other providers, and managed care organizations. A study published in January 2018 found that Medicaid expansion was associated with improved hospital financial performance and significant reductions in the probability of hospital closure, especially in rural areas and areas with higher pre-ACA uninsured rates. Another analysis found that expansion’s effects on margins were strongest for small hospitals, for-profit and non-federal-government-operated hospitals, and hospitals located in non-metropolitan areas. A third study found larger expansion-related improvements in operating margins for public (compared to nonprofit or for-profit) hospitals and rural (compared to non-rural) hospitals.1023 1024 1025 1026 1027 1028 1029 1030 1031 1032 1033 1034 1035
- A study of Ascension Health hospitals nationwide found that the decrease in uncompensated care costs for hospitals in expansion states was greater than the increase in Medicaid shortfalls between 2013 and 2014, whereas for hospitals in non-expansion states, the increase in Medicaid shortfalls exceeded the decrease in uncompensated care.1036
- A survey of Medicaid managed care organizations found that nearly two-thirds of plans in expansion states reported that the expansion has had a positive effect on their financial performance.1037
- Recent studies on the association between expansion and hospital costs or charges for specific conditions have found mixed results. One study found expansion was associated with increased diagnosis-related group charges for lupus hospitalizations, but another study found an association between expansion and reduced hospital costs for ambulatory care-sensitive conditions and a third found lower total index hospital charges within the homeless population in expansion states. An additional study found that hospital costs for minimally-invasive surgical care decreased for Medicaid-insured patients in expansion states, but increased for uninsured/self-pay patients.1038 1039 1040 1041
Some research suggests that savings to providers following expansion may be partially offset by increases in Medicaid shortfalls (the difference between what Medicaid pays and the cost of care for Medicaid patients). One recent study found that while expansion led to substantial reductions in hospitals’ uncompensated care costs, savings were offset somewhat by increased Medicaid payment shortfalls (increases were greater in expansion relative to non-expansion states).1042
Employment and Labor Market Effects
State-specific studies have documented significant job growth resulting from expansion. Studies in Louisiana found that in FY 2017, the injection of federal expansion funds created and supported 19,195 jobs (while creating and supporting personal earnings of $1.12 billion) in sectors throughout the economy and across the state; in FY 2018, continued federal healthcare spending supported 14,263 jobs and $889.0 million in personal earnings. A study in Colorado found that the state supported 31,074 additional jobs due to Medicaid expansion as of FY 2015-2016.1043 1044 1045 1046 1047
Some studies found expansion was linked to increased employment. National research found increases in the share of individuals with disabilities reporting employment and decreases in the share reporting not working due to a disability in Medicaid expansion states following expansion implementation, with no corresponding trends observed in non-expansion states; other research found a decline in participation in Supplemental Security Income, which requires people to demonstrate having a work-limiting disability and limits their allowable earned income. Another national study found evidence that for many of the demographic groups included in the analysis, expansion was associated with an increase in labor force participation and employment. The study also found a significant decrease in involuntary part-time work for both the full population sample and the sample of those with incomes at or below 138% FPL. A multi-state study found that by the fourth year of expansion, growth in total employment was 1.3 percentage points higher and employment growth in the health care sector was 3.2 percentage points higher in the expansion states studied than in non-expansion states.1048 1049 1050 1051 1052 1053
Multiple studies showed that expansion supported enrollees’ ability to work, seek work, or volunteer. Single-state studies in Ohio and Michigan showed that large percentages of expansion beneficiaries reported that Medicaid enrollment made it easier to seek employment (among those who were unemployed but looking for work) or continue working (among those who were employed). The Michigan study found that 69% of enrollees who were working said they performed better at work once they got expansion coverage. Another study found that 46% of primary care physicians surveyed in Michigan reported that Michigan’s Medicaid expansion had a positive impact on patients’ ability to work. An additional study in Michigan found that enrollees who reported improved health due to expansion were more likely to say that expansion coverage improved their ability to work and to seek a new job. In addition, a national study found an association between Medicaid expansion and volunteer work (both formal volunteering for organizations and informally helping a neighbor), with significant increases in volunteer work occurring among low-income individuals in expansion states in the post-expansion period (through 2015) but no corresponding increase in non-expansion states. The researchers connect this finding to previous literature showing an association between improvements in individual health and household financial stabilization and an increased likelihood of volunteering.1054 1055 1056 1057 1058
Some studies found no effects of expansion on some measures of employment or employee behavior; just one study found a negative effect of expansion on these measures. Measures in this area that showed no changes related to expansion in some studies include measures of employment rates, transitions from employment to non-employment, the rate of job switches, transitions from full- to part-time employment, labor force participation, usual hours worked per week, self-employment, and Supplemental Security Income applications. Authors of two studies note that expansion had no effect on employment and job-seeking despite concerns that the availability of free non-employer health insurance could be a disincentive to finding employment. A 2019 study comparing pairs of bordering counties in expansion and non-expansion states found that expansion was associated with a temporary 1.2% decrease in employment one year after implementation (although this effect did not persist two years after expansion) and no effect on wages at any point.1059 1060 1061 1062 1063 1064 1065 1066 1067 1068
Emerging Studies
Medicaid expansion was associated with a statistically significant decrease in reported cases of neglect for children younger than six years, but no significant change in rates of physical abuse for children under six. Another 2019 study found that Medicaid expansion was associated with increased undercounting of Medicaid enrollment in the American Community Survey. A 2017 study found that expansion was negatively associated with the prevalence of divorce among those ages 50-64 and infers that this likely indicates a reduction in medical divorce. A study found that expansion was not associated with increased migration from non-expansion states to expansion states in 2014, indicating that individuals did not migrate in order to gain access to Medicaid benefits. An additional group of studies suggests that Medicaid expansion may have significant effects on measures related to individuals’ political activity and views. Specifically, studies show associations between Medicaid expansion and increases in voter registration, ACA favorability, and gubernatorial approval. One study found that the increase in Medicaid enrollment following Medicaid expansion was associated with increases in voter turnout for U.S. House races in 2014 compared to 2012 (i.e., a reduction in the size of the usual midterm drop-off in turnout), but another study showed only weak evidence of a potential turnout effect of expansion in the 2014 election, and a consistent lack of any impact on turnout in 2016.1069 1070 1071 1072 1073 1074 1075 1076 1077
The authors thank Larisa Antonisse for her work on previous versions of this brief and assistance with reviewing recently published studies included in this update, as well as Eva Allen from The Urban Institute for her assistance with reviewing studies first included in an earlier version of this brief.
Appendix
| Coverage Effects of Expansion Impact of Expansion on Access to Care, Utilization, Affordability, and Health Outcomes |
Coverage Effects of Expansion
NATIONWIDE STUDIES (back to top)
- Jesse C. Baumgartner, Sara R. Collins, David C. Radley, and Susan L. Hayes, How the Affordable Care Act Has Narrowed Racial and Ethnic Disparities in Access to Health Care (The Commonwealth Fund, January 2020), https://www.commonwealthfund.org/publications/2020/jan/how-ACA-narrowed-racial-ethnic-disparities-access
- Anna L. Goldman and Benjamin D. Sommers, “Among Low-Income Adults Enrolled In Medicaid, Churning Decreased After The Affordable Care Act,” Health Affairs 39, no. 1 (January 2020): 85-93, https://doi.org/10.1377/hlthaff.2019.00378
- Jennifer M. Lobo et al., “Trends in Uninsured Rates Before and After Medicaid Expansion in Counties Within and Outside of the Diabetes Belt,” Diabetes Care Epub ahead of print (January 2020), https://doi.org/10.2337/dc19-0874
- Scott R. Sanders et al., “Infants Without Health Insurance: Racial/Ethnic and Rural/Urban Disparities in Infant Households’ Insurance Coverage,” PLoS One 15, no. 1 (January 2020), https://doi.org/10.1371/journal.pone.0222387
- Helmneh M. Sineshaw et al., “Association of Medicaid Expansion Under the Affordable Care Act With Stage at Diagnosis and Time to Treatment Initiation for Patients With Head and Neck Squamous Cell Carcinoma,” JAMA Otolaryngology–Head & Neck Surgery Epub ahead of print (January 2020), https://doi.org/10.1001/jamaoto.2019.4310
- Jean M. Abraham, Anne B. Royalty, and Coleman Drake, “The Impact of Medicaid Expansion on Employer Provision of Health Insurance,” International Journal of Health Economics and Management 19, no. 3-4 (December 2019): 317-340, https://doi.org/10.1007/s10754-018-9256-x
- Michel Boudreaux, James M. Noon, Brett Fried, and Joanne Pascale, “Medicaid Expansion and the Medicaid Undercount in the American Community Survey,” Health Services Research 54, no. 6 (December 2019): 1263-1272, https://doi.org/10.1111/1475-6773.13213
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553
- Hiroshi Gotanda, Gerald Kominski, and Yusuke Tsugawa, “Association Between the ACA Medicaid Expansions and Primary Care and Emergency Department Use During the First 3 Years,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05458-w
- Lizhong Peng, Xiaohui Guo, and Chad D. Meyerhoefer, “The Effects of Medicaid Expansion on Labor Market Outcomes: Evidence from Border Counties,” Health Economics Epub ahead of print (December 2019), https://doi.org/10.1002/hec.3976
- Kelsey L. Corrigan et al., “The Impact of the Patient Protection and Affordable Care Act on Insurance Coverage and Cancer-Directed Treatment in HIV-Infected Patients With Cancer in the United States,” Cancer (November 2019), https://doi.org/10.1002/cncr.32563
- Xuesong Han et al., “Changes in Noninsurance and Care Unaffordability Among Cancer Survivors Following the Affordable Care Act,” Journal of the National Cancer Institute Epub ahead of print (November 2019), https://doi.org/10.1093/jnci/djz218
- Claire E. Margerison et al., “Impacts of Medicaid Expansion on Health Among Women of Reproductive Age,” American Journal of Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.amepre.2019.08.019
- John J. Park et al., “Medicaid and Private Insurance Coverage for Low-Income Asian Americans, Native Hawaiians, and Pacific Islanders, 2010-16,” Health Affairs 38, no. 11 (November 2019): 1911-1917, https://doi.org/10.1377/hlthaff.2019.00316
- Jin Huang and Shirley L. Porterfield, “Changes in Health Insurance Coverage and Health Care Access as Teens with Disabilities Transition to Adulthood,” Disability and Health Journal 12, no. 4 (October 2019): 551-556, https://doi.org/10.1016/j.dhjo.2019.06.009
- Mark Olfson et al., “A National Survey of Trends in Health Insurance Coverage of Low-Income Adults Following Medicaid Expansion,” Journal of General Internal Medicine Epub ahead of print (October 2019), https://doi.org/10.1007/s11606-019-05409-5
- Jim P. Stimpson, Jessie Kemmick Pintor, and Fernando A. Wilson, “Association of Medicaid Expansion with Health Insurance Coverage by Marital Status and Sex,” PLoS One 14, no. 10 (October 2019), https://doi.org/10.1371/journal.pone.0223556
- Gracie Himmelstein, “Effect of the Affordable Care Act’s Medicaid Expansions on Food Security, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1243-1248, https://doi.org/10.2105/ajph.2019.305168
- Taylor Kelley, Renuka Tipirneni, and Helen Levy, “Changes in Veterans’ Coverage and Access to Care Following the Affordable Care Act, 2011-2017,” American Journal of Public Health 109, no. 9 (September 2019): 1233-1235, https://doi.org/10.2105/ajph.2019.305160
- Lindsay C. Kobayashi, Onur Altindag, Yulya Truskinovsky, and Lisa F. Berkman, “Effects of the Affordable Care Act Medicaid Expansion on Subjective Well-Being in the US Adult Population, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1236-1242, https://doi.org/10.2105/ajph.2019.305164
- Charles J. Courtemanche et al., The Impact of the ACA on Insurance Coverage Disparities After Four Years (National Bureau of Economic Research, Working Paper No. 26157, August 2019), http://www.nber.org/papers/w26157
- Lucie Schmidt, Lara Shore-Sheppard, and Tara Watson, The Impact of the ACA Medicaid Expansion on Disability Program Applications (National Bureau of Economic Research, Working Paper No. 26192, August 2019), http://www.nber.org/papers/w26192
- Laura Skopec, John Holahan, and Caroline Elmendorf, Health Insurance Coverage Declined for Nonelderly Americans Between 2016 and 2017, Primarily in States That Did Not Expand Medicaid (Washington, DC: The Urban Institute, August 2019), https://www.urban.org/research/publication/health-insurance-coverage-declined-nonelderly-americans-between-2016-and-2017-primarily-states-did-not-expand-medicaid
- Sri Lekha Tummalapalli, Samuel Leonard, Michelle M. Estrella, and Salomeh Keyhani, “The Effect of Medicaid Expansion on Self-Reported Kidney Disease,” Clinical Journal of American Society of Nephrology 14, no. 8 (August 2019): 1238-1240, https://doi.org/10.2215/cjn.02310219
- Sumit D. Agarwal, Anna L. Goldman, and Benjamin D. Sommers, “Blue-Collar Workers Had Greatest Insurance Gains After ACA Implementation,” Health Affairs 38, no. 7 (July 2019): 1140-1144, https://doi.org/10.1377/hlthaff.2018.05454
- Kevin N. Griffith, “Changes in Insurance Coverage and Access to Care for Young Adults in 2017,” Journal of Adolescent Health Epub ahead of print (July 2019), https://doi.org/10.1016/j.jadohealth.2019.05.020
- Sameed Ahmed Khatana et al., “Association of Medicaid Expansion With Cardiovascular Mortality,” JAMA Cardiology 4, no. 7 (July 2019): 671-679, https://doi.org/10.1001/jamacardio.2019.1651
- Sarah Miller, Sean Altekruse, Norman Johnson, and Laura R. Wherry, Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data (National Bureau of Economic Research, Working Paper No. 26081, July 2019), http://www.nber.org/papers/w26081
- Jim P. Stimpson et al., “Association of Medicaid Expansion With Health Insurance Coverage Among Persons With a Disability,” JAMA Network Open 2, no. 7 (July 2019), https://doi.org/10.1001/jamanetworkopen.2019.7136
- Ameen Barghi, Hugo Torres, Nancy Kressin, and Danny McCormick, “Coverage and Access for Americans with Cardiovascular Disease or Risk Factors After the ACA: a Quasi-experimental Study,” Journal of General Internal Medicine epub ahead of print (June 2019), https://link.springer.com/article/10.1007%2Fs11606-019-05108-1
- Emily Brown, Michelle Garrison, Hao Bao, Pingping Qu, Carole Jenny, and Ali Rowhani-Rahbar, “Assessment of Rates of Child Maltreatment in States With Medicaid Expansion vs States Without Medicaid Expansion,” JAMA Network Open 2, no. 6 (June 2019), https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2735758
- Ankit Agarwal, Aaron Katz, and Ronald Chen, “The Impact of the Affordable Care Act on Disparities in Private and Medicaid Insurance Coverage among Patients Under 65 with Newly Diagnosed Cancer,” International Journal of Radiation Oncology, Biology, Physics (May 2019), https://www.redjournal.org/article/S0360-3016(19)30783-7/pdf
- Robin Cohen, Emily Terlizzi, and Michael Martinez, Health Insurance Coverage: Early Release of Estimates from the National Health Interview Survey, 2018 (National Center for Health Statistics, May 2019), https://www.cdc.gov/nchs/data/nhis/earlyrelease/insur201905.pdf
- Sarah Miller and Laura Wherry, “Four Years Later: Insurance Coverage and Access to Care Continue to Diverge between ACA Medicaid Expansion and Non-Expansion States,” American Economic Association Papers and Proceedings 109 (May 2019): 327-333, https://www.aeaweb.org/articles?id=10.1257/pandp.20191046
- Joanna Woronkowicz, Aparna Soni, Seth Freedman, and Kosali Simon, “How Have Recent Health Insurance Expansions Affected Coverage Among Artist Occupations In The USA?,” Journal of Cultural Economics (May 2019), https://link.springer.com/article/10.1007/s10824-019-09352-5
- Abeer Alharbi, M. Mahmud Khan, Ronnie Horner, Heather Brandt, and Cole Chapman, “Impact Of Medicaid Coverage Expansion Under The Affordable Care Act On Mammography And Pap Tests Utilization Among Low-Income Women,” PLOS One (April 2019), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0214886
- Helen Levy, Thomas Buchmueller, and Sayeh Nikpay, “The Impact of Medicaid Expansion on Household Consumption,” Eastern Economic Journal 45, no. 1 (January 2019): 34-57, https://link.springer.com/article/10.1057/s41302-018-0124-7
- Colleen M. Carey, Sarah Miller, and Laura R. Wherry, “The Impact of Insurance Expansions on the Already Insured: The Affordable Care Act and Medicare,” National Bureau of Economic Research Working Paper Series No. 25153 (October 2018), https://www.nber.org/papers/w25153
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, and Ishtiaque Fazlul, “The Three‐Year Impact of the Affordable Care Act on Disparities in Insurance Coverage,” Health Services Research (October 2018), https://onlinelibrary.wiley.com/doi/10.1111/1475-6773.13077
- Hyunjung Lee and Frank Porell, “The Effect of the Affordable Care Act Medicaid Expansion on Disparities in Access to Care and Health Status,” Medical Care Research and Review epub ahead of print (October 2018), https://journals.sagepub.com/doi/abs/10.1177/1077558718808709?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=mcrd
- Jim Stimpson and Fernando Wilson, “Medicaid Expansion Improved Health Insurance Coverage For Immigrants, But Disparities Persist,” Health Affairs 37, no. 10 (October 2018), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.0181
- Christian Wolfe, Kathryn Rennie, and Christopher Truffer, 2017 Actuarial Report on the Financial Outlook for Medicaid (Office of the Actuary, Centers for Medicare and Medicaid Services, September 2018), https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/Downloads/MedicaidReport2017.pdf
- Xuesong Han, Robin Yabroff, Elizabeth Ward, Otis Brawley, and Ahmedin Jemal, “Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act,” JAMA Oncology 4, no. 12 (August 2018): 1713-1720, https://jamanetwork.com/journals/jamaoncology/article-abstract/2697226
- Mark Olfson, Melanie Wall, Colleen Barry, Christine Mauro, and Ramin Mojtabai, “Impact Of Medicaid Expansion On Coverage And Treatment Of Low-Income Adults With Substance Use Disorders,” Health Affairs 37, no. 8 (August 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.0124
- Jessica Vistnes and Joel Cohen, “Duration of Uninsured Spells For Nonelderly Adults Declined After 2014,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2017.1638
- Adele Shartzer, Frederic Blavin, and John Holohan, “Employer-Sponsored Insurance Stable For Low-Income Workers In Medicaid Expansion States,” Health Affairs 37, no. 4 (April 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1205
- Amy Davidoff et al., “Changes in Health Insurance Coverage Associated With the Affordable Care Act Among Adults With and Without a Cancer History: Population-based National Estimates,” Medical Care 56, no. 3 (March 2018), https://journals.lww.com/lww-medicalcare/Abstract/2018/03000/Changes_in_Health_Insurance_Coverage_Associated.5.aspx
- Kevin Callison and Paul Sicilian, “Economic Freedom and the Affordable Care Act: Medicaid Expansions and Labor Mobility by Race and Ethnicity,” Public Finance Review 46, no. 2 (March 2018), https://journals.sagepub.com/doi/abs/10.1177/1091142116668254
- Michael Cohen and William Schpero, “Household Immigration Status Had Differential Impact On Medicaid Enrollment In Expansion And Nonexpansion States,” Health Affairs 37, no. 3 (March 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.0978
- Joshua Clinton and Michael Sances, “The Politics of Policy: The Initial Mass Political Effects of Medicaid Expansion in the States,” American Political Science Review 112, no. 1 (February 2018): 167-185, https://www.cambridge.org/core/journals/american-political-science-review/article/politics-of-policy-the-initial-mass-political-effects-of-medicaid-expansion-in-the-states/246AA0F10B44EFD62A7B27C661730823
- Emily Johnston, Andrea Strahan, Peter Joski, Anne Dunlop, and E. Kathleen Adams, “Impacts of the Affordable Care Act’s Medicaid Expansion on Women of Reproductive Age,” Women’s Health Issues, 28, no. 2 (February 2018), http://www.whijournal.com/article/S1049-3867(17)30242-6/pdf
- Dahai Yue, Petra Rasmussen, and Ninez Ponce, “Racial/Ethnic Differential Effects of Medicaid Expansion on Health Care Access,” Health Services Research (February 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12834/abstract
- Frederic Blavin, Michael Karpman, Genevieve Kenney, and Benjamin Sommers, “Medicaid Versus Marketplace Coverage for Near-Poor Adults: Effects on Out-Of-Pocket Spending and Coverage,” Health Affairs 37 no. 2 (January 2018): 122-129 https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.1166
- Lindsey Dawson, Jennifer Kates, and Anthony Damico, The Affordable Care Act and Insurance Coverage Changes by Sexual Orientation (Washington, DC: Kaiser Family Foundation, January 2018), https://www.kff.org/disparities-policy/issue-brief/the-affordable-care-act-and-insurance-coverage-changes-by-sexual-orientation/
- Jennifer Haley, Robin Wang, Matthew Buettgens, and Genevieve Kenney, Health Insurance Coverage among Children Ages 3 and Younger and Their Parents in 2016 (The Urban Institute, January 2018), https://www.urban.org/research/publication/health-insurance-coverage-among-children-ages-3-and-younger-and-their-parents-2016
- Aparna Soni, Lindsay Sabik, Kosali Simon, and Benjamin Sommers, “Changes in Insurance Coverage Among Cancer Patients Under the Affordable Care Act,” Journal of the American Medical Association 4, no. 1 (January 2018): 122-124, https://jamanetwork.com/journals/jamaoncology/article-abstract/2657670?redirect=true&redirect=true
- Susan Hayes, Sara Collins, David Radley, and Douglas McCarthy, What’s at Stake: States’ Progress on Health Coverage and Access to Care, 2013-2016 (The Commonwealth Fund, December 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/dec/states-progress-health-coverage-and-access
- Ahmedin Jemal, Chun Chieh Lin, Amy Davidoff, and Xuesong Han, “Changes in Insurance Coverage and Stage at Diagnosis Among Nonelderly Patients with Cancer after the Affordable Care Act,” Journal of Clinical Oncology 35, no. 35 (December 2017), http://ascopubs.org/doi/pdf/10.1200/JCO.2017.73.7817
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830
- Michael Dworsky, Carrie Farmer, and Mimi Shen, Veterans’ Health Insurance Coverage Under the Affordable Care Act and Implications of Repeal for the Department of Veterans Affairs, (RAND Corporation, 2017), https://www.rand.org/pubs/research_reports/RR1955.html
- Samantha Artiga, Barbara DiPietro, and Petry Ubri, The Role of Medicaid and the Impact of the Medicaid Expansion for Veterans Experiencing Homelessness, (Washington, DC: Kaiser Family Foundation, October 2017), https://www.kff.org/medicaid/issue-brief/the-role-of-medicaid-and-impact-of-the-medicaid-expansion-for-veterans-experiencing-homelessness/
- Sunha Choi, Sungkyu Lee, and Jason Matejkowski, “The Effects of State Medicaid Expansion on Low-Income Individuals’ Access to Health Care: Multilevel Modeling,” Population Health Management epub ahead of print (September 2017), http://online.liebertpub.com/doi/abs/10.1089/pop.2017.0104
- Julie Hudson and Asako Moriya, “Medicaid Expansion for Adults Had Measureable ‘Welcome Mat’ Effects on Their Children,” Health Affairs, 36 no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0347
- Sharon Long, Lea Bart, Michael Karpman, Adele Shartzer, and Stephen Zuckerman, “Sustained Gains in Coverage, Access, and Affordability Under the ACA: A 2017 Update,” Health Affairs 36 no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0798
- Haley Moss, Laura Havrilesky, and Junzo Chino, “Insurance Coverage Among Women Diagnosed with a Gynecologic Malignancy Before and After Implementation of the Affordable Care Act,” Gynecologic Oncology 146, no. 3 (September 2017), https://www.ncbi.nlm.nih.gov/pubmed/28641821
- Kevin Griffith, Leigh Evans, and Jacob Bor, “The Affordable Care Act Reduced Socioeconomic Disparities in Health Care Access,” Health Affairs 36 no. 8 (August 2017), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0083
- Susan Hayes, Pamela Riley, David Radley, and Douglas McCarthy, Reducing Racial and Ethnic Disparities in Access to Care: Has the Affordable Care Act Made a Difference? (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/racial-ethnic-disparities-care
- Aaron Sojourner and Ezra Golberstein, “Medicaid Expansion Reduced Unpaid Medical Debt and Increased Financial Satisfaction,” Health Affairs (July 2017), https://www.healthaffairs.org/do/10.1377/hblog20170724.061160/full/
- MaryBeth Musumeci, Priya Chidambaram, and Molly O’Malley Watts, Key Questions About Medicaid Home and Community-Based Services Waiver Waiting Lists (Washington, DC: Kaiser Family Foundation, April 2019), https://www.kff.org/medicaid/issue-brief/key-questions-about-medicaid-home-and-community-based-services-waiver-waiting-lists/
- Rene Flores and Robert Vargas, “Medicaid Expansion And Ethnoracial Disparities In Health Insurance Coverage,” Journal of Ethnic and Migration Studies 43, no. 12 (June 2017), https://www.tandfonline.com/doi/full/10.1080/1369183X.2017.1323451?needAccess=true
- Sergio Gonzales and Benjamin Sommers, “Intra-Ethnic Coverage Disparities among Latinos and the Effects of Health Reform” Health Services Research epub ahead of print (June 2017), http://onlinelibrary.wiley.com/wol1/doi/10.1111/1475-6773.12733/full
- Abigail Barker, Kelsey Huntzberry, Timothy McBride, and Keith Mueller, Changing Rural and Urban Enrollment in State Medicaid Programs (Iowa City, IA: Rural Policy Research Institute, May 2017), https://cph.uiowa.edu/rupri/publications/policybriefs/2017/Changing%20Rural%20and%20Urban%20Enrollment%20in%20State%20Medicaid%20Programs.pdf
- Sandra Decker, Brandy Lipton, and Benjamin Sommers, “Medicaid Expansion Coverage Effects Grew in 2015 With Continued Improvements in Coverage Quality,” Health Affairs 36 no. 5 (May 2017): 819-825, http://content.healthaffairs.org/content/36/5/819.full
- Stacey McMorrow, Jason Gates, Sharon Long, and Genevieve Kenney, “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents,” Health Affairs 36 no. 5 (May 2017): 808-818, https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650
- George Wehby and Wei Lyu, “The Impact of the ACA Medicaid Expansions on Health Insurance Coverage through 2015 and Coverage Disparities by Age, Race/Ethnicity, and Gender” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12711/abstract
- Julia Foutz, Samantha Artiga, and Rachel Garfield, The Role of Medicaid in Rural America (Washington, DC: Kaiser Family Foundation, April 2017), http://kff.org/medicaid/issue-brief/the-role-of-medicaid-in-rural-america/
- Jennifer Haley, Genevieve Kenney, and Jason Gates, Veterans Saw Broad Coverage Gains Between 2013 and 2015 (Washington, DC: The Urban Institute, April 2017), http://www.urban.org/research/publication/veterans-saw-broad-coverage-gains-between-2013-and-2015
- Brandy Lipton, Sandra Decker, and Benjamin Sommers, “The Affordable Care Act Appears to Have Narrowed Racial and Ethnic Disparities in Insurance Coverage and Access to Care Among Young Adults” Medical Care Research and Review 76, no.1 (April 2017): 32–55, https://www.ncbi.nlm.nih.gov/pubmed/29148341
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Jason Gates, The ACA Medicaid Expansion Led to Widespread Reductions in Uninsurance Among Poor Childless Adults (The Urban Institute, April 2017), http://www.urban.org/sites/default/files/publication/89536/2001222-aca_medicaid_expansion_led_to_widespread_reductions_in_uninsurance_among_poor_childless_adults.pdf
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, Early Effects of the Affordable Care Act on Health Care Access, Risky Health Behaviors, and Self-Assessed Health (National Bureau of Economic Research, Working Paper no. 23269, March 2017), http://www.nber.org/papers/w23269
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890
- Kosali Simon, Aparna Soni, and John Cawley, “The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions” Journal of Policy Analysis and Management 36, no. 2 (March 2017), https://onlinelibrary.wiley.com/doi/abs/10.1002/pam.21972
- Jennifer Kates and Lindsey Dawson, Insurance Coverage Changes for People with HIV Under the ACA (Washington, DC: Kaiser Family Foundation, February 2017), http://kff.org/health-reform/issue-brief/insurance-coverage-changes-for-people-with-hiv-under-the-aca/
- Sandra Decker and Brandy Lipton, “Most Newly Insured People in 2014 Were Long-Term Uninsured,” Health Affairs 36 no. 1 (January 2017): 16-20, http://content.healthaffairs.org/content/36/1/16.full?sid=982b20c0-0a17-4dc4-a35a-b0302d4ec289
- Anne Martin et al., “National Health Spending: Faster Growth in 2015 As Coverage Expands and Utilization Increases,” Health Affairs 36 no. 1 (January 2017): 166-176, http://content.healthaffairs.org/content/36/1/166.full?sid=982b20c0-0a17-4dc4-a35a-b0302d4ec289
- Aparna Soni, Michael Hendryx, and Kosali Simon, “Medicaid Expansion under the Affordable Care Act and Insurance Coverage in Rural and Urban Areas,” The Journal of Rural Health epub ahead of print (January 2017), http://onlinelibrary.wiley.com/doi/10.1111/jrh.12234/full
- Tyler Winkelman, Edith Kieffer, Susan Goold, Jeffrey Morenoff, Kristen Cross, and John Ayanian, “Health Insurance Trends and Access to Behavioral Health Care Among Justice-Involved Individuals,” Journal of General Internal Medicine 31, no. 12 (December 2016): 1523-1529, https://www.ncbi.nlm.nih.gov/pubmed/27638837
- Kamyar Nasseh and Marko Vujicic, Early Impact of the Affordable Care Act’s Medicaid Expansion on Dental Care Use (Health Services Research, November 2016), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12606/full
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Jason Gates, “Marketplaces Helped Drive Coverage Gains in 2015; Affordability Problems Remained,” Health Affairs 35 no. 10 (October 2016): 1810-1815, http://content.healthaffairs.org/content/35/10/1810.full
- Robin Rudowitz, Allison Valentine, and Vernon Smith, Medicaid Enrollment and Spending Growth: FY 2016 & 2017 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, October 2016), http://kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2016-2017/
- Jessica Vistnes and Joel Cohen, “Gaining Coverage in 2014: New Estimates of Marketplace and Medicaid Transitions,” Health Affairs 35 no. 10 (October 2016): 1825-1829, http://content.healthaffairs.org/content/35/10/1825.full?sid=cc385dd5-9c95-4ee1-9c58-888408d49c54
- Kelsey Avery, Kenneth Finegold, and Amelia Whitman, Affordable Care Act Has Led to Historic, Widespread Increase in Health Insurance Coverage (Office of the Assistant Secretary for Planning and Evaluation, September 2016), https://aspe.hhs.gov/sites/default/files/pdf/207946/ACAHistoricIncreaseCoverage.pdf
- Helen Levy, Thomas Buchmueller, and Sayeh Nikpay, Health Reform and Health Insurance Coverage of Early Retirees (Ann Arbor, MI: University of Michigan Retirement Research Center Working Paper, September 2016), http://www.mrrc.isr.umich.edu/publications/papers/pdf/wp345.pdf
- Andrew Mulcahy, Christine Eibner, and Kenneth Finegold, “Gaining Coverage Through Medicaid Or Private Insurance Increased Prescription Use and Lowered Out-Of-Pocket Spending,” Health Affairs 35, no. 9 (September 2016), http://content.healthaffairs.org/content/early/2016/08/16/hlthaff.2016.0091.full
- Pauline Leung and Alexandre Mas, Employment Effects of the ACA Medicaid Expansions (Working Paper No. 22540, National Bureau of Economic Research, August 2016), http://www.nber.org/papers/w22540
- Office of the Assistant Secretary for Planning and Evaluation (ASPE), Impacts of the Affordable Care Act’s Medicaid Expansion on Insurance Coverage and Access to Care (Office of the Assistant Secretary for Planning and Evaluation, June 2016), https://aspe.hhs.gov/sites/default/files/pdf/205141/medicaidexpansion.pdf
- Brendan Saloner, Sachini Bandara, Emma McGinty, and Colleen Barry, “Justice-Involved Adults With Substance Use Disorders: Coverage Increased but Rates of Treatment Did Not in 2014,” Health Affairs 35 no. 6 (June 2016), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2016.0005
- Alanna Williamson, Larisa Antonisse, Jennifer Tolbert, Rachel Garfield, and Anthony Damico, ACA Coverage Expansions and Low-Income Workers (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2016), http://kff.org/report-section/aca-coverage-expansions-and-low-income-workers-issue-brief/
- Thomas Buchmueller, Zachary Levinson, Helen Levy, and Barbara Wolfe, “Effect of the Affordable Care Act on Racial and Ethnic Disparities in Health Insurance Coverage,” American Journal of Public Health (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27196653
- Sara Collins, Munira Gunja, Michelle Doty, and Sophie Beutel, Americans’ Experiences with ACA Marketplace and Medicaid Coverage: Access to Care and Satisfaction (The Commonwealth Fund, May 2016), http://www.commonwealthfund.org/publications/issue-briefs/2016/may/aca-tracking-survey-access-to-care-and-satisfaction
- Michael Karpman, Jason Gates, Genevieve Kenney, Stacey McMorrow, How Are Moms Faring under the Affordable Care Act? Evidence Through 2014, (The Urban Institute, May 2016), http://www.urban.org/research/publication/how-are-moms-faring-under-affordable-care-act-evidence-through-2014
- Genevieve Kenney, Jennifer Haley, Clare Pan, Victoria Lynch, and Matthew Buettgens, Children’s Coverage Climb Continues: Uninsurance and Medicaid/CHIP Eligibility and Participation Under the ACA, (Washington, DC: The Urban Institute, May 2016), http://www.urban.org/research/publication/childrens-coverage-climb-continues-uninsurance-and-medicaidchip-eligibility-and-participation-under-aca
- Jessica Sharac, Rachel Gunsalus, Chi Tran, Peter Shin, and Sara Rosenbaum, How are Migrant Health Centers and their Patients Faring Under the Affordable Care Act? (Geiger Gibson/RCHN Community Health Foundation Research Collaborative, The George Washington University Milken Institute of Public Health, May 2016), http://www.rchnfoundation.org/wp-content/uploads/2016/05/Migrant-Health-Centers-Patients-Under-Affordable-Care-Act.pdf
- John Cawley, Aparna Soni, and Kosali Simon, “Third Year of Survey Data Shows Continuing Benefits of Medicaid Expansions for Low-Income Childless Adults in the U.S.,” Journal of General Internal Medicine 33, no. 9 (September 2018): 1495-1497, https://link.springer.com/article/10.1007%2Fs11606-018-4537-0
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, and Daniela Zapata, Impacts of the Affordable Care Act on Health Insurance Coverage in Medicaid Expansion and Non-Expansion States (Working Paper No. 22182, The National Bureau of Economic Research, April 2016), http://www.nber.org/papers/w22182
- Molly Frean, Jonathan Gruber, and Benjamin Sommers, Premium Subsidies, the Mandate, and Medicaid Expansion: Coverage Effects of the Affordable Care Act (Working Paper No. 22213, National Bureau of Economic Research, April 2016), http://www.nber.org/papers/w22213?utm_campaign=ntw&utm_medium=email&utm_source=ntw
- Laura Wherry and Sarah Miller, “Early Coverage, Access, Utilization, and Health Effects Associated with the Affordable Care Act Medicaid Expansions: A Quasi-experimental Study,” Annals of Internal Medicine, Epub ahead of print (April 2016), http://annals.org/article.aspx?articleid=2513980
- Centers for Medicare and Medicaid Services, Monthly Medicaid and CHIP Application, Eligibility, Determination, and Enrollment Reports, (Centers for Medicare and Medicaid Services, March 2016), https://www.medicaid.gov/medicaid-chip-program-information/program-information/medicaid-and-chip-enrollment-data/medicaid-and-chip-application-eligibility-determination-and-enrollment-data.html
- Matt Warfield, Barbara DiPietro, and Samantha Artiga, How has the ACA Medicaid Expansion Affected Providers Serving the Homeless Population: Analysis of Coverage, Revenues, and Costs (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, March 2016), https://files.kff.org/attachment/issue-brief-how-has-the-aca-medicaid-expansion-affected-providers-serving-the-homeless-population
- Robin Rudowitz, Samantha Artiga, Anthony Damico, and Rachel Garfield, A Closer Look at the Remaining Uninsured Population Eligible for Medicaid and CHIP (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, February 2016), http://kff.org/uninsured/issue-brief/a-closer-look-at-the-remaining-uninsured-population-eligible-for-medicaid-and-chip/
- Christopher Truffer, Christian Wolfe, and Kathryn Rennie, 2016 Actuarial Report on the Financial Outlook for Medicaid, (Office of the Actuary, Centers for Medicare and Medicaid Services, 2016), https://www.cms.gov/Research-Statistics-Data-and Systems/Research/ActuarialStudies/Downloads/MedicaidReport2016.pdf
- Robert Kaestner, Bowen Garrett, Anuj Gangopadhyaya, and Caitlyn Fleming, Effects of ACA Medicaid Expansions on Health Insurance Coverage and Labor Supply (Working Paper No. 21836, National Bureau of Economic Research, December 2015), http://www.nber.org/papers/w21836
- Robin Rudowitz, Laura Snyder, and Vernon Smith, Medicaid Enrollment and Spending Growth: FY 2015 & 2016 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, October 2015), http://kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2015-2016/
- Jessica Smith and Carla Medalia, Health Insurance Coverage in the United States: 2014 (U.S. Census Bureau, September 2015), https://www.census.gov/content/dam/Census/library/publications/2015/demo/p60-253.pdf
- Benjamin Sommers, Munira Gunja, Kenneth Finegold, and Thomas Musco, “Changes in Self-Reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act,” The Journal of the American Medical Association 314 no. 4 (July 2015): 366-374, http://jama.jamanetwork.com/article.aspx?articleid=2411283&resultClick=3
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Nathaniel Anderson, “Uninsurance Among Young Adults Continues to Decline, Particularly in Medicaid Expansion States,” Health Affairs 34, no. 4 (April 2015): 616-620, http://content.healthaffairs.org/content/34/4/616.full
- Sara Collins, Petra Rasmussen, Michelle Doty, and Sophie Beutel The Rise in Health Care Coverage and Affordability Since Health Reform Took Effect: Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2014 (The Commonwealth Fund, January 2015), http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2015/jan/1800_collins_biennial_survey_brief.pdf?la=en
- Sharon Long, Michael Karpman, Adele Shartzer, Douglas Wissoker, Genevieve Kenney, Stephen Zuckerman, Nathaniel Anderson, and Katherine Hempstead, Taking Stock: Health Insurance Coverage under the ACA as of September 2014 (The Urban Institute, December 2014), http://hrms.urban.org/briefs/Health-Insurance-Coverage-under-the-ACA-as-of-September-2014.html
- Benjamin Sommers, Thomas Musco, Kenneth Finegold, Munira Gunja, Amy Burke, and Audrey McDowell, “Health Reform and Changes in Health Insurance Coverage in 2014” The New England Journal of Medicine 371 (August 2014): 867-874, http://www.nejm.org/doi/full/10.1056/NEJMsr1406753
MULTI-STATE STUDIES (back to top)
- Sarah H. Gordon, Benjamin D. Sommers, Ira B. Wilson, and Amal N. Trivedi, “Effects Of Medicaid Expansion On Postpartum Coverage And Outpatient Utilization,” Health Affairs 39, no. 1 (January 2020): 77-84, https://doi.org/10.1377/hlthaff.2019.00547
- John A. Graves et al., “Medicaid Expansion Slowed Rates of Health Decline for Low-Income Adults in Southern States,” Health Affairs 39, no. 1 (January 2020): 67-76, https://doi.org/10.1377/hlthaff.2019.00929
- Amandeep R. Mahal et al., “Early Impact of the Affordable Care Act and Medicaid Expansion on Racial and Socioeconomic Disparities in Cancer Care,” American Journal of Clinical Oncology Epub ahead of print (January 2020), https://doi.org/10.1097/coc.0000000000000588
- Shiho Kino and Ichiro Kawachi, “Can Health Literacy Boost Health Services Utilization in the Context of Expanded Access to Health Insurance?,” Health Education & Behavior Epub ahead of print (October 2019), https://doi.org/10.1177/1090198119875998
- Charles J. Courtemanche, James Marton, and Aaron Yelowitz, Medicaid Coverage across the Income Distribution under the Affordable Care Act (National Bureau of Economic Research, Working Paper No. 26145, August 2019), http://www.nber.org/papers/w26145
- Huabin Luo, Zhuo Chen, Lei Xu, and Ronny Bell, “Health Care Access and Receipt of Clinical Diabetes Preventive Care for Working-Age Adults With Diabetes in States With and Without Medicaid Expansion: Results from the 2013 and 2015 BRFSS,” Journal of Public Health Management and Practice 25, no. 4 (July/August 2019): 34-43, https://doi.org/10.1097/phh.0000000000000832
- Deborah Yip et al., “Association of Medicaid Expansion and Health Insurance with Receipt of Smoking Cessation Services and Smoking Behaviors in Substance Use Disorder Treatment,” The Journal of Behavioral Health Services & Research (July 2019), https://doi.org/10.1007/s11414-019-09669-1
- Sarah Gordon, Benjamin Sommers, Ira Wilson, Omar Galarraga, and Amal Trivedi, “The Impact of Medicaid Expansion on Continuous Enrollment: a Two State Analysis,” Journal of General Internal Medicine epub ahead of print (June 2019), https://link.springer.com/article/10.1007/s11606-019-05101-8
- Jose Mesquita-Neto, Peter Cmorej, Hassan Mouzaihem, Donald Weaver, Steve Kim, and Francis Macedo, “Disparities In Access To Cancer Surgery After Medicaid Expansion,” The American Journal of Surgery epub ahead of print (June 2019), https://www.sciencedirect.com/science/article/abs/pii/S0002961019306889
- Benjamin Sommers, Anna Goldman, Robert Blendon, E. John Orav, and Arnold Epstein, “Medicaid Work Requirements – Results from the First Year in Arkansas,” The New England Journal of Medicine Special Report (June 2019), https://www.nejm.org/doi/full/10.1056/NEJMsr1901772
- Vikki Wachino and Samantha Artiga, How Connecting Justice-Involved Individuals to Medicaid Can Help Address the Opioid Epidemic (Washington, DC: Kaiser Family Foundation, June 2019), https://www.kff.org/medicaid/issue-brief/how-connecting-justice-involved-individuals-to-medicaid-can-help-address-the-opioid-epidemic/
- Alina Denham and Peter Veazie, “Did Medicaid Expansion Matter in States with Generous Medicaid?” The American Journal of Managed Care 25, no. 3 (March 2019): 129-134, https://www.ajmc.com/journals/issue/2019/2019-vol25-n3/did-medicaid-expansion-matter-in-states-with-generous-medicaid
- Andrew Admon, Michael Sjoding, Sarah Lyon, John Ayanian, Theodore Iwashyna, and Colin Cooke, “Medicaid Expansion and Mechanical Ventilation in Asthma, Chronic Obstructive Pulmonary Disease, and Heart Failure,” Annals of the American Thoracic Society epub ahead of print (February 2019), https://www.atsjournals.org/doi/pdf/10.1513/AnnalsATS.201811-777OC
- Carrie Fry and Benjamin Sommers, “Effect of Medicaid Expansion on Health Insurance Coverage and Access to Care Among Adults With Depression,” Psychiatric Services 69, no. 11 (November 2018), https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201800181
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562
- Xuesong Han, Robin Yabroff, Elizabeth Ward, Otis Brawley, and Ahmedin Jemal, “Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act,” JAMA Oncology 4, no. 12 (August 2018): 1713-1720, https://jamanetwork.com/journals/jamaoncology/article-abstract/2697226
- Benjamin Sommers, Carrie Fry, Robert Blendon, and Arnold Epstein, “New Approaches in Medicaid: Work Requirements, Health Savings Accounts, and Health Care Access,” Health Affairs 37, no. 7 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2018.0331
- Emily Zylla, Colin Planalp, Elizabeth Lukanen, and Lynn Blewett, Section 1115 Medicaid Expansion Waivers: Implementation Experiences, (Medicaid and CHIP Payment and Access Commission, February 2018), https://www.macpac.gov/publication/section-1115-medicaid-expansion-waivers-implementation-experiences/
- Fumiko Chino, Gita Suneja, Haley Moss, S. Yousuf Zafar, Laura Havrilesky, and Junzo Chino, “Healthcare Disparities in Cancer Patients Receiving Radiation: Changes in Insurance Status After Medicaid Expansion Under the Affordable Care Act,” International Journal of Radiation Oncology (December 2017), http://www.sciencedirect.com/science/article/pii/S0360301617341883
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293
- MaryBeth Musumeci, Robin Rudowitz, Petry Ubri, and Elizabeth Hinton, An Early Look at Medicaid Expansion Waiver Implementation in Michigan and Indiana (Washington, DC: The Kaiser Family Foundation, January 2017), http://kff.org/medicaid/issue-brief/an-early-look-at-medicaid-expansion-waiver-implementation-in-michigan-and-indiana/
- Benjamin Sommers, Robert Blendon, E. John Orav, and Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420
- Benjamin Sommers, Rebecca Gourevitch, Bethany Maylone, Robert Blendon, and Arnold Epstein, “Insurance Churning Rates for Low-Income Adults Under Health Reform: Lower Than Expected but Still Harmful for Many,” Health Affairs 35 no. 10 (October 2016): 1816-1824, http://content.healthaffairs.org/content/35/10/1816.full?sid=f4835910-ffd0-4864-a76a-b4f207ccd018
- Stephen Berry et al., “Healthcare Coverage for HIV Provider Visits before and after Implementation of the Affordable Care Act,” Clinical Infectious Diseases, (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27143660
- Benjamin Sommers, Robert Blendon, and E. John Orav, “Both the ‘Private Option’ And Traditional Medicaid Expansions Improved Access To Care For Low-Income Adults,” Health Affairs 35, no. 1 (January 2016): 96-105, http://content.healthaffairs.org/content/35/1/96.abstract
- Michael Dworsky and Christine Eibner, The Effect of the 2014 Medicaid Expansion on Insurance Coverage for Newly Eligible Childless Adults (Santa Monica, CA: Rand Corporation, 2016), https://www.rand.org/pubs/research_reports/RR1736.html
- Samantha Artiga and Robin Rudowitz, How Have State Medicaid Expansion Decisions Affected the Experiences of Low-Income Adults? Perspectives from Ohio, Arkansas, and Missouri (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/medicaid/issue-brief/how-have-state-medicaid-expansion-decisions-affected-the-experiences-of-low-income-adults-perspectives-from-ohio-arkansas-and-missouri/
- Samantha Artiga, Jennifer Tolbert, and Robin Rudowitz, Year Two of the ACA Coverage Expansions: On-the-Ground Experiences from Five States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/health-reform/issue-brief/year-two-of-the-aca-coverage-expansions-on-the-ground-experiences-from-five-states/
- Stan Dorn, Norton Francis, Laura Snyder, and Robin Rudowitz, The Effects of the Medicaid Expansion on State Budgets: An Early Look in Select States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, March 2015), http://kff.org/medicaid/issue-brief/the-effects-of-the-medicaid-expansion-on-state-budgets-an-early-look-in-select-states/
- Barbara DiPietro, Samantha Artiga, and Alexandra Gates, Early Impacts of the Medicaid Expansion for the Homeless Population (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, November 2014), http://kff.org/uninsured/issue-brief/early-impacts-of-the-medicaid-expansion-for-the-homeless-population/
SINGLE STATE STUDIES (back to top)
- Nevada’s Medicaid Population, (Las Vegas, NV: The Guinn Center, September 2019), https://guinncenter.org/wp-content/uploads/2019/09/Guinn-Center-NV-Medicaid-Population-Characteristics-2019.pdf
- Dennis McCarty, Yifan Gu, John W. McIlveen, and Bonnie K. Lind, “Medicaid Expansion and Treatment for Opioid Use Disorders in Oregon: An Interrupted Time-Series Analysis,” Addiction Science & Clinical Practice 14 (August 2019), https://doi.org/10.1186/s13722-019-0160-6
- James A. Richardson, Jared J. Llorens, and Roy L. Heidelberg. Medicaid Expansion and the Louisiana Economy, 2018 and 2019 (Louisiana Department of Health, Prepared by Louisiana State University, August 2019), http://ldh.la.gov/assets/media/3and4.2019FinalReportMedicaidExpansionstudy.pdf
- MaryBeth Musumeci, Disability and Technical Issues Were Key Barriers to Meeting Arkansas’ Medicaid Work and Reporting Requirements in 2018 (Washington, DC: Kaiser Family Foundation, June 2019), https://www.kff.org/medicaid/issue-brief/disability-and-technical-issues-were-key-barriers-to-meeting-arkansas-medicaid-work-and-reporting-requirements-in-2018/
- Robin Rudowitz, MaryBeth Musumeci, and Cornelia Hall, February State Data for Medicaid Work Requirements in Arkansas (Washington, DC: Kaiser Family Foundation, March 2019), https://www.kff.org/medicaid/issue-brief/state-data-for-medicaid-work-requirements-in-arkansas/
- MaryBeth Musumeci, Robin Rudowitz, and Barbara Lyons, Medicaid Work Requirements in Arkansas: Experience and Perspectives of Enrollees (Washington, DC: Kaiser Family Foundation, December 2018), https://www.kff.org/medicaid/issue-brief/medicaid-work-requirements-in-arkansas-experience-and-perspectives-of-enrollees/
- MaryBeth Musumeci, Robin Rudowitz, and Cornelia Hall, An Early Look at Implementation of Medicaid Work Requirements in Arkansas (Washington, DC: Kaiser Family Foundation, October 2018), https://www.kff.org/medicaid/issue-brief/an-early-look-at-implementation-of-medicaid-work-requirements-in-arkansas/
- Stephen Barnes, Mike Henderson, Dek Terrell, and Stephanie Virgets, 2017 Louisiana Health Insurance Survey (Louisiana Department of Health, prepared by the Louisana State University E.J. Ourso College of Business, August 2018), http://ldh.la.gov/assets/media/2017-Louisiana-Health-Insurance-Survey-Report.pdf
- Seth Freedman, Lilliard Richardson, and Kosali Simon, “Learning From Waiver States: Coverage Effects Under Indiana’s HIP Medicaid Expansion,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1596
- Manatt Health, Medicaid Expansion: How It Affects Montana’s State Budget, Economy, and Residents (Montana Healthcare Foundation, prepared by Manatt Health, June 2018), https://mthcf.org/wp-content/uploads/2018/06/Manatt-MedEx_FINAL_6.1.18.pdf
- Louisiana Department of Health, Medicaid Expansion 2016/17 (Baton Rouge, Louisiana Department of Health, June 2017), http://dhh.louisiana.gov/assets/HealthyLa/Resources/MdcdExpnAnnlRprt_2017_WEB.pdf
- Eric Seiber and Micah Berman, “Medicaid Expansion and ACA Repeal: Evidence from Ohio,” American Journal of Public Health epub ahead of print (April 2017), http://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.2017.303722
- The Lewin Group, Healthy Indiana Plan 2.0: POWER Account Contribution Assessment, (The Lewin Group, prepared for the Indiana Family and Social Services Administration, March 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-POWER-acct-cont-assesmnt-03312017.pdf
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf
- Pennsylvania Department of Human Services, Medicaid Expansion Report, (Pennsylvania Department of Human Services, January 2017), http://www.dhs.pa.gov/cs/groups/webcontent/documents/document/c_257436.pdf
- The Lewin Group, Indiana Healthy Indiana Plan 2.0: Interim Evaluation Report (The Lewin Group, Prepared for Indiana Family and Social Services Administration, July 2016), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-interim-evl-rpt-07062016.pdf
- John Heintzman, Steffani Bailey, Jennifer DeVoe, Stuart Cowburn, Tanya Kapka, Truc-Vi Duong, and Miguel Marino, “In Low-Income Latino Patients, Post-Affordable Care Act Insurance Disparities May Be Reduced Even More than Broader National Estimates: Evidence from Oregon,” Journal of Racial and Ethnic Health Disparities (April 2016), http://www.ncbi.nlm.nih.gov/pubmed/27105630
- Joseph Benitez, Liza Creel, and J’Aime Jennings, “Kentucky’s Medicaid Expansion Showing Early Promise on Coverage and Access to Care,” Health Affairs (February 2016), http://content.healthaffairs.org/content/early/2016/02/16/hlthaff.2015.1294
- Arkansas Health Reform Legislative Task Force, Health Care Task Force Preliminary Report, (Arkansas Health Reform Legislative Task Force, December 2015), http://www.arkleg.state.ar.us/assembly/2015/Meeting%20Attachments/836/I14218/Task%20Force%20report%2012-17-15%20sent%20to%20Jill.pdf
- Jocelyn Guyer, Naomi Shine, MaryBeth Musumeci, and Robin Rudowitz, A Look at the Private Option in Arkansas (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, August 2015), http://kff.org/medicaid/issue-brief/a-look-at-the-private-option-in-arkansas/
- Michael McCue, “The Impact of Medicaid Expansion on Medicaid Focused Insurers in California,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 52 (July 2015), http://inq.sagepub.com/content/52/0046958015595960.full.pdf+html
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf
Impact of Expansion on Access to Care, Utilization, Affordability, and Health Outcomes
NATIONWIDE STUDIES (back to top)
- Jesse C. Baumgartner, Sara R. Collins, David C. Radley, and Susan L. Hayes, How the Affordable Care Act Has Narrowed Racial and Ethnic Disparities in Access to Health Care (The Commonwealth Fund, January 2020), https://www.commonwealthfund.org/publications/2020/jan/how-ACA-narrowed-racial-ethnic-disparities-access
- Anna L. Goldman and Benjamin D. Sommers, “Among Low-Income Adults Enrolled In Medicaid, Churning Decreased After The Affordable Care Act,” Health Affairs 39, no. 1 (January 2020): 85-93, https://doi.org/10.1377/hlthaff.2019.00378
- Nicole Kravitz-Wirtz et al., “Association of Medicaid Expansion With Opioid Overdose Mortality in the United States,” JAMA Network Open 3, no. 1 (January 2020), https://doi.org/10.1001/jamanetworkopen.2019.19066
- Helmneh M. Sineshaw et al., “Association of Medicaid Expansion Under the Affordable Care Act With Stage at Diagnosis and Time to Treatment Initiation for Patients With Head and Neck Squamous Cell Carcinoma,” JAMA Otolaryngology–Head & Neck Surgery Epub ahead of print (January 2020), https://doi.org/10.1001/jamaoto.2019.4310
- Jean M. Abraham, Anne B. Royalty, and Coleman Drake, “The Impact of Medicaid Expansion on Employer Provision of Health Insurance,” International Journal of Health Economics and Management 19, no. 3-4 (December 2019): 317-340, https://doi.org/10.1007/s10754-018-9256-x
- Susan L. Averett, Julie K. Smith, and Yang Wang, “Medicaid Expansion and Opioid Deaths,” Health Economics 28, no. 12 (December 2019): 1491-1496, https://doi.org/10.1002/hec.3945
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553
- Travis Donahoe et al., “The Affordable Care Act Medicaid Expansion and Smoking Cessation Among Low-Income Smokers,” American Journal of Preventive Medicine 57, no. 6 (December 2019): 203-210, https://doi.org/10.1016/j.amepre.2019.07.004
- Hiroshi Gotanda, Gerald Kominski, and Yusuke Tsugawa, “Association Between the ACA Medicaid Expansions and Primary Care and Emergency Department Use During the First 3 Years,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05458-w
- Kelsey L. Corrigan et al., “The Impact of the Patient Protection and Affordable Care Act on Insurance Coverage and Cancer-Directed Treatment in HIV-Infected Patients With Cancer in the United States,” Cancer (November 2019), https://doi.org/10.1002/cncr.32563
- Xuesong Han et al., “Changes in Noninsurance and Care Unaffordability Among Cancer Survivors Following the Affordable Care Act,” Journal of the National Cancer Institute Epub ahead of print (November 2019), https://doi.org/10.1093/jnci/djz218
- Claire E. Margerison et al., “Impacts of Medicaid Expansion on Health Among Women of Reproductive Age,” American Journal of Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.amepre.2019.08.019
- James A. Swartz and Susanny J. Beltran, “Prescription Opioid Availability and Opioid Overdose-Related Mortality Rates in Medicaid Expansion and Non-Expansion States,” Addiction 114, no. 11 (November 2019): 2016-2025, https://doi.org/10.1111/add.14741
- Yunwei Gai and John Marthinsen, “Medicaid Expansion, HIV Testing, and HIV-Related Risk Behaviors in the United States, 2010-2017,” American Journal of Public Health 109, no. 10 (October 2019): 1404-1412, https://doi.org/10.2105/ajph.2019.305220
- Jin Huang and Shirley L. Porterfield, “Changes in Health Insurance Coverage and Health Care Access as Teens with Disabilities Transition to Adulthood,” Disability and Health Journal 12, no. 4 (October 2019): 551-556, https://doi.org/10.1016/j.dhjo.2019.06.009
- Jusung Lee et al., “The Impact of Medicaid Expansion on Diabetes Management,” Diabetes Care Epub ahead of print (October 2019), https://doi.org/10.2337/dc19-1173
- Johanna Catherine Maclean, Michael F. Pesko, and Steven C. Hill, “Public Insurance Expansions and Smoking Cessation Medications,” Economic Inquiry 57, no. 4 (October 2019): 1798-1820, https://doi.org/10.1111/ecin.12794
- Chelsea L. Shover et al., “The Relationship of Medicaid Expansion to Psychiatric Comorbidity Care within Substance Use Disorder Treatment Programs,” Journal of Substance Abuse Treatment 105 (October 2019): 44-50, https://doi.org/10.1016/j.jsat.2019.07.012
- Naomi Zewde, Erica Eliason, Heidi Allen, and Tal Gross, “The Effects of the ACA Medicaid Expansion on Nationwide Home Evictions and Eviction-Court Initiations: United States, 2000-2016,” American Journal of Public Health 109, no. 10 (October 2019): 1379-1383, https://doi.org/10.2105/ajph.2019.305230
- Evan M. Chen et al., “Association of the Affordable Care Act Medicaid Expansion with Dilated Eye Examinations among the United States Population with Diabetes,” Ophthalmology Epub ahead of print (September 2019), https://doi.org/10.1016/j.ophtha.2019.09.010
- Taressa K. Fraze et al., “Prevalence of Screening for Food Insecurity, Housing Instability, Utility Needs, Transportation Needs, and Interpersonal Violence by US Physician Practices and Hospitals,” JAMA Network Open 2, no. 9 (September 2019), https://doi.org/10.1001/jamanetworkopen.2019.11514
- Gracie Himmelstein, “Effect of the Affordable Care Act’s Medicaid Expansions on Food Security, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1243-1248, https://doi.org/10.2105/ajph.2019.305168
- Taylor Kelley, Renuka Tipirneni, and Helen Levy, “Changes in Veterans’ Coverage and Access to Care Following the Affordable Care Act, 2011-2017,” American Journal of Public Health 109, no. 9 (September 2019): 1233-1235, https://doi.org/10.2105/ajph.2019.305160
- Lindsay C. Kobayashi, Onur Altindag, Yulya Truskinovsky, and Lisa F. Berkman, “Effects of the Affordable Care Act Medicaid Expansion on Subjective Well-Being in the US Adult Population, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1236-1242, https://doi.org/10.2105/ajph.2019.305164
- Sanders Korenman, Dahlia K. Remler, and Rosemary T. Hyson, “Medicaid Expansions and Poverty: Comparing Supplemental and Health-Inclusive Poverty Measures,” Social Service Review 93, no. 3 (September 2019): 429-483, https://doi.org/10.1086/705319
- Fredric Blavin, Impact of the Affordable Care Act’s Medicaid Expansion on Medicare Enrollees’ Access to Physician Services (Washington, DC: The Urban Institute, August 2019), https://www.urban.org/research/publication/effect-affordable-care-act-medicare-enrollees-access-physician-services
- Lisa Clemans-Cope, Victoria Lynch, Emma Winiski, and Marni Epstein, State Variation in Medicaid Prescriptions for Opioid Use Disorder from 2011 to 2018 (Washington, DC: The Urban Institute, August 2019), https://www.urban.org/research/publication/state-variation-medicaid-prescriptions-opioid-use-disorder-2011-2018
- Sri Lekha Tummalapalli, Samuel Leonard, Michelle M. Estrella, and Salomeh Keyhani, “The Effect of Medicaid Expansion on Self-Reported Kidney Disease,” Clinical Journal of American Society of Nephrology 14, no. 8 (August 2019): 1238-1240, https://doi.org/10.2215/cjn.02310219
- Kevin N. Griffith, “Changes in Insurance Coverage and Access to Care for Young Adults in 2017,” Journal of Adolescent Health Epub ahead of print (July 2019), https://doi.org/10.1016/j.jadohealth.2019.05.020
- Sameed Ahmed Khatana et al., “Association of Medicaid Expansion With Cardiovascular Mortality,” JAMA Cardiology 4, no. 7 (July 2019): 671-679, https://doi.org/10.1001/jamacardio.2019.1651
- Sarah Miller, Sean Altekruse, Norman Johnson, and Laura R. Wherry, Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data (National Bureau of Economic Research, Working Paper No. 26081, July 2019), http://www.nber.org/papers/w26081
- Ameen Barghi, Hugo Torres, Nancy Kressin, and Danny McCormick, “Coverage and Access for Americans with Cardiovascular Disease or Risk Factors After the ACA: a Quasi-experimental Study,” Journal of General Internal Medicine epub ahead of print (June 2019), https://link.springer.com/article/10.1007%2Fs11606-019-05108-1
- Nimish Valvi, Neomi Vin-Raviv, and Tomi Akinyemiju, “Current Smoking and Quit-Attempts Among US Adults Following Medicaid Expansion,” Preventive Medicine Reports epub ahead of print (June 2019), https://www.sciencedirect.com/science/article/pii/S2211335519300981
- Johanna Maclean and Brendan Saloner, “The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act,” Journal of Policy Analysis and Management 38, no. 2 (Spring 2019): 366-393, https://www.ncbi.nlm.nih.gov/pubmed/30882195
- Stacey Fedewa, K. Robin Yabroff, Robert Smith, Ann Goding Sauer, Xuesong Han, and Ahmedin Jemal, “Changes in Breast and Colorectal Cancer Screening After Medicaid Expansion Under the Affordable Care Act,” American Journal of Preventive Medicine epub ahead of print (May 2019), https://www.sciencedirect.com/science/article/pii/S0749379719301163
- Jevay Grooms and Alberto Ortega, “Examining Medicaid Expansion and the Treatment of Substance Use Disorders,” American Economic Association Papers and Proceedings 109 (May 2019): 187-192, https://www.aeaweb.org/articles?id=10.1257/pandp.20191090
- Nathalie Huguet et al., “Cervical And Colorectal Cancer Screening Prevalence Before And After Affordable Care Act Medicaid Expansion,” Preventative Medicine (May 2019), https://doi.org/10.1016/j.ypmed.2019.05.003
- Sarah Miller and Laura Wherry, “Four Years Later: Insurance Coverage and Access to Care Continue to Diverge between ACA Medicaid Expansion and Non-Expansion States,” American Economic Association Papers and Proceedings 109 (May 2019): 327-333, https://www.aeaweb.org/articles?id=10.1257/pandp.20191046
- Gary Pickens et al., “Changes In Hospital Service Demand, Cost, And Patient Illness Severity Following Health Reform,” Health Services Research (May 2019), https://doi.org/10.1111/1475-6773.13165
- Matthew Present, Aviva Nathan, Sandra Ham, Robert Sargis, Michael Quinn, and Elbert Huang, “The Impact of the Affordable Care Act Medicaid Expansion on Type 2 Diabetes Diagnosis and Treatment: A National Survey of Physicians,” Journal of Community Health epub ahead of print (May 2019), https://link.springer.com/article/10.1007%2Fs10900-019-00637-6
- Abeer Alharbi, M. Mahmud Khan, Ronnie Horner, Heather Brandt, and Cole Chapman, “Impact Of Medicaid Coverage Expansion Under The Affordable Care Act On Mammography And Pap Tests Utilization Among Low-Income Women,” PLOS One (April 2019), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0214886
- Christina Andrews et al., “Medicaid Coverage In Substance Use Disorder Treatment After The Affordable Care Act,” Journal of Substance Abuse Treatment epub ahead of print (April 2019), https://www.sciencedirect.com/science/article/pii/S0740547218305750
- Clare Brown et al., “Association of State Medicaid Expansion Status With Low Birth Weight and Preterm Birth” Journal of the American Medical Association 321, no. 16 (April 2019), https://jamanetwork.com/journals/jama/fullarticle/2731179
- Richard Frank and Carrie Fry, “The Impact of Expanded Medicaid Eligibility on Access To Naloxone,” Addiction epub ahead of print (April 2019), https://onlinelibrary.wiley.com/doi/abs/10.1111/add.14634
- Ramin Mojtabai, Christine Mauro, Melanie Wall, Colleen Barry, and Mark Olfson, “The Affordable Care Act and Opioid Agonist Therapy for Opioid Use Disorder,” Psychiatry Online (April 2019), https://doi.org/10.1176/appi.ps.201900025
- Benjamin Cher, Nancy Morden, and Ellen Meara, “Medicaid Expansion and Prescription Trends: Opioids, Addiction Therapies, and Other Drugs,” Medical Care 57, no. 3 (March 2019): 208-212, https://journals.lww.com/lww-medicalcare/fulltext/2019/03000/Medicaid_Expansion_and_Prescription_Trends_.6.aspx
- Lisa Clemans-Cope, Marni Epstein, Victoria Lynch, and Emma Winiski, Rapid Growth in Medicaid Spending and Prescriptions to Treat Opioid Use Disorder and Opioid Overdose from 2010 to 2017 (Washington, DC: The Urban Institute, March 2019), https://www.urban.org/sites/default/files/publication/99798/rapid_growth_in_medicaid_spending_and_prescriptions_to_treat_opioid_use_disorder_and_opioid_overdose_from_2010_to_2017_2.pdf
- Robert Sandstrom, “Increased Utilization of Ambulatory Occupational Therapy and Physical Therapy After Medicaid Expansion” Archives of Physical Medicine and Rehabilitation epub ahead of print (March 2019), https://www.archives-pmr.org/article/S0003-9993(19)30161-3/fulltext
- Bernard Black, Alex Hollingsworth, Leticia Nunes, and Kosali Simon, The Effect of Health Insurance on Mortality: Power Analysis and What We Can Learn from the Affordable Care Act Coverage Expansions, (National Bureau of Economic Research, Working Paper Series No. 25568, February 2019), https://www.nber.org/papers/w25568
- Chad Cotti, Erik Nesson, and Nathan Tefft, “Impacts Of The ACA Medicaid Expansion On Health Behaviors: Evidence From Household Panel Data,” Health Economics 28, no. 2 (February 2019): 219-244, https://onlinelibrary.wiley.com/doi/pdf/10.1002/hec.3838
- J.W. Awori Hayanga et al., “Lung Transplantation and Affordable Care Act Medicaid Expansion in the Era of Lung Allocation Score” Transplant International epub ahead of print (February 2019), https://onlinelibrary.wiley.com/doi/pdf/10.1111/tri.13420
- Ausmita Ghosh, Kosali Simon, and Benjamin Sommers, “The Effect of Health Insurance on Prescription Drug Use Among Low-Income Adults: Evidence from Recent Medicaid Expansions,” Journal of Health Economics 63 (January 2019): 64-80, https://www.sciencedirect.com/science/article/pii/S0167629617300206
- De-Chih Lee, Leiyu Shi, and Hailun Liang, “Primary Care Utilization And Clinical Quality Performance: A Comparison Between Health Centres In Medicaid Expansion States And Non-Expansion States,” Journal of Health Services Research & Policy 24, no. 1 (January 2019): 19-24, https://journals.sagepub.com/doi/abs/10.1177/1355819618788592
- Helen Levy, Thomas Buchmueller, and Sayeh Nikpay, “The Impact of Medicaid Expansion on Household Consumption,” Eastern Economic Journal 45, no. 1 (January 2019): 34-57, https://link.springer.com/article/10.1057/s41302-018-0124-7
- Ramin Mojtabai, Christine Mauro, Melanie Wall, Colleen Barry, and Mark Olfson, “Medication Treatment For Opioid Use Disorders In Substance Use Treatment Facilities,” Health Affairs 38, no. 1 (January 2019), https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.05162
- Rishi Wadhera et al., “Association of State Medicaid Expansion With Quality of Care and Outcomes for Low-Income Patients Hospitalized With Acute Myocardial Infarction,” JAMA Cardiology 4, no. 2 (January 2019): 120-127, https://jamanetwork.com/journals/jamacardiology/article-abstract/2720425?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamacardio.2018.4577
- Yasmin Zerhouni et al., “Effect of Medicaid Expansion on Colorectal Cancer Screening Rates,” Diseases of the Colon & Rectum 62, no. 1 (January 2019): 97-103, https://journals.lww.com/dcrjournal/Abstract/2019/01000/Effect_of_Medicaid_Expansion_on_Colorectal_Cancer.16.aspx
- Naomi Zewde and Christopher Wimer, “Antipoverty Impact Of Medicaid Growing With State Expansions Over Time,” Health Affairs 38, no. 1 (January 2019), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05155
- Shiho Kino and Ichiro Kawachi, “The Impact Of ACA Medicaid Expansion On Socioeconomic Inequality In Health Care Services Utilization,” PLoS ONE 13, no. 2 (December 2018), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0209935
- Shailender Swaminathan, Benjamin Sommers, Rebecca Thorsness, Rajnish Mehrotra, Yoojin Lee, and Amal Trivedi, “Association of Medicaid Expansion With 1-Year Mortality Among Patients With End-Stage Renal Disease,” Journal of the American Medical Association (JAMA) 320, no. 21 (December 2018): 2242-2250, https://jamanetwork.com/journals/jama/fullarticle/2710505?guestAccessKey=ea3a8641-320b-4afd-b96e-dc59fbd90b20&utm_source=TrendMD&utm_medium=cpc&utm_campaign=J_Am_Med_TrendMD_1&utm_content=olf&utm_term=102518
- Michael Hendryx and Juhua Luo, “Increased Cancer Screening for Low-income Adults Under the Affordable Care Act Medicaid Expansion,” Medical Care 56, no. 11 (November 2018): 944-949, https://www.ingentaconnect.com/content/wk/mcar/2018/00000056/00000011/art00009
- Elham Mahmoudi, Alicia Cohen, Jason Buxbaum, Caroline Richardson, and Wassim Tarraf, “Gaining Medicaid Coverage During ACA Implementation: Effects on Access to Care and Preventive Services,” Journal of Health Care for the Poor and Underserved 29, no. 4 (November 2018): 1472-1487, https://muse.jhu.edu/article/708253
- Hyunjung Lee and Frank Porell, “The Effect of the Affordable Care Act Medicaid Expansion on Disparities in Access to Care and Health Status,” Medical Care Research and Review epub ahead of print (October 2018), https://journals.sagepub.com/doi/abs/10.1177/1077558718808709?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=mcrd
- Xuesong Han, Robin Yabroff, Elizabeth Ward, Otis Brawley, and Ahmedin Jemal, “Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act,” JAMA Oncology 4, no. 12 (August 2018): 1713-1720, https://jamanetwork.com/journals/jamaoncology/article-abstract/2697226
- Rebecca Myerson, Tianyi Lu, Ivy Tonnu-Mihara, and Elbert Huang, “Medicaid Eligibility Expansions May Address Gaps In Access To Diabetes Medications,” Health Affairs 37, no. 8 (August 2018), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.0154
- Mark Olfson, Melanie Wall, Colleen Barry, Christine Mauro, and Ramin Mojtabai, “Impact Of Medicaid Expansion On Coverage And Treatment Of Low-Income Adults With Substance Use Disorders,” Health Affairs 37, no. 8 (August 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.0124
- Hannah Neprash, Anna Zink, Joshua Gray, and Katherine Hempstead, “Physicians’ Participation In Medicaid Increased Only Slightly Following Expansion” Health Affairs 37, no. 7 (July 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1085
- Hilary Barnes, Michael Richards, Matthew McHugh, and Grant Martsolf, “Rural And Nonrural Primary Care Physician Practices Increasingly Rely On Nurse Practitioners,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1158
- Megan Cole, Brad Wright, Ira Wilson, Omar Gallarraga, and Amal Trivedi, “Medicaid Expansion And Community Health Centers: Care Quality And Service Use Increased For Rural Patients” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1542
- Angelica Meinhofer and Allison Witman, “The Role Of Health Insurance On Treatment For Opioid Use Disorders: Evidence From The Affordable Care Act Medicaid Expansion,” Journal of Health Economics 60 (June 2018): 177-197, https://www.sciencedirect.com/science/article/abs/pii/S0167629617311530
- Rishi Wadhera et al., “Association of the Affordable Care Act’s Medicaid Expansion With Care Quality and Outcomes for Low-Income Patients Hospitalized With Heart Failure,” Circulation: Cardiovascular Quality and Outcomes 11, no. 7 (June 2018), https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.118.004729
- Alana Sharp, Austin Jones, Jennifer Sherwood, Oksana Kutsa, Brian Honermann, and Gregorio Millett, “Impact of Medicaid Expansion on Access to Opioid Analgesic Medications and Medication-Assisted Treatment,” American Journal of Public Health 108, no. 5 (May 2018): 642-648, https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2018.304338?journalCode=ajph
- Rachel Garfield, Elizabeth Hinton, Elizabeth Cornachione, and Cornelia Hall, Medicaid Managed Care Plans and Access to Care: Results from the Kaiser Family Foundation 2017 Survey of Medicaid Managed Care Plans (Washington, DC: Kaiser Family Foundation, March 2018), https://www.kff.org/medicaid/report/medicaid-managed-care-plans-and-access-to-care-results-from-the-kaiser-family-foundation-2017-survey-of-medicaid-managed-care-plans
- Sara Rosenbaum, Jennifer Tolbert, Jessica Sharac, Peter Shin, Rachel Gunsalus, and Julia Zur, Community Health Centers: Growing Importance in a Changing Health Care System (Washington, DC: Kaiser Family Foundation, March 2018), https://www.kff.org/medicaid/issue-brief/community-health-centers-growing-importance-in-a-changing-health-care-system/
- Nicolas Ajkay et al, “Early Impact of Medicaid Expansion and Quality of Breast Cancer Care in Kentucky,” Journal of the American College of Surgeons, epub ahead of print, February 2018, https://www.sciencedirect.com/science/article/pii/S107275151830022X
- Emily Johnston, Andrea Strahan, Peter Joski, Anne Dunlop, and E. Kathleen Adams, “Impacts of the Affordable Care Act’s Medicaid Expansion on Women of Reproductive Age,” Women’s Health Issues, 28, no. 2 (February 2018), http://www.whijournal.com/article/S1049-3867(17)30242-6/pdf
- Dahai Yue, Petra Rasmussen, and Ninez Ponce, “Racial/Ethnic Differential Effects of Medicaid Expansion on Health Care Access,” Health Services Research (February 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12834/abstract
- Chintan Bhatt and Consuelo Beck-Sague, “Medicaid Expansion and Infant Mortality in the United States,” American Journal of Public Health 108, no. 4 (April 2018): 565-567, https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2017.304218
- Frederic Blavin, Michael Karpman, Genevieve Kenney, and Benjamin Sommers, “Medicaid Versus Marketplace Coverage for Near-Poor Adults: Effects on Out-Of-Pocket Spending and Coverage,” Health Affairs 37 no. 2 (January 2018): 122-129 https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.1166
- Anna Goldman, Steffie Woolhandler, and David Himmelstein, “Out-of-pocket Spending and Premium Contributions After Implementation of the Affordable Care Act,” Journal of the American Medical Association epub ahead of print (January 2018), https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2669908
- Andrew Loehrer et al., “Association of the Affordable Care Act Medicaid Expansion with Access to and Quality of Care for Surgical Conditions,” Journal of the American Medical Association Surgery, epub ahead of print (January 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2670459?redirect=true
- Susan Hayes, Sara Collins, David Radley, and Douglas McCarthy, What’s at Stake: States’ Progress on Health Coverage and Access to Care, 2013-2016 (The Commonwealth Fund, December 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/dec/states-progress-health-coverage-and-access
- Ahmedin Jemal, Chun Chieh Lin, Amy Davidoff, and Xuesong Han, “Changes in Insurance Coverage and Stage at Diagnosis Among Nonelderly Patients with Cancer after the Affordable Care Act,” Journal of Clinical Oncology 35, no. 35 (December 2017), http://ascopubs.org/doi/pdf/10.1200/JCO.2017.73.7817
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830
- Kenneth Brevoort, Daniel Grodzicki, and Martin Hackmann, Medicaid and Financial Health (National Bureau of Economic Research, Working Paper No. 24002, November 2017), http://www.nber.org/papers/w24002
- Tyler Winkelman and Virginia Chang, “Medicaid Expansion, Mental Health, and Access to Care Among Childless Adults With and Without Chronic Conditions,” Journal of General Internal Medicine epub ahead of print (November 2017), https://www.ncbi.nlm.nih.gov/pubmed/29181792
- Michael Dworsky, Carrie Farmer, and Mimi Shen, Veterans’ Health Insurance Coverage Under the Affordable Care Act and Implications of Repeal for the Department of Veterans Affairs, (RAND Corporation, 2017), https://www.rand.org/pubs/research_reports/RR1955.html
- Samantha Artiga, Barbara DiPietro, and Petry Ubri, The Role of Medicaid and the Impact of the Medicaid Expansion for Veterans Experiencing Homelessness, (Washington, DC: Kaiser Family Foundation, October 2017), https://www.kff.org/medicaid/issue-brief/the-role-of-medicaid-and-impact-of-the-medicaid-expansion-for-veterans-experiencing-homelessness/
- Kyle Caswell and Timothy Waidmann, The Affordable Care Act Medicaid Expansions and Personal Finance (Washington, DC: The Urban Institute, September 2017), https://www.urban.org/research/publication/affordable-care-act-medicaid-expansions-and-personal-finance
- Sunha Choi, Sungkyu Lee, and Jason Matejkowski, “The Effects of State Medicaid Expansion on Low-Income Individuals’ Access to Health Care: Multilevel Modeling,” Population Health Management epub ahead of print (September 2017), http://online.liebertpub.com/doi/abs/10.1089/pop.2017.0104
- Sharon Long, Lea Bart, Michael Karpman, Adele Shartzer, and Stephen Zuckerman, “Sustained Gains in Coverage, Access, and Affordability Under the ACA: A 2017 Update,” Health Affairs 36 no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0798
- Haley Moss, Laura Havrilesky, and Junzo Chino, “Insurance Coverage Among Women Diagnosed with a Gynecologic Malignancy Before and After Implementation of the Affordable Care Act,” Gynecologic Oncology 146, no. 3 (September 2017), https://www.ncbi.nlm.nih.gov/pubmed/28641821
- Sherry Glied, Ougni Chakraborty, and Therese Russo, How Medicaid Expansion Affected Out-of-Pocket Health Care Spending for Low-Income Families (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/medicaid-expansion-out-of-pocket-spending-low-income
- Kevin Griffith, Leigh Evans, and Jacob Bor, “The Affordable Care Act Reduced Socioeconomic Disparities in Health Care Access,” Health Affairs 36 no. 8 (August 2017), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0083
- Susan Hayes, Pamela Riley, David Radley, and Douglas McCarthy, Reducing Racial and Ethnic Disparities in Access to Care: Has the Affordable Care Act Made a Difference? (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/racial-ethnic-disparities-care
- Dmitry Tumin et al., “Medicaid Participation among Liver Transplant Candidates after the Affordable Care Act Medicaid Expansion” Journal of the American College of Surgeons 225, no. 2 (August 2017): 173-180.e2, https://www.journalacs.org/article/S1072-7515(17)30454-4/fulltext
- Jacqueline Fiore, The Impact of the Affordable Care Act’s Medicaid Expansion on Medicaid Spending by Health Care Service Category (Tulane University, July 2017), http://econ.tulane.edu/RePEc/pdf/tul1706.pdf
- Aaron Sojourner and Ezra Golberstein, “Medicaid Expansion Reduced Unpaid Medical Debt and Increased Financial Satisfaction,” Health Affairs (July 2017), https://www.healthaffairs.org/do/10.1377/hblog20170724.061160/full/
- Lisa Clemans-Cope, Victoria Lynch, Marni Epstein, and Genevieve Kenney, Medicaid Coverage of Effective Treatment for Opioid Use Disorder, (Washington, DC: The Urban Institute, June 2017), https://www.urban.org/sites/default/files/publication/90461/2001287_medicaid_coverage_of_effective_treatment_for_opioid_use_disorder.pdf
- Joseph Labrum et al., “Does Medicaid Insurance Confer Adequate Access to Adult Orthopaedic Care in the Era of the Patient Protection and Affordable Care Act?” Clinical Orthopaedics and Related Research 475 no. 6 (June 2017): 1527-1536, https://link.springer.com/article/10.1007%2Fs11999-017-5263-3
- Gary Pickens et al., “Changes in Hospital Inpatient Utilization Following Health Care Reform,” Health Services Research epub ahead of print (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28664983
- Stacey McMorrow, Jason Gates, Sharon Long, and Genevieve Kenney, “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents,” Health Affairs 36 no. 5 (May 2017): 808-818, https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650
- Brandy Lipton, Sandra Decker, and Benjamin Sommers, “The Affordable Care Act Appears to Have Narrowed Racial and Ethnic Disparities in Insurance Coverage and Access to Care Among Young Adults” Medical Care Research and Review 76, no.1 (April 2017): 32–55, https://www.ncbi.nlm.nih.gov/pubmed/29148341
- Johanna Maclean and Brendan Saloner, The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act (National Bureau of Economic Research Working Paper No. 23342, April 2017), http://www.nber.org/papers/w23342.pdf
- Astha Singhal, Peter Damiano, and Lindsay Sabik, “Medicaid Adult Dental Benefits Increase Use Of Dental Care, But Impact Of Expansion On Dental Services Use Was Mixed,” Health Affairs 36 no. 4 (April 2017): 723-732, http://content.healthaffairs.org/content/36/4/723.short
- Hefei Wen, Jason Hockenberry, Tyrone Borders, and Benjamin Druss, “Impact of Medicaid Expansion on Medicaid-covered Utilization of Buprenorphine for Opioid Use Disorder Treatment,” Medical Care 55 no. 4 (April 2017): 336-341, http://journals.lww.com/lww-medicalcare/Fulltext/2017/04000/Impact_of_Medicaid_Expansion_on_Medicaid_covered.5.aspx
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, Early Effects of the Affordable Care Act on Health Care Access, Risky Health Behaviors, and Self-Assessed Health (National Bureau of Economic Research, Working Paper no. 23269, March 2017), http://www.nber.org/papers/w23269
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890
- Kosali Simon, Aparna Soni, and John Cawley, “The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions” Journal of Policy Analysis and Management 36, no. 2 (March 2017), https://onlinelibrary.wiley.com/doi/abs/10.1002/pam.21972
- Craig Garthwaite, Tal Gross, Matthew Notowidigdo, and John Graves, “Insurance Expansion and Hospital Emergency Department Access: Evidence from the Affordable Care Act,” Annals of Internal Medicine 166 no. 3 (February 2017): 172-179, http://annals.org/aim/article/2593599/insurance-expansion-hospital-emergency-department-access-evidence-from-affordable-care
- Khadijah Breathett et al., “The Affordable Care Act Medicaid Expansion Correlated with Increased Heart Transplant Listings in African Americans but Not Hispanics or Caucasians,” JACC: Heart Failure 5 no. 2 (January 2017): 136-147, https://www.ncbi.nlm.nih.gov/pubmed/28109783
- Megan Cole, Omar Galarraga, Ira Wilson, Brad Wright, and Amal Trivedi, “At Federally Funded Health Centers, Medicaid Expansion was Associated with Improved Quality of Care,” Health Affairs 36 no. 1 (January 2017): 40-48, http://content.healthaffairs.org/content/36/1/40.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19
- Xinxin Han, Quian Luo, and Leighton Ku, “Medicaid Expansion and Grant Funding Increases Helped Improve Community Health Center Capacity,” Health Affairs 36 no. 1 (January 2017): 49-56, http://content.healthaffairs.org/content/36/1/49.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19
- Ausmita Ghosh, Kosali Simon, and Benjamin Sommers, The Effect of State Medicaid Expansions on Prescription Drug Use: Evidence from the Affordable Care Act (Working Paper No. 23044, National Bureau of Economic Research, January 2017), http://www.nber.org/papers/w23044?utm_campaign=ntw&utm_medium=email&utm_source=ntw
- Anne DiGiulio et al., “State Medicaid Expansion Tobacco Cessation Coverage and Number of Adult Smokers Enrolled in Expansion Coverage – United States, 2016,” Morbidity and Mortality Weekly Report 65, no. 48 (December 2016), https://www.cdc.gov/mmwr/volumes/65/wr/mm6548a2.htm
- Kamyar Nasseh and Marko Vujicic, Early Impact of the Affordable Care Act’s Medicaid Expansion on Dental Care Use (Health Services Research, November 2016), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12606/full
- James Kirby and Jessica Vistnes, “Access to Care Improved for People Who Gained Medicaid or Marketplace Coverage in 2014,” Health Affairs 35 no. 10 (October 2016): 1830-1834, http://content.healthaffairs.org/content/35/10/1830.full
- Jessica Vistnes and Joel Cohen, “Gaining Coverage in 2014: New Estimates of Marketplace and Medicaid Transitions,” Health Affairs 35 no. 10 (October 2016): 1825-1829, http://content.healthaffairs.org/content/35/10/1825.full?sid=cc385dd5-9c95-4ee1-9c58-888408d49c54
- Andrew Mulcahy, Christine Eibner, and Kenneth Finegold, “Gaining Coverage Through Medicaid Or Private Insurance Increased Prescription Use and Lowered Out-Of-Pocket Spending,” Health Affairs 35, no. 9 (September 2016), http://content.healthaffairs.org/content/early/2016/08/16/hlthaff.2016.0091.full
- Hefei Wen, Tyrone Borders, and Benjamin Druss, ”Number of Medicaid Prescriptions Grew, Drug Spending was Steady in Medicaid Expansion States,” Health Affairs 35, no. 12 (September 2016): 1604-1607, http://content.healthaffairs.org/content/35/9/1604.full
- Jesse M. Pines, Mark Zocchi, Ali Moghtaderi, Bernard Black, Steven A. Farmer, Greg Hufstetler, Kevin Klauer and Randy Pilgrim, “Medicaid Expansion In 2014 Did Not Increase Emergency Department Use But Did Change Insurance Payer Mix,” Health Affairs 35, no. 8 (August 2016), http://content.healthaffairs.org/content/35/8/1480.full
- Sara Collins, Munira Gunja, Michelle Doty, and Sophie Beutel, Americans’ Experiences with ACA Marketplace and Medicaid Coverage: Access to Care and Satisfaction (The Commonwealth Fund, May 2016), http://www.commonwealthfund.org/publications/issue-briefs/2016/may/aca-tracking-survey-access-to-care-and-satisfaction
- John Cawley, Aparna Soni, and Kosali Simon, “Third Year of Survey Data Shows Continuing Benefits of Medicaid Expansions for Low-Income Childless Adults in the U.S.,” Journal of General Internal Medicine 33, no. 9 (September 2018): 1495-1497, https://link.springer.com/article/10.1007%2Fs11606-018-4537-0
- Luojia Hu, Robert Kaestenr, Bhashkar Mazumder, Sarah Miller, and Ashley Wong, “The Effect of the Affordable Care Act Medicaid Expansions on Financial Wellbeing,” Journal of Public Economics 163 (July 2018): 99-112, https://www.sciencedirect.com/science/article/abs/pii/S0047272718300707
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Jason Gates, “Marketplaces Helped Drive Coverage Gains in 2015; Affordability Problems Remained,” Health Affairs 35 no. 10 (October 2016): 1810-1815, http://content.healthaffairs.org/content/35/10/1810.full
- Mary Anderson, Jeffrey Glasheen, Debra Anoff, “Impact of State Medicaid Expansion Status on Length of Stay and In-Hospital Mortality for General Medicine Patients at US Academic Medical Centers,” Journal of Hospital Medicine Epub ahead of print (August 2016), http://onlinelibrary.wiley.com/wol1/doi/10.1002/jhm.2649/citedby
- Laura Wherry and Sarah Miller, “Early Coverage, Access, Utilization, and Health Effects Associated with the Affordable Care Act Medicaid Expansions: A Quasi-experimental Study,” Annals of Internal Medicine, Epub ahead of print (April 2016), http://annals.org/article.aspx?articleid=2513980
- Josh Gray, Anna Zink, and Tony Dreyfus, Effects of the Affordable Care Act Through 2015, (athenaResearch and Robert Wood Johnson Foundation ACA View Report, March 2016), http://www.athenahealth.com/~/media/athenaweb/files/pdf/acaview_tracking_the_impact_of_health_care_reform
- Adele Shartzer, Sharon Long, and Nathaniel Anderson, “Access To Care and Affordability have Improved Following Affordable Care Act Implementation; Problems Remain,” Health Affairs (December 2015), http://content.healthaffairs.org/content/early/2015/12/14/hlthaff.2015.0755.full
- Peter Shin, Jessica Sharac, Julia Zur, Sara Rosenbaum, and Julia Paradise, Health Center Patient Trends, Enrollment Activities, and Service Capacity: Recent Experience in Medicaid Expansion and Non-Expansion States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, December 2015), http://kff.org/medicaid/issue-brief/health-center-patient-trends-enrollment-activities-and-service-capacity-recent-experience-in-medicaid-expansion-and-non-expansion-states/
- Benjamin Sommers, Munira Gunja, Kenneth Finegold, and Thomas Musco, “Changes in Self-Reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act,” The Journal of the American Medical Association 314 no. 4 (July 2015): 366-374, http://jama.jamanetwork.com/article.aspx?articleid=2411283&resultClick=3
- Harvey Kaufman, Zhen Chen, Vivian Fonseca, and Michael McPhaul, “Surge in Newly Identified Diabetes Among Medicaid Patients in 2014 Within Medicaid Expansion States Under the Affordable Care Act,” Diabetes Care 38, no. 5 (May 2015): 833, http://care.diabetesjournals.org/content/early/2015/03/19/dc14-2334.full.pdf+html
- IMS Institute for Healthcare Informatics, Medicines Use and Spending Shifts: A Review of the Use of Medicines in the US in 2014 IMS Institute for Healthcare Informatics, April 2015), http://www.imshealth.com/en/thought-leadership/ims-institute/reports/medicines-use-in-the-us-2014
- Josh Gray, Iyue Sung, and Stewart Richardson, Observations on the Affordable Care Act: 2014 (athenaResearch and Robert Wood Johnson Foundation ACA View Report, February 2015), http://www.athenahealth.com/~/media/athenaweb/files/pdf/acaview_year_end_2014.pdf
MULTI-STATE STUDIES (back to top)
- Emanuel Eguia et al., “The Impact of the Affordable Care Act Medicaid Expansion on Vascular Surgery,” Annals of Vascular Surgery Epub ahead of print (January 2020), https://doi.org/10.1016/j.avsg.2020.01.006
- Hawazin W. Elani, Ichiro Kawachi, and Benjamin D. Sommers, “Changes in Emergency Department Dental Visits after Medicaid Expansion,” Health Services Research Epub ahead of print (January 2020), https://doi.org/10.1111/1475-6773.13261
- Sarah H. Gordon, Benjamin D. Sommers, Ira B. Wilson, and Amal N. Trivedi, “Effects Of Medicaid Expansion On Postpartum Coverage And Outpatient Utilization,” Health Affairs 39, no. 1 (January 2020): 77-84, https://doi.org/10.1377/hlthaff.2019.00547
- John A. Graves et al., “Medicaid Expansion Slowed Rates of Health Decline for Low-Income Adults in Southern States,” Health Affairs 39, no. 1 (January 2020): 67-76, https://doi.org/10.1377/hlthaff.2019.00929
- Alexander T. Janke, Shooshan Danagoulian, Arjun K. Venkatesh, and Phillip D. Levy, “Medicaid Expansion and Resource Utilization in the Emergency Department,” The American Journal of Emergency Medicine Epub ahead of print (January 2020), https://doi.org/10.1016/j.ajem.2019.12.050
- Adam M. Almaguer et al., “Do Geographic Region, Medicaid Status, and Academic Affiliation Affect Access to Care Among Medicaid and Privately Insured Total Hip Arthroplasty Patients?,” Journal of Arthroplasty 34, no. 12 (December 2019): 2866-2871, https://doi.org/10.1016/j.arth.2019.07.030
- Mark Clapp et al., “Association of Medicaid Expansion With Coverage and Access to Care for Pregnant Women,” Obstetrics & Gynecology 134, no. 5 (November 2019): 1066-1074, https://doi.org/10.1097/aog.0000000000003501
- Afshin Ehsan et al., “Utilization of Left Ventricular Assist Devices in Vulnerable Adults Across Medicaid Expansion,” Journal of Surgical Research 243 (November 2019): 503-508, https://doi.org/10.1016/j.jss.2019.05.015
- Kelsie M. Gould et al., “Bariatric Surgery Among Vulnerable Populations: The Effect of the Affordable Care Act’s Medicaid Expansion,” Surgery 166, no. 5 (November 2019): 820-828, https://doi.org/10.1016/j.surg.2019.05.005
- Jesse M. Hinde et al., “Increasing Access to Opioid Use Disorder Treatment: Assessing State Policies and the Evidence Behind Them,” Journal of Studies on Alcohol and Drugs 80, no. 6 (November 2019): 693-697, https://doi.org/10.15288/jsad.2019.80.693
- Hefei Wen, Kenton J. Johnston, Lindsay Allen, and Teresa M. Waters, “Medicaid Expansion Associated With Reductions In Preventable Hospitalizations,” Health Affairs 38, no. 11 (November 2019): 1845-1849, https://doi.org/10.1377/hlthaff.2019.00483
- Mohammad Eslami et al., “Impact of Medicaid Expansion of the Affordable Care on the Outcomes of Lower Extremity Bypass for Patients With Peripheral Artery Disease in the Vascular Quality Initiative Database,” Annals of Surgery 270, no. 4 (October 2019): 647-655, https://doi.org/10.1097/sla.0000000000003521
- Shiho Kino and Ichiro Kawachi, “Can Health Literacy Boost Health Services Utilization in the Context of Expanded Access to Health Insurance?,” Health Education & Behavior Epub ahead of print (October 2019), https://doi.org/10.1177/1090198119875998
- Nadia Laniado, Avery R. Brow, Eric Tranby, and Victor M. Badner, “Trends in Non-Traumatic Dental Emergency Department Use in New York and New Jersey: A Look at Medicaid Expansion from Both Sides of the Hudson River,” Journal of Public Health Dentistry Epub ahead of print (October 2019), https://doi.org/10.1111/jphd.12343
- Elizabeth A. Brown et al., “The Impact of the ACA Medicaid Expansion on Access to Care and Hospitalization Charges for Lupus Patients,” Arthritis Care & Research Epub ahead of print (September 2019), https://doi.org/10.1002/acr.24080
- Craig Garthwaite et al., All Medicaid Expansions Are Not Created Equal: The Geography and Targeting of the Affordable Care Act (National Bureau of Economic Research, Working Paper No. 26289, September 2019), http://www.nber.org/papers/w26289
- Nathalie Huguet et al., “Following Uninsured Patients Through Medicaid Expansion: Ambulatory Care Use and Diagnosed Conditions,” Annals of Family Medicine 17, no. 4 (July/August 2019): 336-344, https://doi.org/10.1370/afm.2385
- Huabin Luo, Zhuo Chen, Lei Xu, and Ronny Bell, “Health Care Access and Receipt of Clinical Diabetes Preventive Care for Working-Age Adults With Diabetes in States With and Without Medicaid Expansion: Results from the 2013 and 2015 BRFSS,” Journal of Public Health Management and Practice 25, no. 4 (July/August 2019): 34-43, https://doi.org/10.1097/phh.0000000000000832
- Emanuel Eguia et al., “The Impact of the Affordable Care Act (ACA) Medicaid Expansion on Access to Minimally Invasive Surgical Care,” The American Journal of Surgery Epub ahead of print (July 2019), https://doi.org/10.1016/j.amjsurg.2019.07.003
- Deborah Yip et al., “Association of Medicaid Expansion and Health Insurance with Receipt of Smoking Cessation Services and Smoking Behaviors in Substance Use Disorder Treatment,” The Journal of Behavioral Health Services & Research (July 2019), https://doi.org/10.1007/s11414-019-09669-1
- Andrew Crocker et al., “Expansion Coverage And Preferential Utilization Of Cancer Surgery Among Racial And Ethnic Minorities And Low-Income Groups,” Surgery epub ahead of print (June 2019), https://www.surgjournal.com/article/S0039-6060(19)30198-9/fulltext
- Ramiro Manzano-Nunez et al., “Association of Medicaid Expansion Policy with Outcomes in Homeless Patients Requiring Emergency General Surgery,” World Journal of Surgery 43, no. 6 (June 2019): 1483-1489, https://link.springer.com/article/10.1007/s00268-019-04932-0
- Jose Mesquita-Neto, Peter Cmorej, Hassan Mouzaihem, Donald Weaver, Steve Kim, and Francis Macedo, “Disparities In Access To Cancer Surgery After Medicaid Expansion,” The American Journal of Surgery epub ahead of print (June 2019), https://www.sciencedirect.com/science/article/abs/pii/S0002961019306889
- Vikki Wachino and Samantha Artiga, How Connecting Justice-Involved Individuals to Medicaid Can Help Address the Opioid Epidemic (Washington, DC: Kaiser Family Foundation, June 2019), https://www.kff.org/medicaid/issue-brief/how-connecting-justice-involved-individuals-to-medicaid-can-help-address-the-opioid-epidemic/
- Hefei Wen, Adam S. Wilk, and Benjamin G. Druss, “Medicaid Acceptance by Psychiatrists Before and After Medicaid Expansion,” JAMA Psychiatry epub ahead of print (June 2019), https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2735109?resultClick=1
- Steffani Bailey et al., “Tobacco Cessation in Affordable Care Act Medicaid Expansion States Versus Non-expansion States,” Nicotine & Tobacco Research epub ahead of print (May 2019), https://academic.oup.com/ntr/advance-article-abstract/doi/10.1093/ntr/ntz087/5498071
- Rahul Ladhania, Amelia Haviland, Arvind Venkat, Rahul Telang, and Jesse Pines, “The Effect of Medicaid Expansion on the Nature of New Enrollees’ Emergency Department Use,” Medical Care Research and Review epub ahead of print (May 2019), https://journals.sagepub.com/doi/abs/10.1177/1077558719848270
- Andrew Admon, Thomas Valley, John Ayanian, Theodore Iwashyna, Colin Cooke, and Renuka Tipirneni, “Trends in Hospital Utilization After Medicaid Expansion,” Medical Care 57, no. 4 (April 2019): 312-317, https://journals.lww.com/lww-medicalcare/Abstract/publishahead/Brief_Report__Trends_in_Hospital_Utilization_After.98489.aspx
- Andrew Admon, Michael Sjoding, Sarah Lyon, John Ayanian, Theodore Iwashyna, and Colin Cooke, “Medicaid Expansion and Mechanical Ventilation in Asthma, Chronic Obstructive Pulmonary Disease, and Heart Failure,” Annals of the American Thoracic Society epub ahead of print (February 2019), https://www.atsjournals.org/doi/pdf/10.1513/AnnalsATS.201811-777OC
- Jenny Nguyen, Nidharshan Anandasivam, Daniel Cooperman, Richard Pelker, and Daniel Wiznia, “Does Medicaid Insurance Provide Sufficient Access to Pediatric Orthopedic Care Under the Affordable Care Act?,” Global Pediatric Health epub ahead of print (February 2019), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6381430/
- Jonathan Routh et al., “Early Impact of the Patient Protection and Affordable Care Act on Delivery of Children’s Surgical Care,” Clinical Pediatrics 58, no. 4 (January 2019) 453-460, https://journals.sagepub.com/doi/abs/10.1177/0009922818825156?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=cpja
- Cheryl Zogg et al., “Association of Medicaid Expansion With Access to Rehabilitative Care in Adult Trauma Patients,” JAMA Surgery epub ahead of print (January 2019), https://jamanetwork.com/journals/jamasurgery/article-abstract/2719270?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamasurg.2018.5177
- Cheryl Zogg et al., “Impact of Affordable Care Act Insurance Expansion on Pre-Hospital Access to Care: Changes in Adult Perforated Appendix Admission Rates after Medicaid Expansion and the Dependent Coverage Provision,” Journal of the American College of Surgeons 228, no. 1 (January 2019): 29-43, https://www.journalacs.org/article/S1072-7515(18)32078-7/fulltext
- Andrew Crocker et al., “The Affordable Care Act’s Medicaid Expansion And Utilization Of Discretionary Vs. Non-Discretionary Inpatient Surgery,” Surgery 164, no. 6 (December 2018): 1156-1161, https://www.sciencedirect.com/science/article/pii/S0039606018302186
- Carrie Fry and Benjamin Sommers, “Effect of Medicaid Expansion on Health Insurance Coverage and Access to Care Among Adults With Depression,” Psychiatric Services 69, no. 11 (November 2018), https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201800181
- James McDermott et al., “Affordable Care Act’s Medicaid Expansion and Use of Regionalized Surgery at High-Volume Hospitals,” Journal of the American College of Surgeons 227, no. 5 (November 2018): 507-520.e9, https://www.journalacs.org/article/S1072-7515(18)31993-8/abstract
- Emanuel Eguia et al., “Impact of the Affordable Care Act (ACA) Medicaid Expansion on Cancer Admissions and Surgeries,” Annals of Surgery 268, no. 4 (October 2018): 584-590, https://journals.lww.com/annalsofsurgery/Abstract/2018/10000/Impact_of_the_Affordable_Care_Act__ACA__Medicaid.6.aspx
- Manzilat Akande Peter Minneci, Katherine Deans, Henry Xiang, and Jennifer Cooper, “Association of Medicaid Expansion Under the Affordable Care Act With Outcomes and Access to Rehabilitation in Young Adult Trauma Patients,” JAMA Surgery 153, no. 8 (August 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2682872?widget=personalizedcontent&previousarticle=2719270
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562
- Ehimare Akhabue, Lindsay Pool, Clyde Yancy, Philip Greenland, and Donald Lloyd-Jones, “Association of State Medicaid Expansion With Rate of Uninsured Hospitalizations for Major Cardiovascular Events, 2009-2014,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2698077
- Brendan Saloner, Jonathan Levin, Hsien-Yen Chang, Christopher Jones, and G. Caleb Alexander, “Changes in Buprenorphine-Naloxone and Opioid Pain Reliever Prescriptions After the Affordable Care Act Medicaid Expansion,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2696873
- Benjamin Sommers, Carrie Fry, Robert Blendon, and Arnold Epstein, “New Approaches in Medicaid: Work Requirements, Health Savings Accounts, and Health Care Access,” Health Affairs 37, no. 7 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2018.0331
- Emily Zylla, Colin Planalp, Elizabeth Lukanen, and Lynn Blewett, Section 1115 Medicaid Expansion Waivers: Implementation Experiences (Medicaid and CHIP Payment and Access Commission, February 2018), https://www.macpac.gov/publication/section-1115-medicaid-expansion-waivers-implementation-experiences/
- Aparna Soni, Kosali Simon, John Cawley, and Lindsay Sabik, “Effect of Medicaid Expansions of 2014 on Overall and Early-Stage Cancer Diagnoses,” American Journal of Public Health epub ahead of print (December 2017), http://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2017.304166
- Paul Jacobs, Genevieve Kenney, and Thomas Selden, “Newly Eligible Enrollees In Medicaid Spend Less And Use Less Care Than Those Previously Eligible,” Health Affairs 36, no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0252
- Eric Charles et al., “Impact of Medicaid Expansion on Cardiac Surgery Volume and Outcomes,” The Annals of Thoracic Surgery (June 2017), http://www.annalsthoracicsurgery.org/article/S0003-4975(17)30552-0/pdf
- Jeremy Holzmacher et al., “Association of Expanded Medicaid Coverage with Hospital Length of Stay After Injury,” JAMA Surgery published online (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28658482
- United States Government Accountability Office (GAO), Medicaid Expansion: Behavioral Health Treatment Use in Selected States in 2014 (Washington, DC: GAO Report to Congressional Requesters, June 2017), https://www.gao.gov/assets/690/685415.pdf
- Nathalie Huguet et al., “Medicaid Expansion Produces Long-Term Impact on Insurance Coverage Rates in Community Health Centers,” Journal of Primary Care & Community Health epub ahead of print (May 2017), http://journals.sagepub.com/doi/full/10.1177/2150131917709403
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293
- Molly Candon et al., Primary Care Appointment Availability and the ACA Insurance Expansions (Philadelphia, PA: University of Pennsylvania Leonard Davis Institute of Health Economics, March 2017), https://ldi.upenn.edu/brief/primary-care-appointment-availability-and-aca-insurance-expansions
- Nirosha Mahendraratnam, Stacie Dusetzina, and Joel Farley, “Prescription Drug Utilization and Reimbursement Increased Following State Medicaid Expansion in 2014,” Journal of Managed Care & Specialty Pharmacy 23 no. 3 (March 2017): 355-363, http://www.jmcp.org/doi/10.18553/jmcp.2017.23.3.355
- MaryBeth Musumeci, Robin Rudowitz, Petry Ubri, and Elizabeth Hinton, An Early Look at Medicaid Expansion Waiver Implementation in Michigan and Indiana (Washington, DC: The Kaiser Family Foundation, January 2017), http://kff.org/medicaid/issue-brief/an-early-look-at-medicaid-expansion-waiver-implementation-in-michigan-and-indiana/
- Megan Hoopes, Heather Angier, Rachel Gold, Steffani Bailey, Nathalie Huguet, Miguel Marino, and Jennifer DeVoe, “Utilization of Community Health Centers in Medicaid Expansion and Nonexpansion States, 2013-2014,” Journal of Ambulatory Care Management 39 no. 4 (October 2016): 290-298, https://www.ncbi.nlm.nih.gov/pubmed/26765808
- Benjamin Sommers, Robert Blendon, E. John Orav, Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420
- Samantha Artiga, Robin Rudowitz, Jennifer Tolbert, Julia Paradise, and Melissa Majerol, Findings from the Field: Medicaid Delivery Systems and Access to Care in Four States in Year Three of the ACA (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, September 2016), http://kff.org/medicaid/issue-brief/findings-from-the-field-medicaid-delivery-systems-and-access-to-care-in-four-states-in-year-three-of-the-aca/
- Simon Basseyn, Brendan Saloner, Genevieve Kenney, Douglas Wissoker, Daniel Polsky, and Karin Rhodes, Primary Care Appointment Availability for Medicaid Patients: Comparing Traditional and Premium Assistance Plans, (Penn Leonard Davis Institute of Health Economics, July 2016), http://ldi.upenn.edu/brief/primary-care-appointment-availability-medicaid-patients-comparing-traditional-and-premium
- Jane Wishner, Patricia Solleveld, Robin Rudowitz, Julia Paradise, and Larisa Antonisse, A Look at Rural Hospital Closures and Implications for Access to Care: Three Case Studies (Washington, DC: Kaiser Commission on Medicaid and the Uninsured and The Urban Institute, July 2016), http://kff.org/medicaid/issue-brief/a-look-at-rural-hospital-closures-and-implications-for-access-to-care/
- Benjamin Sommers, Robert Blendon, and E. John Orav, “Both the ‘Private Option’ And Traditional Medicaid Expansions Improved Access To Care For Low-Income Adults,” Health Affairs 35, no. 1 (January 2016): 96-105, http://content.healthaffairs.org/content/35/1/96.abstract
- Samantha Artiga and Robin Rudowitz, How Have State Medicaid Expansion Decisions Affected the Experiences of Low-Income Adults? Perspectives from Ohio, Arkansas, and Missouri (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/medicaid/issue-brief/how-have-state-medicaid-expansion-decisions-affected-the-experiences-of-low-income-adults-perspectives-from-ohio-arkansas-and-missouri/
- Samantha Artiga, Jennifer Tolbert, and Robin Rudowitz, Year Two of the ACA Coverage Expansions: On-the-Ground Experiences from Five States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/health-reform/issue-brief/year-two-of-the-aca-coverage-expansions-on-the-ground-experiences-from-five-states/
- Government Accountability Office, Behavioral Health: Options for Low-Income Adults to Receive Treatment in Selected States (Washington, DC: Government Accountability Office, June 2015), http://www.gao.gov/assets/680/670894.pdf
- Barbara DiPietro, Samantha Artiga, and Alexandra Gates, Early Impacts of the Medicaid Expansion for the Homeless Population (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, November 2014), http://kff.org/uninsured/issue-brief/early-impacts-of-the-medicaid-expansion-for-the-homeless-population/
SINGLE STATE STUDIES (back to top)
- Susan Dorr Goold et al., “Primary Care, Health Promotion, and Disease Prevention with Michigan Medicaid Expansion,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05370-3
- Susannah Gibbs et al., “Evaluating the Effect of Medicaid Expansion on Access to Preventive Reproductive Care for Women in Oregon,” Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.ypmed.2019.105899
- Ann-Marie Rosland et al., “Diagnosis and Care of Chronic Health Conditions Among Medicaid Expansion Enrollees: a Mixed-Methods Observational Study,” Journal of General Internal Medicine 34, no. 11 (November 2019): 2549-2558, https://doi.org/10.1007/s11606-019-05323-w
- Heather Holderness et al., “Where Do Oregon Medicaid Enrollees Seek Outpatient Care Post-Affordable Care Act Medicaid Expansion?,” Medical Care 57, no. 10 (October 2019): 788-794, https://doi.org/10.1097/mlr.0000000000001189
- Charles A. Daly et al., “The Effects of Medicaid Expansion on Triage and Regional Transfer After Upper-Extremity Trauma,” The Journal of Hand Surgery 44, no. 9 (September 2019): 720-727, https://doi.org/10.1016/j.jhsa.2019.05.020
- John Scott et al., “Lifting the Burden: State Medicaid Expansion Reduces Financial Risk for the Injured,” Journal of Trauma and Acute Care Surgery Epub ahead of print (September 2019), https://doi.org/10.1097/ta.0000000000002493
- Renuka Tipirneni et al., “Association of Expanded Medicaid Coverage With Health and Job-Related Outcomes Among Enrollees With Behavioral Health Disorders,” Psychiatric Services Epub ahead of print (September 2019), https://doi.org/10.1176/appi.ps.201900179
- Dennis McCarty, Yifan Gu, John W. McIlveen, and Bonnie K. Lind, “Medicaid Expansion and Treatment for Opioid Use Disorders in Oregon: An Interrupted Time-Series Analysis,” Addiction Science & Clinical Practice 14 (August 2019), https://doi.org/10.1186/s13722-019-0160-6
- Mark L. Diana et al. Louisiana Medicaid Expansion and Access to Care (Louisiana Department of Health, Prepared by Tulane University, July 2019), http://ldh.la.gov/assets/media/AccesstoCareReport20132018final.pdf
- Tong Gan et al., “Impact of the Affordable Care Act on Colorectal Cancer Screening, Incidence, and Survival in Kentucky,” Journal of the American College of Surgeons 228, no. 4 (April 2019): 342-353.e1, https://www.journalacs.org/article/S1072-7515(19)30046-8/fulltext
- Brendan Saloner, Rachel Landis, Bradley Stein, and Colleen Barry, “The Affordable Care Act in the Heart of the Opioid Crisis: Evidence from West Virginia,” Health Affairs 38, no. 4 (April 2019), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05049
- Renuka Tipirneni et al., “Changes in Health and Ability to Work Among Medicaid Expansion Enrollees: a Mixed Methods Study,” Journal of General Internal Medicine 34, no. 2 (February 2019): 272-280, https://link.springer.com/article/10.1007/s11606-018-4736-8
- Neal Bhutiani, Brian Harbrecht, Charles Scoggins, and Matthew Bozeman, “Evaluating The Early Impact Of Medicaid Expansion On Trends In Diagnosis And Treatment Of Benign Gallbladder Disease In Kentucky,” The American Journal of Surgery (January 2019), https://www.americanjournalofsurgery.com/article/S0002-9610(18)30894-8/fulltext
- Mark Duggan, Atul Gupta, and Emilie Jackson, The Impact of the Affordable Care Act: Evidence from California’s Hospital Sector (National Bureau of Economic Research, working paper no. 25488, January 2019), https://www.nber.org/papers/w25488.pdf
- Sarah Miller, Luojia Hu, Robert Kaestner, Bhashkar Mazumder, and Ashley Wong, The ACA Medicaid Expansion in Michigan and Financial Health, (National Bureau of Economic Research, working paper no. 25053, September 2018), https://www.nber.org/papers/w25053.pdf
- Michelle Moniz et al., “Association of Access to Family Planning Services With Medicaid Expansion Among Female Enrollees in Michigan,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2698636
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf
- Susan Dorr Goold et al., “Primary Care Clinicians’ Views About the Impact of Medicaid Expansion in Michigan: A Mixed Methods Study,” Journal of General Internal Medicine 33, no. 8 (June 2018): 1307-1316, https://link.springer.com/article/10.1007/s11606-018-4487-6
- Manatt Health, Medicaid Expansion: How It Affects Montana’s State Budget, Economy, and Residents, (Manatt Health, prepared for the Montana Healthcare Foundation, June 2018), https://mthcf.org/wp-content/uploads/2018/06/Manatt-MedEx_FINAL_6.1.18.pdf
- Shannon McConville, Maria Raven, Sarah Sabbagh, and Renee Hsia, “Frequent Emergency Department Users: A Statewide Comparison Before And After Affordable Care Act Implementation,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0784
- Donald Likosky, Devraj Sukul, Milan Seth, Chang He, Hitlander Gurm, and Richard Prager, “The Association Between Medicaid Expansion and Cardiovascular Interventions: The Michigan Experience,” Journal of the American College of Cardiology 71, no. 9 (March 2018): 1050-1051, https://www.sciencedirect.com/science/article/pii/S0735109718300056?via%3Dihub
- Brad Wright et al., “Completion of Requirements in Iowa’s Medicaid Expansion Premium Disincentive Program, 2014–2015,” American Journal of Public Health 108, no. 2 (February 2018): 219-223, http://ajph.aphapublications.org/doi/full/10.2105/AJPH.2017.304178
- Eili Klein et al., “The Effect of Medicaid Expansion on Utilization in Maryland Emergency Departments,” Annals of Emergency Medicine epub ahead of print (June 2017), http://www.annemergmed.com/article/S0196-0644(17)30784-9/pdf
- Louisiana Department of Health, Medicaid Expansion 2016/17 (Baton Rouge, Louisiana Department of Health, June 2017), http://dhh.louisiana.gov/assets/HealthyLa/Resources/MdcdExpnAnnlRprt_2017_WEB.pdf
- Aabha Sharma, Scott Dresden, Emilie Powell, Raymond Kang, Joe Feinglass, “Emergency Department Visits and Hospitalizations for the Uninsured in Illinois Before and After Affordable Care Act Insurance Expansion,” Journal of Community Health 42 no. 3 (June 2017): 591-597, https://link.springer.com/article/10.1007/s10900-016-0293-4
- Natoshia Askelson, Brad Wright, Suzanne Bentler, Elizabeth Momany, and Peter Damiano, “Iowa’s Medicaid Expansion Promoted Healthy Behaviors But Was Challenging to Implement and Attracted Few Participants,” Health Affairs 36 no. 5, (May 2017): 799-807, http://content.healthaffairs.org/content/36/5/799.full
- Angela Fertig, Caroline Carlin, Scote Ode, and Sharon Long, “Evidence of Pent-Up Demand for Care After Medicaid Expansion,” Medical Care Research and Review epub ahead of print (March 2017), http://journals.sagepub.com/eprint/wDsfA74fuA3BIw5ZWyYT/full
- The Lewin Group, Healthy Indiana Plan 2.0: POWER Account Contribution Assessment, (The Lewin Group, prepared for the Indiana Family and Social Services Administration, March 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-POWER-acct-cont-assesmnt-03312017.pdf
- Daniel Gingold, Rachelle Pierre-Mathieu, Brandon Cole, Andrew Miller, and Joneigh Khaldun, “Impact of the Affordable Care Act Medicaid Expansion on Emergency Department High Utilizers with Ambulatory Care Sensitive Conditions: A Cross-Sectional Study,” The American Journal of Emergency Medicine (January 2017), http://www.sciencedirect.com/science/article/pii/S0735675717300141
- Pennsylvania Department of Human Services, Medicaid Expansion Report, (Pennsylvania Department of Human Services, January 2017), http://www.dhs.pa.gov/cs/groups/webcontent/documents/document/c_257436.pdf
- Natalia Chalmers, Jane Grover, and Rob Compton, “After Medicaid Expansion in Kentucky, Use of Hospital Emergency Departments for Dental Conditions Increased,” Health Affairs 35, no. 12 (December 2016), http://content.healthaffairs.org/content/35/12/2268.full#xref-ref-32-1
- Jeffrey Horn et al., “New Medicaid Enrollees See Health and Social Benefits in Pennsylvania’s Expansion,” INQUIRY: the Journal of Health Care Organization, Provision, and Financing 53 (October 2016): 1-8, http://journals.sagepub.com/doi/full/10.1177/0046958016671807#
- The Lewin Group, Indiana Healthy Indiana Plan 2.0: Interim Evaluation Report (The Lewin Group, Prepared for Indiana Family and Social Services Administration, July 2016), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-interim-evl-rpt-07062016.pdf
- Renuka Tipirneni et al., “Primary Care Appointment Availability and Nonphysician Providers One Year After Medicaid Expansion,” The American Journal of Managed Care 22 no. 6 (June 2016): 427-431, http://www.ajmc.com/journals/issue/2016/2016-vol22-n6/primary-care-appointment-availability-and-nonphysician-providers-one-year-after-medicaid-expansion
- Joseph Benitez, Liza Creel, and J’Aime Jennings, “Kentucky’s Medicaid Expansion Showing Early Promise on Coverage and Access to Care,” Health Affairs (February 2016), http://content.healthaffairs.org/content/early/2016/02/16/hlthaff.2015.1294
- Arkansas Health Reform Legislative Task Force, Health Care Task Force Preliminary Report, (Arkansas Health Reform Legislative Task Force, December 2015), http://www.arkleg.state.ar.us/assembly/2015/Meeting%20Attachments/836/I14218/Task%20Force%20report%2012-17-15%20sent%20to%20Jill.pdf
- Michael McCue, “The Impact of Medicaid Expansion on Medicaid Focused Insurers in California,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 52 (July 2015), http://inq.sagepub.com/content/52/0046958015595960.full.pdf+html
- Renuka Tipirneni et al., “Primary Care Appointment Availability For New Medicaid Patients Increased After Medicaid Expansion In Michigan,” Health Affairs (July 2015), http://content.healthaffairs.org/content/early/2015/07/15/hlthaff.2014.1425.full
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf
Economic Effects of Expansion
Impact on State Budgets and Economies
NATIONWIDE STUDIES (back to top)
- Qiwei He and Scott Barkowski, “The Effect of Health Insurance on Crime: Evidence from the Affordable Care Act Medicaid Expansion,” Health Economics Epub ahead of print (January 2020): 261-277, https://doi.org/10.1002/hec.3977
- Robin Rudowitz et al., Medicaid Enrollment and Spending Growth: FY 2019 & 2020 (Washington, DC: Kaiser Family Foundation, October 2019), https://www.kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2019-2020/
- Johanna Maclean and Brendan Saloner, “The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act,” Journal of Policy Analysis and Management 38, no. 2 (Spring 2019): 366-393, https://www.ncbi.nlm.nih.gov/pubmed/30882195
- Amanda Abraham et al., “Changes in State Technical Assistance Priorities and Block Grant Funds for Addiction After ACA Implementation,” American Journal of Public Health epub ahead of print (May 2019), https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2019.305052
- Gary Pickens et al., “Changes In Hospital Service Demand, Cost, And Patient Illness Severity Following Health Reform,” Health Services Research (May 2019), https://doi.org/10.1111/1475-6773.13165
- Robin Rudowitz, Elizabeth Hinton, and Larisa Antonisse, Medicaid Enrollment and Spending Growth: FY 2018 & 2019 (Washington, DC: Kaiser Family Foundation, October 2018), https://www.kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2018-2019/
- Christian Wolfe, Kathryn Rennie, and Christopher Truffer, 2017 Actuarial Report on the Financial Outlook for Medicaid (Office of the Actuary, Centers for Medicare and Medicaid Services, September 2018), https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/Downloads/MedicaidReport2017.pdf
- Aditi Sen and Thomas DeLeire, “How Does Expansion Of Public Health Insurance Affect Risk Pools And Premiums In The Market For Private Health Insurance? Evidence From Medicaid And The Affordable Care Act Marketplaces,” Health Economics 27 (July 2018): 1877–1903, https://onlinelibrary.wiley.com/doi/abs/10.1002/hec.3809
- Micah Hartman et al., “National Health Care Spending in 2016: Spending and Enrollment Growth Slow After Initial Coverage Expansions,” Health Affairs epub ahead of print (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1299
- Aparna Soni, Marguerite Burns, Laura Dague, and Kosali Simon, “Medicaid Expansion and State Trends in Supplemental Security Income Program Participation,” Health Affairs 36 no. 8, (August 2017): 1485-1488, http://content.healthaffairs.org/content/36/8/1485.full?sid=982b20c0-0a17-4dc4-a35a-b0302d4ec289
- Seth Freedman, Sayeh Nikpay, Aaron Carroll, and Kosali Simon, “Changes in inpatient payer-mix and hospitalizations following Medicaid expansion: Evidence from all-capture hospital discharge data,” PLoS One 12 no. 9 (September 2017), http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0183616
- Jacqueline Fiore, The Impact of the Affordable Care Act’s Medicaid Expansion on Medicaid Spending by Health Care Service Category (Tulane University, July 2017), http://econ.tulane.edu/RePEc/pdf/tul1706.pdf
- David Lassman et al., “Health Spending by State 1991-2014: Measuring Per Capita Spending by Payers and Programs,” Health Affairs epub ahead of print (June 2017), http://content.healthaffairs.org/content/early/2017/06/13/hlthaff.2017.0416
- Benjamin Sommers and Jonathan Gruber, “Federal Funding Insulated State Budgets From Increased Spending Related To Medicaid Expansion,” Health Affairs epub ahead of print (April 2017), http://content.healthaffairs.org/content/early/2017/04/10/hlthaff.2016.1666.full
- Ashley Semanskee, Cynthia Cox, and Larry Levitt, Data Note: Effect of State Decisions on State Risk Scores (Kaiser Family Foundation, October 2016), https://www.kff.org/health-reform/issue-brief/data-note-effect-of-state-decisions-on-state-risk-scores/
- Aditi Sen and Thomas DeLeire, The Effect of Medicaid Expansion on Marketplace Premiums (Office of the Assistant Secretary for Planning and Evaluation, August 2016), https://aspe.hhs.gov/sites/default/files/pdf/206761/McaidExpMktplcPrem.pdf
- Laura Snyder, Katherine Young, Robin Rudowitz, and Rachel Garfield, Medicaid Expansion Spending and Enrollment in Context: An Early Look at CMS Claims Data for 2014 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, January 2016), http://kff.org/medicaid/issue-brief/medicaid-expansion-spending-and-enrollment-in-context-an-early-look-at-cms-claims-data-for-2014/
- Christopher Truffer, Christian Wolfe, and Kathryn Rennie, 2016 Actuarial Report on the Financial Outlook for Medicaid, (Office of the Actuary, Centers for Medicare and Medicaid Services, 2016), https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/Downloads/MedicaidReport2016.pdf
- Robin Rudowitz, Laura Snyder, and Vernon Smith, Medicaid Enrollment and Spending Growth: FY 2015 & 2016 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, October 2015), http://kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2015-2016/
MULTI-STATE STUDIES (back to top)
- Jesse M. Hinde et al., “Increasing Access to Opioid Use Disorder Treatment: Assessing State Policies and the Evidence Behind Them,” Journal of Studies on Alcohol and Drugs 80, no. 6 (November 2019): 693-697, https://doi.org/10.15288/jsad.2019.80.693
- Vikki Wachino and Samantha Artiga, How Connecting Justice-Involved Individuals to Medicaid Can Help Address the Opioid Epidemic (Washington, DC: Kaiser Family Foundation, June 2019), https://www.kff.org/medicaid/issue-brief/how-connecting-justice-involved-individuals-to-medicaid-can-help-address-the-opioid-epidemic/
- Bryce Ward and Brandon Bridge, The Economic Impact of Medicaid Expansion in Montana: Updated Findings (Bureau of Business and Economic Research, January 2019), https://mthcf.org/wp-content/uploads/2019/01/Economic-Impact-of-MedEx-in-MT_1.28.19-FINAL.pdf
- Paul Jacobs, Genevieve Kenney, and Thomas Selden, “Newly Eligible Enrollees In Medicaid Spend Less And Use Less Care Than Those Previously Eligible,” Health Affairs 36, no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0252
- Deborah Bachrach, Patricia Boozang, Avi Herring, and Dori Glanz Reyneri, States Expanding Medicaid See Significant Budget Savings and Revenue Gains, (Manatt Health Solutions, prepared by the Robert Wood Johnson Foundation’s State Health Reform Assistance Network, March 2016), http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2016/rwjf419097
- Stan Dorn, Norton Francis, Laura Snyder, and Robin Rudowitz, The Effects of the Medicaid Expansion on State Budgets: An Early Look in Select States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, March 2015), http://kff.org/medicaid/issue-brief/the-effects-of-the-medicaid-expansion-on-state-budgets-an-early-look-in-select-states/
SINGLE STATE STUDIES (back to top)
- Stephan R. Lindner et al., “Health Care Expenditures Among Adults With Diabetes After Oregon’s Medicaid Expansion,” Diabetes Care Epub ahead of print (December 2019), https://doi.org/10.2337/dc19-1343
- Heather Holderness et al., “Where Do Oregon Medicaid Enrollees Seek Outpatient Care Post-Affordable Care Act Medicaid Expansion?,” Medical Care 57, no. 10 (October 2019): 788-794, https://doi.org/10.1097/mlr.0000000000001189
- Helen Levy et al., “Macroeconomic Feedback Effects of Medicaid Expansion: Evidence from Michigan,” Journal of Health Politics, Policy and Law Epub ahead of print (October 2019), https://doi.org/10.1215/03616878-7893555
- James A. Richardson, Jared J. Llorens, and Roy L. Heidelberg. Medicaid Expansion and the Louisiana Economy, 2018 and 2019 (Louisiana Department of Health, Prepared by Louisiana State University, August 2019), http://ldh.la.gov/assets/media/3and4.2019FinalReportMedicaidExpansionstudy.pdf
- Mark Duggan, Atul Gupta, and Emilie Jackson, The Impact of the Affordable Care Act: Evidence from California’s Hospital Sector (National Bureau of Economic Research, working paper no. 25488, January 2019), https://www.nber.org/papers/w25488.pdf
- Aaron McNay, Amy Watson, Barbara Wagner, and Chris Bradley, Montana Medicaid and Montana Employers (Montana Department of Revenue and Montana Department of Labor & Industry, January 2019), http://lmi.mt.gov/Portals/193/Publications/LMI-Pubs/Special%20Reports%20and%20Studies/MT-Medicaid_Report.pdf
- Susan Dorr Goold et al., “Primary Care Clinicians’ Views About the Impact of Medicaid Expansion in Michigan: A Mixed Methods Study,” Journal of General Internal Medicine 33, no. 8 (June 2018): 1307-1316, https://link.springer.com/article/10.1007/s11606-018-4487-6
- Manatt Health, Medicaid Expansion: How It Affects Montana’s State Budget, Economy, and Residents (Montana Healthcare Foundation, prepared by Manatt Health, June 2018), https://mthcf.org/wp-content/uploads/2018/06/Manatt-MedEx_FINAL_6.1.18.pdf
- James Richardson, Jared Llorens, and Roy Heidelberg, Medicaid Expansion and the Louisiana Economy (Louisiana Department of Health, March 2018), http://gov.louisiana.gov/assets/MedicaidExpansion/MedicaidExpansionStudy.pdf
- Bela Gorman and Jenn Smagula, 2016 Actuarial Analysis of NH Premium Assistance Program, (Gorman Actuarial, Inc., August 2017), https://www.nh.gov/insurance/reports/documents/08-28-17-ga-nh-pap-analysis-final.pdf
- Louisiana Department of Health, Medicaid Expansion 2016/17 (Baton Rouge, Louisiana Department of Health, June 2017), http://dhh.louisiana.gov/assets/HealthyLa/Resources/MdcdExpnAnnlRprt_2017_WEB.pdf
- John Ayanian, Gabriel Ehrlich, Donald Grimes, and Helen Levy, “Economic Effects of Medicaid Expansion in Michigan,” The New England Journal of Medicine epub ahead of print (January 2017), http://www.nejm.org/doi/full/10.1056/NEJMp1613981
- Pennsylvania Department of Human Services, Medicaid Expansion Report, (Pennsylvania Department of Human Services, January 2017), http://www.dhs.pa.gov/cs/groups/webcontent/documents/document/c_257436.pdf
- The Colorado Health Institute, Medicaid Expansion in Colorado: An Analysis of Enrollment, Costs and Benefits—and How They Exceeded Expectations (The Colorado Health Institute, May 2016), http://www.coloradohealthinstitute.org/uploads/postfiles/MK_Expansion_Report.pdf
- The Colorado Health Foundation, Assessing the Economic and Budgetary Impact of Medicaid Expansion in Colorado, (The Colorado Health Foundation, March 2016), https://www.coloradohealth.org/sites/default/files/documents/2017-01/Medicaid_ExecutiveSummary_ONLINE.pdf
- Lee A. Reynis, Economic and Fiscal Impacts of the Medicaid Expansion in New Mexico, (The University of New Mexico Bureau of Business and Economic Research, February 2016), http://bber.unm.edu/media/publications/Medicaid_Expansion_Final2116R.pdf
- Abby Evans, John Folkemer, Joel Menges, Amira Mouna, Nick Pantaleo, Emily Ricci, and Poornima Sigh, Assessment of Medicaid Expansion and Reform, Initial Analysis (The Menges Group, January 2016), https://alaskamentalhealthtrust.org/wp-content/uploads/2018/08/HandOut-MedicaidExpansionAndReformInitialAnalysis-011516-TheMengesGroup.pdf
- Chris Brown and John Bennett, Economic Impacts of the Arkansas Private Option (Regional Economic Models, Inc., August 2015), http://www.arkhospitals.org/Misc.%20Files/August2015APOEconomicImpacts.pdf
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf
Impact on Payer Mix for Hospitals, Clinics, and Other Providers
NATIONWIDE STUDIES (back to top)
- Meera N. Harhay, Ryan M. McKenna, and Michael O. Harhay, “Association Between Medicaid Expansion Under the Affordable Care Act and Medicaid-Covered Pre-emptive Kidney Transplantation,” Journal of General Internal Medicine 34, no. 11 (November 2019): 2322-2325, https://doi.org/10.1007/s11606-019-05279-x
- Johanna Maclean and Brendan Saloner, “The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act,” Journal of Policy Analysis and Management 38, no. 2 (Spring 2019): 366-393, https://www.ncbi.nlm.nih.gov/pubmed/30882195
- Christina Andrews et al., “Medicaid Coverage In Substance Use Disorder Treatment After The Affordable Care Act,” Journal of Substance Abuse Treatment epub ahead of print (April 2019), https://www.sciencedirect.com/science/article/pii/S0740547218305750
- Michel Boudreaux, Yoon Choi, Liyang Xie, and Daniel Marthey, “Medicaid Expansion at Title X Clinics: Client Volume, Payer Mix, and Contraceptive Method Type,” Medical Care epub ahead of print (April 2019), https://www.ncbi.nlm.nih.gov/pubmed/30973473
- Ramin Mojtabai, Christine Mauro, Melanie Wall, Colleen Barry, and Mark Olfson, “The Affordable Care Act and Opioid Agonist Therapy for Opioid Use Disorder,” Psychiatry Online (April 2019), https://doi.org/10.1176/appi.ps.201900025
- Jordan Rhodes, Thomas Buchmueller, Helen Levy, and Sayeh Nikpay, “Heterogeneous Effects Of The Aca Medicaid Expansion On Hospital Financial Outcomes,” Contemporary Economic Policy epub ahead of print (April 2019), https://onlinelibrary.wiley.com/doi/full/10.1111/coep.12428
- Tyler McClintock, Ye Wang, Mahek Shah, Benjamin Chung, and Steven Chang, “How Have Hospital Pricing Practices for Surgical Episodes of Care Responded to Affordable Care Act-Related Medicaid Expansion?” Urology 125 (March 2019): 79-85, https://doi.org/10.1016/j.urology.2018.10.034
- Gary Young, Stephen Flaherty, E. Zepeda, Simone Singh, and Sara Rosenbaum, “Impact of ACA Medicaid Expansion on Hospitals’ Financial Status” Journal of Healthcare Management 64, no. 2 (March 2019): 91–102, https://insights.ovid.com/crossref?an=00115514-201904000-00007
- J.W. Awori Hayanga et al., “Lung Transplantation and Affordable Care Act Medicaid Expansion in the Era of Lung Allocation Score” Transplant International epub ahead of print (February 2019), https://onlinelibrary.wiley.com/doi/pdf/10.1111/tri.13420
- Rishi Wadhera et al., “Association of State Medicaid Expansion With Quality of Care and Outcomes for Low-Income Patients Hospitalized With Acute Myocardial Infarction,” JAMA Cardiology 4, no. 2 (January 2019): 120-127, https://jamanetwork.com/journals/jamacardiology/article-abstract/2720425?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamacardio.2018.4577
- Meera Harhay et al., “Association between Medicaid Expansion under the Affordable Care Act and Preemptive Listings for Kidney Transplantation,” Clinical Journal of the American Society of Nephrology 13 (July 2018), https://cjasn.asnjournals.org/content/13/7/1069
- Megan Cole, Brad Wright, Ira Wilson, Omar Gallarraga, and Amal Trivedi, “Medicaid Expansion And Community Health Centers: Care Quality And Service Use Increased For Rural Patients” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1542
- Angelica Meinhofer and Allison Witman, “The Role Of Health Insurance On Treatment For Opioid Use Disorders: Evidence From The Affordable Care Act Medicaid Expansion,” Journal of Health Economics 60 (June 2018): 177-197, https://www.sciencedirect.com/science/article/abs/pii/S0167629617311530
- Rishi Wadhera et al., “Association of the Affordable Care Act’s Medicaid Expansion With Care Quality and Outcomes for Low-Income Patients Hospitalized With Heart Failure,” Cardiovascular Quality and Outcomes 11, no. 7 (June 2018), https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.118.004729
- Rachel Garfield, Elizabeth Hinton, Elizabeth Cornachione, and Cornelia Hall, Medicaid Managed Care Plans and Access to Care: Results from the Kaiser Family Foundation 2017 Survey of Medicaid Managed Care Plans (Washington, DC: Kaiser Family Foundation, March 2018), https://www.kff.org/medicaid/report/medicaid-managed-care-plans-and-access-to-care-results-from-the-kaiser-family-foundation-2017-survey-of-medicaid-managed-care-plans
- Sara Rosenbaum, Jennifer Tolbert, Jessica Sharac, Peter Shin, Rachel Gunsalus, and Julia Zur, Community Health Centers: Growing Importance in a Changing Health Care System (Washington, DC: Kaiser Family Foundation, March 2018), https://www.kff.org/medicaid/issue-brief/community-health-centers-growing-importance-in-a-changing-health-care-system/
- Nicolas Ajkay et al, “Early Impact of Medicaid Expansion and Quality of Breast Cancer Care in Kentucky,” Journal of the American College of Surgeons, epub ahead of print, February 2018, https://www.sciencedirect.com/science/article/pii/S107275151830022X
- Richard Lindrooth, Marcelo Perraillon, Rose Hardy, and Gregory Tung, “Understanding the Relationship Between Medicaid Expansions and Hospital Closures,” Health Affairs epub ahead of print (January 2018), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0976
- Andrew Loehrer et al., “Association of the Affordable Care Act Medicaid Expansion with Access to and Quality of Care for Surgical Conditions,” Journal of the American Medical Association Surgery, epub ahead of print (January 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2670459?redirect=true
- Allen Dobson, Joan DaVanzo, Randy Haught, and Phap Hoa Luu, Comparing the Affordable Care Act’s Financial Impact on Safety-Net Hospitals in States that Expanded Medicaid and Those That Did Not (The Commonwealth Fund, November 2017), http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2017/nov/dobson_impact_medicaid_expanion_safety_net_hosps_ib.pdf
- Jacob Vogler, Access to Health Care and Criminal Behavior: Short-Run Evidence from the ACA Medicaid Expansions (University of Illinois at Urbana-Champaign, November 2017), https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3042267
- Kurt Gillis, Physicians’ Patient Mix – A Snapshot from the 2016 Benchmark Survey and Changes Associated with the ACA (American Medical Association, October 2017), https://www.ama-assn.org/sites/default/files/media-browser/public/health-policy/PRP-2017-physician-benchmark-survey-patient-mix.pdf
- Heather Angier et al., “Uninsured Primary Care Visit Disparities under the Affordable Care Act,” Annals of Family Medicine, 15 no. 5 (September 2017): 434-442, http://www.annfammed.org/content/15/5/434.full.pdf+html
- Sayeh Nikpay, Seth Freedman, Helen Levy, and Tom Buchmueller, “Effect of the Affordable Care Act Medicaid Expansion on Emergency Department Visits: Evidence From State-Level Emergency Department Databases,” Annals of Emergency Medicine 70, no.2 (August 2017), http://www.annemergmed.com/article/S0196-0644(17)30319-0/pdf
- Dmitry Tumin et al., “Medicaid Participation among Liver Transplant Candidates after the Affordable Care Act Medicaid Expansion” Journal of the American College of Surgeons 225, no. 2 (August 2017): 173-180.e2, https://www.journalacs.org/article/S1072-7515(17)30454-4/fulltext
- Gary Pickens et al., “Changes in Hospital Inpatient Utilization Following Health Care Reform,” Health Services Research epub ahead of print (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28664983
- Susan Camilleri, “The ACA Medicaid Expansion, Disproportionate Share Hospitals, and Uncompensated Care” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12702/abstract
- David Dranove, Craig Garthwaite, and Christopher Ody, The Impact of the ACA’s Medicaid Expansion on Hospitals’ Uncompensated Care Burden and the Potential Effects of Repeal, (The Commonwealth Fund, May 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/may/aca-medicaid-expansion-hospital-uncompensated-care
- Fredric Blavin, How Has the ACA Changed Finances for Different Types of Hospitals? Updated Insights from 2015 Cost Report Data (The Urban Institute, April 2017), http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2017/rwjf436310
- Craig Garthwaite, Tal Gross, Matthew Notowidigdo, and John Graves, “Insurance Expansion and Hospital Emergency Department Access: Evidence from the Affordable Care Act,” Annals of Internal Medicine 166 no. 3 (February 2017): 172-179, http://annals.org/aim/article/2593599/insurance-expansion-hospital-emergency-department-access-evidence-from-affordable-care
- Megan Cole, Omar Galarraga, Ira Wilson, Brad Wright, and Amal Trivedi, “At Federally Funded Health Centers, Medicaid Expansion was Associated with Improved Quality of Care,” Health Affairs 36 no. 1 (January 2017): 40-48, http://content.healthaffairs.org/content/36/1/40.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19
- Xinxin Han, Quian Luo, and Leighton Ku, “Medicaid Expansion and Grant Funding Increases Helped Improve Community Health Center Capacity,” Health Affairs 36 no. 1 (January 2017): 49-56, http://content.healthaffairs.org/content/36/1/49.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19
- Fredric Blavin, “Association Between the 2014 Medicaid Expansion and US Hospital Finances,” The Journal of the American Medical Association 316 no. 14 (October 2016): 1475-1483, http://jamanetwork.com/journals/jama/article-abstract/2565750
- Brystana Kaufman, Kristin Reiter, George Pink, and George Holmes, “Medicaid Expansion Affects Rural and Urban Hospitals Differently,” Health Affairs 35 no. 9 (September 2016): 1665-1672, http://content.healthaffairs.org/content/35/9/1665.full?sid=4aea494e-8e02-4c66-8298-3c828bfc313b
- Mary Anderson, Jeffrey Glasheen, Debra Anoff, “Impact of State Medicaid Expansion Status on Length of Stay and In-Hospital Mortality for General Medicine Patients at US Academic Medical Centers,” Journal of Hospital Medicine Epub ahead of print (August 2016), http://onlinelibrary.wiley.com/wol1/doi/10.1002/jhm.2649/citedby
- David Dranove, Craig Garthwaite, and Christopher Ody, “Uncompensated Care Decreased At Hospitals In Medicaid Expansion States But Not At Hospitals In Nonexpansion States,” Health Affairs 35 no. 8 (August 2016): 1471-1479, http://content.healthaffairs.org/content/35/8/1471.full
- Jesse M. Pines, Mark Zocchi, Ali Moghtaderi, Bernard Black, Steven A. Farmer, Greg Hufstetler, Kevin Klauer and Randy Pilgrim, “Medicaid Expansion In 2014 Did Not Increase Emergency Department Use But Did Change Insurance Payer Mix,” Health Affairs 35, no. 8 (August 2016), http://content.healthaffairs.org/content/35/8/1480.full
- Peter Cunningham, Robin Rudowitz, Katherine Young, Rachel Garfield, and Julia Foutz, Understanding Medicaid Hospital Payments and the Impact of Recent Policy Changes (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2016), http://kff.org/medicaid/issue-brief/understanding-medicaid-hospital-payments-and-the-impact-of-recent-policy-changes/
- Brendan Saloner, Sachini Bandara, Emma McGinty, and Colleen Barry, “Justice-Involved Adults With Substance Use Disorders: Coverage Increased but Rates of Treatment Did Not in 2014,” Health Affairs 35 no. 6 (June 2016), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2016.0005
- Dmitry Tumin, Don Hayes Jr., Kenneth Washburn, Joseph Tobias, and Sylvester Black, “Medicaid Enrollment after Liver Transplantation: Effects of Medicaid Expansion,” Liver Transplantation (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27152888
- Matt Warfield, Barbara DiPietro, and Samantha Artiga, How has the ACA Medicaid Expansion Affected Providers Serving the Homeless Population: Analysis of Coverage, Revenues, and Costs (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, March 2016), https://files.kff.org/attachment/issue-brief-how-has-the-aca-medicaid-expansion-affected-providers-serving-the-homeless-population
- Peter Shin, Jessica Sharac, Julia Zur, Sara Rosenbaum, and Julia Paradise, Health Center Patient Trends, Enrollment Activities, and Service Capacity: Recent Experience in Medicaid Expansion and Non-Expansion States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, December 2015), http://kff.org/medicaid/issue-brief/health-center-patient-trends-enrollment-activities-and-service-capacity-recent-experience-in-medicaid-expansion-and-non-expansion-states/
- Deborah Bachrach, Patricia Boozang, and Mindy Lipson, The Impact of Medicaid Expansion on Uncompensated Care Costs: Early Results and Policy Implications for States, (Manatt Health Solutions, prepared by the Robert Wood Johnson Foundation’s State Health Reform Assistance Network, June 2015), https://www.manatt.com/uploadedFiles/Content/5_Insights/White_Papers/State-Network-Manatt-Impact-of-Medicaid-Expansion-on-Uncompensated-Care-Costs-June-2015.pdf
- Josh Gray, Iyue Sung, and Stewart Richardson, Observations on the Affordable Care Act: 2014 (athenaResearch and Robert Wood Johnson Foundation ACA View Report, February 2015), http://www.athenahealth.com/~/media/athenaweb/files/pdf/acaview_year_end_2014.pdf
- Thomas DeLeire, Karen Joynt, and Ruth McDonald, Impact of Insurance Expansion on Hospital Uncompensated Care Costs in 2014 (Office of the Assistant Secretary for Planning and Evaluation, September 2014), https://aspe.hhs.gov/sites/default/files/pdf/77061/ib_UncompensatedCare.pdf
- PricewaterhouseCoopers LLP Health Research Institute, Medicaid 2.0: Health System Haves and Have Nots (PwC Health Research Institute, September 2014), http://www.pwc.com/us/en/health-industries/health-research-institute/assets/pwc-hri-medicaid-report-final.pdf
MULTI-STATE STUDIES (back to top)
- Emanuel Eguia et al., “The Impact of the Affordable Care Act Medicaid Expansion on Vascular Surgery,” Annals of Vascular Surgery Epub ahead of print (January 2020), https://doi.org/10.1016/j.avsg.2020.01.006
- Hawazin W. Elani, Ichiro Kawachi, and Benjamin D. Sommers, “Changes in Emergency Department Dental Visits after Medicaid Expansion,” Health Services Research Epub ahead of print (January 2020), https://doi.org/10.1111/1475-6773.13261
- Alexander T. Janke, Shooshan Danagoulian, Arjun K. Venkatesh, and Phillip D. Levy, “Medicaid Expansion and Resource Utilization in the Emergency Department,” The American Journal of Emergency Medicine Epub ahead of print (January 2020), https://doi.org/10.1016/j.ajem.2019.12.050
- Mark Clapp et al., “Association of Medicaid Expansion With Coverage and Access to Care for Pregnant Women,” Obstetrics & Gynecology 134, no. 5 (November 2019): 1066-1074, https://doi.org/10.1097/aog.0000000000003501
- Hefei Wen, Kenton J. Johnston, Lindsay Allen, and Teresa M. Waters, “Medicaid Expansion Associated With Reductions In Preventable Hospitalizations,” Health Affairs 38, no. 11 (November 2019): 1845-1849, https://doi.org/10.1377/hlthaff.2019.00483
- Nadia Laniado, Avery R. Brow, Eric Tranby, and Victor M. Badner, “Trends in Non-Traumatic Dental Emergency Department Use in New York and New Jersey: A Look at Medicaid Expansion from Both Sides of the Hudson River,” Journal of Public Health Dentistry Epub ahead of print (October 2019), https://doi.org/10.1111/jphd.12343
- Elizabeth A. Brown et al., “The Impact of the ACA Medicaid Expansion on Access to Care and Hospitalization Charges for Lupus Patients,” Arthritis Care & Research Epub ahead of print (September 2019), https://doi.org/10.1002/acr.24080
- Craig Garthwaite et al., All Medicaid Expansions Are Not Created Equal: The Geography and Targeting of the Affordable Care Act (National Bureau of Economic Research, Working Paper No. 26289, September 2019), http://www.nber.org/papers/w26289
- Emanuel Eguia et al., “The Impact of the Affordable Care Act (ACA) Medicaid Expansion on Access to Minimally Invasive Surgical Care,” The American Journal of Surgery Epub ahead of print (July 2019), https://doi.org/10.1016/j.amjsurg.2019.07.003
- Andrew Crocker et al., “Expansion Coverage And Preferential Utilization Of Cancer Surgery Among Racial And Ethnic Minorities And Low-Income Groups,” Surgery epub ahead of print (June 2019), https://www.surgjournal.com/article/S0039-6060(19)30198-9/fulltext
- Ramiro Manzano-Nunez et al., “Association of Medicaid Expansion Policy with Outcomes in Homeless Patients Requiring Emergency General Surgery,” World Journal of Surgery 43, no. 6 (June 2019): 1483-1489, https://link.springer.com/article/10.1007/s00268-019-04932-0
- Rahul Ladhania, Amelia Haviland, Arvind Venkat, Rahul Telang, and Jesse Pines, “The Effect of Medicaid Expansion on the Nature of New Enrollees’ Emergency Department Use,” Medical Care Research and Review epub ahead of print (May 2019), https://journals.sagepub.com/doi/abs/10.1177/1077558719848270
- Favel Mondesir et al., “Medicaid Expansion and Hospitalization for Ambulatory Care–Sensitive Conditions Among Nonelderly Adults With Diabetes,” Journal of Ambulatory Care Management epub ahead of print (May 2019), https://insights.ovid.com/pubmed?pmid=31107800
- Heather Angier et al., “Racial/Ethnic Disparities in Health Insurance and Differences in Visit Type for a Population of Patients with Diabetes after Medicaid Expansion” Journal of Health Care for the Poor and Underserved 30, no.1, (March 2019) 116–130: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6429963/
- Jesse Pines, Rahul Ladhania BTech, Bernard Black , Christopher Corbit, Jestin Carlson, and Arvind Venkat, “Changes in Reimbursement to Emergency Physicians After Medicaid Expansion Under the Patient Protection and Affordable Care Act,” Annals of Emergency Medicine 73, no. 3 (March 2019): 213-224, https://www.sciencedirect.com/science/article/pii/S019606441831374X
- Cheryl Zogg et al., “Association of Medicaid Expansion With Access to Rehabilitative Care in Adult Trauma Patients,” JAMA Surgery epub ahead of print (January 2019), https://jamanetwork.com/journals/jamasurgery/article-abstract/2719270?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamasurg.2018.5177
- Cheryl Zogg et al., “Impact of Affordable Care Act Insurance Expansion on Pre-Hospital Access to Care: Changes in Adult Perforated Appendix Admission Rates after Medicaid Expansion and the Dependent Coverage Provision,” Journal of the American College of Surgeons 228, no. 1 (January 2019): 29-43, https://www.journalacs.org/article/S1072-7515(18)32078-7/fulltext
- Nathalie Huguet et al., “The Impact of the Affordable Care Act (ACA) Medicaid Expansion on Visit Rates for Diabetes in Safety Net Health Centers,” Journal of the American Board of Family Medicine 31, no. 6 (November 2018): 905-916, https://www.jabfm.org/content/31/6/905.full
- Emanuel Eguia et al., “Impact of the Affordable Care Act (ACA) Medicaid Expansion on Cancer Admissions and Surgeries,” Annals of Surgery 268, no. 4 (October 2018): 584-590, https://journals.lww.com/annalsofsurgery/Abstract/2018/10000/Impact_of_the_Affordable_Care_Act__ACA__Medicaid.6.aspx
- Manzilat Akande Peter Minneci, Katherine Deans, Henry Xiang, and Jennifer Cooper, “Association of Medicaid Expansion Under the Affordable Care Act With Outcomes and Access to Rehabilitation in Young Adult Trauma Patients,” JAMA Surgery 153, no. 8 (August 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2682872?widget=personalizedcontent&previousarticle=2719270
- Ehimare Akhabue, Lindsay Pool, Clyde Yancy, Philip Greenland, and Donald Lloyd-Jones, “Association of State Medicaid Expansion With Rate of Uninsured Hospitalizations for Major Cardiovascular Events, 2009-2014,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2698077
- Vivian Wu et al., “Early Impact of the Affordable Care Act Coverage Expansion on Safety-Net Hospital Inpatient Payer Mix and Market Shares,” Health Services Research (January 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12812/full
- Monique Barakat et al., “Affordable Care Act and Healthcare Delivery: A Comparison of California and Florida Hospitals and Emergency Departments,” PLoS ONE 12 no. 8 (August 2017), http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0182346
- Eric Charles et al., “Impact of Medicaid Expansion on Cardiac Surgery Volume and Outcomes,” The Annals of Thoracic Surgery (June 2017), http://www.annalsthoracicsurgery.org/article/S0003-4975(17)30552-0/pdf
- Nathalie Huguet et al., “Medicaid Expansion Produces Long-Term Impact on Insurance Coverage Rates in Community Health Centers,” Journal of Primary Care & Community Health epub ahead of print (May 2017), http://journals.sagepub.com/doi/full/10.1177/2150131917709403
- Laurie Felland, Peter Cunningham, Annie Doubleday, and Cannon Warren, Effects of the Affordable Care Act on Safety Net Hospitals (Washington, DC: Mathematica Policy Research, prepared for the Assistant Secretary for Planning and Evaluation, November 2016), https://aspe.hhs.gov/sites/default/files/pdf/255491/SafetyNetHospital.pdf
- Megan Hoopes, Heather Angier, Rachel Gold, Steffani Bailey, Nathalie Huguet, Miguel Marino, and Jennifer DeVoe, “Utilization of Community Health Centers in Medicaid Expansion and Nonexpansion States, 2013-2014,” Journal of Ambulatory Care Management 39 no. 4 (October 2016): 290-298, https://www.ncbi.nlm.nih.gov/pubmed/26765808
- Steven Wallace, Maria-Elena Young, Michael Rodriguez, Amy Bonilla, and Nadereh Pourat, Community Health Centers Play a Critical Role in Caring for the Remaining Uninsured in the Affordable Care Act Era (UCLA Center for Health Policy Research, October 2016), http://healthpolicy.ucla.edu/publications/Documents/PDF/2016/FQHC_PB-oct2016.pdf
- Jane Wishner, Patricia Solleveld, Robin Rudowitz, Julia Paradise, and Larisa Antonisse, A Look at Rural Hospital Closures and Implications for Access to Care: Three Case Studies (Washington, DC: Kaiser Commission on Medicaid and the Uninsured and The Urban Institute, July 2016), http://kff.org/medicaid/issue-brief/a-look-at-rural-hospital-closures-and-implications-for-access-to-care/
- Stephen Berry et al., “Healthcare Coverage for HIV Provider Visits before and after Implementation of the Affordable Care Act,” Clinical Infectious Diseases, (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27143660
- Sayeh Nikpay, Thomas Buchmueller, and Helen Levy. “Affordable Care Act Medicaid Expansion Reduced Uninsured Hospital Stays in 2014,” Health Affairs 35, no.1 (January 2016): 106-110, http://content.healthaffairs.org/content/35/1/106.full
- Fred Hellinger, “In Four ACA Expansion States, The Percentage of Uninsured Hospitalizations for People With HIV Declined, 2012-14,” Health Affairs 34, no. 12 (December 2015): 2061-2068, http://search.proquest.com/docview/1749932806/627DA95CDEA44BE7PQ/77?accountid=39486#
- Robin Rudowitz and Rachel Garfield, New Analysis Shows States with Medicaid Expansion Experienced Declines in Uninsured Hospital Discharges (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, September 2015), http://kff.org/health-reform/issue-brief/new-analysis-shows-states-with-medicaid-expansion-experienced-declines-in-uninsured-hospital-discharges/
- Samantha Artiga, Jennifer Tolbert, and Robin Rudowitz, Year Two of the ACA Coverage Expansions: On-the-Ground Experiences from Five States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/health-reform/issue-brief/year-two-of-the-aca-coverage-expansions-on-the-ground-experiences-from-five-states/
- Peter Cunningham, Rachel Garfield, and Robin Rudowitz, How Are Hospitals Faring Under the Affordable Care Act? Early Experiences from Ascension Health (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, April 2015), http://kff.org/health-reform/issue-brief/how-are-hospitals-faring-under-the-affordable-care-act-early-experiences-from-ascension-health/
- Colorado Hospital Association, Impact of Medicaid Expansion on Hospital Volumes (Colorado Hospital Association Center for Health Information and Data Analytics, June 2014), http://www.cha.com/documents/press-releases/cha-medicaid-expansion-study-june-2014.aspx
SINGLE STATE STUDIES (back to top)
- Charles A. Daly et al., “The Effects of Medicaid Expansion on Triage and Regional Transfer After Upper-Extremity Trauma,” The Journal of Hand Surgery 44, no. 9 (September 2019): 720-727, https://doi.org/10.1016/j.jhsa.2019.05.020
- Beatrice D. Probst, Luther Walls, Michael Cirone, and Talar Markossian, “Examining the Effect of the Affordable Care Act on Two Illinois Emergency Departments,” Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health 20, no. 5 (September 2019): 710-716, https://doi.org/10.5811/westjem.2019.6.41943
- John Scott et al., “Lifting the Burden: State Medicaid Expansion Reduces Financial Risk for the Injured,” Journal of Trauma and Acute Care Surgery Epub ahead of print (September 2019), https://doi.org/10.1097/ta.0000000000002493
- Neal Bhutiani, Brian Harbrecht, Charles Scoggins, and Matthew Bozeman, “Evaluating The Early Impact Of Medicaid Expansion On Trends In Diagnosis And Treatment Of Benign Gallbladder Disease In Kentucky,” The American Journal of Surgery (January 2019), https://www.americanjournalofsurgery.com/article/S0002-9610(18)30894-8/fulltext
- Mark Duggan, Atul Gupta, and Emilie Jackson, The Impact of the Affordable Care Act: Evidence from California’s Hospital Sector (National Bureau of Economic Research, working paper no. 25488, January 2019), https://www.nber.org/papers/w25488.pdf
- Manatt Health, Medicaid Expansion: How It Affects Montana’s State Budget, Economy, and Residents (Montana Healthcare Foundation, prepared by Manatt Health, June 2018), https://mthcf.org/wp-content/uploads/2018/06/Manatt-MedEx_FINAL_6.1.18.pdf
- Shannon McConville, Maria Raven, Sarah Sabbagh, and Renee Hsia, “Frequent Emergency Department Users: A Statewide Comparison Before And After Affordable Care Act Implementation,” Health Affairs 37, no. 6, (June 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0784
- Donald Likosky, Devraj Sukul, Milan Seth, Chang He, Hitlander Gurm, and Richard Prager, “The Association Between Medicaid Expansion and Cardiovascular Interventions: The Michigan Experience,” Journal of the American College of Cardiology 71, no. 9 (March 2018): 1050-1051, https://www.sciencedirect.com/science/article/pii/S0735109718300056?via%3Dihub
- Eili Klein et al., “The Effect of Medicaid Expansion on Utilization in Maryland Emergency Departments,” Annals of Emergency Medicine epub ahead of print (June 2017), http://www.annemergmed.com/article/S0196-0644(17)30784-9/pdf
- Pennsylvania Department of Human Services, Medicaid Expansion Report, (Pennsylvania Department of Human Services, January 2017), http://www.dhs.pa.gov/cs/groups/webcontent/documents/document/c_257436.pdf
- Natalia Chalmers, Jane Grover, and Rob Compton, “After Medicaid Expansion in Kentucky, Use of Hospital Emergency Departments for Dental Conditions Increased,” Health Affairs 35, no. 12 (December 2016), http://content.healthaffairs.org/content/35/12/2268.full#xref-ref-32-1
- The University of Michigan Institute for Healthcare Policy & Innovation, The Healthy Michigan Plan: 2015 Report on Uncompensated Care and Insurance Rates (The University of Michigan Institute for Healthcare Policy & Innovation, prepared for the Michigan Department of Health and Human Services and the Michigan Department of Insurance and Financial Services, December 2016), http://www.michigan.gov/documents/mdhhs/2015_Report_on_Uncompensated_Care_and_Insurance_Rates-HMP_547720_7.pdf
- Mathew Davis, Achamyeleh Gebremariam, John Ayanian, “Changes in Insurance Coverage Among Hospitalized Nonelderly Adults After Medicaid Expansion in Michigan,” The Journal of the American Medical Association 315 no. 23 (June 2016): 2617-2618, http://jamanetwork.com/journals/jama/fullarticle/2529615
- Abby Evans, John Folkemer, Joel Menges, Amira Mouna, Nick Pantaleo, Emily Ricci, and Poornima Sigh, Assessment of Medicaid Expansion and Reform, Initial Analysis (The Menges Group, January 2016), https://alaskamentalhealthtrust.org/wp-content/uploads/2018/08/HandOut-MedicaidExpansionAndReformInitialAnalysis-011516-TheMengesGroup.pdf
- Arkansas Health Reform Legislative Task Force, Health Care Task Force Preliminary Report, (Arkansas Health Reform Legislative Task Force, December 2015), http://www.arkleg.state.ar.us/assembly/2015/Meeting%20Attachments/836/I14218/Task%20Force%20report%2012-17-15%20sent%20to%20Jill.pdf
- Jocelyn Guyer, Naomi Shine, MaryBeth Musumeci, and Robin Rudowitz, A Look at the Private Option in Arkansas (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, August 2015), http://kff.org/medicaid/issue-brief/a-look-at-the-private-option-in-arkansas/
- Christine Jones, Serena Scott, Debra Anoff, Read Pierce, Jeffrey Glasheen, “Changes in Payer Mix and Physician Reimbursement After the Affordable Care Act and Medicaid Expansion,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 52 (August 2015), http://inq.sagepub.com/content/52/0046958015602464.full
- Michael McCue, “The Impact of Medicaid Expansion on Medicaid Focused Insurers in California,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 52 (July 2015), http://inq.sagepub.com/content/52/0046958015595960.full.pdf+html
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf
- Arkansas Hospital Association, “Survey Reveals Private Option Impact on Hospitals,” The Notebook 21, no. 33 (November 2014), http://www.arkhospitals.org/archive/notebookpdf/Notebook_11-03-14.pdf
Impact on Employment and the Labor Market
NATIONWIDE STUDIES (back to top)
- Olga Scrivner et al., “Job Postings in the Substance Use Disorder Treatment Related Sector During the First Five Years of Medicaid Expansion,” PLoS One 15, no. 1 (January 2020), https://doi.org/10.1371/journal.pone.0228394
- Renuka Tipirneni et al., “Association of Medicaid Expansion With Enrollee Employment and Student Status in Michigan,” JAMA Network Open 3, no. 1 (January 2020), https://doi.org/10.1001/jamanetworkopen.2019.20316
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553
- Lizhong Peng, Xiaohui Guo, and Chad D. Meyerhoefer, “The Effects of Medicaid Expansion on Labor Market Outcomes: Evidence from Border Counties,” Health Economics Epub ahead of print (December 2019), https://doi.org/10.1002/hec.3976
- Lucie Schmidt, Lara Shore-Sheppard, and Tara Watson, The Impact of the ACA Medicaid Expansion on Disability Program Applications (National Bureau of Economic Research, Working Paper No. 26192, August 2019), http://www.nber.org/papers/w26192
- Jean Hall, Adele Shartzer, Noelle Kurth, and Kathleen Thomas, “Medicaid Expansion as an Employment Incentive Program for People With Disabilities,” American Journal of Public Health epub ahead of print (July 2018), https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.2018.304536
- Kevin Callison and Paul Sicilian, “Economic Freedom and the Affordable Care Act: Medicaid Expansions and Labor Mobility by Race and Ethnicity,” Public Finance Review 46, no. 2 (March 2018), https://journals.sagepub.com/doi/abs/10.1177/1091142116668254
- Aparna Soni, Marguerite Burns, Laura Dague, and Kosali Simon, “Medicaid Expansion and State Trends in Supplemental Security Income Program Participation,” Health Affairs 36 no. 8, (August 2017): 1485-1488, http://content.healthaffairs.org/content/36/8/1485.full?sid=982b20c0-0a17-4dc4-a35a-b0302d4ec289
- Pauline Leung and Alexandre Mas, Employment Effects of the ACA Medicaid Expansions (Working Paper No. 22540, National Bureau of Economic Research, August 2016), http://www.nber.org/papers/w22540
- Angshuman Gooptu, Asako Moriya, Kosali Simon, and Benjamin Sommers, “Medicaid Expansion Did Not Result in Significant Employment Changes or Job Reductions in 2014,” Health Affairs 35, no. 1 (January 2016): 111-118, 1-12, http://content.healthaffairs.org/content/35/1/111.short
- Robert Kaestner, Bowen Garrett, Anuj Gangopadhyaya, and Caitlyn Fleming, Effects of ACA Medicaid Expansions on Health Insurance Coverage and Labor Supply (Working Paper No. 21836, National Bureau of Economic Research, December 2015), http://www.nber.org/papers/w21836
- Bowen Garrett and Robert Kaestner, Recent Evidence on the ACA and Employment: Has the ACA Been a Job Killer? (Washington, DC: The Urban Institute and the Robert Wood Johnson Foundation, August 2015), http://www.urban.org/research/publication/recent-evidence-aca-and-employment-has-aca-been-job-killer/view/full_report
MULTI-STATE STUDIES (back to top)
- Priyanka Anand, Jody Schimmel Hyde, Maggie Colby, and Paul O’Leary, “The Impact of Affordable Care Act Medicaid Expansions on Applications to Federal Disability Programs,” Forum for Health Economics and Policy (February 2019), https://www.ncbi.nlm.nih.gov/pubmed/30796844
- Bryce Ward and Brandon Bridge, The Economic Impact of Medicaid Expansion in Montana: Updated Findings (Bureau of Business and Economic Research, January 2019), https://mthcf.org/wp-content/uploads/2019/01/Economic-Impact-of-MedEx-in-MT_1.28.19-FINAL.pdf
SINGLE STATE STUDIES (back to top)
- Renuka Tipirneni et al., “Association of Expanded Medicaid Coverage With Health and Job-Related Outcomes Among Enrollees With Behavioral Health Disorders,” Psychiatric Services Epub ahead of print (September 2019), https://doi.org/10.1176/appi.ps.201900179
- James A. Richardson, Jared J. Llorens, and Roy L. Heidelberg. Medicaid Expansion and the Louisiana Economy, 2018 and 2019 (Louisiana Department of Health, Prepared by Louisiana State University, August 2019), http://ldh.la.gov/assets/media/3and4.2019FinalReportMedicaidExpansionstudy.pdf
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf
- Susan Dorr Goold et al., “Primary Care Clinicians’ Views About the Impact of Medicaid Expansion in Michigan: A Mixed Methods Study,” Journal of General Internal Medicine 33, no. 8 (June 2018): 1307-1316, https://link.springer.com/article/10.1007/s11606-018-4487-6
- James Richardson, Jared Llorens, and Roy Heidelberg, Medicaid Expansion and the Louisiana Economy (Louisiana Department of Health, March 2018), http://gov.louisiana.gov/assets/MedicaidExpansion/MedicaidExpansionStudy.pdf
- John Ayanian, Gabriel Ehrlich, Donald Grimes, and Helen Levy, “Economic Effects of Medicaid Expansion in Michigan,” The New England Journal of Medicine epub ahead of print (January 2017), http://www.nejm.org/doi/full/10.1056/NEJMp1613981
- The Colorado Health Foundation, Assessing the Economic and Budgetary Impact of Medicaid Expansion in Colorado, (The Colorado Health Foundation, March 2016), https://www.coloradohealth.org/sites/default/files/documents/2017-01/Medicaid_ExecutiveSummary_ONLINE.pdf
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf
Additional Emerging Studies (back to top)
- Michel Boudreaux, James M. Noon, Brett Fried, and Joanne Pascale, “Medicaid Expansion and the Medicaid Undercount in the American Community Survey,” Health Services Research 54, no. 6 (December 2019): 1263-1272, https://doi.org/10.1111/1475-6773.13213
- Emily Brown, Michelle Garrison, Hao Bao, Pingping Qu, Carole Jenny, and Ali Rowhani-Rahbar, “Assessment of Rates of Child Maltreatment in States With Medicaid Expansion vs States Without Medicaid Expansion,” JAMA Network Open 2, no. 6 (June 2019), https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2735758
- Daniel Hopkins and Kalind Parish, “The Medicaid Expansion and Attitudes toward the Affordable Care Act: Testing for a Policy Feedback on Mass Opinion,” Public Opinion Quarterly 83, no. 1 (April 2019): 123-134, https://academic.oup.com/poq/article-abstract/83/1/123/5430239
- Richard Fording and Dana Patton, “Medicaid Expansion and the Political Fate of the Governors Who Support It,” Policy Studies Journal 47, no. 2 (January 2019), https://onlinelibrary.wiley.com/doi/full/10.1111/psj.12311
- Joshua Clinton and Michael Sances, “The Politics of Policy: The Initial Mass Political Effects of Medicaid Expansion in the States,” American Political Science Review 112, no. 1 (February 2018): 167-185, https://www.cambridge.org/core/journals/american-political-science-review/article/politics-of-policy-the-initial-mass-political-effects-of-medicaid-expansion-in-the-states/246AA0F10B44EFD62A7B27C661730823
- Jake Haselswerdt, “Expanding Medicaid, Expanding the Electorate: The Affordable Care Act’s Short-Term Impact on Political Participation,” Journal of Health Politics, Policy, and Law 42, no. 4 (August 2017), https://read.dukeupress.edu/jhppl/article-abstract/42/4/667/130386/Expanding-Medicaid-Expanding-the-Electorate-The?redirectedFrom=fulltext
- Michael Sances and Joshua Clinton, New Policy, New Politics? The Effect of Medicaid Expansion on Public Support for the Affordable Care Act, (University of Memphis and Vanderbilt University, February 2017), https://csap.yale.edu/sites/default/files/files/apppw_jc2_3-8-17.pdf
- David Slusky and Donna Ginther, Did Medicaid Expansion Reduce Medical Divorce? (Working Paper No. 23139, National Bureau of Economic Research, February 2017), http://www.nber.org/papers/w23139?utm_campaign=ntw&utm_medium=email&utm_source=ntw
- Lucas Goodman, “The Effect of the Affordable Care Act Medicaid Expansion on Migration,” Journal of Policy Analysis 36, no. 1 (November 2016): 211-238, http://onlinelibrary.wiley.com/doi/10.1002/pam.21952/abstract
Bibliography
- Jean M. Abraham, Anne B. Royalty, and Coleman Drake, “The Impact of Medicaid Expansion on Employer Provision of Health Insurance,” International Journal of Health Economics and Management 19, no. 3-4 (December 2019): 317-340, https://doi.org/10.1007/s10754-018-9256-x
- Amanda Abraham et al., “Changes in State Technical Assistance Priorities and Block Grant Funds for Addiction After ACA Implementation,” American Journal of Public Health epub ahead of print (May 2019), https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2019.305052
- Andrew Admon, Thomas Valley, John Ayanian, Theodore Iwashyna, Colin Cooke, and Renuka Tipirneni, “Trends in Hospital Utilization After Medicaid Expansion,” Medical Care 57, no. 4 (April 2019): 312-317, https://journals.lww.com/lww-medicalcare/Abstract/publishahead/Brief_Report__Trends_in_Hospital_Utilization_After.98489.aspx
- Andrew Admon, Michael Sjoding, Sarah Lyon, John Ayanian, Theodore Iwashyna, and Colin Cooke, “Medicaid Expansion and Mechanical Ventilation in Asthma, Chronic Obstructive Pulmonary Disease, and Heart Failure,” Annals of the American Thoracic Society epub ahead of print (February 2019), https://www.atsjournals.org/doi/pdf/10.1513/AnnalsATS.201811-777OC
- Sumit D. Agarwal, Anna L. Goldman, and Benjamin D. Sommers, “Blue-Collar Workers Had Greatest Insurance Gains After ACA Implementation,” Health Affairs 38, no. 7 (July 2019): 1140-1144, https://doi.org/10.1377/hlthaff.2018.05454
- Ankit Agarwal, Aaron Katz, and Ronald Chen, “The Impact of the Affordable Care Act on Disparities in Private and Medicaid Insurance Coverage among Patients Under 65 with Newly Diagnosed Cancer,” International Journal of Radiation Oncology, Biology, Physics (May 2019), https://www.redjournal.org/article/S0360-3016(19)30783-7/pdf
- Nicolas Ajkay et al, “Early Impact of Medicaid Expansion and Quality of Breast Cancer Care in Kentucky,” Journal of the American College of Surgeons, epub ahead of print, February 2018, https://www.sciencedirect.com/science/article/pii/S107275151830022X
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562
- Manzilat Akande Peter Minneci, Katherine Deans, Henry Xiang, and Jennifer Cooper, “Association of Medicaid Expansion Under the Affordable Care Act With Outcomes and Access to Rehabilitation in Young Adult Trauma Patients,” JAMA Surgery 153, no. 8 (August 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2682872?widget=personalizedcontent&previousarticle=2719270
- Ehimare Akhabue, Lindsay Pool, Clyde Yancy, Philip Greenland, and Donald Lloyd-Jones, “Association of State Medicaid Expansion With Rate of Uninsured Hospitalizations for Major Cardiovascular Events, 2009-2014,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2698077
- Abeer Alharbi, M. Mahmud Khan, Ronnie Horner, Heather Brandt, and Cole Chapman, “Impact Of Medicaid Coverage Expansion Under The Affordable Care Act On Mammography And Pap Tests Utilization Among Low-Income Women,” PLOS One (April 2019), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0214886
- Adam M. Almaguer et al., “Do Geographic Region, Medicaid Status, and Academic Affiliation Affect Access to Care Among Medicaid and Privately Insured Total Hip Arthroplasty Patients?,” Journal of Arthroplasty 34, no. 12 (December 2019): 2866-2871, https://doi.org/10.1016/j.arth.2019.07.030
- Priyanka Anand, Jody Schimmel Hyde, Maggie Colby, and Paul O’Leary, “The Impact of Affordable Care Act Medicaid Expansions on Applications to Federal Disability Programs,” Forum for Health Economics and Policy (February 2019), https://www.ncbi.nlm.nih.gov/pubmed/30796844
- Mary Anderson, Jeffrey Glasheen, Debra Anoff, “Impact of State Medicaid Expansion Status on Length of Stay and In-Hospital Mortality for General Medicine Patients at US Academic Medical Centers,” Journal of Hospital Medicine Epub ahead of print (August 2016), http://onlinelibrary.wiley.com/wol1/doi/10.1002/jhm.2649/citedby
- Christina Andrews et al., “Medicaid Coverage In Substance Use Disorder Treatment After The Affordable Care Act,” Journal of Substance Abuse Treatment epub ahead of print (April 2019), https://www.sciencedirect.com/science/article/pii/S0740547218305750
- Heather Angier et al., “Racial/Ethnic Disparities in Health Insurance and Differences in Visit Type for a Population of Patients with Diabetes after Medicaid Expansion” Journal of Health Care for the Poor and Underserved 30, no.1, (March 2019) 116–130: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6429963/
- Heather Angier et al., “Uninsured Primary Care Visit Disparities under the Affordable Care Act,” Annals of Family Medicine, 15 no. 5 (September 2017): 434-442,http://www.annfammed.org/content/15/5/434.full.pdf+html
- Arkansas Health Reform Legislative Task Force, Health Care Task Force Preliminary Report, (Arkansas Health Reform Legislative Task Force, December 2015), http://www.arkleg.state.ar.us/assembly/2015/Meeting%20Attachments/836/I14218/Task%20Force%20report%2012-17-15%20sent%20to%20Jill.pdf
- Arkansas Hospital Association, “Survey Reveals Private Option Impact on Hospitals,” The Notebook 21, no. 33 (November 2014), http://www.arkhospitals.org/archive/notebookpdf/Notebook_11-03-14.pdf
- Samantha Artiga, Barbara DiPietro, and Petry Ubri, The Role of Medicaid and the Impact of the Medicaid Expansion for Veterans Experiencing Homelessness, (Washington, DC: Kaiser Family Foundation, October 2017), https://www.kff.org/medicaid/issue-brief/the-role-of-medicaid-and-impact-of-the-medicaid-expansion-for-veterans-experiencing-homelessness/
- Samantha Artiga and Robin Rudowitz, How Have State Medicaid Expansion Decisions Affected the Experiences of Low-Income Adults? Perspectives from Ohio, Arkansas, and Missouri (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/medicaid/issue-brief/how-have-state-medicaid-expansion-decisions-affected-the-experiences-of-low-income-adults-perspectives-from-ohio-arkansas-and-missouri/
- Samantha Artiga, Robin Rudowitz, Jennifer Tolbert, Julia Paradise, and Melissa Majerol, Findings from the Field: Medicaid Delivery Systems and Access to Care in Four States in Year Three of the ACA (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, September 2016), http://kff.org/medicaid/issue-brief/findings-from-the-field-medicaid-delivery-systems-and-access-to-care-in-four-states-in-year-three-of-the-aca/
- Samantha Artiga, Jennifer Tolbert, and Robin Rudowitz, Year Two of the ACA Coverage Expansions: On-the-Ground Experiences from Five States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/health-reform/issue-brief/year-two-of-the-aca-coverage-expansions-on-the-ground-experiences-from-five-states/
- Natoshia Askelson, Brad Wright, Suzanne Bentler, Elizabeth Momany, and Peter Damiano, “Iowa’s Medicaid Expansion Promoted Healthy Behaviors But Was Challenging to Implement and Attracted Few Participants,” Health Affairs 36 no. 5, (May 2017): 799-807, http://content.healthaffairs.org/content/36/5/799.full
- Susan L. Averett, Julie K. Smith, and Yang Wang, “Medicaid Expansion and Opioid Deaths,” Health Economics 28, no. 12 (December 2019): 1491-1496, https://doi.org/10.1002/hec.3945
- Kelsey Avery, Kenneth Finegold, and Amelia Whitman, Affordable Care Act Has Led to Historic, Widespread Increase in Health Insurance Coverage (Office of the Assistant Secretary for Planning and Evaluation, September 2016), https://aspe.hhs.gov/sites/default/files/pdf/207946/ACAHistoricIncreaseCoverage.pdf
- John Ayanian, Gabriel Ehrlich, Donald Grimes, and Helen Levy, “Economic Effects of Medicaid Expansion in Michigan,” The New England Journal of Medicine epub ahead of print (January 2017), http://www.nejm.org/doi/full/10.1056/NEJMp1613981
- Deborah Bachrach, Patricia Boozang, Avi Herring, and Dori Glanz Reyneri, States Expanding Medicaid See Significant Budget Savings and Revenue Gains, (Manatt Health Solutions, prepared by the Robert Wood Johnson Foundation’s State Health Reform Assistance Network, March 2016), http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2016/rwjf419097
- Deborah Bachrach, Patricia Boozang, and Mindy Lipson, The Impact of Medicaid Expansion on Uncompensated Care Costs: Early Results and Policy Implications for States, (Manatt Health Solutions, prepared by the Robert Wood Johnson Foundation’s State Health Reform Assistance Network, June 2015), https://www.manatt.com/uploadedFiles/Content/5_Insights/White_Papers/State-Network-Manatt-Impact-of-Medicaid-Expansion-on-Uncompensated-Care-Costs-June-2015.pdf
- Steffani Bailey et al., “Tobacco Cessation in Affordable Care Act Medicaid Expansion States Versus Non-expansion States,” Nicotine & Tobacco Research epub ahead of print (May 2019), https://academic.oup.com/ntr/advance-article-abstract/doi/10.1093/ntr/ntz087/5498071
- Monique Barakat et al., “Affordable Care Act and Healthcare Delivery: A Comparison of California and Florida Hospitals and Emergency Departments,” PLoS ONE 12 no. 8 (August 2017), http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0182346
- Ameen Barghi, Hugo Torres, Nancy Kressin, and Danny McCormick, “Coverage and Access for Americans with Cardiovascular Disease or Risk Factors After the ACA: a Quasi-experimental Study,” Journal of General Internal Medicine epub ahead of print (June 2019), https://link.springer.com/article/10.1007%2Fs11606-019-05108-1
- Abigail Barker, Kelsey Huntzberry, Timothy McBride, and Keith Mueller, Changing Rural and Urban Enrollment in State Medicaid Programs (Iowa City, IA: Rural Policy Research Institute, May 2017), https://cph.uiowa.edu/rupri/publications/policybriefs/2017/Changing%20Rural%20and%20Urban%20Enrollment%20in%20State%20Medicaid%20Programs.pdf
- Stephen Barnes, Mike Henderson, Dek Terrell, and Stephanie Virgets, 2017 Louisiana Health Insurance Survey (Louisiana Department of Health, prepared by the Louisana State University E.J. Ourso College of Business, August 2018), http://ldh.la.gov/assets/media/2017-Louisiana-Health-Insurance-Survey-Report.pdf
- Hilary Barnes, Michael Richards, Matthew McHugh, and Grant Martsolf, “Rural And Nonrural Primary Care Physician Practices Increasingly Rely On Nurse Practitioners,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1158
- Simon Basseyn, Brendan Saloner, Genevieve Kenney, Douglas Wissoker, Daniel Polsky, and Karin Rhodes, Primary Care Appointment Availability for Medicaid Patients: Comparing Traditional and Premium Assistance Plans, (Penn Leonard Davis Institute of Health Economics, July 2016), http://ldi.upenn.edu/brief/primary-care-appointment-availability-medicaid-patients-comparing-traditional-and-premium
- Jesse C. Baumgartner, Sara R. Collins, David C. Radley, and Susan L. Hayes, How the Affordable Care Act Has Narrowed Racial and Ethnic Disparities in Access to Health Care (The Commonwealth Fund, January 2020), https://www.commonwealthfund.org/publications/2020/jan/how-ACA-narrowed-racial-ethnic-disparities-access
- Joseph Benitez, Liza Creel, and J’Aime Jennings, “Kentucky’s Medicaid Expansion Showing Early Promise on Coverage and Access to Care,” Health Affairs (February 2016), http://content.healthaffairs.org/content/early/2016/02/16/hlthaff.2015.1294
- Stephen Berry et al., “Healthcare Coverage for HIV Provider Visits before and after Implementation of the Affordable Care Act,” Clinical Infectious Diseases, (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27143660
- Chintan Bhatt and Consuelo Beck-Sague, “Medicaid Expansion and Infant Mortality in the United States,” American Journal of Public Health 108, no. 4 (April 2018): 565-567, https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2017.304218
- Neal Bhutiani, Brian Harbrecht, Charles Scoggins, and Matthew Bozeman, “Evaluating The Early Impact Of Medicaid Expansion On Trends In Diagnosis And Treatment Of Benign Gallbladder Disease In Kentucky,” The American Journal of Surgery (January 2019), https://www.americanjournalofsurgery.com/article/S0002-9610(18)30894-8/fulltext
- Bernard Black, Alex Hollingsworth, Leticia Nunes, and Kosali Simon, The Effect of Health Insurance on Mortality: Power Analysis and What We Can Learn from the Affordable Care Act Coverage Expansions, (National Bureau of Economic Research, Working Paper Series No. 25568, February 2019), https://www.nber.org/papers/w25568
- Fredric Blavin, “Association Between the 2014 Medicaid Expansion and US Hospital Finances,” The Journal of the American Medical Association 316 no. 14 (October 2016): 1475-1483, http://jamanetwork.com/journals/jama/article-abstract/2565750
- Fredric Blavin, How Has the ACA Changed Finances for Different Types of Hospitals? Updated Insights from 2015 Cost Report Data (The Urban Institute, April 2017), http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2017/rwjf436310
- Fredric Blavin, Impact of the Affordable Care Act’s Medicaid Expansion on Medicare Enrollees’ Access to Physician Services (Washington, DC: The Urban Institute, August 2019), https://www.urban.org/research/publication/effect-affordable-care-act-medicare-enrollees-access-physician-services
- Frederic Blavin, Michael Karpman, Genevieve Kenney, and Benjamin Sommers, “Medicaid Versus Marketplace Coverage for Near-Poor Adults: Effects on Out-Of-Pocket Spending and Coverage,” Health Affairs 37 no. 2 (January 2018), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.1166
- Michel Boudreaux, Yoon Choi, Liyang Xie, and Daniel Marthey, “Medicaid Expansion at Title X Clinics: Client Volume, Payer Mix, and Contraceptive Method Type,” Medical Care epub ahead of print (April 2019), https://www.ncbi.nlm.nih.gov/pubmed/30973473
- Michel Boudreaux, James M. Noon, Brett Fried, and Joanne Pascale, “Medicaid Expansion and the Medicaid Undercount in the American Community Survey,” Health Services Research 54, no. 6 (December 2019): 1263-1272, https://doi.org/10.1111/1475-6773.13213
- Khadijah Breathett et al., “The Affordable Care Act Medicaid Expansion Correlated with Increased Heart Transplant Listings in African Americans but Not Hispanics or Caucasians,” JACC: Heart Failure 5 no. 2 (January 2017): 136-147, https://www.ncbi.nlm.nih.gov/pubmed/28109783
- Kenneth Brevoort, Daniel Grodzicki, and Martin Hackmann, Medicaid and Financial Health (National Bureau of Economic Research, Working Paper No. 24002, November 2017), http://www.nber.org/papers/w24002
- Chris Brown and John Bennett, Economic Impacts of the Arkansas Private Option (Regional Economic Models, Inc., August 2015), http://www.arkhospitals.org/Misc.%20Files/August2015APOEconomicImpacts.pdf
- Emily Brown, Michelle Garrison, Hao Bao, Pingping Qu, Carole Jenny, and Ali Rowhani-Rahbar, “Assessment of Rates of Child Maltreatment in States With Medicaid Expansion vs States Without Medicaid Expansion,” JAMA Network Open 2, no. 6 (June 2019), https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2735758
- Clare Brown et al., “Association of State Medicaid Expansion Status With Low Birth Weight and Preterm Birth” Journal of the American Medical Association 321, no. 16 (April 2019), https://jamanetwork.com/journals/jama/fullarticle/2731179
- Elizabeth A. Brown et al., “The Impact of the ACA Medicaid Expansion on Access to Care and Hospitalization Charges for Lupus Patients,” Arthritis Care & Research Epub ahead of print (September 2019), https://doi.org/10.1002/acr.24080
- Thomas Buchmueller, Zachary Levinson, Helen Levy, and Barbara Wolfe, “Effect of the Affordable Care Act on Racial and Ethnic Disparities in Health Insurance Coverage,” American Journal of Public Health (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27196653
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553
- Kevin Callison and Paul Sicilian, “Economic Freedom and the Affordable Care Act: Medicaid Expansions and Labor Mobility by Race and Ethnicity,” Public Finance Review 46, no. 2 (March 2018), https://journals.sagepub.com/doi/abs/10.1177/1091142116668254
- Susan Camilleri, “The ACA Medicaid Expansion, Disproportionate Share Hospitals, and Uncompensated Care” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12702/abstract
- Molly Candon et al., Primary Care Appointment Availability and the ACA Insurance Expansions (Philadelphia, PA: University of Pennsylvania Leonard Davis Institute of Health Economics, March 2017), https://ldi.upenn.edu/brief/primary-care-appointment-availability-and-aca-insurance-expansions
- Colleen M. Carey, Sarah Miller, and Laura R. Wherry, “The Impact of Insurance Expansions on the Already Insured: The Affordable Care Act and Medicare,” National Bureau of Economic Research Working Paper Series No. 25153 (October 2018), https://www.nber.org/papers/w25153
- Kyle Caswell and Timothy Waidmann, The Affordable Care Act Medicaid Expansions and Personal Finance (Washington, DC: The Urban Institute, September 2017), https://www.urban.org/research/publication/affordable-care-act-medicaid-expansions-and-personal-finance
- John Cawley, Aparna Soni, and Kosali Simon, “Third Year of Survey Data Shows Continuing Benefits of Medicaid Expansions for Low-Income Childless Adults in the U.S.,” Journal of General Internal Medicine 33, no. 9 (September 2018): 1495-1497, https://link.springer.com/article/10.1007%2Fs11606-018-4537-0
- Centers for Medicare and Medicaid Services, Monthly Medicaid and CHIP Application, Eligibility, Determination, and Enrollment Reports, (Centers for Medicare and Medicaid Services, March 2016), https://www.medicaid.gov/medicaid-chip-program-information/program-information/medicaid-and-chip-enrollment-data/medicaid-and-chip-application-eligibility-determination-and-enrollment-data.html
- Natalia Chalmers, Jane Grover, and Rob Compton, “After Medicaid Expansion in Kentucky, Use of Hospital Emergency Departments for Dental Conditions Increased,” Health Affairs 35, no. 12 (December 2016), http://content.healthaffairs.org/content/35/12/2268.full#xref-ref-32-1
- Eric Charles et al., “Impact of Medicaid Expansion on Cardiac Surgery Volume and Outcomes,” The Annals of Thoracic Surgery (June 2017), http://www.annalsthoracicsurgery.org/article/S0003-4975(17)30552-0/pdf
- Evan M. Chen et al., “Association of the Affordable Care Act Medicaid Expansion with Dilated Eye Examinations among the United States Population with Diabetes,” Ophthalmology Epub ahead of print (September 2019), https://doi.org/10.1016/j.ophtha.2019.09.010
- Benjamin Cher, Nancy Morden, and Ellen Meara, “Medicaid Expansion and Prescription Trends: Opioids, Addiction Therapies, and Other Drugs,” Medical Care 57, no. 3 (March 2019): 208-212, https://journals.lww.com/lww-medicalcare/fulltext/2019/03000/Medicaid_Expansion_and_Prescription_Trends_.6.aspx
- Fumiko Chino, Gita Suneja, Haley Moss, S. Yousuf Zafar, Laura Havrilesky, and Junzo Chino, “Healthcare Disparities in Cancer Patients Receiving Radiation: Changes in Insurance Status After Medicaid Expansion Under the Affordable Care Act,” International Journal of Radiation Oncology (December 2017), http://www.sciencedirect.com/science/article/pii/S0360301617341883
- Sunha Choi, Sungkyu Lee, and Jason Matejkowski, “The Effects of State Medicaid Expansion on Low-Income Individuals’ Access to Health Care: Multilevel Modeling,” Population Health Management epub ahead of print (September 2017), http://online.liebertpub.com/doi/abs/10.1089/pop.2017.0104
- Mark Clapp et al., “Association of Medicaid Expansion With Coverage and Access to Care for Pregnant Women,” Obstetrics & Gynecology 134, no. 5 (November 2019): 1066-1074, https://doi.org/10.1097/aog.0000000000003501
- Lisa Clemans-Cope, Marni Epstein, Victoria Lynch, and Emma Winiski, Rapid Growth in Medicaid Spending and Prescriptions to Treat Opioid Use Disorder and Opioid Overdose from 2010 to 2017 (Washington, DC: The Urban Institute, March 2019), https://www.urban.org/sites/default/files/publication/99798/rapid_growth_in_medicaid_spending_and_prescriptions_to_treat_opioid_use_disorder_and_opioid_overdose_from_2010_to_2017_2.pdf
- Lisa Clemans-Cope, Victoria Lynch, Marni Epstein, and Genevieve Kenney, Medicaid Coverage of Effective Treatment for Opioid Use Disorder, (Washington, DC: The Urban Institute, June 2017), https://www.urban.org/sites/default/files/publication/90461/2001287_medicaid_coverage_of_effective_treatment_for_opioid_use_disorder.pdf
- Lisa Clemans-Cope, Victoria Lynch, Emma Winiski, and Marni Epstein, State Variation in Medicaid Prescriptions for Opioid Use Disorder from 2011 to 2018 (Washington, DC: The Urban Institute, August 2019), https://www.urban.org/research/publication/state-variation-medicaid-prescriptions-opioid-use-disorder-2011-2018
- Joshua Clinton and Michael Sances, “The Politics of Policy: The Initial Mass Political Effects of Medicaid Expansion in the States,” American Political Science Review 112, no. 1 (February 2018): 167-185, https://www.cambridge.org/core/journals/american-political-science-review/article/politics-of-policy-the-initial-mass-political-effects-of-medicaid-expansion-in-the-states/246AA0F10B44EFD62A7B27C661730823
- Michael Cohen and William Schpero, “Household Immigration Status Had Differential Impact On Medicaid Enrollment In Expansion And Nonexpansion States,” Health Affairs 37, no. 3 (March 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.0978
- Robin Cohen, Emily Terlizzi, and Michael Martinez, Health Insurance Coverage: Early Release of Estimates from the National Health Interview Survey, 2018 (National Center for Health Statistics, May 2019), https://www.cdc.gov/nchs/data/nhis/earlyrelease/insur201905.pdf
- Megan Cole, Omar Galarraga, Ira Wilson, Brad Wright, and Amal Trivedi, “At Federally Funded Health Centers, Medicaid Expansion was Associated with Improved Quality of Care,” Health Affairs 36 no. 1 (January 2017): 40-48, http://content.healthaffairs.org/content/36/1/40.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19
- Megan Cole, Brad Wright, Ira Wilson, Omar Gallarraga, and Amal Trivedi, “Medicaid Expansion And Community Health Centers: Care Quality And Service Use Increased For Rural Patients” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1542
- Sara Collins, Munira Gunja, Michelle Doty, and Sophie Beutel, Americans’ Experiences with ACA Marketplace and Medicaid Coverage: Access to Care and Satisfaction (The Commonwealth Fund, May 2016), http://www.commonwealthfund.org/publications/issue-briefs/2016/may/aca-tracking-survey-access-to-care-and-satisfaction
- Sara Collins, Petra Rasmussen, Michelle Doty, and Sophie Beutel The Rise in Health Care Coverage and Affordability Since Health Reform Took Effect: Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2014 (The Commonwealth Fund, January 2015), http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2015/jan/1800_collins_biennial_survey_brief.pdf?la=en
- The Colorado Health Foundation, Assessing the Economic and Budgetary Impact of Medicaid Expansion in Colorado, (The Colorado Health Foundation, March 2016), https://www.coloradohealth.org/sites/default/files/documents/2017-01/Medicaid_ExecutiveSummary_ONLINE.pdf
- The Colorado Health Institute, Medicaid Expansion in Colorado: An Analysis of Enrollment, Costs and Benefits—and How They Exceeded Expectations (The Colorado Health Institute, May 2016), http://www.coloradohealthinstitute.org/uploads/postfiles/MK_Expansion_Report.pdf
- Colorado Hospital Association, Impact of Medicaid Expansion on Hospital Volumes (Colorado Hospital Association Center for Health Information and Data Analytics, June 2014), http://www.cha.com/documents/press-releases/cha-medicaid-expansion-study-june-2014.aspx
- Kelsey L. Corrigan et al., “The Impact of the Patient Protection and Affordable Care Act on Insurance Coverage and Cancer-Directed Treatment in HIV-Infected Patients With Cancer in the United States,” Cancer (November 2019), https://doi.org/10.1002/cncr.32563
- Chad Cotti, Erik Nesson, and Nathan Tefft, “Impacts Of The ACA Medicaid Expansion On Health Behaviors: Evidence From Household Panel Data,” Health Economics 28, no. 2 (February 2019): 219-244, https://onlinelibrary.wiley.com/doi/pdf/10.1002/hec.3838
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, Early Effects of the Affordable Care Act on Health Care Access, Risky Health Behaviors, and Self-Assessed Health (National Bureau of Economic Research, Working Paper no. 23269, March 2017), http://www.nber.org/papers/w23269
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, and Daniela Zapata, Impacts of the Affordable Care Act on Health Insurance Coverage in Medicaid Expansion and Non-Expansion States (Working Paper No. 22182, The National Bureau of Economic Research, April 2016), http://www.nber.org/papers/w22182
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, and Ishtiaque Fazlul, “The Three‐Year Impact of the Affordable Care Act on Disparities in Insurance Coverage,” Health Services Research (October 2018), https://onlinelibrary.wiley.com/doi/10.1111/1475-6773.13077
- Charles J. Courtemanche, James Marton, and Aaron Yelowitz, Medicaid Coverage across the Income Distribution under the Affordable Care Act (National Bureau of Economic Research, Working Paper No. 26145, August 2019), http://www.nber.org/papers/w26145
- Charles J. Courtemanche et al., The Impact of the ACA on Insurance Coverage Disparities After Four Years (National Bureau of Economic Research, Working Paper No. 26157, August 2019), http://www.nber.org/papers/w26157
- Andrew Crocker et al., “The Affordable Care Act’s Medicaid Expansion And Utilization Of Discretionary Vs. Non-Discretionary Inpatient Surgery,” Surgery 164, no. 6 (December 2018): 1156-1161, https://www.sciencedirect.com/science/article/pii/S0039606018302186
- Andrew Crocker et al., “Expansion Coverage And Preferential Utilization Of Cancer Surgery Among Racial And Ethnic Minorities And Low-Income Groups,” Surgery epub ahead of print (June 2019), https://www.surgjournal.com/article/S0039-6060(19)30198-9/fulltext
- Peter Cunningham, Rachel Garfield, and Robin Rudowitz, How Are Hospitals Faring Under the Affordable Care Act? Early Experiences from Ascension Health (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, April 2015), http://kff.org/health-reform/issue-brief/how-are-hospitals-faring-under-the-affordable-care-act-early-experiences-from-ascension-health/
- Peter Cunningham, Robin Rudowitz, Katherine Young, Rachel Garfield, and Julia Foutz, Understanding Medicaid Hospital Payments and the Impact of Recent Policy Changes (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2016), http://kff.org/medicaid/issue-brief/understanding-medicaid-hospital-payments-and-the-impact-of-recent-policy-changes/
- Charles A. Daly et al., “The Effects of Medicaid Expansion on Triage and Regional Transfer After Upper-Extremity Trauma,” The Journal of Hand Surgery 44, no. 9 (September 2019): 720-727, https://doi.org/10.1016/j.jhsa.2019.05.020
- Amy Davidoff et al., “Changes in Health Insurance Coverage Associated With the Affordable Care Act Among Adults With and Without a Cancer History: Population-based National Estimates,” Medical Care 56, no. 3 (March 2018), https://journals.lww.com/lww-medicalcare/Abstract/2018/03000/Changes_in_Health_Insurance_Coverage_Associated.5.aspx
- Mathew Davis, Achamyeleh Gebremariam, John Ayanian, “Changes in Insurance Coverage Among Hospitalized Nonelderly Adults After Medicaid Expansion in Michigan,” The Journal of the American Medical Association 315 no. 23 (June 2016): 2617-2618, http://jamanetwork.com/journals/jama/fullarticle/2529615
- Lindsey Dawson, Jennifer Kates, and Anthony Damico, The Affordable Care Act and Insurance Coverage Changes by Sexual Orientation (Washington, DC: Kaiser Family Foundation, January 2018), https://www.kff.org/disparities-policy/issue-brief/the-affordable-care-act-and-insurance-coverage-changes-by-sexual-orientation/
- Sandra Decker and Brandy Lipton, “Most Newly Insured People in 2014 Were Long-Term Uninsured,” Health Affairs 36 no. 1 (January 2017): 16-20, http://content.healthaffairs.org/content/36/1/16.full?sid=982b20c0-0a17-4dc4-a35a-b0302d4ec289
- Sandra Decker, Brandy Lipton, and Benjamin Sommers, “Medicaid Expansion Coverage Effects Grew in 2015 With Continued Improvements in Coverage Quality,” Health Affairs 36 no. 5 (May 2017): 819-825, http://content.healthaffairs.org/content/36/5/819.full
- Thomas DeLeire, Karen Joynt, and Ruth McDonald, Impact of Insurance Expansion on Hospital Uncompensated Care Costs in 2014 (Office of the Assistant Secretary for Planning and Evaluation, September 2014), https://aspe.hhs.gov/sites/default/files/pdf/77061/ib_UncompensatedCare.pdf
- Alina Denham and Peter Veazie, “Did Medicaid Expansion Matter in States with Generous Medicaid?” The American Journal of Managed Care 25, no. 3 (March 2019): 129-134, https://www.ajmc.com/journals/issue/2019/2019-vol25-n3/did-medicaid-expansion-matter-in-states-with-generous-medicaid
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf
- Mark L. Diana et al., Louisiana Medicaid Expansion and Access to Care (Louisiana Department of Health, Prepared by Tulane University, July 2019), http://ldh.la.gov/assets/media/AccesstoCareReport20132018final.pdf
- Anne DiGiulio et al., “State Medicaid Expansion Tobacco Cessation Coverage and Number of Adult Smokers Enrolled in Expansion Coverage – United States, 2016,” Morbidity and Mortality Weekly Report 65, no. 48 (December 2016), https://www.cdc.gov/mmwr/volumes/65/wr/mm6548a2.htm
- Barbara DiPietro, Samantha Artiga, and Alexandra Gates, Early Impacts of the Medicaid Expansion for the Homeless Population (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, November 2014), http://kff.org/uninsured/issue-brief/early-impacts-of-the-medicaid-expansion-for-the-homeless-population/
- Allen Dobson, Joan DaVanzo, Randy Haught, and Phap Hoa Luu, Comparing the Affordable Care Act’s Financial Impact on Safety-Net Hospitals in States that Expanded Medicaid and Those That Did Not (The Commonwealth Fund, November 2017), http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2017/nov/dobson_impact_medicaid_expanion_safety_net_hosps_ib.pdf
- Travis Donahoe et al., “The Affordable Care Act Medicaid Expansion and Smoking Cessation Among Low-Income Smokers,” American Journal of Preventive Medicine 57, no. 6 (December 2019): 203-210, https://doi.org/10.1016/j.amepre.2019.07.004
- Stan Dorn, Norton Francis, Laura Snyder, and Robin Rudowitz, The Effects of the Medicaid Expansion on State Budgets: An Early Look in Select States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, March 2015), http://kff.org/medicaid/issue-brief/the-effects-of-the-medicaid-expansion-on-state-budgets-an-early-look-in-select-states/
- David Dranove, Craig Garthwaite, and Christopher Ody, The Impact of the ACA’s Medicaid Expansion on Hospitals’ Uncompensated Care Burden and the Potential Effects of Repeal, (The Commonwealth Fund, May 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/may/aca-medicaid-expansion-hospital-uncompensated-care
- David Dranove, Craig Garthwaite, and Christopher Ody, “Uncompensated Care Decreased At Hospitals In Medicaid Expansion States But Not At Hospitals In Nonexpansion States,” Health Affairs 35 no. 8 (August 2016): 1471-1479, http://content.healthaffairs.org/content/35/8/1471.full
- Mark Duggan, Atul Gupta, and Emilie Jackson, The Impact of the Affordable Care Act: Evidence from California’s Hospital Sector (National Bureau of Economic Research, working paper no. 25488, January 2019), https://www.nber.org/papers/w25488.pdf
- Michael Dworsky and Christine Eibner, The Effect of the 2014 Medicaid Expansion on Insurance Coverage for Newly Eligible Childless Adults (Santa Monica, CA: Rand Corporation, 2016), https://www.rand.org/pubs/research_reports/RR1736.html
- Michael Dworsky, Carrie Farmer, and Mimi Shen, Veterans’ Health Insurance Coverage Under the Affordable Care Act and Implications of Repeal for the Department of Veterans Affairs, (RAND Corporation, 2017), https://www.rand.org/pubs/research_reports/RR1955.html
- Emanuel Eguia et al., “The Impact of the Affordable Care Act (ACA) Medicaid Expansion on Access to Minimally Invasive Surgical Care,” The American Journal of Surgery Epub ahead of print (July 2019), https://doi.org/10.1016/j.amjsurg.2019.07.003
- Emanuel Eguia et al., “Impact of the Affordable Care Act (ACA) Medicaid Expansion on Cancer Admissions and Surgeries,” Annals of Surgery 268, no. 4 (October 2018): 584-590, https://journals.lww.com/annalsofsurgery/Abstract/2018/10000/Impact_of_the_Affordable_Care_Act__ACA__Medicaid.6.aspx
- Emanuel Eguia et al., “The Impact of the Affordable Care Act Medicaid Expansion on Vascular Surgery,” Annals of Vascular Surgery Epub ahead of print (January 2020), https://doi.org/10.1016/j.avsg.2020.01.006
- Afshin Ehsan et al., “Utilization of Left Ventricular Assist Devices in Vulnerable Adults Across Medicaid Expansion,” Journal of Surgical Research 243 (November 2019): 503-508, https://doi.org/10.1016/j.jss.2019.05.015
- Hawazin W. Elani, Ichiro Kawachi, and Benjamin D. Sommers, “Changes in Emergency Department Dental Visits after Medicaid Expansion,” Health Services Research Epub ahead of print (January 2020), https://doi.org/10.1111/1475-6773.13261
- Mohammad Eslami et al., “Impact of Medicaid Expansion of the Affordable Care on the Outcomes of Lower Extremity Bypass for Patients With Peripheral Artery Disease in the Vascular Quality Initiative Database,” Annals of Surgery 270, no. 4 (October 2019): 647-655, https://doi.org/10.1097/sla.0000000000003521
- Abby Evans, John Folkemer, Joel Menges, Amira Mouna, Nick Pantaleo, Emily Ricci, and Poornima Sigh, Assessment of Medicaid Expansion and Reform, Initial Analysis (The Menges Group, January 2016), https://alaskamentalhealthtrust.org/wp-content/uploads/2018/08/HandOut-MedicaidExpansionAndReformInitialAnalysis-011516-TheMengesGroup.pdf
- Stacey Fedewa, K. Robin Yabroff, Robert Smith, Ann Goding Sauer, Xuesong Han, and Ahmedin Jemal, “Changes in Breast and Colorectal Cancer Screening After Medicaid Expansion Under the Affordable Care Act,” American Journal of Preventive Medicine epub ahead of print (May 2019), https://www.sciencedirect.com/science/article/pii/S0749379719301163
- Laurie Felland, Peter Cunningham, Annie Doubleday, and Cannon Warren, Effects of the Affordable Care Act on Safety Net Hospitals (Washington, DC: Mathematica Policy Research, prepared for the Assistant Secretary for Planning and Evaluation, November 2016), https://aspe.hhs.gov/sites/default/files/pdf/255491/SafetyNetHospital.pdf
- Angela Fertig, Caroline Carlin, Scote Ode, and Sharon Long, “Evidence of Pent-Up Demand for Care After Medicaid Expansion,” Medical Care Research and Review epub ahead of print (March 2017), http://journals.sagepub.com/eprint/wDsfA74fuA3BIw5ZWyYT/full
- Jacqueline Fiore, The Impact of the Affordable Care Act’s Medicaid Expansion on Medicaid Spending by Health Care Service Category (Tulane University, July 2017), http://econ.tulane.edu/RePEc/pdf/tul1706.pdf
- Rene Flores and Robert Vargas, “Medicaid Expansion And Ethnoracial Disparities In Health Insurance Coverage,” Journal of Ethnic and Migration Studies 43, no. 12 (June 2017), https://www.tandfonline.com/doi/full/10.1080/1369183X.2017.1323451?needAccess=true
- Richard Fording and Dana Patton, “Medicaid Expansion and the Political Fate of the Governors Who Support It,” Policy Studies Journal 47, no. 2 (January 2019), https://onlinelibrary.wiley.com/doi/full/10.1111/psj.12311
- Julia Foutz, Samantha Artiga, and Rachel Garfield, The Role of Medicaid in Rural America (Washington, DC: Kaiser Family Foundation, April 2017), http://kff.org/medicaid/issue-brief/the-role-of-medicaid-in-rural-america/
- Richard Frank and Carrie Fry, “The Impact of Expanded Medicaid Eligibility on Access To Naloxone,” Addiction epub ahead of print (April 2019), https://onlinelibrary.wiley.com/doi/abs/10.1111/add.14634
- Taressa K. Fraze et al., “Prevalence of Screening for Food Insecurity, Housing Instability, Utility Needs, Transportation Needs, and Interpersonal Violence by US Physician Practices and Hospitals,” JAMA Network Open 2, no. 9 (September 2019), https://doi.org/10.1001/jamanetworkopen.2019.11514
- Molly Frean, Jonathan Gruber, and Benjamin Sommers, Premium Subsidies, the Mandate, and Medicaid Expansion: Coverage Effects of the Affordable Care Act (Working Paper No. 22213, National Bureau of Economic Research, April 2016), http://www.nber.org/papers/w22213?utm_campaign=ntw&utm_medium=email&utm_source=ntw
- Seth Freedman, Sayeh Nikpay, Aaron Carroll, and Kosali Simon, “Changes in inpatient payer-mix and hospitalizations following Medicaid expansion: Evidence from all-capture hospital discharge data,” PLoS One 12 no. 9 (September 2017), http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0183616
- Seth Freedman, Lilliard Richardson, and Kosali Simon, “Learning From Waiver States: Coverage Effects Under Indiana’s HIP Medicaid Expansion,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1596
- Carrie Fry and Benjamin Sommers, “Effect of Medicaid Expansion on Health Insurance Coverage and Access to Care Among Adults With Depression,” Psychiatric Services 69, no. 11 (November 2018), https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201800181
- Yunwei Gai and John Marthinsen, “Medicaid Expansion, HIV Testing, and HIV-Related Risk Behaviors in the United States, 2010-2017,” American Journal of Public Health 109, no. 10 (October 2019): 1404-1412, https://doi.org/10.2105/ajph.2019.305220
- Tong Gan et al., “Impact of the Affordable Care Act on Colorectal Cancer Screening, Incidence, and Survival in Kentucky,” Journal of the American College of Surgeons 228, no. 4 (April 2019): 342-353.e1, https://www.journalacs.org/article/S1072-7515(19)30046-8/fulltext
- Rachel Garfield, Elizabeth Hinton, Elizabeth Cornachione, and Cornelia Hall, Medicaid Managed Care Plans and Access to Care: Results from the Kaiser Family Foundation 2017 Survey of Medicaid Managed Care Plans (Washington, DC: Kaiser Family Foundation, March 2018), https://www.kff.org/medicaid/report/medicaid-managed-care-plans-and-access-to-care-results-from-the-kaiser-family-foundation-2017-survey-of-medicaid-managed-care-plans
- Bowen Garrett and Robert Kaestner, Recent Evidence on the ACA and Employment: Has the ACA Been a Job Killer? (Washington, DC: The Urban Institute and the Robert Wood Johnson Foundation, August 2015), http://www.urban.org/research/publication/recent-evidence-aca-and-employment-has-aca-been-job-killer/view/full_report
- Craig Garthwaite, Tal Gross, Matthew Notowidigdo, and John Graves, “Insurance Expansion and Hospital Emergency Department Access: Evidence from the Affordable Care Act,” Annals of Internal Medicine 166 no. 3 (February 2017): 172-179, http://annals.org/aim/article/2593599/insurance-expansion-hospital-emergency-department-access-evidence-from-affordable-care
- Craig Garthwaite et al., All Medicaid Expansions Are Not Created Equal: The Geography and Targeting of the Affordable Care Act (National Bureau of Economic Research, Working Paper No. 26289, September 2019), http://www.nber.org/papers/w26289
- Ausmita Ghosh, Kosali Simon, and Benjamin Sommers, “The Effect of Health Insurance on Prescription Drug Use Among Low-Income Adults: Evidence from Recent Medicaid Expansions,” Journal of Health Economics 63 (January 2019): 64-80, https://www.sciencedirect.com/science/article/pii/S0167629617300206
- Ausmita Ghosh, Kosali Simon, and Benjamin Sommers, The Effect of State Medicaid Expansions on Prescription Drug Use: Evidence from the Affordable Care Act (Working Paper No. 23044, National Bureau of Economic Research, January 2017), http://www.nber.org/papers/w23044?utm_campaign=ntw&utm_medium=email&utm_source=ntw
- Susannah Gibbs et al., “Evaluating the Effect of Medicaid Expansion on Access to Preventive Reproductive Care for Women in Oregon,” Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.ypmed.2019.105899
- Kurt Gillis, Physicians’ Patient Mix – A Snapshot from the 2016 Benchmark Survey and Changes Associated with the ACA (American Medical Association, October 2017), https://www.ama-assn.org/sites/default/files/media-browser/public/health-policy/PRP-2017-physician-benchmark-survey-patient-mix.pdf
- Daniel Gingold, Rachelle Pierre-Mathieu, Brandon Cole, Andrew Miller, and Joneigh Khaldun, “Impact of the Affordable Care Act Medicaid Expansion on Emergency Department High Utilizers with Ambulatory Care Sensitive Conditions: A Cross-Sectional Study,” The American Journal of Emergency Medicine (January 2017), http://www.sciencedirect.com/science/article/pii/S0735675717300141
- Sherry Glied, Ougni Chakraborty, and Therese Russo, How Medicaid Expansion Affected Out-of-Pocket Health Care Spending for Low-Income Families (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/medicaid-expansion-out-of-pocket-spending-low-income
- Anna L. Goldman and Benjamin D. Sommers, “Among Low-Income Adults Enrolled In Medicaid, Churning Decreased After The Affordable Care Act,” Health Affairs 39, no. 1 (January 2020): 85-93, https://doi.org/10.1377/hlthaff.2019.00378
- Anna Goldman, Steffie Woolhandler, and David Himmelstein, “Out-of-pocket Spending and Premium Contributions After Implementation of the Affordable Care Act,” Journal of the American Medical Association epub ahead of print (January 2018), https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2669908
- Sergio Gonzales and Benjamin Sommers, “Intra-Ethnic Coverage Disparities among Latinos and the Effects of Health Reform” Health Services Research epub ahead of print (June 2017), http://onlinelibrary.wiley.com/wol1/doi/10.1111/1475-6773.12733/full
- Lucas Goodman, “The Effect of the Affordable Care Act Medicaid Expansion on Migration,” Journal of Policy Analysis 36, no. 1 (November 2016): 211-238, http://onlinelibrary.wiley.com/doi/10.1002/pam.21952/abstract
- Susan Dorr Goold et al., “Primary Care Clinicians’ Views About the Impact of Medicaid Expansion in Michigan: A Mixed Methods Study,” Journal of General Internal Medicine 33, no. 8 (June 2018): 1307-1316, https://link.springer.com/article/10.1007/s11606-018-4487-6
- Susan Dorr Goold et al., “Primary Care, Health Promotion, and Disease Prevention with Michigan Medicaid Expansion,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05370-3
- Angshuman Gooptu, Asako Moriya, Kosali Simon, and Benjamin Sommers, “Medicaid Expansion Did Not Result in Significant Employment Changes or Job Reductions in 2014,” Health Affairs 35, no. 1 (January 2016): 111-118, 1-12, http://content.healthaffairs.org/content/35/1/111.short
- Sarah Gordon, Benjamin Sommers, Ira Wilson, Omar Galarraga, and Amal Trivedi, “The Impact of Medicaid Expansion on Continuous Enrollment: a Two State Analysis,” Journal of General Internal Medicine epub ahead of print (June 2019), https://link.springer.com/article/10.1007/s11606-019-05101-8
- Sarah H. Gordon, Benjamin D. Sommers, Ira B. Wilson, and Amal N. Trivedi, “Effects Of Medicaid Expansion On Postpartum Coverage And Outpatient Utilization,” Health Affairs 39, no. 1 (January 2020): 77-84, https://doi.org/10.1377/hlthaff.2019.00547
- Bela Gorman and Jenn Smagula, 2016 Actuarial Analysis of NH Premium Assistance Program, (Gorman Actuarial, Inc., August 2017), https://www.nh.gov/insurance/reports/documents/08-28-17-ga-nh-pap-analysis-final.pdf
- Hiroshi Gotanda, Gerald Kominski, and Yusuke Tsugawa, “Association Between the ACA Medicaid Expansions and Primary Care and Emergency Department Use During the First 3 Years,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05458-w
- Kelsie M. Gould et al., “Bariatric Surgery Among Vulnerable Populations: The Effect of the Affordable Care Act’s Medicaid Expansion,” Surgery 166, no. 5 (November 2019): 820-828, https://doi.org/10.1016/j.surg.2019.05.005
- Government Accountability Office, Behavioral Health: Options for Low-Income Adults to Receive Treatment in Selected States (Washington, DC: Government Accountability Office, June 2015), http://www.gao.gov/assets/680/670894.pdf
- John A. Graves et al., “Medicaid Expansion Slowed Rates of Health Decline for Low-Income Adults in Southern States,” Health Affairs 39, no. 1 (January 2020): 67-76, https://doi.org/10.1377/hlthaff.2019.00929
- Josh Gray, Iyue Sung, and Stewart Richardson, Observations on the Affordable Care Act: 2014 (athenaResearch and Robert Wood Johnson Foundation ACA View Report, February 2015), http://www.athenahealth.com/~/media/athenaweb/files/pdf/acaview_year_end_2014.pdf
- Josh Gray, Anna Zink, and Tony Dreyfus, Effects of the Affordable Care Act Through 2015, (athenaResearch and Robert Wood Johnson Foundation ACA View Report, March 2016), http://www.athenahealth.com/~/media/athenaweb/files/pdf/acaview_tracking_the_impact_of_health_care_reform
- Kevin Griffith, Leigh Evans, and Jacob Bor, “The Affordable Care Act Reduced Socioeconomic Disparities in Health Care Access,” Health Affairs 36 no. 8 (August 2017), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0083
- Kevin N. Griffith, “Changes in Insurance Coverage and Access to Care for Young Adults in 2017,” Journal of Adolescent Health Epub ahead of print (July 2019), https://doi.org/10.1016/j.jadohealth.2019.05.020
- Jevay Grooms and Alberto Ortega, “Examining Medicaid Expansion and the Treatment of Substance Use Disorders,” American Economic Association Papers and Proceedings 109 (May 2019): 187-192, https://www.aeaweb.org/articles?id=10.1257/pandp.20191090
- Jocelyn Guyer, Naomi Shine, MaryBeth Musumeci, and Robin Rudowitz, A Look at the Private Option in Arkansas (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, August 2015), http://kff.org/medicaid/issue-brief/a-look-at-the-private-option-in-arkansas/
- Jennifer Haley, Genevieve Kenney, and Jason Gates, Veterans Saw Broad Coverage Gains Between 2013 and 2015 (Washington, DC: The Urban Institute, April 2017), http://www.urban.org/research/publication/veterans-saw-broad-coverage-gains-between-2013-and-2015
- Jennifer Haley, Robin Wang, Matthew Buettgens, and Genevieve Kenney, Health Insurance Coverage among Children Ages 3 and Younger and Their Parents in 2016 (The Urban Institute, January 2018), https://www.urban.org/research/publication/health-insurance-coverage-among-children-ages-3-and-younger-and-their-parents-2016
- Jean Hall, Adele Shartzer, Noelle Kurth, and Kathleen Thomas, “Medicaid Expansion as an Employment Incentive Program for People With Disabilities,” American Journal of Public Health epub ahead of print (July 2018), https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.2018.304536
- Xinxin Han, Quian Luo, and Leighton Ku, “Medicaid Expansion and Grant Funding Increases Helped Improve Community Health Center Capacity,” Health Affairs 36 no. 1 (January 2017): 49-56, http://content.healthaffairs.org/content/36/1/49.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19
- Xuesong Han, Robin Yabroff, Elizabeth Ward, Otis Brawley, and Ahmedin Jemal, “Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act,” JAMA Oncology 4, no. 12 (August 2018): 1713-1720, https://jamanetwork.com/journals/jamaoncology/article-abstract/2697226
- Xuesong Han et al., “Changes in Noninsurance and Care Unaffordability Among Cancer Survivors Following the Affordable Care Act,” Journal of the National Cancer Institute Epub ahead of print (November 2019), https://doi.org/10.1093/jnci/djz218
- Micah Hartman et al., “National Health Care Spending in 2016: Spending and Enrollment Growth Slow After Initial Coverage Expansions,” Health Affairs epub ahead of print (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1299
- Meera N. Harhay, Ryan M. McKenna, and Michael O. Harhay, “Association Between Medicaid Expansion Under the Affordable Care Act and Medicaid-Covered Pre-emptive Kidney Transplantation,” Journal of General Internal Medicine 34, no. 11 (November 2019): 2322-2325, https://doi.org/10.1007/s11606-019-05279-x
- Meera Harhay et al., “Association between Medicaid Expansion under the Affordable Care Act and Preemptive Listings for Kidney Transplantation,” Clinical Journal of the American Society of Nephrology 13 (July 2018), https://cjasn.asnjournals.org/content/13/7/1069
- Jake Haselswerdt, “Expanding Medicaid, Expanding the Electorate: The Affordable Care Act’s Short-Term Impact on Political Participation,” Journal of Health Politics, Policy, and Law 42, no. 4 (August 2017), https://read.dukeupress.edu/jhppl/article-abstract/42/4/667/130386/Expanding-Medicaid-Expanding-the-Electorate-The?redirectedFrom=fulltext
- J.W. Awori Hayanga et al., “Lung Transplantation and Affordable Care Act Medicaid Expansion in the Era of Lung Allocation Score” Transplant International epub ahead of print (February 2019), https://onlinelibrary.wiley.com/doi/pdf/10.1111/tri.13420
- Susan Hayes, Sara Collins, David Radley, and Douglas McCarthy, What’s at Stake: States’ Progress on Health Coverage and Access to Care, 2013-2016 (The Commonwealth Fund, December 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/dec/states-progress-health-coverage-and-access
- Susan Hayes, Pamela Riley, David Radley, and Douglas McCarthy, Reducing Racial and Ethnic Disparities in Access to Care: Has the Affordable Care Act Made a Difference? (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/racial-ethnic-disparities-care
- Qiwei He and Scott Barkowski, “The Effect of Health Insurance on Crime: Evidence from the Affordable Care Act Medicaid Expansion,” Health Economics Epub ahead of print (January 2020): 261-277, https://doi.org/10.1002/hec.3977
- John Heintzman, Steffani Bailey, Jennifer DeVoe, Stuart Cowburn, Tanya Kapka, Truc-Vi Duong, and Miguel Marino, “In Low-Income Latino Patients, Post-Affordable Care Act Insurance Disparities May Be Reduced Even More than Broader National Estimates: Evidence from Oregon,” Journal of Racial and Ethnic Health Disparities (April 2016), http://www.ncbi.nlm.nih.gov/pubmed/27105630
- Fred Hellinger, “In Four ACA Expansion States, The Percentage of Uninsured Hospitalizations for People With HIV Declined, 2012-14,” Health Affairs 34, no. 12 (December 2015): 2061-2068, http://search.proquest.com/docview/1749932806/627DA95CDEA44BE7PQ/77?accountid=39486#
- Michael Hendryx and Juhua Luo, “Increased Cancer Screening for Low-income Adults Under the Affordable Care Act Medicaid Expansion,” Medical Care 56, no. 11 (November 2018): 944-949, https://www.ingentaconnect.com/content/wk/mcar/2018/00000056/00000011/art00009
- Gracie Himmelstein, “Effect of the Affordable Care Act’s Medicaid Expansions on Food Security, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1243-1248, https://doi.org/10.2105/ajph.2019.305168
- Jesse M. Hinde et al., “Increasing Access to Opioid Use Disorder Treatment: Assessing State Policies and the Evidence Behind Them,” Journal of Studies on Alcohol and Drugs 80, no. 6 (November 2019): 693-697, https://doi.org/10.15288/jsad.2019.80.693
- Heather Holderness et al., “Where Do Oregon Medicaid Enrollees Seek Outpatient Care Post-Affordable Care Act Medicaid Expansion?,” Medical Care 57, no. 10 (October 2019): 788-794, https://doi.org/10.1097/mlr.0000000000001189
- Jeremy Holzmacher et al., “Association of Expanded Medicaid Coverage with Hospital Length of Stay After Injury,” JAMA Surgery published online (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28658482
- Megan Hoopes, Heather Angier, Rachel Gold, Steffani Bailey, Nathalie Huguet, Miguel Marino, and Jennifer DeVoe, “Utilization of Community Health Centers in Medicaid Expansion and Nonexpansion States, 2013-2014,” Journal of Ambulatory Care Management 39 no. 4 (October 2016): 290-298, https://www.ncbi.nlm.nih.gov/pubmed/26765808
- Daniel Hopkins and Kalind Parish, “The Medicaid Expansion and Attitudes toward the Affordable Care Act: Testing for a Policy Feedback on Mass Opinion,” Public Opinion Quarterly 83, no. 1 (April 2019): 123-134, https://academic.oup.com/poq/article-abstract/83/1/123/5430239
- Jeffrey Horn et al., “New Medicaid Enrollees See Health and Social Benefits in Pennsylvania’s Expansion,” INQUIRY: the Journal of Health Care Organization, Provision, and Financing 53 (October 2016): 1-8, http://journals.sagepub.com/doi/full/10.1177/0046958016671807#
- Luojia Hu, Robert Kaestenr, Bhashkar Mazumder, Sarah Miller, and Ashley Wong, “The Effect of the Affordable Care Act Medicaid Expansions on Financial Wellbeing,” Journal of Public Economics 163 (July 2018): 99-112, https://www.sciencedirect.com/science/article/abs/pii/S0047272718300707
- Jin Huang and Shirley L. Porterfield, “Changes in Health Insurance Coverage and Health Care Access as Teens with Disabilities Transition to Adulthood,” Disability and Health Journal 12, no. 4 (October 2019): 551-556, https://doi.org/10.1016/j.dhjo.2019.06.009
- Julie Hudson and Asako Moriya, “Medicaid Expansion for Adults Had Measureable ‘Welcome Mat’ Effects on Their Children,” Health Affairs, 36 no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0347
- Nathalie Huguet et al., “Cervical And Colorectal Cancer Screening Prevalence Before And After Affordable Care Act Medicaid Expansion,” Preventative Medicine (May 2019), https://doi.org/10.1016/j.ypmed.2019.05.003
- Nathalie Huguet et al., “Following Uninsured Patients Through Medicaid Expansion: Ambulatory Care Use and Diagnosed Conditions,” Annals of Family Medicine 17, no. 4 (July/August 2019): 336-344, https://doi.org/10.1370/afm.2385
- Nathalie Huguet et al., “Medicaid Expansion Produces Long-Term Impact on Insurance Coverage Rates in Community Health Centers,” Journal of Primary Care & Community Health epub ahead of print (May 2017), http://journals.sagepub.com/doi/full/10.1177/2150131917709403
- Nathalie Huguet et al., “The Impact of the Affordable Care Act (ACA) Medicaid Expansion on Visit Rates for Diabetes in Safety Net Health Centers,” Journal of the American Board of Family Medicine 31, no. 6 (November 2018): 905-916, https://www.jabfm.org/content/31/6/905.full
- IMS Institute for Healthcare Informatics, Medicines Use and Spending Shifts: A Review of the Use of Medicines in the US in 2014 IMS Institute for Healthcare Informatics, April 2015), http://www.imshealth.com/en/thought-leadership/ims-institute/reports/medicines-use-in-the-us-2014
- Paul Jacobs, Genevieve Kenney, and Thomas Selden, “Newly Eligible Enrollees In Medicaid Spend Less And Use Less Care Than Those Previously Eligible,” Health Affairs 36, no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0252
- Alexander T. Janke, Shooshan Danagoulian, Arjun K. Venkatesh, and Phillip D. Levy, “Medicaid Expansion and Resource Utilization in the Emergency Department,” The American Journal of Emergency Medicine Epub ahead of print (January 2020), https://doi.org/10.1016/j.ajem.2019.12.050
- Ahmedin Jemal, Chun Chieh Lin, Amy Davidoff, and Xuesong Han, “Changes in Insurance Coverage and Stage at Diagnosis Among Nonelderly Patients with Cancer after the Affordable Care Act,” Journal of Clinical Oncology 35, no. 35 (December 2017), http://ascopubs.org/doi/pdf/10.1200/JCO.2017.73.7817
- Emily Johnston, Andrea Strahan, Peter Joski, Anne Dunlop, and E. Kathleen Adams, “Impacts of the Affordable Care Act’s Medicaid Expansion on Women of Reproductive Age,” Women’s Health Issues, 28, no. 2 (February 2018), http://www.whijournal.com/article/S1049-3867(17)30242-6/pdf
- Christine Jones, Serena Scott, Debra Anoff, Read Pierce, Jeffrey Glasheen, “Changes in Payer Mix and Physician Reimbursement After the Affordable Care Act and Medicaid Expansion,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 52 (August 2015), http://inq.sagepub.com/content/52/0046958015602464.full
- Robert Kaestner, Bowen Garrett, Anuj Gangopadhyaya, and Caitlyn Fleming, Effects of ACA Medicaid Expansions on Health Insurance Coverage and Labor Supply (Working Paper No. 21836, National Bureau of Economic Research, December 2015), http://www.nber.org/papers/w21836
- Michael Karpman, Jason Gates, Genevieve Kenney, Stacey McMorrow, How Are Moms Faring under the Affordable Care Act? Evidence Through 2014, (The Urban Institute, May 2016), http://www.urban.org/research/publication/how-are-moms-faring-under-affordable-care-act-evidence-through-2014
- Jennifer Kates and Lindsey Dawson, Insurance Coverage Changes for People with HIV Under the ACA (Washington, DC: Kaiser Family Foundation, February 2017), http://kff.org/health-reform/issue-brief/insurance-coverage-changes-for-people-with-hiv-under-the-aca/
- Harvey Kaufman, Zhen Chen, Vivian Fonseca, and Michael McPhaul, “Surge in Newly Identified Diabetes Among Medicaid Patients in 2014 Within Medicaid Expansion States Under the Affordable Care Act,” Diabetes Care 38, no. 5 (May 2015): 833, http://care.diabetesjournals.org/content/early/2015/03/19/dc14-2334.full.pdf+html
- Brystana Kaufman, Kristin Reiter, George Pink, and George Holmes, “Medicaid Expansion Affects Rural and Urban Hospitals Differently,” Health Affairs 35 no. 9 (September 2016): 1665-1672, http://content.healthaffairs.org/content/35/9/1665.full?sid=4aea494e-8e02-4c66-8298-3c828bfc313b
- Taylor Kelley, Renuka Tipirneni, and Helen Levy, “Changes in Veterans’ Coverage and Access to Care Following the Affordable Care Act, 2011-2017,” American Journal of Public Health 109, no. 9 (September 2019): 1233-1235, https://doi.org/10.2105/ajph.2019.305160
- Genevieve Kenney, Jennifer Haley, Clare Pan, Victoria Lynch, and Matthew Buettgens, Children’s Coverage Climb Continues: Uninsurance and Medicaid/CHIP Eligibility and Participation Under the ACA, (Washington, DC: The Urban Institute, May 2016), http://www.urban.org/research/publication/childrens-coverage-climb-continues-uninsurance-and-medicaidchip-eligibility-and-participation-under-aca
- Sameed Ahmed Khatana et al., “Association of Medicaid Expansion With Cardiovascular Mortality,” JAMA Cardiology 4, no. 7 (July 2019): 671-679, https://doi.org/10.1001/jamacardio.2019.1651
- Shiho Kino and Ichiro Kawachi, “Can Health Literacy Boost Health Services Utilization in the Context of Expanded Access to Health Insurance?,” Health Education & Behavior Epub ahead of print (October 2019), https://doi.org/10.1177/1090198119875998
- Shiho Kino and Ichiro Kawachi, “The Impact Of ACA Medicaid Expansion On Socioeconomic Inequality In Health Care Services Utilization,” PLoS ONE 13, no. 2 (December 2018), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0209935
- James Kirby and Jessica Vistnes, “Access to Care Improved for People Who Gained Medicaid or Marketplace Coverage in 2014,” Health Affairs 35 no. 10 (October 2016): 1830-1834, http://content.healthaffairs.org/content/35/10/1830.full
- Eili Klein et al., “The Effect of Medicaid Expansion on Utilization in Maryland Emergency Departments,” Annals of Emergency Medicine epub ahead of print (June 2017), http://www.annemergmed.com/article/S0196-0644(17)30784-9/pdf
- Lindsay C. Kobayashi, Onur Altindag, Yulya Truskinovsky, and Lisa F. Berkman, “Effects of the Affordable Care Act Medicaid Expansion on Subjective Well-Being in the US Adult Population, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1236-1242, https://doi.org/10.2105/ajph.2019.305164
- Sanders Korenman, Dahlia K. Remler, and Rosemary T. Hyson, “Medicaid Expansions and Poverty: Comparing Supplemental and Health-Inclusive Poverty Measures,” Social Service Review 93, no. 3 (September 2019): 429-483, https://doi.org/10.1086/705319
- Nicole Kravitz-Wirtz et al., “Association of Medicaid Expansion With Opioid Overdose Mortality in the United States,” JAMA Network Open 3, no. 1 (January 2020), https://doi.org/10.1001/jamanetworkopen.2019.19066
- Joseph Labrum et al., “Does Medicaid Insurance Confer Adequate Access to Adult Orthopaedic Care in the Era of the Patient Protection and Affordable Care Act?” Clinical Orthopaedics and Related Research 475 no. 6 (June 2017): 1527-1536, https://link.springer.com/article/10.1007%2Fs11999-017-5263-3
- Rahul Ladhania, Amelia Haviland, Arvind Venkat, Rahul Telang, and Jesse Pines, “The Effect of Medicaid Expansion on the Nature of New Enrollees’ Emergency Department Use,” Medical Care Research and Review epub ahead of print (May 2019), https://journals.sagepub.com/doi/abs/10.1177/1077558719848270
- Nadia Laniado, Avery R. Brow, Eric Tranby, and Victor M. Badner, “Trends in Non-Traumatic Dental Emergency Department Use in New York and New Jersey: A Look at Medicaid Expansion from Both Sides of the Hudson River,” Journal of Public Health Dentistry Epub ahead of print (October 2019), https://doi.org/10.1111/jphd.12343
- David Lassman et al., “Health Spending by State 1991-2014: Measuring Per Capita Spending by Payers and Programs,” Health Affairs epub ahead of print (June 2017), http://content.healthaffairs.org/content/early/2017/06/13/hlthaff.2017.0416
- Hyunjung Lee and Frank Porell, “The Effect of the Affordable Care Act Medicaid Expansion on Disparities in Access to Care and Health Status,” Medical Care Research and Review epub ahead of print (October 2018), https://journals.sagepub.com/doi/abs/10.1177/1077558718808709?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=mcrd
- De-Chih Lee, Leiyu Shi, and Hailun Liang, “Primary Care Utilization And Clinical Quality Performance: A Comparison Between Health Centres In Medicaid Expansion States And Non-Expansion States,” Journal of Health Services Research & Policy 24, no. 1 (January 2019): 19-24, https://journals.sagepub.com/doi/abs/10.1177/1355819618788592
- Jusung Lee et al., “The Impact of Medicaid Expansion on Diabetes Management,” Diabetes Care Epub ahead of print (October 2019), https://doi.org/10.2337/dc19-1173
- Helen Levy, Thomas Buchmueller, and Sayeh Nikpay, “The Impact of Medicaid Expansion on Household Consumption,” Eastern Economic Journal 45, no. 1 (January 2019): 34-57, https://link.springer.com/article/10.1057/s41302-018-0124-7
- Pauline Leung and Alexandre Mas, Employment Effects of the ACA Medicaid Expansions (Working Paper No. 22540, National Bureau of Economic Research, August 2016), http://www.nber.org/papers/w22540
- Helen Levy et al., “Macroeconomic Feedback Effects of Medicaid Expansion: Evidence from Michigan,” Journal of Health Politics, Policy and Law Epub ahead of print (October 2019), https://doi.org/10.1215/03616878-7893555
- The Lewin Group, Indiana Healthy Indiana Plan 2.0: Interim Evaluation Report (The Lewin Group, Prepared for Indiana Family and Social Services Administration, July 2016), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-interim-evl-rpt-07062016.pdf
- The Lewin Group, Healthy Indiana Plan 2.0: POWER Account Contribution Assessment, (The Lewin Group, prepared for the Indiana Family and Social Services Administration, March 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-POWER-acct-cont-assesmnt-03312017.pdf
- Helen Levy, Thomas Buchmueller, and Sayeh Nikpay, Health Reform and Health Insurance Coverage of Early Retirees (Ann Arbor, MI: University of Michigan Retirement Research Center Working Paper, September 2016), http://www.mrrc.isr.umich.edu/publications/papers/pdf/wp345.pdf
- Donald Likosky, Devraj Sukul, Milan Seth, Chang He, Hitlander Gurm, and Richard Prager, “The Association Between Medicaid Expansion and Cardiovascular Interventions: The Michigan Experience,” Journal of the American College of Cardiology 71, no. 9 (March 2018): 1050-1051, https://www.sciencedirect.com/science/article/pii/S0735109718300056?via%3Dihub
- Stephan R. Lindner et al., “Health Care Expenditures Among Adults With Diabetes After Oregon’s Medicaid Expansion,” Diabetes Care Epub ahead of print (December 2019), https://doi.org/10.2337/dc19-1343
- Richard Lindrooth, Marcelo Perraillon, Rose Hardy, and Gregory Tung, “Understanding the Relationship Between Medicaid Expansions and Hospital Closures,” Health Affairs epub ahead of print (January 2018), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0976
- Brandy Lipton, Sandra Decker, and Benjamin Sommers, “The Affordable Care Act Appears to Have Narrowed Racial and Ethnic Disparities in Insurance Coverage and Access to Care Among Young Adults” Medical Care Research and Review 76, no.1 (April 2017): 32–55, https://www.ncbi.nlm.nih.gov/pubmed/29148341
- Jennifer M. Lobo et al., “Trends in Uninsured Rates Before and After Medicaid Expansion in Counties Within and Outside of the Diabetes Belt,” Diabetes Care Epub ahead of print (January 2020), https://doi.org/10.2337/dc19-0874
- Andrew Loehrer et al., “Association of the Affordable Care Act Medicaid Expansion with Access to and Quality of Care for Surgical Conditions,” Journal of the American Medical Association Surgery, epub ahead of print (January 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2670459?redirect=true
- Sharon Long, Lea Bart, Michael Karpman, Adele Shartzer, and Stephen Zuckerman, “Sustained Gains in Coverage, Access, and Affordability Under the ACA: A 2017 Update,” Health Affairs 36 no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0798
- Sharon Long, Michael Karpman, Adele Shartzer, Douglas Wissoker, Genevieve Kenney, Stephen Zuckerman, Nathaniel Anderson, and Katherine Hempstead, Taking Stock: Health Insurance Coverage under the ACA as of September 2014 (The Urban Institute, December 2014), http://hrms.urban.org/briefs/Health-Insurance-Coverage-under-the-ACA-as-of-September-2014.html
- Louisiana Department of Health, Medicaid Expansion 2016/17 (Baton Rouge, Louisiana Department of Health, June 2017), http://dhh.louisiana.gov/assets/HealthyLa/Resources/MdcdExpnAnnlRprt_2017_WEB.pdf
- Huabin Luo, Zhuo Chen, Lei Xu, and Ronny Bell, “Health Care Access and Receipt of Clinical Diabetes Preventive Care for Working-Age Adults With Diabetes in States With and Without Medicaid Expansion: Results from the 2013 and 2015 BRFSS,” Journal of Public Health Management and Practice 25, no. 4 (July/August 2019): 34-43, https://doi.org/10.1097/phh.0000000000000832
- Johanna Catherine Maclean, Michael F. Pesko, and Steven C. Hill, “Public Insurance Expansions and Smoking Cessation Medications,” Economic Inquiry 57, no. 4 (October 2019): 1798-1820, https://doi.org/10.1111/ecin.12794
- Johanna Maclean and Brendan Saloner, The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act (National Bureau of Economic Research Working Paper No. 23342, April 2017), http://www.nber.org/papers/w23342.pdf
- Johanna Maclean and Brendan Saloner, “The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act,” Journal of Policy Analysis and Management 38, no. 2 (Spring 2019): 366-393, https://www.ncbi.nlm.nih.gov/pubmed/30882195
- Amandeep R. Mahal et al., “Early Impact of the Affordable Care Act and Medicaid Expansion on Racial and Socioeconomic Disparities in Cancer Care,” American Journal of Clinical Oncology Epub ahead of print (January 2020), https://doi.org/10.1097/coc.0000000000000588
- Nirosha Mahendraratnam, Stacie Dusetzina, and Joel Farley, “Prescription Drug Utilization and Reimbursement Increased Following State Medicaid Expansion in 2014,” Journal of Managed Care & Specialty Pharmacy 23 no. 3 (March 2017): 355-363, http://www.jmcp.org/doi/10.18553/jmcp.2017.23.3.355
- Elham Mahmoudi, Alicia Cohen, Jason Buxbaum, Caroline Richardson, and Wassim Tarraf, “Gaining Medicaid Coverage During ACA Implementation: Effects on Access to Care and Preventive Services,” Journal of Health Care for the Poor and Underserved 29, no. 4 (November 2018): 1472-1487, https://muse.jhu.edu/article/708253
- Manatt Health, Medicaid Expansion: How It Affects Montana’s State Budget, Economy, and Residents, (Manatt Health, prepared for the Montana Healthcare Foundation, June 2018), https://mthcf.org/wp-content/uploads/2018/06/Manatt-MedEx_FINAL_6.1.18.pdf
- Ramiro Manzano-Nunez et al., “Association of Medicaid Expansion Policy with Outcomes in Homeless Patients Requiring Emergency General Surgery,” World Journal of Surgery 43, no. 6 (June 2019): 1483-1489, https://link.springer.com/article/10.1007/s00268-019-04932-0
- Claire E. Margerison et al., “Impacts of Medicaid Expansion on Health Among Women of Reproductive Age,” American Journal of Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.amepre.2019.08.019
- Anne Martin et al., “National Health Spending: Faster Growth in 2015 As Coverage Expands and Utilization Increases,” Health Affairs 36 no. 1 (January 2017): 166-176, http://content.healthaffairs.org/content/36/1/166.full?sid=982b20c0-0a17-4dc4-a35a-b0302d4ec289
- Dennis McCarty, Yifan Gu, John W. McIlveen, and Bonnie K. Lind, “Medicaid Expansion and Treatment for Opioid Use Disorders in Oregon: An Interrupted Time-Series Analysis,” Addiction Science & Clinical Practice 14 (August 2019), https://doi.org/10.1186/s13722-019-0160-6
- Tyler McClintock, Ye Wang, Mahek Shah, Benjamin Chung, and Steven Chang, “How Have Hospital Pricing Practices for Surgical Episodes of Care Responded to Affordable Care Act-Related Medicaid Expansion?” Urology 125 (March 2019): 79-85, https://doi.org/10.1016/j.urology.2018.10.034
- Shannon McConville, Maria Raven, Sarah Sabbagh, and Renee Hsia, “Frequent Emergency Department Users: A Statewide Comparison Before And After Affordable Care Act Implementation,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0784
- Michael McCue, “The Impact of Medicaid Expansion on Medicaid Focused Insurers in California,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 52 (July 2015), http://inq.sagepub.com/content/52/0046958015595960.full.pdf+html
- James McDermott et al., “Affordable Care Act’s Medicaid Expansion and Use of Regionalized Surgery at High-Volume Hospitals,” Journal of the American College of Surgeons 227, no. 5 (November 2018): 507-520.e9, https://www.journalacs.org/article/S1072-7515(18)31993-8/abstract
- Stacey McMorrow, Jason Gates, Sharon Long, and Genevieve Kenney, “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents,” Health Affairs 36 no. 5 (May 2017): 808-818, https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Nathaniel Anderson, “Uninsurance Among Young Adults Continues to Decline, Particularly in Medicaid Expansion States,” Health Affairs 34, no. 4 (April 2015): 616-620, http://content.healthaffairs.org/content/34/4/616.full
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Jason Gates, The ACA Medicaid Expansion Led to Widespread Reductions in Uninsurance Among Poor Childless Adults (The Urban Institute, April 2017), http://www.urban.org/sites/default/files/publication/89536/2001222-aca_medicaid_expansion_led_to_widespread_reductions_in_uninsurance_among_poor_childless_adults.pdf
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Jason Gates, “Marketplaces Helped Drive Coverage Gains in 2015; Affordability Problems Remained,” Health Affairs 35 no. 10 (October 2016): 1810-1815, http://content.healthaffairs.org/content/35/10/1810.full
- Aaron McNay, Amy Watson, Barbara Wagner, and Chris Bradley, Montana Medicaid and Montana Employers (Montana Department of Revenue and Montana Department of Labor & Industry, January 2019), http://lmi.mt.gov/Portals/193/Publications/LMI-Pubs/Special%20Reports%20and%20Studies/MT-Medicaid_Report.pdf
- Angelica Meinhofer and Allison Witman, “The Role Of Health Insurance On Treatment For Opioid Use Disorders: Evidence From The Affordable Care Act Medicaid Expansion,” Journal of Health Economics 60 (June 2018): 177-197, https://www.sciencedirect.com/science/article/abs/pii/S0167629617311530
- Jose Mesquita-Neto, Peter Cmorej, Hassan Mouzaihem, Donald Weaver, Steve Kim, and Francis Macedo, “Disparities In Access To Cancer Surgery After Medicaid Expansion,” The American Journal of Surgery epub ahead of print (June 2019), https://www.sciencedirect.com/science/article/abs/pii/S0002961019306889
- Sarah Miller, Sean Altekruse, Norman Johnson, and Laura R. Wherry, Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data (National Bureau of Economic Research, Working Paper No. 26081, July 2019), http://www.nber.org/papers/w26081
- Sarah Miller, Luojia Hu, Robert Kaestner, Bhashkar Mazumder, and Ashley Wong, The ACA Medicaid Expansion in Michigan and Financial Health, (National Bureau of Economic Research, working paper no. 25053, September 2018), https://www.nber.org/papers/w25053.pdf
- Sarah Miller and Laura Wherry, “Four Years Later: Insurance Coverage and Access to Care Continue to Diverge between ACA Medicaid Expansion and Non-Expansion States,” American Economic Association Papers and Proceedings 109 (May 2019): 327-333, https://www.aeaweb.org/articles?id=10.1257/pandp.20191046
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890
- Ramin Mojtabai, Christine Mauro, Melanie Wall, Colleen Barry, and Mark Olfson, “The Affordable Care Act and Opioid Agonist Therapy for Opioid Use Disorder,” Psychiatry Online (April 2019), https://doi.org/10.1176/appi.ps.201900025
- Ramin Mojtabai, Christine Mauro, Melanie Wall, Colleen Barry, and Mark Olfson, “Medication Treatment For Opioid Use Disorders In Substance Use Treatment Facilities,” Health Affairs 38, no. 1 (January 2019), https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.05162
- Favel Mondesir et al., “Medicaid Expansion and Hospitalization for Ambulatory Care–Sensitive Conditions Among Nonelderly Adults With Diabetes,” Journal of Ambulatory Care Management epub ahead of print (May 2019), https://insights.ovid.com/pubmed?pmid=31107800
- Michelle Moniz et al., “Association of Access to Family Planning Services With Medicaid Expansion Among Female Enrollees in Michigan,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2698636
- Haley Moss, Laura Havrilesky, and Junzo Chino, “Insurance Coverage Among Women Diagnosed with a Gynecologic Malignancy Before and After Implementation of the Affordable Care Act,” Gynecologic Oncology 146, no. 3 (September 2017), https://www.ncbi.nlm.nih.gov/pubmed/28641821
- Andrew Mulcahy, Christine Eibner, and Kenneth Finegold, “Gaining Coverage Through Medicaid Or Private Insurance Increased Prescription Use and Lowered Out-Of-Pocket Spending,” Health Affairs 35, no. 9 (September 2016), http://content.healthaffairs.org/content/early/2016/08/16/hlthaff.2016.0091.full
- MaryBeth Musumeci, Disability and Technical Issues Were Key Barriers to Meeting Arkansas’ Medicaid Work and Reporting Requirements in 2018 (Washington, DC: Kaiser Family Foundation, June 2019), https://www.kff.org/medicaid/issue-brief/disability-and-technical-issues-were-key-barriers-to-meeting-arkansas-medicaid-work-and-reporting-requirements-in-2018/
- MaryBeth Musumeci, Priya Chidambaram, and Molly O’Malley Watts, Key Questions About Medicaid Home and Community-Based Services Waiver Waiting Lists (Washington, DC: Kaiser Family Foundation, April 2019), https://www.kff.org/medicaid/issue-brief/key-questions-about-medicaid-home-and-community-based-services-waiver-waiting-lists/
- MaryBeth Musumeci, Robin Rudowitz, and Cornelia Hall, An Early Look at Implementation of Medicaid Work Requirements in Arkansas (Washington, DC: Kaiser Family Foundation, October 2018), https://www.kff.org/medicaid/issue-brief/an-early-look-at-implementation-of-medicaid-work-requirements-in-arkansas/
- MaryBeth Musumeci, Robin Rudowitz, and Barbara Lyons, Medicaid Work Requirements in Arkansas: Experience and Perspectives of Enrollees (Washington, DC: Kaiser Family Foundation, December 2018), https://www.kff.org/medicaid/issue-brief/medicaid-work-requirements-in-arkansas-experience-and-perspectives-of-enrollees/
- MaryBeth Musumeci, Robin Rudowitz, Petry Ubri, and Elizabeth Hinton, An Early Look at Medicaid Expansion Waiver Implementation in Michigan and Indiana (Washington, DC: The Kaiser Family Foundation, January 2017), http://kff.org/medicaid/issue-brief/an-early-look-at-medicaid-expansion-waiver-implementation-in-michigan-and-indiana/
- Rebecca Myerson, Tianyi Lu, Ivy Tonnu-Mihara, and Elbert Huang, “Medicaid Eligibility Expansions May Address Gaps In Access To Diabetes Medications,” Health Affairs 37, no. 8 (August 2018), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.0154
- Kamyar Nasseh and Marko Vujicic, Early Impact of the Affordable Care Act’s Medicaid Expansion on Dental Care Use (Health Services Research, November 2016), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12606/full
- Hannah Neprash, Anna Zink, Joshua Gray, and Katherine Hempstead, “Physicians’ Participation In Medicaid Increased Only Slightly Following Expansion” Health Affairs 37, no. 7 (July 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1085
- Nevada’s Medicaid Population, (Las Vegas, NV: The Guinn Center, September 2019), https://guinncenter.org/wp-content/uploads/2019/09/Guinn-Center-NV-Medicaid-Population-Characteristics-2019.pdf
- Jenny Nguyen, Nidharshan Anandasivam, Daniel Cooperman, Richard Pelker, and Daniel Wiznia, “Does Medicaid Insurance Provide Sufficient Access to Pediatric Orthopedic Care Under the Affordable Care Act?,” Global Pediatric Health epub ahead of print (February 2019), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6381430/
- Sayeh Nikpay, Thomas Buchmueller, and Helen Levy. “Affordable Care Act Medicaid Expansion Reduced Uninsured Hospital Stays in 2014,” Health Affairs 35, no.1 (January 2016): 106-110, http://content.healthaffairs.org/content/35/1/106.full
- Sayeh Nikpay, Seth Freedman, Helen Levy, and Tom Buchmueller, “Effect of the Affordable Care Act Medicaid Expansion on Emergency Department Visits: Evidence From State-Level Emergency Department Databases,” Annals of Emergency Medicine 70, no.2 (August 2017), http://www.annemergmed.com/article/S0196-0644(17)30319-0/pdf
- Office of the Assistant Secretary for Planning and Evaluation (ASPE), Impacts of the Affordable Care Act’s Medicaid Expansion on Insurance Coverage and Access to Care (Office of the Assistant Secretary for Planning and Evaluation, June 2016), https://aspe.hhs.gov/sites/default/files/pdf/205141/medicaidexpansion.pdf
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf
- Mark Olfson, Melanie Wall, Colleen Barry, Christine Mauro, and Ramin Mojtabai, “Impact Of Medicaid Expansion On Coverage And Treatment Of Low-Income Adults With Substance Use Disorders,” Health Affairs 37, no. 8 (August 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.0124
- Mark Olfson et al., “A National Survey of Trends in Health Insurance Coverage of Low-Income Adults Following Medicaid Expansion,” Journal of General Internal Medicine Epub ahead of print (October 2019), https://doi.org/10.1007/s11606-019-05409-5
- John J. Park et al., “Medicaid and Private Insurance Coverage for Low-Income Asian Americans, Native Hawaiians, and Pacific Islanders, 2010-16,” Health Affairs 38, no. 11 (November 2019): 1911-1917, https://doi.org/10.1377/hlthaff.2019.00316
- Lizhong Peng, Xiaohui Guo, and Chad D. Meyerhoefer, “The Effects of Medicaid Expansion on Labor Market Outcomes: Evidence from Border Counties,” Health Economics Epub ahead of print (December 2019), https://doi.org/10.1002/hec.3976
- Pennsylvania Department of Human Services, Medicaid Expansion Report, (Pennsylvania Department of Human Services, January 2017), http://www.dhs.pa.gov/cs/groups/webcontent/documents/document/c_257436.pdf
- Gary Pickens et al., “Changes in Hospital Inpatient Utilization Following Health Care Reform,” Health Services Research epub ahead of print (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28664983
- Gary Pickens et al., “Changes In Hospital Service Demand, Cost, And Patient Illness Severity Following Health Reform,” Health Services Research (May 2019), https://doi.org/10.1111/1475-6773.13165
- Jesse Pines, Rahul Ladhania BTech, Bernard Black , Christopher Corbit, Jestin Carlson, and Arvind Venkat, “Changes in Reimbursement to Emergency Physicians After Medicaid Expansion Under the Patient Protection and Affordable Care Act,” Annals of Emergency Medicine 73, no. 3 (March 2019): 213-224, https://www.sciencedirect.com/science/article/pii/S019606441831374X
- Jesse M. Pines, Mark Zocchi, Ali Moghtaderi, Bernard Black, Steven A. Farmer, Greg Hufstetler, Kevin Klauer and Randy Pilgrim, “Medicaid Expansion In 2014 Did Not Increase Emergency Department Use But Did Change Insurance Payer Mix,” Health Affairs 35, no. 8 (August 2016), http://content.healthaffairs.org/content/35/8/1480.full
- Matthew Present, Aviva Nathan, Sandra Ham, Robert Sargis, Michael Quinn, and Elbert Huang, “The Impact of the Affordable Care Act Medicaid Expansion on Type 2 Diabetes Diagnosis and Treatment: A National Survey of Physicians,” Journal of Community Health epub ahead of print (May 2019), https://link.springer.com/article/10.1007%2Fs10900-019-00637-6
- PricewaterhouseCoopers LLP Health Research Institute, Medicaid 2.0: Health System Haves and Have Nots (PwC Health Research Institute, September 2014), http://www.pwc.com/us/en/health-industries/health-research-institute/assets/pwc-hri-medicaid-report-final.pdf
- Beatrice D. Probst, Luther Walls, Michael Cirone, and Talar Markossian, “Examining the Effect of the Affordable Care Act on Two Illinois Emergency Departments,” Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health 20, no. 5 (September 2019): 710-716, https://doi.org/10.5811/westjem.2019.6.41943
- Lee A. Reynis, Economic and Fiscal Impacts of the Medicaid Expansion in New Mexico, (The University of New Mexico Bureau of Business and Economic Research, February 2016), http://bber.unm.edu/media/publications/Medicaid_Expansion_Final2116R.pdf
- Jordan Rhodes, Thomas Buchmueller, Helen Levy, and Sayeh Nikpay, “Heterogeneous Effects Of The Aca Medicaid Expansion On Hospital Financial Outcomes,” Contemporary Economic Policy epub ahead of print (April 2019), https://onlinelibrary.wiley.com/doi/full/10.1111/coep.12428
- James Richardson, Jared Llorens, and Roy Heidelberg, Medicaid Expansion and the Louisiana Economy (Louisiana Department of Health, March 2018), http://gov.louisiana.gov/assets/MedicaidExpansion/MedicaidExpansionStudy.pdf
- James A. Richardson, Jared J. Llorens, and Roy L. Heidelberg. Medicaid Expansion and the Louisiana Economy, 2018 and 2019 (Louisiana Department of Health, Prepared by Louisiana State University, August 2019), http://ldh.la.gov/assets/media/3and4.2019FinalReportMedicaidExpansionstudy.pdf
- Sara Rosenbaum, Jennifer Tolbert, Jessica Sharac, Peter Shin, Rachel Gunsalus, and Julia Zur, Community Health Centers: Growing Importance in a Changing Health Care System (Washington, DC: Kaiser Family Foundation, March 2018), https://www.kff.org/medicaid/issue-brief/community-health-centers-growing-importance-in-a-changing-health-care-system/
- Ann-Marie Rosland et al., “Diagnosis and Care of Chronic Health Conditions Among Medicaid Expansion Enrollees: a Mixed-Methods Observational Study,” Journal of General Internal Medicine 34, no. 11 (November 2019): 2549-2558, https://doi.org/10.1007/s11606-019-05323-w
- Jonathan Routh et al., “Early Impact of the Patient Protection and Affordable Care Act on Delivery of Children’s Surgical Care,” Clinical Pediatrics 58, no. 4 (January 2019) 453-460, https://journals.sagepub.com/doi/abs/10.1177/0009922818825156?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=cpja
- Robin Rudowitz, Samantha Artiga, Anthony Damico, and Rachel Garfield, A Closer Look at the Remaining Uninsured Population Eligible for Medicaid and CHIP (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, February 2016), http://kff.org/uninsured/issue-brief/a-closer-look-at-the-remaining-uninsured-population-eligible-for-medicaid-and-chip/
- Robin Rudowitz and Rachel Garfield, New Analysis Shows States with Medicaid Expansion Experienced Declines in Uninsured Hospital Discharges (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, September 2015), http://kff.org/health-reform/issue-brief/new-analysis-shows-states-with-medicaid-expansion-experienced-declines-in-uninsured-hospital-discharges/
- Robin Rudowitz, Elizabeth Hinton, and Larisa Antonisse, Medicaid Enrollment and Spending Growth: FY 2018 & 2019 (Washington, DC: Kaiser Family Foundation, October 2018), https://www.kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2018-2019/
- Robin Rudowitz, MaryBeth Musumeci, and Cornelia Hall, February State Data for Medicaid Work Requirements in Arkansas (Washington, DC: Kaiser Family Foundation, March 2019), https://www.kff.org/medicaid/issue-brief/state-data-for-medicaid-work-requirements-in-arkansas/
- Robin Rudowitz, Laura Snyder, and Vernon Smith, Medicaid Enrollment and Spending Growth: FY 2015 & 2016 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, October 2015), http://kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2015-2016/
- Robin Rudowitz, Allison Valentine, and Vernon Smith, Medicaid Enrollment and Spending Growth: FY 2016 & 2017 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, October 2016), http://kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2016-2017/
- Robin Rudowitz et al., Medicaid Enrollment and Spending Growth: FY 2019 & 2020 (Washington, DC: Kaiser Family Foundation, October 2019), https://www.kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2019-2020/
- Brendan Saloner, Sachini Bandara, Emma McGinty, and Colleen Barry, “Justice-Involved Adults With Substance Use Disorders: Coverage Increased but Rates of Treatment Did Not in 2014,” Health Affairs 35 no. 6 (June 2016), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2016.0005
- Brendan Saloner, Rachel Landis, Bradley Stein, and Colleen Barry, “The Affordable Care Act in the Heart of the Opioid Crisis: Evidence from West Virginia,” Health Affairs 38, no. 4 (April 2019), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05049
- Brendan Saloner, Jonathan Levin, Hsien-Yen Chang, Christopher Jones, and G. Caleb Alexander, “Changes in Buprenorphine-Naloxone and Opioid Pain Reliever Prescriptions After the Affordable Care Act Medicaid Expansion,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2696873
- Michael Sances and Joshua Clinton, New Policy, New Politics? The Effect of Medicaid Expansion on Public Support for the Affordable Care Act, (University of Memphis and Vanderbilt University, February 2017), https://csap.yale.edu/sites/default/files/files/apppw_jc2_3-8-17.pdf
- Scott R. Sanders et al., “Infants Without Health Insurance: Racial/Ethnic and Rural/Urban Disparities in Infant Households’ Insurance Coverage,” PLoS One 15, no. 1 (January 2020), https://doi.org/10.1371/journal.pone.0222387
- Robert Sandstrom, “Increased Utilization of Ambulatory Occupational Therapy and Physical Therapy After Medicaid Expansion” Archives of Physical Medicine and Rehabilitation epub ahead of print (March 2019), https://www.archives-pmr.org/article/S0003-9993(19)30161-3/fulltext
- Lucie Schmidt, Lara Shore-Sheppard, and Tara Watson, The Impact of the ACA Medicaid Expansion on Disability Program Applications (National Bureau of Economic Research, Working Paper No. 26192, August 2019), http://www.nber.org/papers/w26192
- John Scott et al., “Lifting the Burden: State Medicaid Expansion Reduces Financial Risk for the Injured,” Journal of Trauma and Acute Care Surgery Epub ahead of print (September 2019), https://doi.org/10.1097/ta.0000000000002493
- Olga Scrivner et al., “Job Postings in the Substance Use Disorder Treatment Related Sector During the First Five Years of Medicaid Expansion,” PLoS One 15, no. 1 (January 2020), https://doi.org/10.1371/journal.pone.0228394
- Eric Seiber and Micah Berman, “Medicaid Expansion and ACA Repeal: Evidence from Ohio,” American Journal of Public Health epub ahead of print (April 2017), http://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.2017.303722
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830
- Ashley Semanskee, Cynthia Cox, and Larry Levitt, Data Note: Effect of State Decisions on State Risk Scores (Kaiser Family Foundation, October 2016), https://www.kff.org/health-reform/issue-brief/data-note-effect-of-state-decisions-on-state-risk-scores/
- Aditi Sen and Thomas DeLeire, The Effect of Medicaid Expansion on Marketplace Premiums (Office of the Assistant Secretary for Planning and Evaluation, August 2016), https://aspe.hhs.gov/sites/default/files/pdf/206761/McaidExpMktplcPrem.pdf
- Aditi Sen and Thomas DeLeire, “How Does Expansion Of Public Health Insurance Affect Risk Pools And Premiums In The Market For Private Health Insurance? Evidence From Medicaid And The Affordable Care Act Marketplaces,” Health Economics 27 (July 2018): 1877–1903, https://onlinelibrary.wiley.com/doi/abs/10.1002/hec.3809
- Jessica Sharac, Rachel Gunsalus, Chi Tran, Peter Shin, and Sara Rosenbaum, How are Migrant Health Centers and their Patients Faring Under the Affordable Care Act? (Geiger Gibson/RCHN Community Health Foundation Research Collaborative, The George Washington University Milken Institute of Public Health, May 2016), http://www.rchnfoundation.org/wp-content/uploads/2016/05/Migrant-Health-Centers-Patients-Under-Affordable-Care-Act.pdf
- Aabha Sharma, Scott Dresden, Emilie Powell, Raymond Kang, Joe Feinglass, “Emergency Department Visits and Hospitalizations for the Uninsured in Illinois Before and After Affordable Care Act Insurance Expansion,” Journal of Community Health 42 no. 3 (June 2017): 591-597, https://link.springer.com/article/10.1007/s10900-016-0293-4
- Alana Sharp, Austin Jones, Jennifer Sherwood, Oksana Kutsa, Brian Honermann, and Gregorio Millett, “Impact of Medicaid Expansion on Access to Opioid Analgesic Medications and Medication-Assisted Treatment,” American Journal of Public Health 108, no. 5 (May 2018): 642-648, https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2018.304338?journalCode=ajph
- Adele Shartzer, Frederic Blavin, and John Holohan, “Employer-Sponsored Insurance Stable For Low-Income Workers In Medicaid Expansion States,” Health Affairs 37, no. 4 (April 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1205
- Adele Shartzer, Sharon Long, and Nathaniel Anderson, “Access To Care and Affordability have Improved Following Affordable Care Act Implementation; Problems Remain,” Health Affairs (December 2015), http://content.healthaffairs.org/content/early/2015/12/14/hlthaff.2015.0755.full
- Peter Shin, Jessica Sharac, Julia Zur, Sara Rosenbaum, and Julia Paradise, Health Center Patient Trends, Enrollment Activities, and Service Capacity: Recent Experience in Medicaid Expansion and Non-Expansion States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, December 2015), http://kff.org/medicaid/issue-brief/health-center-patient-trends-enrollment-activities-and-service-capacity-recent-experience-in-medicaid-expansion-and-non-expansion-states/
- Chelsea L. Shover et al., “The Relationship of Medicaid Expansion to Psychiatric Comorbidity Care within Substance Use Disorder Treatment Programs,” Journal of Substance Abuse Treatment 105 (October 2019): 44-50, https://doi.org/10.1016/j.jsat.2019.07.012
- Kosali Simon, Aparna Soni, and John Cawley, “The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions” Journal of Policy Analysis and Management 36, no. 2 (March 2017), https://onlinelibrary.wiley.com/doi/abs/10.1002/pam.21972
- Helmneh M. Sineshaw et al., “Association of Medicaid Expansion Under the Affordable Care Act With Stage at Diagnosis and Time to Treatment Initiation for Patients With Head and Neck Squamous Cell Carcinoma,” JAMA Otolaryngology–Head & Neck Surgery Epub ahead of print (January 2020), https://doi.org/10.1001/jamaoto.2019.4310
- Astha Singhal, Peter Damiano, and Lindsay Sabik, “Medicaid Adult Dental Benefits Increase Use Of Dental Care, But Impact Of Expansion On Dental Services Use Was Mixed,” Health Affairs 36 no. 4 (April 2017): 723-732, http://content.healthaffairs.org/content/36/4/723.short
- Laura Skopec, John Holahan, and Caroline Elmendorf, Changes in Health Insurance Coverage 2013–2016: Medicaid Expansion States Lead the Way, (Washington, DC: The Urban Institute, September 2018), https://www.urban.org/sites/default/files/publication/98989/changes_in_health_insurance_coverage_2013-2016_medicaid_expansion_states_lead_the_way_1.pdf
- Laura Skopec, John Holahan, and Caroline Elmendorf, Health Insurance Coverage Declined for Nonelderly Americans Between 2016 and 2017, Primarily in States That Did Not Expand Medicaid (Washington, DC: The Urban Institute, August 2019), https://www.urban.org/research/publication/health-insurance-coverage-declined-nonelderly-americans-between-2016-and-2017-primarily-states-did-not-expand-medicaid
- David Slusky and Donna Ginther, Did Medicaid Expansion Reduce Medical Divorce? (Working Paper No. 23139, National Bureau of Economic Research, February 2017), http://www.nber.org/papers/w23139?utm_campaign=ntw&utm_medium=email&utm_source=ntw
- Jessica Smith and Carla Medalia, Health Insurance Coverage in the United States: 2014 (U.S. Census Bureau, September 2015), https://www.census.gov/content/dam/Census/library/publications/2015/demo/p60-253.pdf
- Laura Snyder, Katherine Young, Robin Rudowitz, and Rachel Garfield, Medicaid Expansion Spending and Enrollment in Context: An Early Look at CMS Claims Data for 2014 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, January 2016), http://kff.org/medicaid/issue-brief/medicaid-expansion-spending-and-enrollment-in-context-an-early-look-at-cms-claims-data-for-2014/
- Aaron Sojourner and Ezra Golberstein, “Medicaid Expansion Reduced Unpaid Medical Debt and Increased Financial Satisfaction,” Health Affairs (July 2017), https://www.healthaffairs.org/do/10.1377/hblog20170724.061160/full/
- Benjamin Sommers, Robert Blendon, and E. John Orav, “Both the ‘Private Option’ And Traditional Medicaid Expansions Improved Access To Care For Low-Income Adults,” Health Affairs 35, no. 1 (January 2016): 96-105, http://content.healthaffairs.org/content/35/1/96.abstract
- Benjamin Sommers, Robert Blendon, E. John Orav, and Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420
- Benjamin Sommers, Carrie Fry, Robert Blendon, and Arnold Epstein, “New Approaches in Medicaid: Work Requirements, Health Savings Accounts, and Health Care Access,” Health Affairs 37, no. 7 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2018.0331
- Benjamin Sommers, Anna Goldman, Robert Blendon, E. John Orav, and Arnold Epstein, “Medicaid Work Requirements – Results from the First Year in Arkansas,” The New England Journal of Medicine Special Report (June 2019), https://www.nejm.org/doi/full/10.1056/NEJMsr1901772
- Benjamin Sommers, Rebecca Gourevitch, Bethany Maylone, Robert Blendon, and Arnold Epstein, “Insurance Churning Rates for Low-Income Adults Under Health Reform: Lower Than Expected but Still Harmful for Many,” Health Affairs 35 no. 10 (October 2016): 1816-1824, http://content.healthaffairs.org/content/35/10/1816.full?sid=f4835910-ffd0-4864-a76a-b4f207ccd018
- Benjamin Sommers and Jonathan Gruber, “Federal Funding Insulated State Budgets From Increased Spending Related To Medicaid Expansion,” Health Affairs epub ahead of print (April 2017), http://content.healthaffairs.org/content/early/2017/04/10/hlthaff.2016.1666.full
- Benjamin Sommers, Munira Gunja, Kenneth Finegold, and Thomas Musco, “Changes in Self-Reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act,” The Journal of the American Medical Association 314 no. 4 (July 2015): 366-374, http://jama.jamanetwork.com/article.aspx?articleid=2411283&resultClick=3
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293
- Benjamin Sommers, Thomas Musco, Kenneth Finegold, Munira Gunja, Amy Burke, and Audrey McDowell, “Health Reform and Changes in Health Insurance Coverage in 2014” The New England Journal of Medicine 371 (August 2014): 867-874, http://www.nejm.org/doi/full/10.1056/NEJMsr1406753
- Aparna Soni, Marguerite Burns, Laura Dague, and Kosali Simon, “Medicaid Expansion and State Trends in Supplemental Security Income Program Participation,” Health Affairs 36 no. 8, (August 2017): 1485-1488, http://content.healthaffairs.org/content/36/8/1485.full?sid=982b20c0-0a17-4dc4-a35a-b0302d4ec289
- Aparna Soni, Michael Hendryx, and Kosali Simon, “Medicaid Expansion under the Affordable Care Act and Insurance Coverage in Rural and Urban Areas,” The Journal of Rural Health epub ahead of print (January 2017), http://onlinelibrary.wiley.com/doi/10.1111/jrh.12234/full
- Aparna Soni, Lindsay Sabik, Kosali Simon, and Benjamin Sommers, “Changes in Insurance Coverage Among Cancer Patients Under the Affordable Care Act,” Journal of the American Medical Association 4, no. 1 (January 2018): 122-124, https://jamanetwork.com/journals/jamaoncology/article-abstract/2657670?redirect=true&redirect=true
- Aparna Soni, Kosali Simon, John Cawley, and Lindsay Sabik, “Effect of Medicaid Expansions of 2014 on Overall and Early-Stage Cancer Diagnoses,” American Journal of Public Health epub ahead of print (December 2017), http://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2017.304166
- Jim P. Stimpson, Jessie Kemmick Pintor, and Fernando A. Wilson, “Association of Medicaid Expansion with Health Insurance Coverage by Marital Status and Sex,” PLoS One 14, no. 10 (October 2019), https://doi.org/10.1371/journal.pone.0223556
- Jim Stimpson and Fernando Wilson, “Medicaid Expansion Improved Health Insurance Coverage For Immigrants, But Disparities Persist,” Health Affairs 37, no. 10 (October 2018), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.0181
- Jim P. Stimpson et al., “Association of Medicaid Expansion With Health Insurance Coverage Among Persons With a Disability,” JAMA Network Open 2, no. 7 (July 2019), https://doi.org/10.1001/jamanetworkopen.2019.7136
- Shailender Swaminathan, Benjamin Sommers, Rebecca Thorsness, Rajnish Mehrotra, Yoojin Lee, and Amal Trivedi, “Association of Medicaid Expansion With 1-Year Mortality Among Patients With End-Stage Renal Disease,” Journal of the American Medical Association (JAMA) 320, no. 21 (December 2018): 2242-2250, https://jamanetwork.com/journals/jama/fullarticle/2710505?guestAccessKey=ea3a8641-320b-4afd-b96e-dc59fbd90b20&utm_source=TrendMD&utm_medium=cpc&utm_campaign=J_Am_Med_TrendMD_1&utm_content=olf&utm_term=102518
- James A. Swartz and Susanny J. Beltran, “Prescription Opioid Availability and Opioid Overdose-Related Mortality Rates in Medicaid Expansion and Non-Expansion States,” Addiction 114, no. 11 (November 2019): 2016-2025, https://doi.org/10.1111/add.14741
- Renuka Tipirneni et al., “Association of Expanded Medicaid Coverage With Health and Job-Related Outcomes Among Enrollees With Behavioral Health Disorders,” Psychiatric Services Epub ahead of print (September 2019), https://doi.org/10.1176/appi.ps.201900179
- Renuka Tipirneni et al., “Association of Medicaid Expansion With Enrollee Employment and Student Status in Michigan,” JAMA Network Open 3, no. 1 (January 2020), https://doi.org/10.1001/jamanetworkopen.2019.20316
- Renuka Tipirneni et al., “Changes in Health and Ability to Work Among Medicaid Expansion Enrollees: a Mixed Methods Study,” Journal of General Internal Medicine 34, no. 2 (February 2019): 272-280, https://link.springer.com/article/10.1007/s11606-018-4736-8
- Renuka Tipirneni et al., “Primary Care Appointment Availability For New Medicaid Patients Increased After Medicaid Expansion In Michigan,” Health Affairs (July 2015), http://content.healthaffairs.org/content/early/2015/07/15/hlthaff.2014.1425.full
- Renuka Tipirneni et al., “Primary Care Appointment Availability and Nonphysician Providers One Year After Medicaid Expansion,” The American Journal of Managed Care 22 no. 6 (June 2016): 427-431, http://www.ajmc.com/journals/issue/2016/2016-vol22-n6/primary-care-appointment-availability-and-nonphysician-providers-one-year-after-medicaid-expansion
- Dmitry Tumin et al., “Medicaid Participation among Liver Transplant Candidates after the Affordable Care Act Medicaid Expansion” Journal of the American College of Surgeons 225, no. 2 (August 2017): 173-180.e2, https://www.journalacs.org/article/S1072-7515(17)30454-4/fulltext
- Dmitry Tumin, Don Hayes Jr., Kenneth Washburn, Joseph Tobias, and Sylvester Black, “Medicaid Enrollment after Liver Transplantation: Effects of Medicaid Expansion,” Liver Transplantation (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27152888
- Sri Lekha Tummalapalli, Samuel Leonard, Michelle M. Estrella, and Salomeh Keyhani, “The Effect of Medicaid Expansion on Self-Reported Kidney Disease,” Clinical Journal of American Society of Nephrology 14, no. 8 (August 2019): 1238-1240, https://doi.org/10.2215/cjn.02310219
- United States Government Accountability Office (GAO), Medicaid Expansion: Behavioral Health Treatment Use in Selected States in 2014 (Washington, DC: GAO Report to Congressional Requesters, June 2017), https://www.gao.gov/assets/690/685415.pdf
- The University of Michigan Institute for Healthcare Policy & Innovation, The Healthy Michigan Plan: 2015 Report on Uncompensated Care and Insurance Rates (The University of Michigan Institute for Healthcare Policy & Innovation, prepared for the Michigan Department of Health and Human Services and the Michigan Department of Insurance and Financial Services, December 2016), http://www.michigan.gov/documents/mdhhs/2015_Report_on_Uncompensated_Care_and_Insurance_Rates-HMP_547720_7.pdf
- Nimish Valvi, Neomi Vin-Raviv, and Tomi Akinyemiju, “Current Smoking and Quit-Attempts Among US Adults Following Medicaid Expansion,” Preventive Medicine Reports epub ahead of print (June 2019), https://www.sciencedirect.com/science/article/pii/S2211335519300981
- Jessica Vistnes and Joel Cohen, “Duration of Uninsured Spells For Nonelderly Adults Declined After 2014,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2017.1638
- Jessica Vistnes and Joel Cohen, “Gaining Coverage in 2014: New Estimates of Marketplace and Medicaid Transitions,” Health Affairs 35 no. 10 (October 2016): 1825-1829, http://content.healthaffairs.org/content/35/10/1825.full?sid=cc385dd5-9c95-4ee1-9c58-888408d49c54
- Jacob Vogler, Access to Health Care and Criminal Behavior: Short-Run Evidence from the ACA Medicaid Expansions (University of Illinois at Urbana-Champaign, November 2017), https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3042267
- Vikki Wachino and Samantha Artiga, How Connecting Justice-Involved Individuals to Medicaid Can Help Address the Opioid Epidemic (Washington, DC: Kaiser Family Foundation, June 2019), https://www.kff.org/medicaid/issue-brief/how-connecting-justice-involved-individuals-to-medicaid-can-help-address-the-opioid-epidemic/
- Rishi Wadhera et al., “Association of the Affordable Care Act’s Medicaid Expansion With Care Quality and Outcomes for Low-Income Patients Hospitalized With Heart Failure,” Circulation: Cardiovascular Quality and Outcomes 11, no. 7 (June 2018), https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.118.004729
- Rishi Wadhera et al., “Association of State Medicaid Expansion With Quality of Care and Outcomes for Low-Income Patients Hospitalized With Acute Myocardial Infarction,” JAMA Cardiology 4, no. 2 (January 2019): 120-127, https://jamanetwork.com/journals/jamacardiology/article-abstract/2720425?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamacardio.2018.4577
- Steven Wallace, Maria-Elena Young, Michael Rodriguez, Amy Bonilla, and Nadereh Pourat, Community Health Centers Play a Critical Role in Caring for the Remaining Uninsured in the Affordable Care Act Era (UCLA Center for Health Policy Research, October 2016), http://healthpolicy.ucla.edu/publications/Documents/PDF/2016/FQHC_PB-oct2016.pdf
- Bryce Ward and Brandon Bridge, The Economic Impact of Medicaid Expansion in Montana: Updated Findings (Bureau of Business and Economic Research, January 2019), https://mthcf.org/wp-content/uploads/2019/01/Economic-Impact-of-MedEx-in-MT_1.28.19-FINAL.pdf
- Matt Warfield, Barbara DiPietro, and Samantha Artiga, How has the ACA Medicaid Expansion Affected Providers Serving the Homeless Population: Analysis of Coverage, Revenues, and Costs (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, March 2016), https://files.kff.org/attachment/issue-brief-how-has-the-aca-medicaid-expansion-affected-providers-serving-the-homeless-population
- George Wehby and Wei Lyu, “The Impact of the ACA Medicaid Expansions on Health Insurance Coverage through 2015 and Coverage Disparities by Age, Race/Ethnicity, and Gender” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12711/abstract
- Hefei Wen, Tyrone Borders, and Benjamin Druss, ”Number of Medicaid Prescriptions Grew, Drug Spending was Steady in Medicaid Expansion States,” Health Affairs 35, no. 12 (September 2016): 1604-1607, http://content.healthaffairs.org/content/35/9/1604.full
- Hefei Wen, Jason Hockenberry, Tyrone Borders, and Benjamin Druss, “Impact of Medicaid Expansion on Medicaid-covered Utilization of Buprenorphine for Opioid Use Disorder Treatment,” Medical Care 55 no. 4 (April 2017): 336-341, http://journals.lww.com/lww-medicalcare/Fulltext/2017/04000/Impact_of_Medicaid_Expansion_on_Medicaid_covered.5.aspx
- Hefei Wen, Kenton J. Johnston, Lindsay Allen, and Teresa M. Waters, “Medicaid Expansion Associated With Reductions In Preventable Hospitalizations,” Health Affairs 38, no. 11 (November 2019): 1845-1849, https://doi.org/10.1377/hlthaff.2019.00483
- Hefei Wen, Adam S. Wilk, and Benjamin G. Druss, “Medicaid Acceptance by Psychiatrists Before and After Medicaid Expansion,” JAMA Psychiatry epub ahead of print (June 2019), https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2735109?resultClick=1
- Laura Wherry and Sarah Miller, “Early Coverage, Access, Utilization, and Health Effects Associated with the Affordable Care Act Medicaid Expansions: A Quasi-experimental Study,” Annals of Internal Medicine, Epub ahead of print (April 2016), http://annals.org/article.aspx?articleid=2513980
- Alanna Williamson, Larisa Antonisse, Jennifer Tolbert, Rachel Garfield, and Anthony Damico, ACA Coverage Expansions and Low-Income Workers (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2016), http://kff.org/report-section/aca-coverage-expansions-and-low-income-workers-issue-brief/
- Tyler Winkelman and Virginia Chang, “Medicaid Expansion, Mental Health, and Access to Care Among Childless Adults With and Without Chronic Conditions,” Journal of General Internal Medicine epub ahead of print (November 2017), https://www.ncbi.nlm.nih.gov/pubmed/29181792
- Tyler Winkelman, Edith Kieffer, Susan Goold, Jeffrey Morenoff, Kristen Cross, and John Ayanian, “Health Insurance Trends and Access to Behavioral Health Care Among Justice-Involved Individuals,” Journal of General Internal Medicine 31, no. 12 (December 2016): 1523-1529, https://www.ncbi.nlm.nih.gov/pubmed/27638837
- Jane Wishner, Patricia Solleveld, Robin Rudowitz, Julia Paradise, and Larisa Antonisse, A Look at Rural Hospital Closures and Implications for Access to Care: Three Case Studies (Washington, DC: Kaiser Commission on Medicaid and the Uninsured and The Urban Institute, July 2016), http://kff.org/medicaid/issue-brief/a-look-at-rural-hospital-closures-and-implications-for-access-to-care/
- Christian Wolfe, Kathryn Rennie, and Christopher Truffer, 2017 Actuarial Report on the Financial Outlook for Medicaid (Office of the Actuary, Centers for Medicare and Medicaid Services, September 2018), https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/Downloads/MedicaidReport2017.pdf
- Joanna Woronkowicz, Aparna Soni, Seth Freedman, and Kosali Simon, “How Have Recent Health Insurance Expansions Affected Coverage Among Artist Occupations In The USA?,” Journal of Cultural Economics (May 2019), https://link.springer.com/article/10.1007/s10824-019-09352-5
- Brad Wright et al., “Completion of Requirements in Iowa’s Medicaid Expansion Premium Disincentive Program, 2014–2015,” American Journal of Public Health 108, no. 2 (February 2018): 219-223, http://ajph.aphapublications.org/doi/full/10.2105/AJPH.2017.304178
- Vivian Wu et al., “Early Impact of the Affordable Care Act Coverage Expansion on Safety-Net Hospital Inpatient Payer Mix and Market Shares,” Health Services Research (January 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12812/full
- Deborah Yip et al., “Association of Medicaid Expansion and Health Insurance with Receipt of Smoking Cessation Services and Smoking Behaviors in Substance Use Disorder Treatment,” The Journal of Behavioral Health Services & Research (July 2019), https://doi.org/10.1007/s11414-019-09669-1
- Gary Young, Stephen Flaherty, E. Zepeda, Simone Singh, and Sara Rosenbaum, “Impact of ACA Medicaid Expansion on Hospitals’ Financial Status” Journal of Healthcare Management 64, no. 2 (March 2019): 91–102, https://insights.ovid.com/crossref?an=00115514-201904000-00007
- Dahai Yue, Petra Rasmussen, and Ninez Ponce, “Racial/Ethnic Differential Effects of Medicaid Expansion on Health Care Access,” Health Services Research (February 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12834/abstract
- Yasmin Zerhouni et al., “Effect of Medicaid Expansion on Colorectal Cancer Screening Rates,” Diseases of the Colon & Rectum 62, no. 1 (January 2019): 97-103, https://journals.lww.com/dcrjournal/Abstract/2019/01000/Effect_of_Medicaid_Expansion_on_Colorectal_Cancer.16.aspx
- Naomi Zewde, Erica Eliason, Heidi Allen, and Tal Gross, “The Effects of the ACA Medicaid Expansion on Nationwide Home Evictions and Eviction-Court Initiations: United States, 2000-2016,” American Journal of Public Health 109, no. 10 (October 2019): 1379-1383, https://doi.org/10.2105/ajph.2019.305230
- Naomi Zewde and Christopher Wimer, “Antipoverty Impact Of Medicaid Growing With State Expansions Over Time,” Health Affairs 38, no. 1 (January 2019), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05155
- Cheryl Zogg et al., “Association of Medicaid Expansion With Access to Rehabilitative Care in Adult Trauma Patients,” JAMA Surgery epub ahead of print (January 2019), https://jamanetwork.com/journals/jamasurgery/article-abstract/2719270?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamasurg.2018.5177
- Cheryl Zogg et al., “Impact of Affordable Care Act Insurance Expansion on Pre-Hospital Access to Care: Changes in Adult Perforated Appendix Admission Rates after Medicaid Expansion and the Dependent Coverage Provision,” Journal of the American College of Surgeons 228, no. 1 (January 2019): 29-43, https://www.journalacs.org/article/S1072-7515(18)32078-7/fulltext
- Emily Zylla, Colin Planalp, Elizabeth Lukanen, and Lynn Blewett, “Section 1115 Medicaid Expansion Waivers: Implementation Experiences,” (Medicaid and CHIP Payment and Access Commission, February 2018), https://www.macpac.gov/publication/section-1115-medicaid-expansion-waivers-implementation-experiences/
Endnotes
- This is an update to four earlier versions of this issue brief that covered studies published through May 2016, January 2017, June 2017, February 2018, and June 2019. ↩︎
- Mark Olfson et al., “A National Survey of Trends in Health Insurance Coverage of Low-Income Adults Following Medicaid Expansion,” Journal of General Internal Medicine Epub ahead of print (October 2019), https://doi.org/10.1007/s11606-019-05409-5 ↩︎
- John A. Graves et al., “Medicaid Expansion Slowed Rates of Health Decline for Low-Income Adults in Southern States,” Health Affairs 39, no. 1 (January 2020): 67-76, https://doi.org/10.1377/hlthaff.2019.00929 ↩︎
- Jim P. Stimpson, Jessie Kemmick Pintor, and Fernando A. Wilson, “Association of Medicaid Expansion with Health Insurance Coverage by Marital Status and Sex,” PLoS One 14, no. 10 (October 2019), https://doi.org/10.1371/journal.pone.0223556 ↩︎
- Jim P. Stimpson et al., “Association of Medicaid Expansion With Health Insurance Coverage Among Persons With a Disability,” JAMA Network Open 2, no. 7 (July 2019), https://doi.org/10.1001/jamanetworkopen.2019.7136 ↩︎
- Gracie Himmelstein, “Effect of the Affordable Care Act’s Medicaid Expansions on Food Security, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1243-1248, https://doi.org/10.2105/ajph.2019.305168 ↩︎
- Sumit D. Agarwal, Anna L. Goldman, and Benjamin D. Sommers, “Blue-Collar Workers Had Greatest Insurance Gains After ACA Implementation,” Health Affairs 38, no. 7 (July 2019): 1140-1144, https://doi.org/10.1377/hlthaff.2018.05454 ↩︎
- Michel Boudreaux, James M. Noon, Brett Fried, and Joanne Pascale, “Medicaid Expansion and the Medicaid Undercount in the American Community Survey,” Health Services Research 54, no. 6 (December 2019): 1263-1272, https://doi.org/10.1111/1475-6773.13213 ↩︎
- Hiroshi Gotanda, Gerald Kominski, and Yusuke Tsugawa, “Association Between the ACA Medicaid Expansions and Primary Care and Emergency Department Use During the First 3 Years,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05458-w ↩︎
- Lucie Schmidt, Lara Shore-Sheppard, and Tara Watson, The Impact of the ACA Medicaid Expansion on Disability Program Applications (National Bureau of Economic Research, Working Paper No. 26192, August 2019), http://www.nber.org/papers/w26192 ↩︎
- James A. Richardson, Jared J. Llorens, and Roy L. Heidelberg. Medicaid Expansion and the Louisiana Economy, 2018 and 2019 (Louisiana Department of Health, Prepared by Louisiana State University, August 2019), http://ldh.la.gov/assets/media/3and4.2019FinalReportMedicaidExpansionstudy.pdf ↩︎
- Nevada’s Medicaid Population, (Las Vegas, NV: The Guinn Center, September 2019), https://guinncenter.org/wp-content/uploads/2019/09/Guinn-Center-NV-Medicaid-Population-Characteristics-2019.pdf ↩︎
- Charles J. Courtemanche et al., The Impact of the ACA on Insurance Coverage Disparities After Four Years (National Bureau of Economic Research, Working Paper No. 26157, August 2019), http://www.nber.org/papers/w26157 ↩︎
- Charles J. Courtemanche, James Marton, and Aaron Yelowitz, Medicaid Coverage across the Income Distribution under the Affordable Care Act (National Bureau of Economic Research, Working Paper No. 26145, August 2019), http://www.nber.org/papers/w26145 ↩︎
- Sarah Miller and Laura Wherry, “Four Years Later: Insurance Coverage and Access to Care Continue to Diverge between ACA Medicaid Expansion and Non-Expansion States,” American Economic Association Papers and Proceedings 109 (May 2019): 327-333, https://www.aeaweb.org/articles?id=10.1257/pandp.20191046 ↩︎
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, and Ishtiaque Fazlul, “The Three‐Year Impact of the Affordable Care Act on Disparities in Insurance Coverage,” Health Services Research (October 2018), https://onlinelibrary.wiley.com/doi/10.1111/1475-6773.13077 ↩︎
- Laura Skopec, John Holahan, and Caroline Elmendorf, Changes in Health Insurance Coverage 2013–2016: Medicaid Expansion States Lead the Way, (Washington, DC: The Urban Institute, September 2018), https://www.urban.org/sites/default/files/publication/98989/changes_in_health_insurance_coverage_2013-2016_medicaid_expansion_states_lead_the_way_1.pdf ↩︎
- Stephen Barnes, Mike Henderson, Dek Terrell, and Stephanie Virgets, 2017 Louisiana Health Insurance Survey (Louisiana Department of Health, Prepared by the Louisana State University E.J. Ourso College of Business, August 2018), http://ldh.la.gov/assets/media/2017-Louisiana-Health-Insurance-Survey-Report.pdf ↩︎
- Pennsylvania Department of Human Services, Medicaid Expansion Report, (Pennsylvania Department of Human Services, January 2017), http://www.dhs.pa.gov/cs/groups/webcontent/documents/document/c_257436.pdf ↩︎
- Seth Freedman, Lilliard Richardson, and Kosali Simon, “Learning From Waiver States: Coverage Effects Under Indiana’s HIP Medicaid Expansion,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1596 ↩︎
- Abeer Alharbi, M. Mahmud Khan, Ronnie Horner, Heather Brandt, and Cole Chapman, “Impact Of Medicaid Coverage Expansion Under The Affordable Care Act On Mammography And Pap Tests Utilization Among Low-Income Women,” PLOS One (April 2019), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0214886 ↩︎
- Alina Denham and Peter Veazie, “Did Medicaid Expansion Matter in States with Generous Medicaid?” The American Journal of Managed Care 25, no. 3 (March 2019): 129-134, https://www.ajmc.com/journals/issue/2019/2019-vol25-n3/did-medicaid-expansion-matter-in-states-with-generous-medicaid ↩︎
- Kevin Callison and Paul Sicilian, “Economic Freedom and the Affordable Care Act: Medicaid Expansions and Labor Mobility by Race and Ethnicity,” Public Finance Review 46, no. 2 (March 2018), https://journals.sagepub.com/doi/abs/10.1177/1091142116668254 ↩︎
- Helen Levy, Thomas Buchmueller, and Sayeh Nikpay, “The Impact of Medicaid Expansion on Household Consumption,” Eastern Economic Journal 45, no. 1 (January 2019): 34-57, https://link.springer.com/article/10.1057/s41302-018-0124-7 ↩︎
- Michael Dworsky and Christine Eibner, The Effect of the 2014 Medicaid Expansion on Insurance Coverage for Newly Eligible Childless Adults (Santa Monica, CA: Rand Corporation, 2016), https://www.rand.org/pubs/research_reports/RR1736.html ↩︎
- Colleen M. Carey, Sarah Miller, and Laura R. Wherry, The Impact of Insurance Expansions on the Already Insured: The Affordable Care Act and Medicare, (National Bureau of Economic Research, Working Paper Series No. 25153, October 2018), https://www.nber.org/papers/w25153 ↩︎
- Frederic Blavin, Michael Karpman, Genevieve Kenney, and Benjamin Sommers, “Medicaid Versus Marketplace Coverage for Near-Poor Adults: Effects on Out-Of-Pocket Spending and Coverage,” Health Affairs 37 no. 2 (January 2018), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.1166 ↩︎
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890 ↩︎
- Louisiana Department of Health, Medicaid Expansion 2016/17 (Baton Rouge, Louisiana Department of Health, June 2017), http://dhh.louisiana.gov/assets/HealthyLa/Resources/MdcdExpnAnnlRprt_2017_WEB.pdf ↩︎
- Joshua Clinton and Michael Sances, “The Politics of Policy: The Initial Mass Political Effects of Medicaid Expansion in the States,” American Political Science Review 112, no. 1 (February 2018): 167-185, https://www.cambridge.org/core/journals/american-political-science-review/article/politics-of-policy-the-initial-mass-political-effects-of-medicaid-expansion-in-the-states/246AA0F10B44EFD62A7B27C661730823 ↩︎
- Sandra Decker, Brandy Lipton, and Benjamin Sommers, “Medicaid Expansion Coverage Effects Grew in 2015 With Continued Improvements in Coverage Quality,” Health Affairs 36 no. 5 (May 2017): 819-825, http://content.healthaffairs.org/content/36/5/819.full ↩︎
- Abigail Barker, Kelsey Huntzberry, Timothy McBride, and Keith Mueller, Changing Rural and Urban Enrollment in State Medicaid Programs (Iowa City, IA: Rural Policy Research Institute, May 2017), https://cph.uiowa.edu/rupri/publications/policybriefs/2017/Changing%20Rural%20and%20Urban%20Enrollment%20in%20State%20Medicaid%20Programs.pdf ↩︎
- George Wehby and Wei Lyu, “The Impact of the ACA Medicaid Expansions on Health Insurance Coverage through 2015 and Coverage Disparities by Age, Race/Ethnicity, and Gender” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12711/abstract ↩︎
- Robin Rudowitz, Laura Snyder, and Vernon Smith, Medicaid Enrollment & Spending Growth: FY 2015 & 2016 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, October 2015), http://kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2015-2016/ ↩︎
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf ↩︎
- Samantha Artiga, Jennifer Tolbert, and Robin Rudowitz, Year Two of the ACA Coverage Expansions: On-the-Ground Experiences from Five States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/health-reform/issue-brief/year-two-of-the-aca-coverage-expansions-on-the-ground-experiences-from-five-states/ ↩︎
- Laura Wherry and Sarah Miller, “Early Coverage, Access, Utilization, and Health Effects Associated with the Affordable Care Act Medicaid Expansions: A Quasi-experimental Study,” Annals of Internal Medicine, Epub ahead of print (April 2016), http://annals.org/article.aspx?articleid=2513980 ↩︎
- Anne Martin et al., “National Health Spending: Faster Growth in 2015 As Coverage Expands and Utilization Increases,” Health Affairs 36 no. 1 (January 2017): 166-176, http://content.healthaffairs.org/content/36/1/166.full?sid=982b20c0-0a17-4dc4-a35a-b0302d4ec289 ↩︎
- Benjamin Sommers, Robert Blendon, and E. John Orav, “Both the ‘Private Option’ And Traditional Medicaid Expansions Improved Access To Care For Low-Income Adults,” Health Affairs 35, no. 1 (January 2016): 96-105, http://content.healthaffairs.org/content/35/1/96.abstract ↩︎
- Robin Rudowitz, Allison Valentine, and Vernon Smith, Medicaid Enrollment and Spending Growth: FY 2016 & 2017 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, October 2016), http://kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2016-2017/ ↩︎
- Jessica Vistnes and Joel Cohen, “Gaining Coverage in 2014: New Estimates of Marketplace and Medicaid Transitions,” Health Affairs 35 no. 10 (October 2016): 1825-1829, http://content.healthaffairs.org/content/35/10/1825.full?sid=cc385dd5-9c95-4ee1-9c58-888408d49c54 ↩︎
- Pauline Leung and Alexandre Mas, Employment Effects of the ACA Medicaid Expansions (Working Paper No. 22540, National Bureau of Economic Research, August 2016), http://www.nber.org/papers/w22540 ↩︎
- Kamyar Nasseh and Marko Vujicic, Early Impact of the Affordable Care Act’s Medicaid Expansion on Dental Care Use (Health Services Research, November 2016), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12606/full ↩︎
- Christian Wolfe, Kathryn Rennie, and Christopher Truffer, 2017 Actuarial Report on the Financial Outlook for Medicaid (Office of the Actuary, Centers for Medicare and Medicaid Services, September 2018), https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/Downloads/MedicaidReport2017.pdf ↩︎
- Aparna Soni, Michael Hendryx, and Kosali Simon, “Medicaid Expansion under the Affordable Care Act and Insurance Coverage in Rural and Urban Areas,” The Journal of Rural Health epub ahead of print (January 2017), http://onlinelibrary.wiley.com/doi/10.1111/jrh.12234/full ↩︎
- Molly Frean, Jonathan Gruber, and Benjamin Sommers, Premium Subsidies, the Mandate, and Medicaid Expansion: Coverage Effects of the Affordable Care Act (Working Paper No. 22213, National Bureau of Economic Research, April 2016), http://www.nber.org/papers/w22213?utm_campaign=ntw&utm_medium=email&utm_source=ntw ↩︎
- Stan Dorn, Norton Francis, Laura Snyder, and Robin Rudowitz, The Effects of the Medicaid Expansion on State Budgets: An Early Look in Select States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, March 2015), http://kff.org/medicaid/issue-brief/the-effects-of-the-medicaid-expansion-on-state-budgets-an-early-look-in-select-states/ ↩︎
- Sarah Gordon, Benjamin Sommers, Ira Wilson, Omar Galarraga, and Amal Trivedi, “The Impact of Medicaid Expansion on Continuous Enrollment: a Two State Analysis,” Journal of General Internal Medicine epub ahead of print (June 2019), https://link.springer.com/article/10.1007/s11606-019-05101-8 ↩︎
- MaryBeth Musumeci, Priya Chidambaram, and Molly O’Malley Watts, Key Questions About Medicaid Home and Community-Based Services Waiver Waiting Lists (Washington, DC: Kaiser Family Foundation, April 2019), https://modern.kff.org/medicaid/issue-brief/key-questions-about-medicaid-home-and-community-based-services-waiver-waiting-lists/ ↩︎
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562 ↩︎
- Jim Stimpson and Fernando Wilson, “Medicaid Expansion Improved Health Insurance Coverage For Immigrants, But Disparities Persist,” Health Affairs 37, no. 10 (October 2018), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.0181 ↩︎
- Adele Shartzer, Frederic Blavin, and John Holohan, “Employer-Sponsored Insurance Stable For Low-Income Workers In Medicaid Expansion States,” Health Affairs 37, no. 4 (April 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1205 ↩︎
- Benjamin Sommers, Carrie Fry, Robert Blendon, and Arnold Epstein, “New Approaches in Medicaid: Work Requirements, Health Savings Accounts, and Health Care Access,” Health Affairs 37, no. 7 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2018.0331 ↩︎
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf ↩︎
- Julia Foutz, Samantha Artiga, and Rachel Garfield, The Role of Medicaid in Rural America (Washington, DC: Kaiser Family Foundation, April 2017), http://kff.org/medicaid/issue-brief/the-role-of-medicaid-in-rural-america/ ↩︎
- Sara Collins, Munira Gunja, Michelle Doty, and Sophie Beutel, Americans’ Experiences with ACA Marketplace and Medicaid Coverage: Access to Care and Satisfaction (The Commonwealth Fund, May 2016), http://www.commonwealthfund.org/publications/issue-briefs/2016/may/aca-tracking-survey-access-to-care-and-satisfaction ↩︎
- Robin Rudowitz, Samantha Artiga, Anthony Damico, and Rachel Garfield, A Closer Look at the Remaining Uninsured Population Eligible for Medicaid and CHIP (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, February 2016), http://kff.org/uninsured/issue-brief/a-closer-look-at-the-remaining-uninsured-population-eligible-for-medicaid-and-chip/ ↩︎
- Michael McCue, “The Impact of Medicaid Expansion on Medicaid Focused Insurers in California,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 52 (July 2015), http://inq.sagepub.com/content/52/0046958015595960.full.pdf+html ↩︎
- Nicolas Ajkay et al, “Early Impact of Medicaid Expansion and Quality of Breast Cancer Care in Kentucky,” Journal of the American College of Surgeons, epub ahead of print, February 2018, https://www.sciencedirect.com/science/article/pii/S107275151830022X ↩︎
- Centers for Medicare and Medicaid Services, Monthly Medicaid and CHIP Application, Eligibility, Determination, and Enrollment Reports, (Centers for Medicare and Medicaid Services, March 2016), https://www.medicaid.gov/medicaid-chip-program-information/program-information/medicaid-and-chip-enrollment-data/medicaid-and-chip-application-eligibility-determination-and-enrollment-data.html ↩︎
- Jessica Vistnes and Joel Cohen, “Duration of Uninsured Spells For Nonelderly Adults Declined After 2014,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2017.1638 ↩︎
- Mark Olfson et al., “A National Survey of Trends in Health Insurance Coverage of Low-Income Adults Following Medicaid Expansion,” Journal of General Internal Medicine Epub ahead of print (October 2019), https://doi.org/10.1007/s11606-019-05409-5 ↩︎
- Jesse C. Baumgartner, Sara R. Collins, David C. Radley, and Susan L. Hayes, How the Affordable Care Act Has Narrowed Racial and Ethnic Disparities in Access to Health Care (The Commonwealth Fund, January 2020), https://www.commonwealthfund.org/publications/2020/jan/how-ACA-narrowed-racial-ethnic-disparities-access ↩︎
- Anna L. Goldman and Benjamin D. Sommers, “Among Low-Income Adults Enrolled In Medicaid, Churning Decreased After The Affordable Care Act,” Health Affairs 39, no. 1 (January 2020): 85-93, https://doi.org/10.1377/hlthaff.2019.00378 ↩︎
- Amandeep R. Mahal et al., “Early Impact of the Affordable Care Act and Medicaid Expansion on Racial and Socioeconomic Disparities in Cancer Care,” American Journal of Clinical Oncology Epub ahead of print (January 2020), https://doi.org/10.1097/coc.0000000000000588 ↩︎
- Jennifer M. Lobo et al., “Trends in Uninsured Rates Before and After Medicaid Expansion in Counties Within and Outside of the Diabetes Belt,” Diabetes Care Epub ahead of print (January 2020), https://doi.org/10.2337/dc19-0874 ↩︎
- John A. Graves et al., “Medicaid Expansion Slowed Rates of Health Decline for Low-Income Adults in Southern States,” Health Affairs 39, no. 1 (January 2020): 67-76, https://doi.org/10.1377/hlthaff.2019.00929 ↩︎
- Lizhong Peng, Xiaohui Guo, and Chad D. Meyerhoefer, “The Effects of Medicaid Expansion on Labor Market Outcomes: Evidence from Border Counties,” Health Economics Epub ahead of print (December 2019), https://doi.org/10.1002/hec.3976 ↩︎
- Deborah Yip et al., “Association of Medicaid Expansion and Health Insurance with Receipt of Smoking Cessation Services and Smoking Behaviors in Substance Use Disorder Treatment,” The Journal of Behavioral Health Services & Research (July 2019), https://doi.org/10.1007/s11414-019-09669-1 ↩︎
- Laura Skopec, John Holahan, and Caroline Elmendorf, Health Insurance Coverage Declined for Nonelderly Americans Between 2016 and 2017, Primarily in States That Did Not Expand Medicaid (Washington, DC: The Urban Institute, August 2019), https://www.urban.org/research/publication/health-insurance-coverage-declined-nonelderly-americans-between-2016-and-2017-primarily-states-did-not-expand-medicaid ↩︎
- Shiho Kino and Ichiro Kawachi, “Can Health Literacy Boost Health Services Utilization in the Context of Expanded Access to Health Insurance?,” Health Education & Behavior Epub ahead of print (October 2019), https://doi.org/10.1177/1090198119875998 ↩︎
- Jim P. Stimpson, Jessie Kemmick Pintor, and Fernando A. Wilson, “Association of Medicaid Expansion with Health Insurance Coverage by Marital Status and Sex,” PLoS One 14, no. 10 (October 2019), https://doi.org/10.1371/journal.pone.0223556 ↩︎
- Jim P. Stimpson et al., “Association of Medicaid Expansion With Health Insurance Coverage Among Persons With a Disability,” JAMA Network Open 2, no. 7 (July 2019), https://doi.org/10.1001/jamanetworkopen.2019.7136 ↩︎
- Aparna Soni, Michael Hendryx, and Kosali Simon, “Medicaid Expansion under the Affordable Care Act and Insurance Coverage in Rural and Urban Areas,” The Journal of Rural Health epub ahead of print (January 2017), http://onlinelibrary.wiley.com/doi/10.1111/jrh.12234/full ↩︎
- Lindsay C. Kobayashi, Onur Altindag, Yulya Truskinovsky, and Lisa F. Berkman, “Effects of the Affordable Care Act Medicaid Expansion on Subjective Well-Being in the US Adult Population, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1236-1242, https://doi.org/10.2105/ajph.2019.305164 ↩︎
- Hiroshi Gotanda, Gerald Kominski, and Yusuke Tsugawa, “Association Between the ACA Medicaid Expansions and Primary Care and Emergency Department Use During the First 3 Years,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05458-w ↩︎
- James A. Richardson, Jared J. Llorens, and Roy L. Heidelberg. Medicaid Expansion and the Louisiana Economy, 2018 and 2019 (Louisiana Department of Health, Prepared by Louisiana State University, August 2019), http://ldh.la.gov/assets/media/3and4.2019FinalReportMedicaidExpansionstudy.pdf ↩︎
- Sri Lekha Tummalapalli, Samuel Leonard, Michelle M. Estrella, and Salomeh Keyhani, “The Effect of Medicaid Expansion on Self-Reported Kidney Disease,” Clinical Journal of American Society of Nephrology 14, no. 8 (August 2019): 1238-1240, https://doi.org/10.2215/cjn.02310219 ↩︎
- Sarah Miller and Laura Wherry, “Four Years Later: Insurance Coverage and Access to Care Continue to Diverge between ACA Medicaid Expansion and Non-Expansion States,” American Economic Association Papers and Proceedings 109 (May 2019): 327-333, https://www.aeaweb.org/articles?id=10.1257/pandp.20191046 ↩︎
- Hyunjung Lee and Frank Porell, “The Effect of the Affordable Care Act Medicaid Expansion on Disparities in Access to Care and Health Status,” Medical Care Research and Review epub ahead of print (October 2018), https://journals.sagepub.com/doi/abs/10.1177/1077558718808709?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=mcrd ↩︎
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, and Ishtiaque Fazlul, “The Three‐Year Impact of the Affordable Care Act on Disparities in Insurance Coverage,” Health Services Research (October 2018), https://onlinelibrary.wiley.com/doi/10.1111/1475-6773.13077 ↩︎
- Laura Skopec, John Holahan, and Caroline Elmendorf, Changes in Health Insurance Coverage 2013–2016: Medicaid Expansion States Lead the Way, (Washington, DC: The Urban Institute, September 2018), https://www.urban.org/sites/default/files/publication/98989/changes_in_health_insurance_coverage_2013-2016_medicaid_expansion_states_lead_the_way_1.pdf ↩︎
- Stephen Barnes, Mike Henderson, Dek Terrell, and Stephanie Virgets, 2017 Louisiana Health Insurance Survey (Louisiana Department of Health, Prepared by the Louisana State University E.J. Ourso College of Business, August 2018), http://ldh.la.gov/assets/media/2017-Louisiana-Health-Insurance-Survey-Report.pdf ↩︎
- Robin Cohen, Emily Terlizzi, and Michael Martinez, Health Insurance Coverage: Early Release of Estimates from the National Health Interview Survey, 2018 (National Center for Health Statistics, May 2019), https://www.cdc.gov/nchs/data/nhis/earlyrelease/insur201905.pdf ↩︎
- Christina Goe, 2018 Report on Health Coverage and Montana’s Uninsured (Montana Helathcare Foundation, prepared by Christina Lechner Goe, May 2018), https://mthcf.org/wp-content/uploads/2018/06/Uninsured-Report_FINAL-Design_5.17.18.pdf ↩︎
- Pennsylvania Department of Human Services, Medicaid Expansion Report, (Pennsylvania Department of Human Services, January 2017), http://www.dhs.pa.gov/cs/groups/webcontent/documents/document/c_257436.pdf ↩︎
- Seth Freedman, Lilliard Richardson, and Kosali Simon, “Learning From Waiver States: Coverage Effects Under Indiana’s HIP Medicaid Expansion,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1596 ↩︎
- John Cawley, Aparna Soni, and Kosali Simon, “Third Year of Survey Data Shows Continuing Benefits of Medicaid Expansions for Low-Income Childless Adults in the U.S.,” Journal of General Internal Medicine 33, no. 9 (September 2018): 1495-1497, https://link.springer.com/article/10.1007%2Fs11606-018-4537-0 ↩︎
- Kosali Simon, Aparna Soni, and John Cawley, “The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions” Journal of Policy Analysis and Management 36, no. 2 (March 2017), https://onlinelibrary.wiley.com/doi/abs/10.1002/pam.21972 ↩︎
- Michael Dworsky and Christine Eibner, The Effect of the 2014 Medicaid Expansion on Insurance Coverage for Newly Eligible Childless Adults (Santa Monica, CA: Rand Corporation, 2016), https://www.rand.org/pubs/research_reports/RR1736.html ↩︎
- Frederic Blavin, Michael Karpman, Genevieve Kenney, and Benjamin Sommers, “Medicaid Versus Marketplace Coverage for Near-Poor Adults: Effects on Out-Of-Pocket Spending and Coverage,” Health Affairs 37 no. 2 (January 2018), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.1166 ↩︎
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830 ↩︎
- Susan Hayes, Sara Collins, David Radley, and Douglas McCarthy, What’s at Stake: States’ Progress on Health Coverage and Access to Care, 2013-2016 (The Commonwealth Fund, December 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/dec/states-progress-health-coverage-and-access ↩︎
- Sharon Long, Lea Bart, Michael Karpman, Adele Shartzer, and Stephen Zuckerman, “Sustained Gains in Coverage, Access, and Affordability Under the ACA: A 2017 Update,” Health Affairs 36 no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0798 ↩︎
- Kevin Griffith, Leigh Evans, and Jacob Bor, “The Affordable Care Act Reduced Socioeconomic Disparities in Health Care Access,” Health Affairs 36 no. 8 (August 2017), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0083 ↩︎
- Aaron Sojourner and Ezra Golberstein, “Medicaid Expansion Reduced Unpaid Medical Debt and Increased Financial Satisfaction,” Health Affairs (July 2017), https://www.healthaffairs.org/do/10.1377/hblog20170724.061160/full/ ↩︎
- Sunha Choi, Sungkyu Lee, and Jason Matejkowski, “The Effects of State Medicaid Expansion on Low-Income Individuals’ Access to Health Care: Multilevel Modeling,” Population Health Management epub ahead of print (September 2017), http://online.liebertpub.com/doi/abs/10.1089/pop.2017.0104 ↩︎
- Dahai Yue, Petra Rasmussen, and Ninez Ponce, “Racial/Ethnic Differential Effects of Medicaid Expansion on Health Care Access,” Health Services Research (February 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12834/abstract ↩︎
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890 ↩︎
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293 ↩︎
- Sandra Decker, Brandy Lipton, and Benjamin Sommers, “Medicaid Expansion Coverage Effects Grew in 2015 With Continued Improvements in Coverage Quality,” Health Affairs 36 no. 5 (May 2017): 819-825, http://content.healthaffairs.org/content/36/5/819.full ↩︎
- Sandra Decker and Brandy Lipton, “Most Newly Insured People in 2014 Were Long-Term Uninsured,” Health Affairs 36 no. 1 (January 2017): 16-20, http://content.healthaffairs.org/content/36/1/16.full?sid=982b20c0-0a17-4dc4-a35a-b0302d4ec289 ↩︎
- George Wehby and Wei Lyu, “The Impact of the ACA Medicaid Expansions on Health Insurance Coverage through 2015 and Coverage Disparities by Age, Race/Ethnicity, and Gender” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12711/abstract ↩︎
- Kelsey Avery, Kenneth Finegold, and Amelia Whitman, Affordable Care Act Has Led to Historic, Widespread Increase in Health Insurance Coverage (Office of the Assistant Secretary for Planning and Evaluation, September 2016), https://aspe.hhs.gov/sites/default/files/pdf/207946/ACAHistoricIncreaseCoverage.pdf ↩︎
- Eric Seiber and Micah Berman, “Medicaid Expansion and ACA Repeal: Evidence from Ohio,” American Journal of Public Health epub ahead of print (April 2017), http://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.2017.303722 ↩︎
- Office of the Assistant Secretary for Planning and Evaluation (ASPE), Impacts of the Affordable Care Act’s Medicaid Expansion on Insurance Coverage and Access to Care (Office of the Assistant Secretary for Planning and Evaluation, June 2016), https://aspe.hhs.gov/sites/default/files/pdf/205141/medicaidexpansion.pdf ↩︎
- Joseph Benitez, Liza Creel, and J’Aime Jennings, “Kentucky’s Medicaid Expansion Showing Early Promise on Coverage and Access to Care,” Health Affairs (February 2016), http://content.healthaffairs.org/content/early/2016/02/16/hlthaff.2015.1294 ↩︎
- Sara Collins, Petra Rasmussen, Michelle Doty, and Sophie Beutel The Rise in Health Care Coverage and Affordability Since Health Reform Took Effect: Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2014 (The Commonwealth Fund, January 2015), http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2015/jan/1800_collins_biennial_survey_brief.pdf?la=en ↩︎
- Benjamin Sommers, Robert Blendon, and E. John Orav, “Both the ‘Private Option’ And Traditional Medicaid Expansions Improved Access To Care For Low-Income Adults,” Health Affairs 35, no. 1 (January 2016): 96-105, http://content.healthaffairs.org/content/35/1/96.abstract ↩︎
- Benjamin Sommers, Munira Gunja, Kenneth Finegold, and Thomas Musco, “Changes in Self-Reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act,” The Journal of the American Medical Association 314 no. 4 (July 2015): 366-374, http://jama.jamanetwork.com/article.aspx?articleid=2411283&resultClick=3 ↩︎
- Jessica Smith and Carla Medalia, Health Insurance Coverage in the United States: 2014 (U.S. Census Bureau, September 2015), https://www.census.gov/content/dam/Census/library/publications/2015/demo/p60-253.pdf ↩︎
- Thomas Buchmueller, Zachary Levinson, Helen Levy, and Barbara Wolfe, “Effect of the Affordable Care Act on Racial and Ethnic Disparities in Health Insurance Coverage,” American Journal of Public Health (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27196653 ↩︎
- Kelsey Avery, Kenneth Finegold, and Amelia Whitman, Affordable Care Act Has Led to Historic, Widespread Increase in Health Insurance Coverage (Office of the Assistant Secretary for Planning and Evaluation, September 2016), https://aspe.hhs.gov/sites/default/files/pdf/207946/ACAHistoricIncreaseCoverage.pdf ↩︎
- Benjamin Sommers, Robert Blendon, E. John Orav, and Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420 ↩︎
- Benjamin Sommers, Thomas Musco, Kenneth Finegold, Munira Gunja, Amy Burke, and Audrey McDowell, “Health Reform and Changes in Health Insurance Coverage in 2014” The New England Journal of Medicine 371 (August 2014): 867-874, http://www.nejm.org/doi/full/10.1056/NEJMsr1406753 ↩︎
- Manatt Health, Medicaid Expansion: How It Affects Montana’s State Budget, Economy, and Residents (Montana Healthcare Foundation, prepared by Manatt Health, June 2018), https://mthcf.org/wp-content/uploads/2018/06/Manatt-MedEx_FINAL_6.1.18.pdf ↩︎
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf ↩︎
- Arkansas Health Reform Legislative Task Force, Health Care Task Force Preliminary Report, (Arkansas Health Reform Legislative Task Force, December 2015), http://www.arkleg.state.ar.us/assembly/2015/Meeting%20Attachments/836/I14218/Task%20Force%20report%2012-17-15%20sent%20to%20Jill.pdf ↩︎
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf ↩︎
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, and Daniela Zapata, Impacts of the Affordable Care Act on Health Insurance Coverage in Medicaid Expansion and Non-Expansion States (Working Paper No. 22182, The National Bureau of Economic Research, April 2016), http://www.nber.org/papers/w22182 ↩︎
- Amy Davidoff et al., “Changes in Health Insurance Coverage Associated With the Affordable Care Act Among Adults With and Without a Cancer History: Population-based National Estimates,” Medical Care 56, no. 3 (March 2018), https://journals.lww.com/lww-medicalcare/Abstract/2018/03000/Changes_in_Health_Insurance_Coverage_Associated.5.aspx ↩︎
- Joshua Clinton and Michael Sances, “The Politics of Policy: The Initial Mass Political Effects of Medicaid Expansion in the States,” American Political Science Review 112, no. 1 (February 2018): 167-185, https://www.cambridge.org/core/journals/american-political-science-review/article/politics-of-policy-the-initial-mass-political-effects-of-medicaid-expansion-in-the-states/246AA0F10B44EFD62A7B27C661730823 ↩︎
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562 ↩︎
- Laura Wherry and Sarah Miller, “Early Coverage, Access, Utilization, and Health Effects Associated with the Affordable Care Act Medicaid Expansions: A Quasi-experimental Study,” Annals of Internal Medicine, Epub ahead of print (April 2016), http://annals.org/article.aspx?articleid=2513980 ↩︎
- Benjamin Sommers, Rebecca Gourevitch, Bethany Maylone, Robert Blendon, and Arnold Epstein, “Insurance Churning Rates for Low-Income Adults Under Health Reform: Lower Than Expected but Still Harmful for Many,” Health Affairs 35 no. 10 (October 2016): 1816-1824, http://content.healthaffairs.org/content/35/10/1816.full?sid=f4835910-ffd0-4864-a76a-b4f207ccd018 ↩︎
- Jessica Vistnes and Joel Cohen, “Duration of Uninsured Spells For Nonelderly Adults Declined After 2014,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2017.1638 ↩︎
- Adele Shartzer, Frederic Blavin, and John Holohan, “Employer-Sponsored Insurance Stable For Low-Income Workers In Medicaid Expansion States,” Health Affairs 37, no. 4 (April 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1205 ↩︎
- Benjamin Sommers, Carrie Fry, Robert Blendon, and Arnold Epstein, “New Approaches in Medicaid: Work Requirements, Health Savings Accounts, and Health Care Access,” Health Affairs 37, no. 7 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2018.0331 ↩︎
- Pauline Leung and Alexandre Mas, Employment Effects of the ACA Medicaid Expansions (Working Paper No. 22540, National Bureau of Economic Research, August 2016), http://www.nber.org/papers/w22540 ↩︎
- John Heintzman, Steffani Bailey, Jennifer DeVoe, Stuart Cowburn, Tanya Kapka, Truc-Vi Duong, and Miguel Marino, “In Low-Income Latino Patients, Post-Affordable Care Act Insurance Disparities May Be Reduced Even More than Broader National Estimates: Evidence from Oregon,” Journal of Racial and Ethnic Health Disparities (April 2016), http://www.ncbi.nlm.nih.gov/pubmed/27105630 ↩︎
- Susan Hayes, Pamela Riley, David Radley, and Douglas McCarthy, Reducing Racial and Ethnic Disparities in Access to Care: Has the Affordable Care Act Made a Difference? (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/racial-ethnic-disparities-care ↩︎
- Sergio Gonzales and Benjamin Sommers, “Intra-Ethnic Coverage Disparities among Latinos and the Effects of Health Reform” Health Services Research epub ahead of print (June 2017), http://onlinelibrary.wiley.com/wol1/doi/10.1111/1475-6773.12733/full ↩︎
- Julia Foutz, Samantha Artiga, and Rachel Garfield, The Role of Medicaid in Rural America (Washington, DC: Kaiser Family Foundation, April 2017), http://kff.org/medicaid/issue-brief/the-role-of-medicaid-in-rural-america/ ↩︎
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, Early Effects of the Affordable Care Act on Health Care Access, Risky Health Behaviors, and Self-Assessed Health (National Bureau of Economic Research, Working Paper no. 23269, March 2017), http://www.nber.org/papers/w23269 ↩︎
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Jason Gates, “Marketplaces Helped Drive Coverage Gains in 2015; Affordability Problems Remained,” Health Affairs 35 no. 10 (October 2016): 1810-1815, http://content.healthaffairs.org/content/35/10/1810.full ↩︎
- Sharon Long, Michael Karpman, Adele Shartzer, Douglas Wissoker, Genevieve Kenney, Stephen Zuckerman, Nathaniel Anderson, and Katherine Hempstead, Taking Stock: Health Insurance Coverage under the ACA as of September 2014 (The Urban Institute, December 2014), http://hrms.urban.org/briefs/Health-Insurance-Coverage-under-the-ACA-as-of-September-2014.html ↩︎
- Nicolas Ajkay et al, “Early Impact of Medicaid Expansion and Quality of Breast Cancer Care in Kentucky,” Journal of the American College of Surgeons, epub ahead of print, February 2018, https://www.sciencedirect.com/science/article/pii/S107275151830022X ↩︎
- Molly Frean, Jonathan Gruber, and Benjamin Sommers, Premium Subsidies, the Mandate, and Medicaid Expansion: Coverage Effects of the Affordable Care Act (Working Paper No. 22213, National Bureau of Economic Research, April 2016), http://www.nber.org/papers/w22213?utm_campaign=ntw&utm_medium=email&utm_source=ntw ↩︎
- Dennis McCarty, Yifan Gu, John W. McIlveen, and Bonnie K. Lind, “Medicaid expansion and treatment for opioid use disorders in Oregon: an interrupted time-series analysis,” Addiction Science & Clinical Practice 14 (August 2019), https://doi.org/10.1186/s13722-019-0160-6 ↩︎
- Sarah H. Gordon, Benjamin D. Sommers, Ira B. Wilson, and Amal N. Trivedi, “Effects Of Medicaid Expansion On Postpartum Coverage And Outpatient Utilization,” Health Affairs 39, no. 1 (January 2020): 77-84, https://doi.org/10.1377/hlthaff.2019.00547 ↩︎
- Helmneh M. Sineshaw et al., “Association of Medicaid Expansion Under the Affordable Care Act With Stage at Diagnosis and Time to Treatment Initiation for Patients With Head and Neck Squamous Cell Carcinoma,” JAMA Otolaryngology–Head & Neck Surgery Epub ahead of print (January 2020), https://doi.org/10.1001/jamaoto.2019.4310 ↩︎
- Scott R. Sanders et al., “Infants Without Health Insurance: Racial/Ethnic and Rural/Urban Disparities in Infant Households’ Insurance Coverage,” PLoS One 15, no. 1 (January 2020), https://doi.org/10.1371/journal.pone.0222387 ↩︎
- John J. Park et al., “Medicaid and Private Insurance Coverage for Low-Income Asian Americans, Native Hawaiians, and Pacific Islanders, 2010-16,” Health Affairs 38, no. 11 (November 2019): 1911-1917, https://doi.org/10.1377/hlthaff.2019.00316 ↩︎
- Kevin N. Griffith, “Changes in Insurance Coverage and Access to Care for Young Adults in 2017,” Journal of Adolescent Health Epub ahead of print (July 2019), https://doi.org/10.1016/j.jadohealth.2019.05.020 ↩︎
- Jessica Sharac, Rachel Gunsalus, Chi Tran, Peter Shin, and Sara Rosenbaum, How are Migrant Health Centers and their Patients Faring Under the Affordable Care Act? (Geiger Gibson/RCHN Community Health Foundation Research Collaborative, The George Washington University Milken Institute of Public Health, May 2016), http://www.rchnfoundation.org/wp-content/uploads/2016/05/Migrant-Health-Centers-Patients-Under-Affordable-Care-Act.pdf ↩︎
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553 ↩︎
- Kelsey L. Corrigan et al., “The Impact of the Patient Protection and Affordable Care Act on Insurance Coverage and Cancer-Directed Treatment in HIV-Infected Patients With Cancer in the United States,” Cancer (November 2019), https://doi.org/10.1002/cncr.32563 ↩︎
- Jin Huang and Shirley L. Porterfield, “Changes in Health Insurance Coverage and Health Care Access as Teens with Disabilities Transition to Adulthood,” Disability and Health Journal 12, no. 4 (October 2019): 551-556, https://doi.org/10.1016/j.dhjo.2019.06.009 ↩︎
- Jim P. Stimpson et al., “Association of Medicaid Expansion With Health Insurance Coverage Among Persons With a Disability,” JAMA Network Open 2, no. 7 (July 2019), https://doi.org/10.1001/jamanetworkopen.2019.7136 ↩︎
- Huabin Luo, Zhuo Chen, Lei Xu, and Ronny Bell, “Health Care Access and Receipt of Clinical Diabetes Preventive Care for Working-Age Adults With Diabetes in States With and Without Medicaid Expansion: Results from the 2013 and 2015 BRFSS,” Journal of Public Health Management and Practice 25, no. 4 (July/August 2019): 34-43, https://doi.org/10.1097/phh.0000000000000832 ↩︎
- Sarah Miller, Sean Altekruse, Norman Johnson, and Laura R. Wherry, Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data (National Bureau of Economic Research, Working Paper No. 26081, July 2019), http://www.nber.org/papers/w26081 ↩︎
- Sameed Ahmed Khatana et al., “Association of Medicaid Expansion With Cardiovascular Mortality,” JAMA Cardiology 4, no. 7 (July 2019): 671-679, https://doi.org/10.1001/jamacardio.2019.1651 ↩︎
- Mark Olfson, Melanie Wall, Colleen Barry, Christine Mauro, and Ramin Mojtabai, “Impact Of Medicaid Expansion On Coverage And Treatment Of Low-Income Adults With Substance Use Disorders,” Health Affairs 37 no. 8 (August 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.0124 ↩︎
- Carrie Fry and Benjamin Sommers, “Effect of Medicaid Expansion on Health Insurance Coverage and Access to Care Among Adults With Depression,” Psychiatric Services 69, no. 11 (November 2018), https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201800181 ↩︎
- Jim Stimpson and Fernando Wilson, “Medicaid Expansion Improved Health Insurance Coverage For Immigrants, But Disparities Persist,” Health Affairs 37, no. 10 (October 2018), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.0181 ↩︎
- Amy Davidoff et al., “Changes in Health Insurance Coverage Associated With the Affordable Care Act Among Adults With and Without a Cancer History: Population-based National Estimates,” Medical Care 56, no. 3 (March 2018), https://journals.lww.com/lww-medicalcare/Abstract/2018/03000/Changes_in_Health_Insurance_Coverage_Associated.5.aspx ↩︎
- Xuesong Han et al., “Changes in Noninsurance and Care Unaffordability Among Cancer Survivors Following the Affordable Care Act,” Journal of the National Cancer Institute Epub ahead of print (November 2019), https://doi.org/10.1093/jnci/djz218 ↩︎
- Xuesong Han, Robin Yabroff, Elizabeth Ward, Otis Brawley, and Ahmedin Jemal, “Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act,” JAMA Oncology 4, no. 12 (August 2018): 1713-1720, https://jamanetwork.com/journals/jamaoncology/article-abstract/2697226 ↩︎
- Michael Cohen and William Schpero, “Household Immigration Status Had Differential Impact On Medicaid Enrollment In Expansion And Nonexpansion States,” Health Affairs 37, no. 3 (March 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.0978 ↩︎
- Tyler Winkelman, Edith Kieffer, Susan Goold, Jeffrey Morenoff, Kristen Cross, and John Ayanian, “Health Insurance Trends and Access to Behavioral Health Care Among Justice-Involved Individuals,” Journal of General Internal Medicine 31, no. 12 (December 2016): 1523-1529, https://www.ncbi.nlm.nih.gov/pubmed/27638837 ↩︎
- Vikki Wachino and Samantha Artiga, How Connecting Justice-Involved Individuals to Medicaid Can Help Address the Opioid Epidemic (Washington, DC: Kaiser Family Foundation, June 2019), https://modern.kff.org/medicaid/issue-brief/how-connecting-justice-involved-individuals-to-medicaid-can-help-address-the-opioid-epidemic/ ↩︎
- Brendan Saloner, Sachini Bandara, Emma McGinty, and Colleen Barry, “Justice-Involved Adults With Substance Use Disorders: Coverage Increased but Rates of Treatment Did Not in 2014,” Health Affairs 35 no. 6 (June 2016), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2016.0005 ↩︎
- Ankit Agarwal, Aaron Katz, and Ronald Chen, “The Impact of the Affordable Care Act on Disparities in Private and Medicaid Insurance Coverage among Patients Under 65 with Newly Diagnosed Cancer,” International Journal of Radiation Oncology, Biology, Physics (May 2019), https://www.redjournal.org/article/S0360-3016(19)30783-7/pdf ↩︎
- Ameen Barghi, Hugo Torres, Nancy Kressin, and Danny McCormick, “Coverage and Access for Americans with Cardiovascular Disease or Risk Factors After the ACA: a Quasi-experimental Study,” Journal of General Internal Medicine epub ahead of print (June 2019), https://link.springer.com/article/10.1007%2Fs11606-019-05108-1 ↩︎
- Emily Brown, Michelle Garrison, Hao Bao, Pingping Qu, Carole Jenny, and Ali Rowhani-Rahbar, “Assessment of Rates of Child Maltreatment in States With Medicaid Expansion vs States Without Medicaid Expansion,” JAMA Network Open 2, no. 6 (June 2019), https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2735758 ↩︎
- Brandy Lipton, Sandra Decker, and Benjamin Sommers, “The Affordable Care Act Appears to Have Narrowed Racial and Ethnic Disparities in Insurance Coverage and Access to Care Among Young Adults” Medical Care Research and Review 76, no.1 (April 2017): 32–55, https://www.ncbi.nlm.nih.gov/pubmed/29148341 ↩︎
- Jose Mesquita-Neto, Peter Cmorej, Hassan Mouzaihem, Donald Weaver, Steve Kim, and Francis Macedo, “Disparities In Access To Cancer Surgery After Medicaid Expansion,” The American Journal of Surgery epub ahead of print (June 2019), https://www.sciencedirect.com/science/article/abs/pii/S0002961019306889 ↩︎
- Lindsey Dawson, Jennifer Kates, and Anthony Damico, The Affordable Care Act and Insurance Coverage Changes by Sexual Orientation (Washington, DC: Kaiser Family Foundation, January 2018), https://modern.kff.org/disparities-policy/issue-brief/the-affordable-care-act-and-insurance-coverage-changes-by-sexual-orientation/ ↩︎
- Aparna Soni, Lindsay Sabik, Kosali Simon, and Benjamin Sommers, “Changes in Insurance Coverage Among Cancer Patients Under the Affordable Care Act,” Journal of the American Medical Association 4, no. 1 (January 2018): 122-124, https://jamanetwork.com/journals/jamaoncology/article-abstract/2657670?redirect=true&redirect=true ↩︎
- Fumiko Chino, Gita Suneja, Haley Moss, S. Yousuf Zafar, Laura Havrilesky, and Junzo Chino, “Healthcare Disparities in Cancer Patients Receiving Radiation: Changes in Insurance Status After Medicaid Expansion Under the Affordable Care Act,” International Journal of Radiation Oncology (December 2017), http://www.sciencedirect.com/science/article/pii/S0360301617341883 ↩︎
- Claire E. Margerison et al., “Impacts of Medicaid Expansion on Health Among Women of Reproductive Age,” American Journal of Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.amepre.2019.08.019 ↩︎
- Emily Johnston, Andrea Strahan, Peter Joski, Anne Dunlop, and E. Kathleen Adams, “Impacts of the Affordable Care Act’s Medicaid Expansion on Women of Reproductive Age,” Women’s Health Issues, 28, no. 2 (February 2018), http://www.whijournal.com/article/S1049-3867(17)30242-6/pdf ↩︎
- Ahmedin Jemal, Chun Chieh Lin, Amy Davidoff, and Xuesong Han, “Changes in Insurance Coverage and Stage at Diagnosis Among Nonelderly Patients with Cancer after the Affordable Care Act,” Journal of Clinical Oncology 35, no. 35 (December 2017), http://ascopubs.org/doi/pdf/10.1200/JCO.2017.73.7817 ↩︎
- Haley Moss, Laura Havrilesky, and Junzo Chino, “Insurance Coverage Among Women Diagnosed with a Gynecologic Malignancy Before and After Implementation of the Affordable Care Act,” Gynecologic Oncology 146, no. 3 (September 2017), https://www.ncbi.nlm.nih.gov/pubmed/28641821 ↩︎
- Barbara DiPietro, Samantha Artiga, and Alexandra Gates, Early Impacts of the Medicaid Expansion for the Homeless Population (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, November 2014), http://kff.org/uninsured/issue-brief/early-impacts-of-the-medicaid-expansion-for-the-homeless-population/ ↩︎
- Matt Warfield, Barbara DiPietro, and Samantha Artiga, How has the ACA Medicaid Expansion Affected Providers Serving the Homeless Population: Analysis of Coverage, Revenues, and Costs (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, March 2016), http://files.kff.org/attachment/issue-brief-how-has-the-aca-medicaid-expansion-affected-providers-serving-the-homeless-population ↩︎
- Samantha Artiga, Barbara DiPietro, and Petry Ubri, The Role of Medicaid and the Impact of the Medicaid Expansion for Veterans Experiencing Homelessness, (Washington, DC: Kaiser Family Foundation, October 2017), https://modern.kff.org/medicaid/issue-brief/the-role-of-medicaid-and-impact-of-the-medicaid-expansion-for-veterans-experiencing-homelessness/ ↩︎
- A. Taylor Kelley, Renuka Tipirneni, and Helen Levy, “Changes in Veterans’ Coverage and Access to Care Following the Affordable Care Act, 2011-2017,” American Journal of Public Health 109, no. 9 (September 2019): 1233-1235, https://doi.org/10.2105/ajph.2019.305160 ↩︎
- Michael Dworsky, Carrie Farmer, and Mimi Shen, Veterans’ Health Insurance Coverage Under the Affordable Care Act and Implications of Repeal for the Department of Veterans Affairs, (RAND Corporation, 2017), https://www.rand.org/pubs/research_reports/RR1955.html ↩︎
- Jennifer Haley, Robin Wang, Matthew Buettgens, and Genevieve Kenney, Health Insurance Coverage among Children Ages 3 and Younger and Their Parents in 2016 (The Urban Institute, January 2018), https://www.urban.org/research/publication/health-insurance-coverage-among-children-ages-3-and-younger-and-their-parents-2016 ↩︎
- Kevin Griffith, Leigh Evans, and Jacob Bor, “The Affordable Care Act Reduced Socioeconomic Disparities in Health Care Access,” Health Affairs 36 no. 8 (August 2017), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0083 ↩︎
- Julie Hudson and Asako Moriya, “Medicaid Expansion for Adults Had Measureable ‘Welcome Mat’ Effects on Their Children,” Health Affairs, 36 no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0347 ↩︎
- Stephen Berry et al., “Healthcare Coverage for HIV Provider Visits before and after Implementation of the Affordable Care Act,” Clinical Infectious Diseases, (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27143660 ↩︎
- Jennifer Kates and Lindsey Dawson, Insurance Coverage Changes for People with HIV Under the ACA (Washington, DC: Kaiser Family Foundation, February 2017), http://kff.org/health-reform/issue-brief/insurance-coverage-changes-for-people-with-hiv-under-the-aca/ ↩︎
- Jennifer Haley, Genevieve Kenney, and Jason Gates, Veterans Saw Broad Coverage Gains Between 2013 and 2015 (Washington, DC: The Urban Institute, April 2017), http://www.urban.org/research/publication/veterans-saw-broad-coverage-gains-between-2013-and-2015 ↩︎
- Stacey McMorrow, Jason Gates, Sharon Long, and Genevieve Kenney, “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents,” Health Affairs 36 no. 5 (May 2017): 808-818, https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650 ↩︎
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Jason Gates, The ACA Medicaid Expansion Led to Widespread Reductions in Uninsurance Among Poor Childless Adults (The Urban Institute, April 2017), http://www.urban.org/sites/default/files/publication/89536/2001222-aca_medicaid_expansion_led_to_widespread_reductions_in_uninsurance_among_poor_childless_adults.pdf ↩︎
- George Wehby and Wei Lyu, “The Impact of the ACA Medicaid Expansions on Health Insurance Coverage through 2015 and Coverage Disparities by Age, Race/Ethnicity, and Gender” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12711/abstract ↩︎
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Nathaniel Anderson, “Uninsurance Among Young Adults Continues to Decline, Particularly in Medicaid Expansion States,” Health Affairs 34, no. 4 (April 2015): 616-620, http://content.healthaffairs.org/content/34/4/616.full ↩︎
- Andrew W. Mulcahy, Christine Eibner, and Kenneth Finegold, “Gaining Coverage Through Medicaid Or Private Insurance Increased Prescription Use and Lowered Out-Of-Pocket Spending,” Health Affairs 35, no. 9 (September 2016), http://content.healthaffairs.org/content/early/2016/08/16/hlthaff.2016.0091.full ↩︎
- Michael Karpman, Jason Gates, Genevieve Kenney, Stacey McMorrow, How Are Moms Faring under the Affordable Care Act? Evidence Through 2014, (The Urban Institute, May 2016), http://www.urban.org/research/publication/how-are-moms-faring-under-affordable-care-act-evidence-through-2014 ↩︎
- Genevieve Kenney, Jennifer Haley, Clare Pan, Victoria Lynch, and Matthew Buettgens, Children’s Coverage Climb Continues: Uninsurance and Medicaid/CHIP Eligibility and Participation Under the ACA, (Washington, DC: The Urban Institute, May 2016), http://www.urban.org/research/publication/childrens-coverage-climb-continues-uninsurance-and-medicaidchip-eligibility-and-participation-under-aca ↩︎
- Alanna Williamson, Larisa Antonisse, Jennifer Tolbert, Rachel Garfield, and Anthony Damico, ACA Coverage Expansions and Low-Income Workers (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2016), http://kff.org/report-section/aca-coverage-expansions-and-low-income-workers-issue-brief/ ↩︎
- Helen Levy, Thomas Buchmueller, and Sayeh Nikpay, Health Reform and Health Insurance Coverage of Early Retirees (Ann Arbor, MI: University of Michigan Retirement Research Center Working Paper, September 2016), http://www.mrrc.isr.umich.edu/publications/papers/pdf/wp345.pdf ↩︎
- Robert Kaestner, Bowen Garrett, Anuj Gangopadhyaya, and Caitlyn Fleming, Effects of ACA Medicaid Expansions on Health Insurance Coverage and Labor Supply (Working Paper No. 21836, National Bureau of Economic Research, December 2015), http://www.nber.org/papers/w21836 ↩︎
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, and Ishtiaque Fazlul, “The Three‐Year Impact of the Affordable Care Act on Disparities in Insurance Coverage,” Health Services Research (October 2018), https://onlinelibrary.wiley.com/doi/10.1111/1475-6773.13077 ↩︎
- Julia Foutz, Samantha Artiga, and Rachel Garfield, The Role of Medicaid in Rural America (Washington, DC: Kaiser Family Foundation, April 2017), http://kff.org/medicaid/issue-brief/the-role-of-medicaid-in-rural-america/ ↩︎
- Aparna Soni, Michael Hendryx, and Kosali Simon, “Medicaid Expansion under the Affordable Care Act and Insurance Coverage in Rural and Urban Areas,” The Journal of Rural Health epub ahead of print (January 2017), http://onlinelibrary.wiley.com/doi/10.1111/jrh.12234/full ↩︎
- Ankit Agarwal, Aaron Katz, and Ronald Chen, “The Impact of the Affordable Care Act on Disparities in Private and Medicaid Insurance Coverage among Patients Under 65 with Newly Diagnosed Cancer,” International Journal of Radiation Oncology, Biology, Physics (May 2019), https://www.redjournal.org/article/S0360-3016(19)30783-7/pdf ↩︎
- Charles J. Courtemanche et al., The Impact of the ACA on Insurance Coverage Disparities After Four Years (National Bureau of Economic Research, Working Paper No. 26157, August 2019), http://www.nber.org/papers/w26157 ↩︎
- Amandeep R. Mahal et al., “Early Impact of the Affordable Care Act and Medicaid Expansion on Racial and Socioeconomic Disparities in Cancer Care,” American Journal of Clinical Oncology Epub ahead of print (January 2020), https://doi.org/10.1097/coc.0000000000000588 ↩︎
- Jesse C. Baumgartner, Sara R. Collins, David C. Radley, and Susan L. Hayes, How the Affordable Care Act Has Narrowed Racial and Ethnic Disparities in Access to Health Care (The Commonwealth Fund, January 2020), https://www.commonwealthfund.org/publications/2020/jan/how-ACA-narrowed-racial-ethnic-disparities-access ↩︎
- Anna L. Goldman and Benjamin D. Sommers, “Among Low-Income Adults Enrolled In Medicaid, Churning Decreased After The Affordable Care Act,” Health Affairs 39, no. 1 (January 2020): 85-93, https://doi.org/10.1377/hlthaff.2019.00378 ↩︎
- Scott R. Sanders et al., “Infants Without Health Insurance: Racial/Ethnic and Rural/Urban Disparities in Infant Households’ Insurance Coverage,” PLoS One 15, no. 1 (January 2020), https://doi.org/10.1371/journal.pone.0222387 ↩︎
- Xuesong Han et al., “Changes in Noninsurance and Care Unaffordability Among Cancer Survivors Following the Affordable Care Act,” Journal of the National Cancer Institute Epub ahead of print (November 2019), https://doi.org/10.1093/jnci/djz218 ↩︎
- Jim P. Stimpson et al., “Association of Medicaid Expansion With Health Insurance Coverage Among Persons With a Disability,” JAMA Network Open 2, no. 7 (July 2019), https://doi.org/10.1001/jamanetworkopen.2019.7136 ↩︎
- Sandra Decker, Brandy Lipton, and Benjamin Sommers, “Medicaid Expansion Coverage Effects Grew in 2015 With Continued Improvements in Coverage Quality,” Health Affairs 36 no. 5 (May 2017): 819-825, http://content.healthaffairs.org/content/36/5/819.full ↩︎
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562 ↩︎
- Hyunjung Lee and Frank Porell, “The Effect of the Affordable Care Act Medicaid Expansion on Disparities in Access to Care and Health Status,” Medical Care Research and Review epub ahead of print (October 2018), https://journals.sagepub.com/doi/abs/10.1177/1077558718808709?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=mcrd ↩︎
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, and Ishtiaque Fazlul, “The Three‐Year Impact of the Affordable Care Act on Disparities in Insurance Coverage,” Health Services Research (October 2018), https://onlinelibrary.wiley.com/doi/10.1111/1475-6773.13077 ↩︎
- Xuesong Han, Robin Yabroff, Elizabeth Ward, Otis Brawley, and Ahmedin Jemal, “Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act,” JAMA Oncology 4, no. 12 (August 2018): 1713-1720, https://jamanetwork.com/journals/jamaoncology/article-abstract/2697226 ↩︎
- Fumiko Chino, Gita Suneja, Haley Moss, S. Yousuf Zafar, Laura Havrilesky, and Junzo Chino, “Healthcare Disparities in Cancer Patients Receiving Radiation: Changes in Insurance Status After Medicaid Expansion Under the Affordable Care Act,” International Journal of Radiation Oncology (December 2017), http://www.sciencedirect.com/science/article/pii/S0360301617341883 ↩︎
- Susan Hayes, Pamela Riley, David Radley, and Douglas McCarthy, Reducing Racial and Ethnic Disparities in Access to Care: Has the Affordable Care Act Made a Difference? (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/racial-ethnic-disparities-care ↩︎
- Kelsey Avery, Kenneth Finegold, and Amelia Whitman, Affordable Care Act Has Led to Historic, Widespread Increase in Health Insurance Coverage (Office of the Assistant Secretary for Planning and Evaluation, September 2016), https://aspe.hhs.gov/sites/default/files/pdf/207946/ACAHistoricIncreaseCoverage.pdf ↩︎
- George Wehby and Wei Lyu, “The Impact of the ACA Medicaid Expansions on Health Insurance Coverage through 2015 and Coverage Disparities by Age, Race/Ethnicity, and Gender” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12711/abstract ↩︎
- Dahai Yue, Petra Rasmussen, and Ninez Ponce, “Racial/Ethnic Differential Effects of Medicaid Expansion on Health Care Access,” Health Services Research (February 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12834/abstract ↩︎
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, and Daniela Zapata, Impacts of the Affordable Care Act on Health Insurance Coverage in Medicaid Expansion and Non-Expansion States (Working Paper No. 22182, The National Bureau of Economic Research, April 2016), http://www.nber.org/papers/w22182 ↩︎
- Thomas Buchmueller, Zachary Levinson, Helen Levy, and Barbara Wolfe, “Effect of the Affordable Care Act on Racial and Ethnic Disparities in Health Insurance Coverage,” American Journal of Public Health (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27196653 ↩︎
- Sergio Gonzales and Benjamin Sommers, “Intra-Ethnic Coverage Disparities among Latinos and the Effects of Health Reform” Health Services Research epub ahead of print (June 2017), http://onlinelibrary.wiley.com/wol1/doi/10.1111/1475-6773.12733/full ↩︎
- Ankit Agarwal, Aaron Katz, and Ronald Chen, “The Impact of the Affordable Care Act on Disparities in Private and Medicaid Insurance Coverage among Patients Under 65 with Newly Diagnosed Cancer,” International Journal of Radiation Oncology, Biology, Physics (May 2019), https://www.redjournal.org/article/S0360-3016(19)30783-7/pdf ↩︎
- John Heintzman, Steffani Bailey, Jennifer DeVoe, Stuart Cowburn, Tanya Kapka, Truc-Vi Duong, and Miguel Marino, “In Low-Income Latino Patients, Post-Affordable Care Act Insurance Disparities May Be Reduced Even More than Broader National Estimates: Evidence from Oregon,” Journal of Racial and Ethnic Health Disparities (April 2016), http://www.ncbi.nlm.nih.gov/pubmed/27105630 ↩︎
- Kevin Griffith, Leigh Evans, and Jacob Bor, “The Affordable Care Act Reduced Socioeconomic Disparities in Health Care Access,” Health Affairs 36 no. 8 (August 2017), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0083 ↩︎
- Michael Dworsky and Christine Eibner, The Effect of the 2014 Medicaid Expansion on Insurance Coverage for Newly Eligible Childless Adults (Santa Monica, CA: Rand Corporation, 2016), https://www.rand.org/pubs/research_reports/RR1736.html ↩︎
- Brandy Lipton, Sandra Decker, and Benjamin Sommers, “The Affordable Care Act Appears to Have Narrowed Racial and Ethnic Disparities in Insurance Coverage and Access to Care Among Young Adults” Medical Care Research and Review 76, no.1 (April 2017): 32–55, https://www.ncbi.nlm.nih.gov/pubmed/29148341 ↩︎
- Aparna Soni, Michael Hendryx, and Kosali Simon, “Medicaid Expansion under the Affordable Care Act and Insurance Coverage in Rural and Urban Areas,” The Journal of Rural Health epub ahead of print (January 2017), http://onlinelibrary.wiley.com/doi/10.1111/jrh.12234/full ↩︎
- Scott R. Sanders et al., “Infants Without Health Insurance: Racial/Ethnic and Rural/Urban Disparities in Infant Households’ Insurance Coverage,” PLoS One 15, no. 1 (January 2020), https://doi.org/10.1371/journal.pone.0222387 ↩︎
- Jin Huang and Shirley L. Porterfield, “Changes in Health Insurance Coverage and Health Care Access as Teens with Disabilities Transition to Adulthood,” Disability and Health Journal 12, no. 4 (October 2019): 551-556, https://doi.org/10.1016/j.dhjo.2019.06.009 ↩︎
- Claire E. Margerison et al., “Impacts of Medicaid Expansion on Health Among Women of Reproductive Age,” American Journal of Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.amepre.2019.08.019 ↩︎
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553 ↩︎
- Kevin N. Griffith, “Changes in Insurance Coverage and Access to Care for Young Adults in 2017,” Journal of Adolescent Health Epub ahead of print (July 2019), https://doi.org/10.1016/j.jadohealth.2019.05.020 ↩︎
- Helen Levy, Thomas Buchmueller, and Sayeh Nikpay, “The Impact of Medicaid Expansion on Household Consumption,” Eastern Economic Journal 45, no. 1 (January 2019): 34-57, https://link.springer.com/article/10.1057/s41302-018-0124-7 ↩︎
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830 ↩︎
- Abigail Barker, Kelsey Huntzberry, Timothy McBride, and Keith Mueller, Changing Rural and Urban Enrollment in State Medicaid Programs (Iowa City, IA: Rural Policy Research Institute, May 2017), https://cph.uiowa.edu/rupri/publications/policybriefs/2017/Changing%20Rural%20and%20Urban%20Enrollment%20in%20State%20Medicaid%20Programs.pdf ↩︎
- Hyunjung Lee and Frank Porell, “The Effect of the Affordable Care Act Medicaid Expansion on Disparities in Access to Care and Health Status,” Medical Care Research and Review epub ahead of print (October 2018), https://journals.sagepub.com/doi/abs/10.1177/1077558718808709?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=mcrd ↩︎
- George Wehby and Wei Lyu, “The Impact of the ACA Medicaid Expansions on Health Insurance Coverage through 2015 and Coverage Disparities by Age, Race/Ethnicity, and Gender” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12711/abstract ↩︎
- Rene Flores and Robert Vargas, “Medicaid Expansion And Ethnoracial Disparities In Health Insurance Coverage,” Journal of Ethnic and Migration Studies 43, no. 12 (June 2017), https://www.tandfonline.com/doi/full/10.1080/1369183X.2017.1323451?needAccess=true ↩︎
- Charles J. Courtemanche et al., The Impact of the ACA on Insurance Coverage Disparities After Four Years (National Bureau of Economic Research, Working Paper No. 26157, August 2019), http://www.nber.org/papers/w26157 ↩︎
- Nevada’s Medicaid Population, (Las Vegas, NV: The Guinn Center, September 2019), https://guinncenter.org/wp-content/uploads/2019/09/Guinn-Center-NV-Medicaid-Population-Characteristics-2019.pdf ↩︎
- Sumit D. Agarwal, Anna L. Goldman, and Benjamin D. Sommers, “Blue-Collar Workers Had Greatest Insurance Gains After ACA Implementation,” Health Affairs 38, no. 7 (July 2019): 1140-1144, https://doi.org/10.1377/hlthaff.2018.05454 ↩︎
- Kelsey L. Corrigan et al., “The Impact of the Patient Protection and Affordable Care Act on Insurance Coverage and Cancer-Directed Treatment in HIV-Infected Patients With Cancer in the United States,” Cancer (November 2019), https://doi.org/10.1002/cncr.32563 ↩︎
- John J. Park et al., “Medicaid and Private Insurance Coverage for Low-Income Asian Americans, Native Hawaiians, and Pacific Islanders, 2010-16,” Health Affairs 38, no. 11 (November 2019): 1911-1917, https://doi.org/10.1377/hlthaff.2019.00316 ↩︎
- Jim P. Stimpson, Jessie Kemmick Pintor, and Fernando A. Wilson, “Association of Medicaid Expansion with Health Insurance Coverage by Marital Status and Sex,” PLoS One 14, no. 10 (October 2019), https://doi.org/10.1371/journal.pone.0223556 ↩︎
- Xuesong Han et al., “Changes in Noninsurance and Care Unaffordability Among Cancer Survivors Following the Affordable Care Act,” Journal of the National Cancer Institute Epub ahead of print (November 2019), https://doi.org/10.1093/jnci/djz218 ↩︎
- Michael Dworsky and Christine Eibner, The Effect of the 2014 Medicaid Expansion on Insurance Coverage for Newly Eligible Childless Adults (Santa Monica, CA: Rand Corporation, 2016), https://www.rand.org/pubs/research_reports/RR1736.html ↩︎
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, and Ishtiaque Fazlul, “The Three‐Year Impact of the Affordable Care Act on Disparities in Insurance Coverage,” Health Services Research (October 2018), https://onlinelibrary.wiley.com/doi/10.1111/1475-6773.13077 ↩︎
- Dahai Yue, Petra Rasmussen, and Ninez Ponce, “Racial/Ethnic Differential Effects of Medicaid Expansion on Health Care Access,” Health Services Research (February 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12834/abstract ↩︎
- Benjamin Sommers, Rebecca Gourevitch, Bethany Maylone, Robert Blendon, and Arnold Epstein, “Insurance Churning Rates for Low-Income Adults Under Health Reform: Lower Than Expected but Still Harmful for Many,” Health Affairs 35 no. 10 (October 2016): 1816-1824, http://content.healthaffairs.org/content/35/10/1816.full?sid=f4835910-ffd0-4864-a76a-b4f207ccd018 ↩︎
- Sergio Gonzales and Benjamin Sommers, “Intra-Ethnic Coverage Disparities among Latinos and the Effects of Health Reform” Health Services Research epub ahead of print (June 2017), http://onlinelibrary.wiley.com/wol1/doi/10.1111/1475-6773.12733/full ↩︎
- Mark Olfson et al., “A National Survey of Trends in Health Insurance Coverage of Low-Income Adults Following Medicaid Expansion,” Journal of General Internal Medicine Epub ahead of print (October 2019), https://doi.org/10.1007/s11606-019-05409-5 ↩︎
- John J. Park et al., “Medicaid and Private Insurance Coverage for Low-Income Asian Americans, Native Hawaiians, and Pacific Islanders, 2010-16,” Health Affairs 38, no. 11 (November 2019): 1911-1917, https://doi.org/10.1377/hlthaff.2019.00316 ↩︎
- Jin Huang and Shirley L. Porterfield, “Changes in Health Insurance Coverage and Health Care Access as Teens with Disabilities Transition to Adulthood,” Disability and Health Journal 12, no. 4 (October 2019): 551-556, https://doi.org/10.1016/j.dhjo.2019.06.009 ↩︎
- Laura Skopec, John Holahan, and Caroline Elmendorf, Health Insurance Coverage Declined for Nonelderly Americans Between 2016 and 2017, Primarily in States That Did Not Expand Medicaid (Washington, DC: The Urban Institute, August 2019), https://www.urban.org/research/publication/health-insurance-coverage-declined-nonelderly-americans-between-2016-and-2017-primarily-states-did-not-expand-medicaid ↩︎
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553 ↩︎
- Stephen Berry et al., “Healthcare Coverage for HIV Provider Visits before and after Implementation of the Affordable Care Act,” Clinical Infectious Diseases, (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27143660 ↩︎
- Helen Levy, Thomas Buchmueller, and Sayeh Nikpay, “The Impact of Medicaid Expansion on Household Consumption,” Eastern Economic Journal 45, no. 1 (January 2019): 34-57, https://link.springer.com/article/10.1057/s41302-018-0124-7 ↩︎
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830 ↩︎
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562 ↩︎
- Jean M. Abraham, Anne B. Royalty, and Coleman Drake, “The Impact of Medicaid Expansion on Employer Provision of Health Insurance,” International Journal of Health Economics and Management 19, no. 3-4 (December 2019): 317-340, https://doi.org/10.1007/s10754-018-9256-x ↩︎
- Kelsey L. Corrigan et al., “The Impact of the Patient Protection and Affordable Care Act on Insurance Coverage and Cancer-Directed Treatment in HIV-Infected Patients With Cancer in the United States,” Cancer (November 2019), https://doi.org/10.1002/cncr.32563 ↩︎
- Adele Shartzer, Frederic Blavin, and John Holohan, “Employer-Sponsored Insurance Stable For Low-Income Workers In Medicaid Expansion States,” Health Affairs 37, no. 4 (April 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1205 ↩︎
- Molly Frean, Jonathan Gruber, and Benjamin Sommers, Premium Subsidies, the Mandate, and Medicaid Expansion: Coverage Effects of the Affordable Care Act (Working Paper No. 22213, National Bureau of Economic Research, April 2016), http://www.nber.org/papers/w22213?utm_campaign=ntw&utm_medium=email&utm_source=ntw ↩︎
- Sarah Miller and Laura Wherry, “Four Years Later: Insurance Coverage and Access to Care Continue to Diverge between ACA Medicaid Expansion and Non-Expansion States,” American Economic Association Papers and Proceedings 109 (May 2019): 327-333, https://www.aeaweb.org/articles?id=10.1257/pandp.20191046 ↩︎
- Michael Dworsky and Christine Eibner, The Effect of the 2014 Medicaid Expansion on Insurance Coverage for Newly Eligible Childless Adults (Santa Monica, CA: Rand Corporation, 2016), https://www.rand.org/pubs/research_reports/RR1736.html ↩︎
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Nathaniel Anderson, “Uninsurance Among Young Adults Continues to Decline, Particularly in Medicaid Expansion States,” Health Affairs 34, no. 4 (April 2015): 616-620, http://content.healthaffairs.org/content/34/4/616.full ↩︎
- Sandra Decker, Brandy Lipton, and Benjamin Sommers, “Medicaid Expansion Coverage Effects Grew in 2015 With Continued Improvements in Coverage Quality,” Health Affairs 36 no. 5 (May 2017): 819-825, http://content.healthaffairs.org/content/36/5/819.full ↩︎
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890 ↩︎
- Pauline Leung and Alexandre Mas, Employment Effects of the ACA Medicaid Expansions (Working Paper No. 22540, National Bureau of Economic Research, August 2016), http://www.nber.org/papers/w22540 ↩︎
- George Wehby and Wei Lyu, “The Impact of the ACA Medicaid Expansions on Health Insurance Coverage through 2015 and Coverage Disparities by Age, Race/Ethnicity, and Gender” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12711/abstract ↩︎
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, and Daniela Zapata, Impacts of the Affordable Care Act on Health Insurance Coverage in Medicaid Expansion and Non-Expansion States (Working Paper No. 22182, The National Bureau of Economic Research, April 2016), http://www.nber.org/papers/w22182 ↩︎
- Seth Freedman, Lilliard Richardson, and Kosali Simon, “Learning From Waiver States: Coverage Effects Under Indiana’s HIP Medicaid Expansion,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1596 ↩︎
- Joanna Woronkowicz, Aparna Soni, Seth Freedman, and Kosali Simon, “How Have Recent Health Insurance Expansions Affected Coverage Among Artist Occupations In The USA?,” Journal of Cultural Economics (May 2019), https://link.springer.com/article/10.1007/s10824-019-09352-5 ↩︎
- Ankit Agarwal, Aaron Katz, and Ronald Chen, “The Impact of the Affordable Care Act on Disparities in Private and Medicaid Insurance Coverage among Patients Under 65 with Newly Diagnosed Cancer,” International Journal of Radiation Oncology, Biology, Physics (May 2019), https://www.redjournal.org/article/S0360-3016(19)30783-7/pdf ↩︎
- Aparna Soni, Michael Hendryx, and Kosali Simon, “Medicaid Expansion under the Affordable Care Act and Insurance Coverage in Rural and Urban Areas,” The Journal of Rural Health epub ahead of print (January 2017), http://onlinelibrary.wiley.com/doi/10.1111/jrh.12234/full ↩︎
- Benjamin Sommers, Robert Blendon, E. John Orav, and Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420 ↩︎
- Benjamin Sommers, Robert Blendon, and E. John Orav, “Both the ‘Private Option’ And Traditional Medicaid Expansions Improved Access To Care For Low-Income Adults,” Health Affairs 35, no. 1 (January 2016): 96-105, http://content.healthaffairs.org/content/35/1/96.abstract ↩︎
- Anna L. Goldman and Benjamin D. Sommers, “Among Low-Income Adults Enrolled In Medicaid, Churning Decreased After The Affordable Care Act,” Health Affairs 39, no. 1 (January 2020): 85-93, https://doi.org/10.1377/hlthaff.2019.00378 ↩︎
- Jocelyn Guyer, Naomi Shine, MaryBeth Musumeci, and Robin Rudowitz, A Look at the Private Option in Arkansas (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, August 2015), http://kff.org/medicaid/issue-brief/a-look-at-the-private-option-in-arkansas/ ↩︎
- Benjamin Sommers, Carrie Fry, Robert Blendon, and Arnold Epstein, “New Approaches in Medicaid: Work Requirements, Health Savings Accounts, and Health Care Access,” Health Affairs 37, no. 7 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2018.0331 ↩︎
- MaryBeth Musumeci, Robin Rudowitz, Petry Ubri, and Elizabeth Hinton, An Early Look at Medicaid Expansion Waiver Implementation in Michigan and Indiana (Washington, DC: The Kaiser Family Foundation, January 2017), http://kff.org/medicaid/issue-brief/an-early-look-at-medicaid-expansion-waiver-implementation-in-michigan-and-indiana/ ↩︎
- Benjamin Sommers, Anna Goldman, Robert Blendon, E. John Orav, and Arnold Epstein, “Medicaid Work Requirements – Results from the First Year in Arkansas,” The New England Journal of Medicine Special Report (June 2019), https://www.nejm.org/doi/full/10.1056/NEJMsr1901772 ↩︎
- Amandeep R. Mahal et al., “Early Impact of the Affordable Care Act and Medicaid Expansion on Racial and Socioeconomic Disparities in Cancer Care,” American Journal of Clinical Oncology Epub ahead of print (January 2020), https://doi.org/10.1097/coc.0000000000000588 ↩︎
- MaryBeth Musumeci, Robin Rudowitz, and Barbara Lyons, Medicaid Work Requirements in Arkansas: Experience and Perspectives of Enrollees (Washington, DC: Kaiser Family Foundation, December 2018), https://modern.kff.org/medicaid/issue-brief/medicaid-work-requirements-in-arkansas-experience-and-perspectives-of-enrollees/ ↩︎
- MaryBeth Musumeci, Robin Rudowitz, and Cornelia Hall, An Early Look at Implementation of Medicaid Work Requirements in Arkansas (Washington, DC: Kaiser Family Foundation, October 2018), https://modern.kff.org/medicaid/issue-brief/an-early-look-at-implementation-of-medicaid-work-requirements-in-arkansas/ ↩︎
- Robin Rudowitz, MaryBeth Musumeci, and Cornelia Hall, February State Data for Medicaid Work Requirements in Arkansas (Washington, DC: Kaiser Family Foundation, March 2019), https://modern.kff.org/medicaid/issue-brief/state-data-for-medicaid-work-requirements-in-arkansas/ ↩︎
- MaryBeth Musumeci, Disability and Technical Issues Were Key Barriers to Meeting Arkansas’ Medicaid Work and Reporting Requirements in 2018 (Washington, DC: Kaiser Family Foundation, June 2019), https://modern.kff.org/medicaid/issue-brief/disability-and-technical-issues-were-key-barriers-to-meeting-arkansas-medicaid-work-and-reporting-requirements-in-2018/ ↩︎
- The Lewin Group, Healthy Indiana Plan 2.0: POWER Account Contribution Assessment, (The Lewin Group, prepared for the Indiana Family and Social Services Administration, March 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-POWER-acct-cont-assesmnt-03312017.pdf ↩︎
- The Lewin Group, Indiana Healthy Indiana Plan 2.0: Interim Evaluation Report (The Lewin Group, Prepared for Indiana Family and Social Services Administration, July 2016), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-interim-evl-rpt-07062016.pdf ↩︎
- Emily Zylla, Colin Planalp, Elizabeth Lukanen, and Lynn Blewett, Section 1115 Medicaid Expansion Waivers: Implementation Experiences, (Medicaid and CHIP Payment and Access Commission, February 2018), https://www.macpac.gov/publication/section-1115-medicaid-expansion-waivers-implementation-experiences/ ↩︎
- MaryBeth Musumeci, Robin Rudowitz, Petry Ubri, and Elizabeth Hinton, An Early Look at Medicaid Expansion Waiver Implementation in Michigan and Indiana (Washington, DC: The Kaiser Family Foundation, January 2017), http://kff.org/medicaid/issue-brief/an-early-look-at-medicaid-expansion-waiver-implementation-in-michigan-and-indiana/ ↩︎
- Benjamin Sommers, Carrie Fry, Robert Blendon, and Arnold Epstein, “New Approaches in Medicaid: Work Requirements, Health Savings Accounts, and Health Care Access,” Health Affairs 37, no. 7 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2018.0331 ↩︎
- Jusung Lee et al., “The Impact of Medicaid Expansion on Diabetes Management,” Diabetes Care Epub ahead of print (October 2019), https://doi.org/10.2337/dc19-1173 ↩︎
- Emanuel Eguia et al., “The Impact of the Affordable Care Act Medicaid Expansion on Vascular Surgery,” Annals of Vascular Surgery Epub ahead of print (January 2020), https://doi.org/10.1016/j.avsg.2020.01.006 ↩︎
- Alexander T. Janke, Shooshan Danagoulian, Arjun K. Venkatesh, and Phillip D. Levy, “Medicaid Expansion and Resource Utilization in the Emergency Department,” The American Journal of Emergency Medicine Epub ahead of print (January 2020), https://doi.org/10.1016/j.ajem.2019.12.050 ↩︎
- Helmneh M. Sineshaw et al., “Association of Medicaid Expansion Under the Affordable Care Act With Stage at Diagnosis and Time to Treatment Initiation for Patients With Head and Neck Squamous Cell Carcinoma,” JAMA Otolaryngology–Head & Neck Surgery Epub ahead of print (January 2020), https://doi.org/10.1001/jamaoto.2019.4310 ↩︎
- Jesse C. Baumgartner, Sara R. Collins, David C. Radley, and Susan L. Hayes, How the Affordable Care Act Has Narrowed Racial and Ethnic Disparities in Access to Health Care (The Commonwealth Fund, January 2020), https://www.commonwealthfund.org/publications/2020/jan/how-ACA-narrowed-racial-ethnic-disparities-access ↩︎
- Anna L. Goldman and Benjamin D. Sommers, “Among Low-Income Adults Enrolled In Medicaid, Churning Decreased After The Affordable Care Act,” Health Affairs 39, no. 1 (January 2020): 85-93, https://doi.org/10.1377/hlthaff.2019.00378 ↩︎
- Sarah H. Gordon, Benjamin D. Sommers, Ira B. Wilson, and Amal N. Trivedi, “Effects Of Medicaid Expansion On Postpartum Coverage And Outpatient Utilization,” Health Affairs 39, no. 1 (January 2020): 77-84, https://doi.org/10.1377/hlthaff.2019.00547 ↩︎
- Emanuel Eguia et al., “The Impact of the Affordable Care Act (ACA) Medicaid Expansion on Access to Minimally Invasive Surgical Care,” The American Journal of Surgery Epub ahead of print (July 2019), https://doi.org/10.1016/j.amjsurg.2019.07.003 ↩︎
- Jin Huang and Shirley L. Porterfield, “Changes in Health Insurance Coverage and Health Care Access as Teens with Disabilities Transition to Adulthood,” Disability and Health Journal 12, no. 4 (October 2019): 551-556, https://doi.org/10.1016/j.dhjo.2019.06.009 ↩︎
- Nathalie Huguet et al., “Following Uninsured Patients Through Medicaid Expansion: Ambulatory Care Use and Diagnosed Conditions,” Annals of Family Medicine 17, no. 4 (July/August 2019): 336-344, https://doi.org/10.1370/afm.2385 ↩︎
- Lisa Clemans-Cope, Victoria Lynch, Marni Epstein, and Genevieve Kenney, Medicaid Coverage of Effective Treatment for Opioid Use Disorder, (Washington, DC: The Urban Institute, June 2017), https://www.urban.org/sites/default/files/publication/90461/2001287_medicaid_coverage_of_effective_treatment_for_opioid_use_disorder.pdf ↩︎
- Kelsie M. Gould et al., “Bariatric Surgery Among Vulnerable Populations: The Effect of the Affordable Care Act’s Medicaid Expansion,” Surgery 166, no. 5 (November 2019): 820-828, https://doi.org/10.1016/j.surg.2019.05.005 ↩︎
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553 ↩︎
- Samantha Artiga, Robin Rudowitz, Jennifer Tolbert, Julia Paradise, and Melissa Majerol, Findings from the Field: Medicaid Delivery Systems and Access to Care in Four States in Year Three of the ACA (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, September 2016), http://kff.org/medicaid/issue-brief/findings-from-the-field-medicaid-delivery-systems-and-access-to-care-in-four-states-in-year-three-of-the-aca/ ↩︎
- Michael McCue, “The Impact of Medicaid Expansion on Medicaid Focused Insurers in California,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 52 (July 2015), http://inq.sagepub.com/content/52/0046958015595960.full.pdf+html ↩︎
- Afshin Ehsan et al., “Utilization of Left Ventricular Assist Devices in Vulnerable Adults Across Medicaid Expansion,” Journal of Surgical Research 243 (November 2019): 503-508, https://doi.org/10.1016/j.jss.2019.05.015 ↩︎
- Susannah Gibbs et al., “Evaluating the Effect of Medicaid Expansion on Access to Preventive Reproductive Care for Women in Oregon,” Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.ypmed.2019.105899 ↩︎
- Hefei Wen, Tyrone Borders, and Benjamin Druss, ”Number of Medicaid Prescriptions Grew, Drug Spending was Steady in Medicaid Expansion States,” Health Affairs 35, no. 12 (September 2016): 1604-1607, http://content.healthaffairs.org/content/35/9/1604.full ↩︎
- Jane Wishner, Patricia Solleveld, Robin Rudowitz, Julia Paradise, and Larisa Antonisse, A Look at Rural Hospital Closures and Implications for Access to Care: Three Case Studies (Washington, DC: Kaiser Commission on Medicaid and the Uninsured and The Urban Institute, July 2016), http://kff.org/medicaid/issue-brief/a-look-at-rural-hospital-closures-and-implications-for-access-to-care/ ↩︎
- Mark Duggan, Atul Gupta, and Emilie Jackson, The Impact of the Affordable Care Act: Evidence from California’s Hospital Sector (National Bureau of Economic Research, working paper no. 25488, January 2019), https://www.nber.org/papers/w25488.pdf ↩︎
- Nathalie Huguet et al., “Cervical And Colorectal Cancer Screening Prevalence Before And After Affordable Care Act Medicaid Expansion,” Preventative Medicine (May 2019), https://doi.org/10.1016/j.ypmed.2019.05.003 ↩︎
- Paul Jacobs, Genevieve Kenney, and Thomas Selden, “Newly Eligible Enrollees In Medicaid Spend Less And Use Less Care Than Those Previously Eligible,” Health Affairs 36, no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0252 ↩︎
- Ahmedin Jemal, Chun Chieh Lin, Amy Davidoff, and Xuesong Han, “Changes in Insurance Coverage and Stage at Diagnosis Among Nonelderly Patients with Cancer after the Affordable Care Act,” Journal of Clinical Oncology 35, no. 35 (December 2017), http://ascopubs.org/doi/pdf/10.1200/JCO.2017.73.7817 ↩︎
- Claire E. Margerison et al., “Impacts of Medicaid Expansion on Health Among Women of Reproductive Age,” American Journal of Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.amepre.2019.08.019 ↩︎
- Emily Johnston, Andrea Strahan, Peter Joski, Anne Dunlop, and E. Kathleen Adams, “Impacts of the Affordable Care Act’s Medicaid Expansion on Women of Reproductive Age,” Women’s Health Issues, 28, no. 2 (February 2018), http://www.whijournal.com/article/S1049-3867(17)30242-6/pdf ↩︎
- Andrew W. Mulcahy, Christine Eibner, and Kenneth Finegold, “Gaining Coverage Through Medicaid Or Private Insurance Increased Prescription Use and Lowered Out-Of-Pocket Spending,” Health Affairs 35, no. 9 (September 2016), http://content.healthaffairs.org/content/early/2016/08/16/hlthaff.2016.0091.full ↩︎
- Heather Holderness et al., “Where Do Oregon Medicaid Enrollees Seek Outpatient Care Post-Affordable Care Act Medicaid Expansion?,” Medical Care 57, no. 10 (October 2019): 788-794, https://doi.org/10.1097/mlr.0000000000001189 ↩︎
- Sara Rosenbaum, Jennifer Tolbert, Jessica Sharac, Peter Shin, Rachel Gunsalus, and Julia Zur, Community Health Centers: Growing Importance in a Changing Health Care System (Washington, DC: Kaiser Family Foundation, March 2018), https://modern.kff.org/medicaid/issue-brief/community-health-centers-growing-importance-in-a-changing-health-care-system/ ↩︎
- Brendan Saloner, Rachel Landis, Bradley Stein, and Colleen Barry, “The Affordable Care Act in the Heart of the Opioid Crisis: Evidence from West Virginia,” Health Affairs 38, no. 4 (April 2019), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05049 ↩︎
- Jessica Vistnes and Joel Cohen, “Gaining Coverage in 2014: New Estimates of Marketplace and Medicaid Transitions,” Health Affairs 35 no. 10 (October 2016): 1825-1829, http://content.healthaffairs.org/content/35/10/1825.full?sid=cc385dd5-9c95-4ee1-9c58-888408d49c54 ↩︎
- Johanna Maclean and Brendan Saloner, The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act (National Bureau of Economic Research Working Paper No. 23342, April 2017), http://www.nber.org/papers/w23342.pdf ↩︎
- Craig Garthwaite, Tal Gross, Matthew Notowidigdo, and John Graves, “Insurance Expansion and Hospital Emergency Department Access: Evidence from the Affordable Care Act,” Annals of Internal Medicine 166 no. 3 (February 2017): 172-179, http://annals.org/aim/article/2593599/insurance-expansion-hospital-emergency-department-access-evidence-from-affordable-care ↩︎
- Ramin Mojtabai, Christine Mauro, Melanie Wall, Colleen Barry, and Mark Olfson, “Medication Treatment For Opioid Use Disorders In Substance Use Treatment Facilities,” Health Affairs 38, no. 1 (January 2019), https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.05162 ↩︎
- Yunwei Gai and John Marthinsen, “Medicaid Expansion, HIV Testing, and HIV-Related Risk Behaviors in the United States, 2010-2017,” American Journal of Public Health 109, no. 10 (October 2019): 1404-1412, https://doi.org/10.2105/ajph.2019.305220 ↩︎
- Johanna Catherine Maclean, Michael F. Pesko, and Steven C. Hill, “Public Insurance Expansions and Smoking Cessation Medications,” Economic Inquiry 57, no. 4 (October 2019): 1798-1820, https://doi.org/10.1111/ecin.12794 ↩︎
- Dennis McCarty, Yifan Gu, John W. McIlveen, and Bonnie K. Lind, “Medicaid Expansion and Treatment for Opioid Use Disorders in Oregon: An Interrupted Time-Series Analysis,” Addiction Science & Clinical Practice 14 (August 2019), https://doi.org/10.1186/s13722-019-0160-6 ↩︎
- Huabin Luo, Zhuo Chen, Lei Xu, and Ronny Bell, “Health Care Access and Receipt of Clinical Diabetes Preventive Care for Working-Age Adults With Diabetes in States With and Without Medicaid Expansion: Results from the 2013 and 2015 BRFSS,” Journal of Public Health Management and Practice 25, no. 4 (July/August 2019): 34-43, https://doi.org/10.1097/phh.0000000000000832 ↩︎
- Lindsay C. Kobayashi, Onur Altindag, Yulya Truskinovsky, and Lisa F. Berkman, “Effects of the Affordable Care Act Medicaid Expansion on Subjective Well-Being in the US Adult Population, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1236-1242, https://doi.org/10.2105/ajph.2019.305164 ↩︎
- A. Taylor Kelley, Renuka Tipirneni, and Helen Levy, “Changes in Veterans’ Coverage and Access to Care Following the Affordable Care Act, 2011-2017,” American Journal of Public Health 109, no. 9 (September 2019): 1233-1235, https://doi.org/10.2105/ajph.2019.305160 ↩︎
- Shiho Kino and Ichiro Kawachi, “Can Health Literacy Boost Health Services Utilization in the Context of Expanded Access to Health Insurance?,” Health Education & Behavior Epub ahead of print (October 2019), https://doi.org/10.1177/1090198119875998 ↩︎
- Hiroshi Gotanda, Gerald Kominski, and Yusuke Tsugawa, “Association Between the ACA Medicaid Expansions and Primary Care and Emergency Department Use During the First 3 Years,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05458-w ↩︎
- Evan M. Chen et al., “Association of the Affordable Care Act Medicaid Expansion with Dilated Eye Examinations among the United States Population with Diabetes,” Ophthalmology Epub ahead of print (September 2019), https://doi.org/10.1016/j.ophtha.2019.09.010 ↩︎
- Mark L. Diana et al., Louisiana Medicaid Expansion and Access to Care (Louisiana Department of Health, Prepared by Tulane University, July 2019), http://ldh.la.gov/assets/media/AccesstoCareReport20132018final.pdf ↩︎
- Susan Dorr Goold et al., “Primary Care, Health Promotion, and Disease Prevention with Michigan Medicaid Expansion,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05370-3 ↩︎
- Jesse M. Hinde et al., “Increasing Access to Opioid Use Disorder Treatment: Assessing State Policies and the Evidence Behind Them,” Journal of Studies on Alcohol and Drugs 80, no. 6 (November 2019): 693-697, https://doi.org/10.15288/jsad.2019.80.693 ↩︎
- Ann-Marie Rosland et al., “Diagnosis and Care of Chronic Health Conditions Among Medicaid Expansion Enrollees: a Mixed-Methods Observational Study,” Journal of General Internal Medicine 34, no. 11 (November 2019): 2549-2558, https://doi.org/10.1007/s11606-019-05323-w ↩︎
- Sri Lekha Tummalapalli, Samuel Leonard, Michelle M. Estrella, and Salomeh Keyhani, “The Effect of Medicaid Expansion on Self-Reported Kidney Disease,” Clinical Journal of American Society of Nephrology 14, no. 8 (August 2019): 1238-1240, https://doi.org/10.2215/cjn.02310219 ↩︎
- Chelsea L. Shover et al., “The Relationship of Medicaid Expansion to Psychiatric Comorbidity Care within Substance Use Disorder Treatment Programs,” Journal of Substance Abuse Treatment 105 (October 2019): 44-50, https://doi.org/10.1016/j.jsat.2019.07.012 ↩︎
- Ameen Barghi, Hugo Torres, Nancy Kressin, and Danny McCormick, “Coverage and Access for Americans with Cardiovascular Disease or Risk Factors After the ACA: a Quasi-experimental Study,” Journal of General Internal Medicine epub ahead of print (June 2019), https://link.springer.com/article/10.1007%2Fs11606-019-05108-1 ↩︎
- Hyunjung Lee and Frank Porell, “The Effect of the Affordable Care Act Medicaid Expansion on Disparities in Access to Care and Health Status,” Medical Care Research and Review epub ahead of print (October 2018), https://journals.sagepub.com/doi/abs/10.1177/1077558718808709?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=mcrd ↩︎
- Rebecca Myerson, Tianyi Lu, Ivy Tonnu-Mihara, and Elbert Huang, “Medicaid Eligibility Expansions May Address Gaps In Access To Diabetes Medications,” Health Affairs 37, no. 8 (August 2018), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.0154 ↩︎
- Carrie Fry and Benjamin Sommers, “Effect of Medicaid Expansion on Health Insurance Coverage and Access to Care Among Adults With Depression,” Psychiatric Services 69, no. 11 (November 2018), https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201800181 ↩︎
- Elham Mahmoudi, Alicia Cohen, Jason Buxbaum, Caroline Richardson, and Wassim Tarraf, “Gaining Medicaid Coverage During ACA Implementation: Effects on Access to Care and Preventive Services,” Journal of Health Care for the Poor and Underserved 29, no. 4 (November 2018): 1472-1487, https://muse.jhu.edu/article/708253 ↩︎
- Ausmita Ghosh, Kosali Simon, and Benjamin Sommers, “The Effect of Health Insurance on Prescription Drug Use Among Low-Income Adults: Evidence from Recent Medicaid Expansions,” Journal of Health Economics 63 (January 2019): 64-80, https://www.sciencedirect.com/science/article/pii/S0167629617300206 ↩︎
- Alana Sharp, Austin Jones, Jennifer Sherwood, Oksana Kutsa, Brian Honermann, and Gregorio Millett, “Impact of Medicaid Expansion on Access to Opioid Analgesic Medications and Medication-Assisted Treatment,” American Journal of Public Health 108, no. 5 (May 2018): 642-648, https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2018.304338?journalCode=ajph ↩︎
- Angelica Meinhofer and Allison Witman, “The Role Of Health Insurance On Treatment For Opioid Use Disorders: Evidence From The Affordable Care Act Medicaid Expansion,” Journal of Health Economics 60 (June 2018): 177-197, https://www.sciencedirect.com/science/article/abs/pii/S0167629617311530 ↩︎
- Chad Cotti, Erik Nesson, and Nathan Tefft, “Impacts Of The ACA Medicaid Expansion On Health Behaviors: Evidence From Household Panel Data,” Health Economics 28, no. 2 (February 2019): 219-244, https://onlinelibrary.wiley.com/doi/pdf/10.1002/hec.3838 ↩︎
- Richard Frank and Carrie Fry, “The Impact of Expanded Medicaid Eligibility on Access To Naloxone,” Addiction epub ahead of print (April 2019), https://onlinelibrary.wiley.com/doi/abs/10.1111/add.14634 ↩︎
- Michael Hendryx and Juhua Luo, “Increased Cancer Screening for Low-income Adults Under the Affordable Care Act Medicaid Expansion,” Medical Care 56, no. 11 (November 2018): 944-949, https://www.ingentaconnect.com/content/wk/mcar/2018/00000056/00000011/art00009 ↩︎
- Cheryl Zogg et al., “Association of Medicaid Expansion With Access to Rehabilitative Care in Adult Trauma Patients,” JAMA Surgery epub ahead of print (January 2019), https://jamanetwork.com/journals/jamasurgery/article-abstract/2719270?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamasurg.2018.5177 ↩︎
- Emanuel Eguia et al., “Impact of the Affordable Care Act (ACA) Medicaid Expansion on Cancer Admissions and Surgeries,” Annals of Surgery 268, no. 4 (October 2018): 584-590, https://journals.lww.com/annalsofsurgery/Abstract/2018/10000/Impact_of_the_Affordable_Care_Act__ACA__Medicaid.6.aspx ↩︎
- Jonathan Routh et al., “Early Impact of the Patient Protection and Affordable Care Act on Delivery of Children’s Surgical Care,” Clinical Pediatrics 58, no. 4 (January 2019) 453-460, https://journals.sagepub.com/doi/abs/10.1177/0009922818825156?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=cpja ↩︎
- Andrew Crocker et al., “The Affordable Care Act’s Medicaid Expansion And Utilization Of Discretionary Vs. Non-Discretionary Inpatient Surgery,” Surgery 164, no. 6 (December 2018): 1156-1161, https://www.sciencedirect.com/science/article/pii/S0039606018302186 ↩︎
- Brendan Saloner, Jonathan Levin, Hsien-Yen Chang, Christopher Jones, and G. Caleb Alexander, “Changes in Buprenorphine-Naloxone and Opioid Pain Reliever Prescriptions After the Affordable Care Act Medicaid Expansion,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2696873 ↩︎
- Cheryl Zogg et al., “Impact of Affordable Care Act Insurance Expansion on Pre-Hospital Access to Care: Changes in Adult Perforated Appendix Admission Rates after Medicaid Expansion and the Dependent Coverage Provision,” Journal of the American College of Surgeons 228, no. 1 (January 2019): 29-43, https://www.journalacs.org/article/S1072-7515(18)32078-7/fulltext ↩︎
- Xuesong Han, Robin Yabroff, Elizabeth Ward, Otis Brawley, and Ahmedin Jemal, “Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act,” JAMA Oncology 4, no. 12 (August 2018): 1713-1720, https://jamanetwork.com/journals/jamaoncology/article-abstract/2697226 ↩︎
- Manzilat Akande Peter Minneci, Katherine Deans, Henry Xiang, and Jennifer Cooper, “Association of Medicaid Expansion Under the Affordable Care Act With Outcomes and Access to Rehabilitation in Young Adult Trauma Patients,” JAMA Surgery 153, no. 8 (August 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2682872?widget=personalizedcontent&previousarticle=2719270 ↩︎
- J.W. Awori Hayanga et al., “Lung Transplantation and Affordable Care Act Medicaid Expansion in the Era of Lung Allocation Score” Transplant International epub ahead of print (February 2019), https://onlinelibrary.wiley.com/doi/pdf/10.1111/tri.13420 ↩︎
- Susan Dorr Goold et al., “Primary Care Clinicians’ Views About the Impact of Medicaid Expansion in Michigan: A Mixed Methods Study,” Journal of General Internal Medicine 33, no. 8 (June 2018): 1307-1316, https://link.springer.com/article/10.1007/s11606-018-4487-6 ↩︎
- Michelle Moniz et al., “Association of Access to Family Planning Services With Medicaid Expansion Among Female Enrollees in Michigan,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2698636 ↩︎
- Benjamin Cher, Nancy Morden, and Ellen Meara, “Medicaid Expansion and Prescription Trends: Opioids, Addiction Therapies, and Other Drugs,” Medical Care 57, no. 3 (March 2019): 208-212, https://journals.lww.com/lww-medicalcare/fulltext/2019/03000/Medicaid_Expansion_and_Prescription_Trends_.6.aspx ↩︎
- Robert Sandstrom, “Increased Utilization of Ambulatory Occupational Therapy and Physical Therapy After Medicaid Expansion” Archives of Physical Medicine and Rehabilitation epub ahead of print (March 2019), https://www.archives-pmr.org/article/S0003-9993(19)30161-3/fulltext ↩︎
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf ↩︎
- Matthew Present, Aviva Nathan, Sandra Ham, Robert Sargis, Michael Quinn, and Elbert Huang, “The Impact of the Affordable Care Act Medicaid Expansion on Type 2 Diabetes Diagnosis and Treatment: A National Survey of Physicians,” Journal of Community Health epub ahead of print (May 2019), https://link.springer.com/article/10.1007%2Fs10900-019-00637-6 ↩︎
- Bryce Ward and Brandon Bridge, The Economic Impact of Medicaid Expansion in Montana: Updated Findings (Bureau of Business and Economic Research, January 2019), https://mthcf.org/wp-content/uploads/2019/01/Economic-Impact-of-MedEx-in-MT_1.28.19-FINAL.pdf ↩︎
- Tong Gan et al., “Impact of the Affordable Care Act on Colorectal Cancer Screening, Incidence, and Survival in Kentucky,” Journal of the American College of Surgeons 228, no. 4 (April 2019): 342-353.e1, https://www.journalacs.org/article/S1072-7515(19)30046-8/fulltext ↩︎
- Vikki Wachino and Samantha Artiga, How Connecting Justice-Involved Individuals to Medicaid Can Help Address the Opioid Epidemic (Washington, DC: Kaiser Family Foundation, June 2019), https://modern.kff.org/medicaid/issue-brief/how-connecting-justice-involved-individuals-to-medicaid-can-help-address-the-opioid-epidemic/ ↩︎
- Pennsylvania Department of Human Services, Medicaid Expansion Report, (Pennsylvania Department of Human Services, January 2017), http://www.dhs.pa.gov/cs/groups/webcontent/documents/document/c_257436.pdf ↩︎
- Steffani Bailey et al., “Tobacco Cessation in Affordable Care Act Medicaid Expansion States Versus Non-expansion States,” Nicotine & Tobacco Research epub ahead of print (May 2019), https://academic.oup.com/ntr/advance-article-abstract/doi/10.1093/ntr/ntz087/5498071 ↩︎
- Ramin Mojtabai, Christine Mauro, Melanie Wall, Colleen Barry, and Mark Olfson, “The Affordable Care Act and Opioid Agonist Therapy for Opioid Use Disorder,” Psychiatry Online (April 2019), https://doi.org/10.1176/appi.ps.201900025 ↩︎
- Andrew Crocker et al., “Expansion Coverage And Preferential Utilization Of Cancer Surgery Among Racial And Ethnic Minorities And Low-Income Groups,” Surgery epub ahead of print (June 2019), https://www.surgjournal.com/article/S0039-6060(19)30198-9/fulltext ↩︎
- Sarah Miller and Laura Wherry, “Four Years Later: Insurance Coverage and Access to Care Continue to Diverge between ACA Medicaid Expansion and Non-Expansion States,” American Economic Association Papers and Proceedings 109 (May 2019): 327-333, https://www.aeaweb.org/articles?id=10.1257/pandp.20191046 ↩︎
- Jose Mesquita-Neto, Peter Cmorej, Hassan Mouzaihem, Donald Weaver, Steve Kim, and Francis Macedo, “Disparities In Access To Cancer Surgery After Medicaid Expansion,” The American Journal of Surgery epub ahead of print (June 2019), https://www.sciencedirect.com/science/article/abs/pii/S0002961019306889 ↩︎
- Nicolas Ajkay et al, “Early Impact of Medicaid Expansion and Quality of Breast Cancer Care in Kentucky,” Journal of the American College of Surgeons, epub ahead of print, February 2018, https://www.sciencedirect.com/science/article/pii/S107275151830022X ↩︎
- Sunha Choi, Sungkyu Lee, and Jason Matejkowski, “The Effects of State Medicaid Expansion on Low-Income Individuals’ Access to Health Care: Multilevel Modeling,” Population Health Management epub ahead of print (September 2017), http://online.liebertpub.com/doi/abs/10.1089/pop.2017.0104 ↩︎
- Aparna Soni, Kosali Simon, John Cawley, and Lindsay Sabik, “Effect of Medicaid Expansions of 2014 on Overall and Early-Stage Cancer Diagnoses,” American Journal of Public Health epub ahead of print (December 2017), http://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2017.304166 ↩︎
- Tyler Winkelman and Virginia Chang, “Medicaid Expansion, Mental Health, and Access to Care Among Childless Adults With and Without Chronic Conditions,” Journal of General Internal Medicine epub ahead of print (November 2017), https://www.ncbi.nlm.nih.gov/pubmed/29181792 ↩︎
- Andrew Loehrer et al., “Association of the Affordable Care Act Medicaid Expansion with Access to and Quality of Care for Surgical Conditions,” Journal of the American Medical Association Surgery, epub ahead of print (January 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2670459?redirect=true ↩︎
- Susan Hayes, Pamela Riley, David Radley, and Douglas McCarthy, Reducing Racial and Ethnic Disparities in Access to Care: Has the Affordable Care Act Made a Difference? (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/racial-ethnic-disparities-care ↩︎
- Samantha Artiga, Barbara DiPietro, and Petry Ubri, The Role of Medicaid and the Impact of the Medicaid Expansion for Veterans Experiencing Homelessness, (Washington, DC: Kaiser Family Foundation, October 2017), https://modern.kff.org/medicaid/issue-brief/the-role-of-medicaid-and-impact-of-the-medicaid-expansion-for-veterans-experiencing-homelessness/ ↩︎
- Dahai Yue, Petra Rasmussen, and Ninez Ponce, “Racial/Ethnic Differential Effects of Medicaid Expansion on Health Care Access,” Health Services Research (February 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12834/abstract ↩︎
- Michael Dworsky, Carrie Farmer, and Mimi Shen, Veterans’ Health Insurance Coverage Under the Affordable Care Act and Implications of Repeal for the Department of Veterans Affairs, (RAND Corporation, 2017), https://www.rand.org/pubs/research_reports/RR1955.html ↩︎
- Kevin Griffith, Leigh Evans, and Jacob Bor, “The Affordable Care Act Reduced Socioeconomic Disparities in Health Care Access,” Health Affairs 36 no. 8 (August 2017), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0083 ↩︎
- Jacqueline Fiore, The Impact of the Affordable Care Act’s Medicaid Expansion on Medicaid Spending by Health Care Service Category (Tulane University, July 2017), http://econ.tulane.edu/RePEc/pdf/tul1706.pdf ↩︎
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293 ↩︎
- Louisiana Department of Health, Medicaid Expansion 2016/17 (Baton Rouge, Louisiana Department of Health, June 2017), http://dhh.louisiana.gov/assets/HealthyLa/Resources/MdcdExpnAnnlRprt_2017_WEB.pdf ↩︎
- Nirosha Mahendraratnam, Stacie Dusetzina, and Joel Farley, “Prescription Drug Utilization and Reimbursement Increased Following State Medicaid Expansion in 2014,” Journal of Managed Care & Specialty Pharmacy 23 no. 3 (March 2017): 355-363, http://www.jmcp.org/doi/10.18553/jmcp.2017.23.3.355 ↩︎
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890 ↩︎
- James Kirby and Jessica Vistnes, “Access to Care Improved for People Who Gained Medicaid or Marketplace Coverage in 2014,” Health Affairs 35 no. 10 (October 2016): 1830-1834, http://content.healthaffairs.org/content/35/10/1830.full ↩︎
- Khadijah Breathett et al., “The Affordable Care Act Medicaid Expansion Correlated with Increased Heart Transplant Listings in African Americans but Not Hispanics or Caucasians,” JACC: Heart Failure 5 no. 2 (January 2017): 136-147, https://www.ncbi.nlm.nih.gov/pubmed/28109783 ↩︎
- United States Government Accountability Office (GAO), Medicaid Expansion: Behavioral Health Treatment Use in Selected States in 2014 (Washington, DC: GAO Report to Congressional Requesters, June 2017), https://www.gao.gov/assets/690/685415.pdf ↩︎
- Lisa Clemans-Cope, Marni Epstein, Victoria Lynch, and Emma Winiski, Rapid Growth in Medicaid Spending and Prescriptions to Treat Opioid Use Disorder and Opioid Overdose from 2010 to 2017 (Washington, DC: The Urban Institute, March 2019), https://www.urban.org/sites/default/files/publication/99798/rapid_growth_in_medicaid_spending_and_prescriptions_to_treat_opioid_use_disorder_and_opioid_overdose_from_2010_to_2017_2.pdf ↩︎
- Hefei Wen, Jason Hockenberry, Tyrone Borders, and Benjamin Druss, “Impact of Medicaid Expansion on Medicaid-covered Utilization of Buprenorphine for Opioid Use Disorder Treatment,” Medical Care 55 no. 4 (April 2017): 336-341, http://journals.lww.com/lww-medicalcare/Fulltext/2017/04000/Impact_of_Medicaid_Expansion_on_Medicaid_covered.5.aspx ↩︎
- Megan Cole, Omar Galarraga, Ira Wilson, Brad Wright, and Amal Trivedi, “At Federally Funded Health Centers, Medicaid Expansion was Associated with Improved Quality of Care,” Health Affairs 36 no. 1 (January 2017): 40-48, http://content.healthaffairs.org/content/36/1/40.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19 ↩︎
- Eili Klein et al., “The Effect of Medicaid Expansion on Utilization in Maryland Emergency Departments,” Annals of Emergency Medicine epub ahead of print (June 2017), http://www.annemergmed.com/article/S0196-0644(17)30784-9/pdf ↩︎
- Aabha Sharma, Scott Dresden, Emilie Powell, Raymond Kang, Joe Feinglass, “Emergency Department Visits and Hospitalizations for the Uninsured in Illinois Before and After Affordable Care Act Insurance Expansion,” Journal of Community Health 42 no. 3 (June 2017): 591-597, https://link.springer.com/article/10.1007/s10900-016-0293-4 ↩︎
- Daniel Gingold, Rachelle Pierre-Mathieu, Brandon Cole, Andrew Miller, and Joneigh Khaldun, “Impact of the Affordable Care Act Medicaid Expansion on Emergency Department High Utilizers with Ambulatory Care Sensitive Conditions: A Cross-Sectional Study,” The American Journal of Emergency Medicine (January 2017), http://www.sciencedirect.com/science/article/pii/S0735675717300141 ↩︎
- Gary Pickens et al., “Changes in Hospital Inpatient Utilization Following Health Care Reform,” Health Services Research epub ahead of print (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28664983 ↩︎
- Jeremy Holzmacher et al., “Association of Expanded Medicaid Coverage with Hospital Length of Stay After Injury,” JAMA Surgery published online (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28658482 ↩︎
- Mary Anderson, Jeffrey Glasheen, and Debra Anoff, “Impact of State Medicaid Expansion Status on Length of Stay and In-Hospital Mortality for General Medicine Patients at US Academic Medical Centers,” Journal of Hospital Medicine Epub ahead of print (August 2016), http://onlinelibrary.wiley.com/wol1/doi/10.1002/jhm.2649/citedby ↩︎
- Benjamin Sommers, Robert Blendon, E. John Orav, and Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420 ↩︎
- Megan Hoopes, Heather Angier, Rachel Gold, Steffani Bailey, Nathalie Huguet, Miguel Marino, and Jennifer DeVoe, “Utilization of Community Health Centers in Medicaid Expansion and Nonexpansion States, 2013-2014,” Journal of Ambulatory Care Management 39 no. 4 (October 2016): 290-298, https://www.ncbi.nlm.nih.gov/pubmed/26765808 ↩︎
- Sara Collins, Munira Gunja, Michelle Doty, and Sophie Beutel, Americans’ Experiences with ACA Marketplace and Medicaid Coverage: Access to Care and Satisfaction (The Commonwealth Fund, May 2016), http://www.commonwealthfund.org/publications/issue-briefs/2016/may/aca-tracking-survey-access-to-care-and-satisfaction ↩︎
- Astha Singhal, Peter Damiano, and Lindsay Sabik, “Medicaid Adult Dental Benefits Increase Use Of Dental Care, But Impact Of Expansion On Dental Services Use Was Mixed,” Health Affairs 36 no. 4 (April 2017): 723-732, http://content.healthaffairs.org/content/36/4/723.short ↩︎
- Angela Fertig, Caroline Carlin, Scote Ode, and Sharon Long, “Evidence of Pent-Up Demand for Care After Medicaid Expansion,” Medical Care Research and Review epub ahead of print (March 2017), http://journals.sagepub.com/eprint/wDsfA74fuA3BIw5ZWyYT/full ↩︎
- Anne DiGiulio et al., “State Medicaid Expansion Tobacco Cessation Coverage and Number of Adult Smokers Enrolled in Expansion Coverage – United States, 2016,” Morbidity and Mortality Weekly Report 65, no. 48 (December 2016), https://www.cdc.gov/mmwr/volumes/65/wr/mm6548a2.htm ↩︎
- Ausmita Ghosh, Kosali Simon, and Benjamin Sommers, The Effect of State Medicaid Expansions on Prescription Drug Use: Evidence from the Affordable Care Act (Working Paper No. 23044, National Bureau of Economic Research, January 2017), http://www.nber.org/papers/w23044?utm_campaign=ntw&utm_medium=email&utm_source=ntw ↩︎
- Joseph Benitez, Liza Creel, and J’Aime Jennings, “Kentucky’s Medicaid Expansion Showing Early Promise on Coverage and Access to Care,” Health Affairs (February 2016), http://content.healthaffairs.org/content/early/2016/02/16/hlthaff.2015.1294 ↩︎
- Adele Shartzer, Sharon Long, and Nathaniel Anderson, “Access To Care and Affordability have Improved Following Affordable Care Act Implementation; Problems Remain,” Health Affairs (December 2015), http://content.healthaffairs.org/content/early/2015/12/14/hlthaff.2015.0755.full ↩︎
- Kamyar Nasseh and Marko Vujicic, Early Impact of the Affordable Care Act’s Medicaid Expansion on Dental Care Use (Health Services Research, November 2016), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12606/full ↩︎
- MaryBeth Musumeci, Robin Rudowitz, Petry Ubri, and Elizabeth Hinton, An Early Look at Medicaid Expansion Waiver Implementation in Michigan and Indiana (Washington, DC: The Kaiser Family Foundation, January 2017), http://kff.org/medicaid/issue-brief/an-early-look-at-medicaid-expansion-waiver-implementation-in-michigan-and-indiana/ ↩︎
- Jeffrey Horn et al., “New Medicaid Enrollees See Health and Social Benefits in Pennsylvania’s Expansion,” INQUIRY: the Journal of Health Care Organization, Provision, and Financing 53 (October 2016): 1-8, http://journals.sagepub.com/doi/full/10.1177/0046958016671807# ↩︎
- Benjamin Sommers, Munira Gunja, Kenneth Finegold, and Thomas Musco, “Changes in Self-Reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act,” The Journal of the American Medical Association 314 no. 4 (July 2015): 366-374, http://jama.jamanetwork.com/article.aspx?articleid=2411283&resultClick=3 ↩︎
- IMS Institute for Healthcare Informatics, Medicines Use and Spending Shifts: A Review of the Use of Medicines in the US in 2014 (IMS Institute for Healthcare Informatics, April 2015), http://www.imshealth.com/en/thought-leadership/ims-institute/reports/medicines-use-in-the-us-2014 ↩︎
- Government Accountability Office, Behavioral Health: Options for Low-Income Adults to Receive Treatment in Selected States (Washington, DC: Government Accountability Office, June 2015), http://www.gao.gov/assets/680/670894.pdf ↩︎
- Barbara DiPietro, Samantha Artiga, and Alexandra Gates, Early Impacts of the Medicaid Expansion for the Homeless Population (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, November 2014), http://kff.org/uninsured/issue-brief/early-impacts-of-the-medicaid-expansion-for-the-homeless-population/ ↩︎
- Josh Gray, Anna Zink, and Tony Dreyfus, Effects of the Affordable Care Act Through 2015, (athenaResearch and Robert Wood Johnson Foundation ACA View Report, March 2016), http://www.athenahealth.com/~/media/athenaweb/files/pdf/acaview_tracking_the_impact_of_health_care_reform ↩︎
- Laura Wherry and Sarah Miller, “Early Coverage, Access, Utilization, and Health Effects Associated with the Affordable Care Act Medicaid Expansions: A Quasi-experimental Study,” Annals of Internal Medicine, Epub ahead of print (April 2016), http://annals.org/article.aspx?articleid=2513980 ↩︎
- Josh Gray, Iyue Sung, and Stewart Richardson, Observations on the Affordable Care Act: 2014 (athenaResearch and Robert Wood Johnson Foundation ACA View Report, February 2015), http://www.athenahealth.com/~/media/athenaweb/files/pdf/acaview_year_end_2014.pdf ↩︎
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf ↩︎
- John Cawley, Aparna Soni, and Kosali Simon, “Third Year of Survey Data Shows Continuing Benefits of Medicaid Expansions for Low-Income Childless Adults in the U.S.,” Journal of General Internal Medicine 33, no. 9 (September 2018): 1495-1497, https://link.springer.com/article/10.1007%2Fs11606-018-4537-0 ↩︎
- Kosali Simon, Aparna Soni, and John Cawley, “The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions” Journal of Policy Analysis and Management 36, no. 2 (March 2017), https://onlinelibrary.wiley.com/doi/abs/10.1002/pam.21972 ↩︎
- Harvey Kaufman, Zhen Chen, Vivian Fonseca, and Michael McPhaul, “Surge in Newly Identified Diabetes Among Medicaid Patients in 2014 Within Medicaid Expansion States Under the Affordable Care Act,” Diabetes Care 38, no. 5 (May 2015): 833, http://care.diabetesjournals.org/content/early/2015/03/19/dc14-2334.full.pdf+html ↩︎
- De-Chih Lee, Leiyu Shi, and Hailun Liang, “Primary Care Utilization And Clinical Quality Performance: A Comparison Between Health Centres In Medicaid Expansion States And Non-Expansion States,” Journal of Health Services Research & Policy 24, no. 1 (January 2019): 19-24, https://journals.sagepub.com/doi/abs/10.1177/1355819618788592 ↩︎
- Aparna Soni, Kosali Simon, John Cawley, and Lindsay Sabik, “Effect of Medicaid Expansions of 2014 on Overall and Early-Stage Cancer Diagnoses,” American Journal of Public Health epub ahead of print (December 2017), http://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2017.304166 ↩︎
- Helmneh M. Sineshaw et al., “Association of Medicaid Expansion Under the Affordable Care Act With Stage at Diagnosis and Time to Treatment Initiation for Patients With Head and Neck Squamous Cell Carcinoma,” JAMA Otolaryngology–Head & Neck Surgery Epub ahead of print (January 2020), https://doi.org/10.1001/jamaoto.2019.4310 ↩︎
- Nicolas Ajkay et al, “Early Impact of Medicaid Expansion and Quality of Breast Cancer Care in Kentucky,” Journal of the American College of Surgeons, epub ahead of print, February 2018, https://www.sciencedirect.com/science/article/pii/S107275151830022X ↩︎
- Xuesong Han, Robin Yabroff, Elizabeth Ward, Otis Brawley, and Ahmedin Jemal, “Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act,” JAMA Oncology 4, no. 12 (August 2018): 1713-1720, https://jamanetwork.com/journals/jamaoncology/article-abstract/2697226 ↩︎
- Jose Mesquita-Neto, Peter Cmorej, Hassan Mouzaihem, Donald Weaver, Steve Kim, and Francis Macedo, “Disparities In Access To Cancer Surgery After Medicaid Expansion,” The American Journal of Surgery epub ahead of print (June 2019), https://www.sciencedirect.com/science/article/abs/pii/S0002961019306889 ↩︎
- Tong Gan et al., “Impact of the Affordable Care Act on Colorectal Cancer Screening, Incidence, and Survival in Kentucky,” Journal of the American College of Surgeons 228, no. 4 (April 2019): 342-353.e1, https://www.journalacs.org/article/S1072-7515(19)30046-8/fulltext ↩︎
- Andrew Loehrer et al., “Association of the Affordable Care Act Medicaid Expansion with Access to and Quality of Care for Surgical Conditions,” Journal of the American Medical Association Surgery, epub ahead of print (January 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2670459?redirect=true ↩︎
- Andrew Crocker et al., “Expansion Coverage And Preferential Utilization Of Cancer Surgery Among Racial And Ethnic Minorities And Low-Income Groups,” Surgery epub ahead of print (June 2019), https://www.surgjournal.com/article/S0039-6060(19)30198-9/fulltext ↩︎
- Emanuel Eguia et al., “Impact of the Affordable Care Act (ACA) Medicaid Expansion on Cancer Admissions and Surgeries,” Annals of Surgery 268, no. 4 (October 2018): 584-590, https://journals.lww.com/annalsofsurgery/Abstract/2018/10000/Impact_of_the_Affordable_Care_Act__ACA__Medicaid.6.aspx ↩︎
- Louisiana Department of Health, Medicaid Expansion 2016/17 (Baton Rouge, Louisiana Department of Health, June 2017), http://dhh.louisiana.gov/assets/HealthyLa/Resources/MdcdExpnAnnlRprt_2017_WEB.pdf ↩︎
- Ahmedin Jemal, Chun Chieh Lin, Amy Davidoff, and Xuesong Han, “Changes in Insurance Coverage and Stage at Diagnosis Among Nonelderly Patients with Cancer after the Affordable Care Act,” Journal of Clinical Oncology 35, no. 35 (December 2017), http://ascopubs.org/doi/pdf/10.1200/JCO.2017.73.7817 ↩︎
- Andrew Crocker et al., “The Affordable Care Act’s Medicaid Expansion And Utilization Of Discretionary Vs. Non-Discretionary Inpatient Surgery,” Surgery 164, no. 6 (December 2018): 1156-1161, https://www.sciencedirect.com/science/article/pii/S0039606018302186 ↩︎
- Khadijah Breathett et al., “The Affordable Care Act Medicaid Expansion Correlated with Increased Heart Transplant Listings in African Americans but Not Hispanics or Caucasians,” JACC: Heart Failure 5 no. 2 (January 2017): 136-147, https://www.ncbi.nlm.nih.gov/pubmed/28109783 ↩︎
- J.W. Awori Hayanga et al., “Lung Transplantation and Affordable Care Act Medicaid Expansion in the Era of Lung Allocation Score” Transplant International epub ahead of print (February 2019), https://onlinelibrary.wiley.com/doi/pdf/10.1111/tri.13420 ↩︎
- Johanna Catherine Maclean, Michael F. Pesko, and Steven C. Hill, “Public Insurance Expansions and Smoking Cessation Medications,” Economic Inquiry 57, no. 4 (October 2019): 1798-1820, https://doi.org/10.1111/ecin.12794 ↩︎
- Deborah Yip et al., “Association of Medicaid Expansion and Health Insurance with Receipt of Smoking Cessation Services and Smoking Behaviors in Substance Use Disorder Treatment,” The Journal of Behavioral Health Services & Research (July 2019), https://doi.org/10.1007/s11414-019-09669-1 ↩︎
- Chad Cotti, Erik Nesson, and Nathan Tefft, “Impacts Of The ACA Medicaid Expansion On Health Behaviors: Evidence From Household Panel Data,” Health Economics 28, no. 2 (February 2019): 219-244, https://onlinelibrary.wiley.com/doi/pdf/10.1002/hec.3838 ↩︎
- Anne DiGiulio et al., “State Medicaid Expansion Tobacco Cessation Coverage and Number of Adult Smokers Enrolled in Expansion Coverage – United States, 2016,” Morbidity and Mortality Weekly Report 65, no. 48 (December 2016), https://www.cdc.gov/mmwr/volumes/65/wr/mm6548a2.htm ↩︎
- Steffani Bailey et al., “Tobacco Cessation in Affordable Care Act Medicaid Expansion States Versus Non-expansion States,” Nicotine & Tobacco Research epub ahead of print (May 2019), https://academic.oup.com/ntr/advance-article-abstract/doi/10.1093/ntr/ntz087/5498071 ↩︎
- Kosali Simon, Aparna Soni, and John Cawley, “The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions” Journal of Policy Analysis and Management 36, no. 2 (March 2017), https://onlinelibrary.wiley.com/doi/abs/10.1002/pam.21972 ↩︎
- Dennis McCarty, Yifan Gu, John W. McIlveen, and Bonnie K. Lind, “Medicaid Expansion and Treatment for Opioid Use Disorders in Oregon: An Interrupted Time-Series Analysis,” Addiction Science & Clinical Practice 14 (August 2019), https://doi.org/10.1186/s13722-019-0160-6 ↩︎
- Jesse M. Hinde et al., “Increasing Access to Opioid Use Disorder Treatment: Assessing State Policies and the Evidence Behind Them,” Journal of Studies on Alcohol and Drugs 80, no. 6 (November 2019): 693-697, https://doi.org/10.15288/jsad.2019.80.693 ↩︎
- Chelsea L. Shover et al., “The Relationship of Medicaid Expansion to Psychiatric Comorbidity Care within Substance Use Disorder Treatment Programs,” Journal of Substance Abuse Treatment 105 (October 2019): 44-50, https://doi.org/10.1016/j.jsat.2019.07.012 ↩︎
- Alana Sharp, Austin Jones, Jennifer Sherwood, Oksana Kutsa, Brian Honermann, and Gregorio Millett, “Impact of Medicaid Expansion on Access to Opioid Analgesic Medications and Medication-Assisted Treatment,” American Journal of Public Health 108, no. 5 (May 2018): 642-648, https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2018.304338?journalCode=ajph ↩︎
- Angelica Meinhofer and Allison Witman, “The Role Of Health Insurance On Treatment For Opioid Use Disorders: Evidence From The Affordable Care Act Medicaid Expansion,” Journal of Health Economics 60 (June 2018): 177-197, https://www.sciencedirect.com/science/article/abs/pii/S0167629617311530 ↩︎
- Benjamin Cher, Nancy Morden, and Ellen Meara, “Medicaid Expansion and Prescription Trends: Opioids, Addiction Therapies, and Other Drugs,” Medical Care 57, no. 3 (March 2019): 208-212, https://journals.lww.com/lww-medicalcare/fulltext/2019/03000/Medicaid_Expansion_and_Prescription_Trends_.6.aspx ↩︎
- Brendan Saloner, Jonathan Levin, Hsien-Yen Chang, Christopher Jones, and G. Caleb Alexander, “Changes in Buprenorphine-Naloxone and Opioid Pain Reliever Prescriptions After the Affordable Care Act Medicaid Expansion,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2696873 ↩︎
- Richard Frank and Carrie Fry, “The Impact of Expanded Medicaid Eligibility on Access To Naloxone,” Addiction epub ahead of print (April 2019), https://onlinelibrary.wiley.com/doi/abs/10.1111/add.14634 ↩︎
- Ramin Mojtabai, Christine Mauro, Melanie Wall, Colleen Barry, and Mark Olfson, “The Affordable Care Act and Opioid Agonist Therapy for Opioid Use Disorder,” Psychiatry Online (April 2019), https://doi.org/10.1176/appi.ps.201900025 ↩︎
- Louisiana Department of Health, Medicaid Expansion 2016/17 (Baton Rouge, Louisiana Department of Health, June 2017), http://dhh.louisiana.gov/assets/HealthyLa/Resources/MdcdExpnAnnlRprt_2017_WEB.pdf ↩︎
- Carrie Fry and Benjamin Sommers, “Effect of Medicaid Expansion on Health Insurance Coverage and Access to Care Among Adults With Depression,” Psychiatric Services 69, no. 11 (November 2018), https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201800181 ↩︎
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf ↩︎
- Manatt Health, Medicaid Expansion: How It Affects Montana’s State Budget, Economy, and Residents (Montana Healthcare Foundation, prepared by Manatt Health, June 2018), https://mthcf.org/wp-content/uploads/2018/06/Manatt-MedEx_FINAL_6.1.18.pdf ↩︎
- Pennsylvania Department of Human Services, Medicaid Expansion Report, (Pennsylvania Department of Human Services, January 2017), http://www.dhs.pa.gov/cs/groups/webcontent/documents/document/c_257436.pdf ↩︎
- Brendan Saloner, Rachel Landis, Bradley Stein, and Colleen Barry, “The Affordable Care Act in the Heart of the Opioid Crisis: Evidence from West Virginia,” Health Affairs 38, no. 4 (April 2019), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05049 ↩︎
- Ramin Mojtabai, Christine Mauro, Melanie Wall, Colleen Barry, and Mark Olfson, “Medication Treatment For Opioid Use Disorders In Substance Use Treatment Facilities,” Health Affairs 38, no. 1 (January 2019), https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.05162 ↩︎
- United States Government Accountability Office (GAO), Medicaid Expansion: Behavioral Health Treatment Use in Selected States in 2014 (Washington, DC: GAO Report to Congressional Requesters, June 2017), https://www.gao.gov/assets/690/685415.pdf ↩︎
- Lisa Clemans-Cope, Marni Epstein, Victoria Lynch, and Emma Winiski, Rapid Growth in Medicaid Spending and Prescriptions to Treat Opioid Use Disorder and Opioid Overdose from 2010 to 2017 (Washington, DC: The Urban Institute, March 2019), https://www.urban.org/sites/default/files/publication/99798/rapid_growth_in_medicaid_spending_and_prescriptions_to_treat_opioid_use_disorder_and_opioid_overdose_from_2010_to_2017_2.pdf ↩︎
- Lisa Clemans-Cope, Victoria Lynch, Marni Epstein, and Genevieve Kenney, Medicaid Coverage of Effective Treatment for Opioid Use Disorder, (Washington, DC: The Urban Institute, June 2017), https://www.urban.org/sites/default/files/publication/90461/2001287_medicaid_coverage_of_effective_treatment_for_opioid_use_disorder.pdf ↩︎
- Hefei Wen, Jason Hockenberry, Tyrone Borders, and Benjamin Druss, “Impact of Medicaid Expansion on Medicaid-covered Utilization of Buprenorphine for Opioid Use Disorder Treatment,” Medical Care 55 no. 4 (April 2017): 336-341, http://journals.lww.com/lww-medicalcare/Fulltext/2017/04000/Impact_of_Medicaid_Expansion_on_Medicaid_covered.5.aspx ↩︎
- Brendan Saloner, Sachini Bandara, Emma McGinty, and Colleen Barry, “Justice-Involved Adults With Substance Use Disorders: Coverage Increased but Rates of Treatment Did Not in 2014,” Health Affairs 35 no. 6 (June 2016), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2016.0005 ↩︎
- Government Accountability Office, Behavioral Health: Options for Low-Income Adults to Receive Treatment in Selected States (Washington, DC: Government Accountability Office, June 2015), http://www.gao.gov/assets/680/670894.pdf ↩︎
- Barbara DiPietro, Samantha Artiga, and Alexandra Gates, Early Impacts of the Medicaid Expansion for the Homeless Population (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, November 2014), http://kff.org/uninsured/issue-brief/early-impacts-of-the-medicaid-expansion-for-the-homeless-population/ ↩︎
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf ↩︎
- Samantha Artiga, Barbara DiPietro, and Petry Ubri, The Role of Medicaid and the Impact of the Medicaid Expansion for Veterans Experiencing Homelessness, (Washington, DC: Kaiser Family Foundation, October 2017), https://modern.kff.org/medicaid/issue-brief/the-role-of-medicaid-and-impact-of-the-medicaid-expansion-for-veterans-experiencing-homelessness/ ↩︎
- Johanna Maclean and Brendan Saloner, “The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act,” Journal of Policy Analysis and Management 38, no. 2 (2019): 366-393, https://www.ncbi.nlm.nih.gov/pubmed/30882195 ↩︎
- Lisa Clemans-Cope, Victoria Lynch, Emma Winiski, and Marni Epstein, State Variation in Medicaid Prescriptions for Opioid Use Disorder from 2011 to 2018 (Washington, DC: The Urban Institute, August 2019), https://www.urban.org/research/publication/state-variation-medicaid-prescriptions-opioid-use-disorder-2011-2018 ↩︎
- Alana Sharp, Austin Jones, Jennifer Sherwood, Oksana Kutsa, Brian Honermann, and Gregorio Millett, “Impact of Medicaid Expansion on Access to Opioid Analgesic Medications and Medication-Assisted Treatment,” American Journal of Public Health 108, no. 5 (May 2018): 642-648, https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2018.304338?journalCode=ajph ↩︎
- Benjamin Cher, Nancy Morden, and Ellen Meara, “Medicaid Expansion and Prescription Trends: Opioids, Addiction Therapies, and Other Drugs,” Medical Care 57, no. 3 (March 2019): 208-212, https://journals.lww.com/lww-medicalcare/fulltext/2019/03000/Medicaid_Expansion_and_Prescription_Trends_.6.aspx ↩︎
- Brendan Saloner, Jonathan Levin, Hsien-Yen Chang, Christopher Jones, and G. Caleb Alexander, “Changes in Buprenorphine-Naloxone and Opioid Pain Reliever Prescriptions After the Affordable Care Act Medicaid Expansion,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2696873 ↩︎
- Lisa Clemans-Cope, Marni Epstein, Victoria Lynch, and Emma Winiski, Rapid Growth in Medicaid Spending and Prescriptions to Treat Opioid Use Disorder and Opioid Overdose from 2010 to 2017 (Washington, DC: The Urban Institute, March 2019), https://www.urban.org/sites/default/files/publication/99798/rapid_growth_in_medicaid_spending_and_prescriptions_to_treat_opioid_use_disorder_and_opioid_overdose_from_2010_to_2017_2.pdf ↩︎
- Lisa Clemans-Cope, Victoria Lynch, Marni Epstein, and Genevieve Kenney, Medicaid Coverage of Effective Treatment for Opioid Use Disorder, (Washington, DC: The Urban Institute, June 2017), https://www.urban.org/sites/default/files/publication/90461/2001287_medicaid_coverage_of_effective_treatment_for_opioid_use_disorder.pdf ↩︎
- Angelica Meinhofer and Allison Witman, “The Role Of Health Insurance On Treatment For Opioid Use Disorders: Evidence From The Affordable Care Act Medicaid Expansion,” Journal of Health Economics 60 (June 2018): 177-197, https://www.sciencedirect.com/science/article/abs/pii/S0167629617311530 ↩︎
- Johanna Maclean and Brendan Saloner, “The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act,” Journal of Policy Analysis and Management 38, no. 2 (2019): 366-393, https://www.ncbi.nlm.nih.gov/pubmed/30882195 ↩︎
- Hefei Wen, Jason Hockenberry, Tyrone Borders, and Benjamin Druss, “Impact of Medicaid Expansion on Medicaid-covered Utilization of Buprenorphine for Opioid Use Disorder Treatment,” Medical Care 55 no. 4 (April 2017): 336-341, http://journals.lww.com/lww-medicalcare/Fulltext/2017/04000/Impact_of_Medicaid_Expansion_on_Medicaid_covered.5.aspx ↩︎
- Brendan Saloner, Rachel Landis, Bradley Stein, and Colleen Barry, “The Affordable Care Act in the Heart of the Opioid Crisis: Evidence from West Virginia,” Health Affairs 38, no. 4 (April 2019), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05049 ↩︎
- Emanuel Eguia et al., “Impact of the Affordable Care Act (ACA) Medicaid Expansion on Cancer Admissions and Surgeries,” Annals of Surgery 268, no. 4 (October 2018): 584-590, https://journals.lww.com/annalsofsurgery/Abstract/2018/10000/Impact_of_the_Affordable_Care_Act__ACA__Medicaid.6.aspx ↩︎
- A. Taylor Kelley, Renuka Tipirneni, and Helen Levy, “Changes in Veterans’ Coverage and Access to Care Following the Affordable Care Act, 2011-2017,” American Journal of Public Health 109, no. 9 (September 2019): 1233-1235, https://doi.org/10.2105/ajph.2019.305160 ↩︎
- Kevin Griffith, Leigh Evans, and Jacob Bor, “The Affordable Care Act Reduced Socioeconomic Disparities in Health Care Access,” Health Affairs 36 no. 8 (August 2017), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0083 ↩︎
- Kelsie M. Gould et al., “Bariatric Surgery Among Vulnerable Populations: The Effect of the Affordable Care Act’s Medicaid Expansion,” Surgery 166, no. 5 (November 2019): 820-828, https://doi.org/10.1016/j.surg.2019.05.005 ↩︎
- Shiho Kino and Ichiro Kawachi, “The Impact Of ACA Medicaid Expansion On Socioeconomic Inequality In Health Care Services Utilization,” PLoS ONE 13, no. 2 (December 2018), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0209935 ↩︎
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562 ↩︎
- Susan Hayes, Pamela Riley, David Radley, and Douglas McCarthy, Reducing Racial and Ethnic Disparities in Access to Care: Has the Affordable Care Act Made a Difference? (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/racial-ethnic-disparities-care ↩︎
- Cheryl Zogg et al., “Impact of Affordable Care Act Insurance Expansion on Pre-Hospital Access to Care: Changes in Adult Perforated Appendix Admission Rates after Medicaid Expansion and the Dependent Coverage Provision,” Journal of the American College of Surgeons 228, no. 1 (January 2019): 29-43, https://www.journalacs.org/article/S1072-7515(18)32078-7/fulltext ↩︎
- Hiroshi Gotanda, Gerald Kominski, and Yusuke Tsugawa, “Association Between the ACA Medicaid Expansions and Primary Care and Emergency Department Use During the First 3 Years,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05458-w ↩︎
- Alexander T. Janke, Shooshan Danagoulian, Arjun K. Venkatesh, and Phillip D. Levy, “Medicaid Expansion and Resource Utilization in the Emergency Department,” The American Journal of Emergency Medicine Epub ahead of print (January 2020), https://doi.org/10.1016/j.ajem.2019.12.050 ↩︎
- Hawazin W. Elani, Ichiro Kawachi, and Benjamin D. Sommers, “Changes in Emergency Department Dental Visits after Medicaid Expansion,” Health Services Research Epub ahead of print (January 2020), https://doi.org/10.1111/1475-6773.13261 ↩︎
- Craig Garthwaite et al., All Medicaid Expansions Are Not Created Equal: The Geography and Targeting of the Affordable Care Act (National Bureau of Economic Research, Working Paper No. 26289, September 2019), http://www.nber.org/papers/w26289 ↩︎
- Eili Klein et al., “The Effect of Medicaid Expansion on Utilization in Maryland Emergency Departments,” Annals of Emergency Medicine epub ahead of print (June 2017), http://www.annemergmed.com/article/S0196-0644(17)30784-9/pdf ↩︎
- Heather Holderness et al., “Where Do Oregon Medicaid Enrollees Seek Outpatient Care Post-Affordable Care Act Medicaid Expansion?,” Medical Care 57, no. 10 (October 2019): 788-794, https://doi.org/10.1097/mlr.0000000000001189 ↩︎
- Aabha Sharma, Scott Dresden, Emilie Powell, Raymond Kang, Joe Feinglass, “Emergency Department Visits and Hospitalizations for the Uninsured in Illinois Before and After Affordable Care Act Insurance Expansion,” Journal of Community Health 42 no. 3 (June 2017): 591-597, https://link.springer.com/article/10.1007/s10900-016-0293-4 ↩︎
- Rahul Ladhania, Amelia Haviland, Arvind Venkat, Rahul Telang, and Jesse Pines, “The Effect of Medicaid Expansion on the Nature of New Enrollees’ Emergency Department Use,” Medical Care Research and Review epub ahead of print (May 2019), https://journals.sagepub.com/doi/abs/10.1177/1077558719848270 ↩︎
- Gary Pickens et al., “Changes In Hospital Service Demand, Cost, And Patient Illness Severity Following Health Reform,” Health Services Research (May 2019), https://doi.org/10.1111/1475-6773.13165 ↩︎
- Mark Duggan, Atul Gupta, and Emilie Jackson, The Impact of the Affordable Care Act: Evidence from California’s Hospital Sector (National Bureau of Economic Research, working paper no. 25488, January 2019), https://www.nber.org/papers/w25488.pdf ↩︎
- Jesse M. Pines, Mark Zocchi, Ali Moghtaderi, Bernard Black, Steven A. Farmer, Greg Hufstetler, Kevin Klauer and Randy Pilgrim, “Medicaid Expansion In 2014 Did Not Increase Emergency Department Use But Did Change Insurance Payer Mix,” Health Affairs 35, no. 8 (August 2016), http://content.healthaffairs.org/content/35/8/1480.full ↩︎
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293 ↩︎
- Stacey McMorrow, Jason Gates, Sharon Long, and Genevieve Kenney, “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents,” Health Affairs 36 no. 5 (May 2017): 808-818, https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650 ↩︎
- Manatt Health, Medicaid Expansion: How It Affects Montana’s State Budget, Economy, and Residents (Manatt Health, prepared for the Montana Healthcare Foundation, June 2018), https://mthcf.org/wp-content/uploads/2018/06/Manatt-MedEx_FINAL_6.1.18.pdf ↩︎
- Shannon McConville, Maria Raven, Sarah Sabbagh, and Renee Hsia, “Frequent Emergency Department Users: A Statewide Comparison Before And After Affordable Care Act Implementation,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0784 ↩︎
- Daniel Gingold, Rachelle Pierre-Mathieu, Brandon Cole, Andrew Miller, and Joneigh Khaldun, “Impact of the Affordable Care Act Medicaid Expansion on Emergency Department High Utilizers with Ambulatory Care Sensitive Conditions: A Cross-Sectional Study,” The American Journal of Emergency Medicine (January 2017), http://www.sciencedirect.com/science/article/pii/S0735675717300141 ↩︎
- Benjamin Sommers, Robert Blendon, E. John Orav, Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420 ↩︎
- Paul Jacobs, Genevieve Kenney, and Thomas Selden, “Newly Eligible Enrollees In Medicaid Spend Less And Use Less Care Than Those Previously Eligible,” Health Affairs 36, no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0252 ↩︎
- Elizabeth A. Brown et al., “The Impact of the ACA Medicaid Expansion on Access to Care and Hospitalization Charges for Lupus Patients,” Arthritis Care & Research Epub ahead of print (September 2019), https://doi.org/10.1002/acr.24080 ↩︎
- Charles A. Daly et al., “The Effects of Medicaid Expansion on Triage and Regional Transfer After Upper-Extremity Trauma,” The Journal of Hand Surgery 44, no. 9 (September 2019): 720-727, https://doi.org/10.1016/j.jhsa.2019.05.020 ↩︎
- Craig Garthwaite et al., All Medicaid Expansions Are Not Created Equal: The Geography and Targeting of the Affordable Care Act (National Bureau of Economic Research, Working Paper No. 26289, September 2019), http://www.nber.org/papers/w26289 ↩︎
- Natalia Chalmers, Jane Grover, and Rob Compton, “After Medicaid Expansion in Kentucky, Use of Hospital Emergency Departments for Dental Conditions Increased,” Health Affairs 35, no. 12 (December 2016), http://content.healthaffairs.org/content/35/12/2268.full#xref-ref-32-1 ↩︎
- Benjamin Sommers, Carrie Fry, Robert Blendon, and Arnold Epstein, “New Approaches in Medicaid: Work Requirements, Health Savings Accounts, and Health Care Access,” Health Affairs 37, no. 7 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2018.0331 ↩︎
- MaryBeth Musumeci, Robin Rudowitz, Petry Ubri, and Elizabeth Hinton, An Early Look at Medicaid Expansion Waiver Implementation in Michigan and Indiana (Washington, DC: The Kaiser Family Foundation, January 2017), http://kff.org/medicaid/issue-brief/an-early-look-at-medicaid-expansion-waiver-implementation-in-michigan-and-indiana/ ↩︎
- Natoshia Askelson, Brad Wright, Suzanne Bentler, Elizabeth Momany, and Peter Damiano, “Iowa’s Medicaid Expansion Promoted Healthy Behaviors But Was Challenging to Implement and Attracted Few Participants,” Health Affairs 36 no. 5, (May 2017): 799-807, http://content.healthaffairs.org/content/36/5/799.full ↩︎
- The Lewin Group, Indiana Healthy Indiana Plan 2.0: Interim Evaluation Report (The Lewin Group, Prepared for Indiana Family and Social Services Administration, July 2016), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-interim-evl-rpt-07062016.pdf ↩︎
- The Lewin Group, Healthy Indiana Plan 2.0: POWER Account Contribution Assessment, (The Lewin Group, prepared for the Indiana Family and Social Services Administration, March 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-POWER-acct-cont-assesmnt-03312017.pdf ↩︎
- Brad Wright et al., “Completion of Requirements in Iowa’s Medicaid Expansion Premium Disincentive Program, 2014–2015,” American Journal of Public Health 108, no. 2 (February 2018): 219-223, http://ajph.aphapublications.org/doi/full/10.2105/AJPH.2017.304178 ↩︎
- Emily Zylla, Colin Planalp, Elizabeth Lukanen, and Lynn Blewett, Section 1115 Medicaid Expansion Waivers: Implementation Experiences, (Medicaid and CHIP Payment and Access Commission, February 2018), https://www.macpac.gov/publication/section-1115-medicaid-expansion-waivers-implementation-experiences/ ↩︎
- Shiho Kino and Ichiro Kawachi, “Can Health Literacy Boost Health Services Utilization in the Context of Expanded Access to Health Insurance?,” Health Education & Behavior Epub ahead of print (October 2019), https://doi.org/10.1177/1090198119875998 ↩︎
- Helmneh M. Sineshaw et al., “Association of Medicaid Expansion Under the Affordable Care Act With Stage at Diagnosis and Time to Treatment Initiation for Patients With Head and Neck Squamous Cell Carcinoma,” JAMA Otolaryngology–Head & Neck Surgery Epub ahead of print (January 2020), https://doi.org/10.1001/jamaoto.2019.4310 ↩︎
- Emanuel Eguia et al., “The Impact of the Affordable Care Act Medicaid Expansion on Vascular Surgery,” Annals of Vascular Surgery Epub ahead of print (January 2020), https://doi.org/10.1016/j.avsg.2020.01.006 ↩︎
- Jesse C. Baumgartner, Sara R. Collins, David C. Radley, and Susan L. Hayes, How the Affordable Care Act Has Narrowed Racial and Ethnic Disparities in Access to Health Care (The Commonwealth Fund, January 2020), https://www.commonwealthfund.org/publications/2020/jan/how-ACA-narrowed-racial-ethnic-disparities-access ↩︎
- Dennis McCarty, Yifan Gu, John W. McIlveen, and Bonnie K. Lind, “Medicaid Expansion and Treatment for Opioid Use Disorders in Oregon: An Interrupted Time-Series Analysis,” Addiction Science & Clinical Practice 14 (August 2019), https://doi.org/10.1186/s13722-019-0160-6 ↩︎
- Anna L. Goldman and Benjamin D. Sommers, “Among Low-Income Adults Enrolled In Medicaid, Churning Decreased After The Affordable Care Act,” Health Affairs 39, no. 1 (January 2020): 85-93, https://doi.org/10.1377/hlthaff.2019.00378 ↩︎
- Emanuel Eguia et al., “The Impact of the Affordable Care Act (ACA) Medicaid Expansion on Access to Minimally Invasive Surgical Care,” The American Journal of Surgery Epub ahead of print (July 2019), https://doi.org/10.1016/j.amjsurg.2019.07.003 ↩︎
- Afshin Ehsan et al., “Utilization of Left Ventricular Assist Devices in Vulnerable Adults Across Medicaid Expansion,” Journal of Surgical Research 243 (November 2019): 503-508, https://doi.org/10.1016/j.jss.2019.05.015 ↩︎
- Kevin N. Griffith, “Changes in Insurance Coverage and Access to Care for Young Adults in 2017,” Journal of Adolescent Health Epub ahead of print (July 2019), https://doi.org/10.1016/j.jadohealth.2019.05.020 ↩︎
- Jin Huang and Shirley L. Porterfield, “Changes in Health Insurance Coverage and Health Care Access as Teens with Disabilities Transition to Adulthood,” Disability and Health Journal 12, no. 4 (October 2019): 551-556, https://doi.org/10.1016/j.dhjo.2019.06.009 ↩︎
- Kelsie M. Gould et al., “Bariatric Surgery Among Vulnerable Populations: The Effect of the Affordable Care Act’s Medicaid Expansion,” Surgery 166, no. 5 (November 2019): 820-828, https://doi.org/10.1016/j.surg.2019.05.005 ↩︎
- Michael McCue, “The Impact of Medicaid Expansion on Medicaid Focused Insurers in California,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 52 (July 2015), http://inq.sagepub.com/content/52/0046958015595960.full.pdf+html ↩︎
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553 ↩︎
- Jacqueline Fiore, The Impact of the Affordable Care Act’s Medicaid Expansion on Medicaid Spending by Health Care Service Category (Tulane University, July 2017), http://econ.tulane.edu/RePEc/pdf/tul1706.pdf ↩︎
- Emily Johnston, Andrea Strahan, Peter Joski, Anne Dunlop, and E. Kathleen Adams, “Impacts of the Affordable Care Act’s Medicaid Expansion on Women of Reproductive Age,” Women’s Health Issues, 28, no. 2 (February 2018), http://www.whijournal.com/article/S1049-3867(17)30242-6/pdf ↩︎
- Claire E. Margerison et al., “Impacts of Medicaid Expansion on Health Among Women of Reproductive Age,” American Journal of Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.amepre.2019.08.019 ↩︎
- Elham Mahmoudi, Alicia Cohen, Jason Buxbaum, Caroline Richardson, and Wassim Tarraf, “Gaining Medicaid Coverage During ACA Implementation: Effects on Access to Care and Preventive Services,” Journal of Health Care for the Poor and Underserved 29, no. 4 (November 2018): 1472-1487, https://muse.jhu.edu/article/708253 ↩︎
- Stacey McMorrow, Jason Gates, Sharon Long, and Genevieve Kenney, “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents,” Health Affairs 36 no. 5 (May 2017): 808-818, https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650 ↩︎
- Haley Moss, Laura Havrilesky, and Junzo Chino, “Insurance Coverage Among Women Diagnosed with a Gynecologic Malignancy Before and After Implementation of the Affordable Care Act,” Gynecologic Oncology 146, no. 3 (September 2017), https://www.ncbi.nlm.nih.gov/pubmed/28641821 ↩︎
- Susannah Gibbs et al., “Evaluating the Effect of Medicaid Expansion on Access to Preventive Reproductive Care for Women in Oregon,” Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.ypmed.2019.105899 ↩︎
- Nadia Laniado, Avery R. Brow, Eric Tranby, and Victor M. Badner, “Trends in Non-Traumatic Dental Emergency Department Use in New York and New Jersey: A Look at Medicaid Expansion from Both Sides of the Hudson River,” Journal of Public Health Dentistry Epub ahead of print (October 2019), https://doi.org/10.1111/jphd.12343 ↩︎
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830 ↩︎
- Dahai Yue, Petra Rasmussen, and Ninez Ponce, “Racial/Ethnic Differential Effects of Medicaid Expansion on Health Care Access,” Health Services Research (February 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12834/abstract ↩︎
- Mark Clapp et al., “Association of Medicaid Expansion With Coverage and Access to Care for Pregnant Women,” Obstetrics & Gynecology 134, no. 5 (November 2019): 1066-1074, https://doi.org/10.1097/aog.0000000000003501 ↩︎
- Charles A. Daly et al., “The Effects of Medicaid Expansion on Triage and Regional Transfer After Upper-Extremity Trauma,” The Journal of Hand Surgery 44, no. 9 (September 2019): 720-727, https://doi.org/10.1016/j.jhsa.2019.05.020 ↩︎
- Yunwei Gai and John Marthinsen, “Medicaid Expansion, HIV Testing, and HIV-Related Risk Behaviors in the United States, 2010-2017,” American Journal of Public Health 109, no. 10 (October 2019): 1404-1412, https://doi.org/10.2105/ajph.2019.305220 ↩︎
- Huabin Luo, Zhuo Chen, Lei Xu, and Ronny Bell, “Health Care Access and Receipt of Clinical Diabetes Preventive Care for Working-Age Adults With Diabetes in States With and Without Medicaid Expansion: Results from the 2013 and 2015 BRFSS,” Journal of Public Health Management and Practice 25, no. 4 (July/August 2019): 34-43, https://doi.org/10.1097/phh.0000000000000832 ↩︎
- A. Taylor Kelley, Renuka Tipirneni, and Helen Levy, “Changes in Veterans’ Coverage and Access to Care Following the Affordable Care Act, 2011-2017,” American Journal of Public Health 109, no. 9 (September 2019): 1233-1235, https://doi.org/10.2105/ajph.2019.305160 ↩︎
- J. Travis Donahoe et al., “The Affordable Care Act Medicaid Expansion and Smoking Cessation Among Low-Income Smokers,” American Journal of Preventive Medicine 57, no. 6 (December 2019): 203-210, https://doi.org/10.1016/j.amepre.2019.07.004 ↩︎
- Hiroshi Gotanda, Gerald Kominski, and Yusuke Tsugawa, “Association Between the ACA Medicaid Expansions and Primary Care and Emergency Department Use During the First 3 Years,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05458-w ↩︎
- Evan M. Chen et al., “Association of the Affordable Care Act Medicaid Expansion with Dilated Eye Examinations among the United States Population with Diabetes,” Ophthalmology Epub ahead of print (September 2019), https://doi.org/10.1016/j.ophtha.2019.09.010 ↩︎
- Mark L. Diana et al., Louisiana Medicaid Expansion and Access to Care (Louisiana Department of Health, Prepared by Tulane University, July 2019), http://ldh.la.gov/assets/media/AccesstoCareReport20132018final.pdf ↩︎
- Ann-Marie Rosland et al., “Diagnosis and Care of Chronic Health Conditions Among Medicaid Expansion Enrollees: a Mixed-Methods Observational Study,” Journal of General Internal Medicine 34, no. 11 (November 2019): 2549-2558, https://doi.org/10.1007/s11606-019-05323-w ↩︎
- Chelsea L. Shover et al., “The Relationship of Medicaid Expansion to Psychiatric Comorbidity Care within Substance Use Disorder Treatment Programs,” Journal of Substance Abuse Treatment 105 (October 2019): 44-50, https://doi.org/10.1016/j.jsat.2019.07.012 ↩︎
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890 ↩︎
- Laura Wherry and Sarah Miller, “Early Coverage, Access, Utilization, and Health Effects Associated with the Affordable Care Act Medicaid Expansions: A Quasi-experimental Study,” Annals of Internal Medicine, Epub ahead of print (April 2016), http://annals.org/article.aspx?articleid=2513980 ↩︎
- Adele Shartzer, Sharon Long, and Nathaniel Anderson, “Access To Care and Affordability have Improved Following Affordable Care Act Implementation; Problems Remain,” Health Affairs (December 2015), http://content.healthaffairs.org/content/early/2015/12/14/hlthaff.2015.0755.full ↩︎
- Benjamin Sommers, Robert Blendon, and E. John Orav, “Both the ‘Private Option’ And Traditional Medicaid Expansions Improved Access To Care For Low-Income Adults,” Health Affairs 35, no. 1 (January 2016): 96-105, http://content.healthaffairs.org/content/35/1/96.abstract ↩︎
- Mark Olfson, Melanie Wall, Colleen Barry, Christine Mauro, and Ramin Mojtabai, “Impact Of Medicaid Expansion On Coverage And Treatment Of Low-Income Adults With Substance Use Disorders,” Health Affairs 37, no. 8 (August 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.0124 ↩︎
- Abeer Alharbi, M. Mahmud Khan, Ronnie Horner, Heather Brandt, and Cole Chapman, “Impact Of Medicaid Coverage Expansion Under The Affordable Care Act On Mammography And Pap Tests Utilization Among Low-Income Women,” PLOS One (April 2019), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0214886 ↩︎
- Jevay Grooms and Alberto Ortega, “Examining Medicaid Expansion and the Treatment of Substance Use Disorders,” American Economic Association Papers and Proceedings 109 (May 2019): 187-192, https://www.aeaweb.org/articles?id=10.1257/pandp.20191090 ↩︎
- Nathalie Huguet et al., “Cervical And Colorectal Cancer Screening Prevalence Before And After Affordable Care Act Medicaid Expansion,” Preventative Medicine (May 2019), https://doi.org/10.1016/j.ypmed.2019.05.003 ↩︎
- John Cawley, Aparna Soni, and Kosali Simon, “Third Year of Survey Data Shows Continuing Benefits of Medicaid Expansions for Low-Income Childless Adults in the U.S.,” Journal of General Internal Medicine 33, no. 9 (September 2018): 1495-1497, https://link.springer.com/article/10.1007%2Fs11606-018-4537-0 ↩︎
- Kosali Simon, Aparna Soni, and John Cawley, “The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions” Journal of Policy Analysis and Management 36, no. 2 (March 2017), https://onlinelibrary.wiley.com/doi/abs/10.1002/pam.21972 ↩︎
- Yasmin Zerhouni et al., “Effect of Medicaid Expansion on Colorectal Cancer Screening Rates,” Diseases of the Colon & Rectum 62, no. 1 (January 2019): 97-103, https://journals.lww.com/dcrjournal/Abstract/2019/01000/Effect_of_Medicaid_Expansion_on_Colorectal_Cancer.16.aspx ↩︎
- Carrie Fry and Benjamin Sommers, “Effect of Medicaid Expansion on Health Insurance Coverage and Access to Care Among Adults With Depression,” Psychiatric Services 69, no. 11 (November 2018), https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201800181 ↩︎
- Xuesong Han, Robin Yabroff, Elizabeth Ward, Otis Brawley, and Ahmedin Jemal, “Comparison of Insurance Status and Diagnosis Stage Among Patients With Newly Diagnosed Cancer Before vs After Implementation of the Patient Protection and Affordable Care Act,” JAMA Oncology 4, no. 12 (August 2018): 1713-1720, https://jamanetwork.com/journals/jamaoncology/article-abstract/2697226 ↩︎
- Michael Hendryx and Juhua Luo, “Increased Cancer Screening for Low-income Adults Under the Affordable Care Act Medicaid Expansion,” Medical Care 56, no. 11 (November 2018): 944-949, https://www.ingentaconnect.com/content/wk/mcar/2018/00000056/00000011/art00009 ↩︎
- Brandy Lipton, Sandra Decker, and Benjamin Sommers, “The Affordable Care Act Appears to Have Narrowed Racial and Ethnic Disparities in Insurance Coverage and Access to Care Among Young Adults” Medical Care Research and Review 76, no.1 (April 2017): 32–55, https://www.ncbi.nlm.nih.gov/pubmed/29148341 ↩︎
- Stacey Fedewa, K. Robin Yabroff, Robert Smith, Ann Goding Sauer, Xuesong Han, and Ahmedin Jemal, “Changes in Breast and Colorectal Cancer Screening After Medicaid Expansion Under the Affordable Care Act,” American Journal of Preventive Medicine epub ahead of print (May 2019), https://www.sciencedirect.com/science/article/pii/S0749379719301163 ↩︎
- Tong Gan et al., “Impact of the Affordable Care Act on Colorectal Cancer Screening, Incidence, and Survival in Kentucky,” Journal of the American College of Surgeons 228, no. 4 (April 2019): 342-353.e1, https://www.journalacs.org/article/S1072-7515(19)30046-8/fulltext ↩︎
- Dmitry Tumin et al., “Medicaid Participation among Liver Transplant Candidates after the Affordable Care Act Medicaid Expansion” Journal of the American College of Surgeons 225, no. 2 (August 2017): 173-180.e2, https://www.journalacs.org/article/S1072-7515(17)30454-4/fulltext ↩︎
- Christina Andrews et al., “Medicaid Coverage In Substance Use Disorder Treatment After The Affordable Care Act,” Journal of Substance Abuse Treatment epub ahead of print (April 2019), https://www.sciencedirect.com/science/article/pii/S0740547218305750 ↩︎
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562 ↩︎
- Shiho Kino and Ichiro Kawachi, “The Impact Of ACA Medicaid Expansion On Socioeconomic Inequality In Health Care Services Utilization,” PLoS ONE 13, no. 2 (December 2018), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0209935 ↩︎
- James McDermott et al., “Affordable Care Act’s Medicaid Expansion and Use of Regionalized Surgery at High-Volume Hospitals,” Journal of the American College of Surgeons 227, no. 5 (November 2018): 507-520.e9, https://www.journalacs.org/article/S1072-7515(18)31993-8/abstract ↩︎
- Andrew Crocker et al., “Expansion Coverage And Preferential Utilization Of Cancer Surgery Among Racial And Ethnic Minorities And Low-Income Groups,” Surgery epub ahead of print (June 2019), https://www.surgjournal.com/article/S0039-6060(19)30198-9/fulltext ↩︎
- Emanuel Eguia et al., “The Impact of the Affordable Care Act (ACA) Medicaid Expansion on Access to Minimally Invasive Surgical Care,” The American Journal of Surgery Epub ahead of print (July 2019), https://doi.org/10.1016/j.amjsurg.2019.07.003 ↩︎
- Taressa K. Fraze et al., “Prevalence of Screening for Food Insecurity, Housing Instability, Utility Needs, Transportation Needs, and Interpersonal Violence by US Physician Practices and Hospitals,” JAMA Network Open 2, no. 9 (September 2019), https://doi.org/10.1001/jamanetworkopen.2019.11514 ↩︎
- Kelsey L. Corrigan et al., “The Impact of the Patient Protection and Affordable Care Act on Insurance Coverage and Cancer-Directed Treatment in HIV-Infected Patients With Cancer in the United States,” Cancer (November 2019), https://doi.org/10.1002/cncr.32563 ↩︎
- Andrew Loehrer et al., “Association of the Affordable Care Act Medicaid Expansion with Access to and Quality of Care for Surgical Conditions,” Journal of the American Medical Association Surgery, epub ahead of print (January 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2670459?redirect=true ↩︎
- Megan Cole, Omar Galarraga, Ira Wilson, Brad Wright, and Amal Trivedi, “At Federally Funded Health Centers, Medicaid Expansion was Associated with Improved Quality of Care,” Health Affairs 36 no. 1 (January 2017): 40-48, http://content.healthaffairs.org/content/36/1/40.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19 ↩︎
- Megan Cole, Brad Wright, Ira Wilson, Omar Gallarraga, and Amal Trivedi, “Medicaid Expansion And Community Health Centers: Care Quality And Service Use Increased For Rural Patients” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1542 ↩︎
- Benjamin Sommers, Robert Blendon, E. John Orav, and Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420 ↩︎
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293 ↩︎
- Hefei Wen, Kenton J. Johnston, Lindsay Allen, and Teresa M. Waters, “Medicaid Expansion Associated With Reductions In Preventable Hospitalizations,” Health Affairs 38, no. 11 (November 2019): 1845-1849, https://doi.org/10.1377/hlthaff.2019.00483 ↩︎
- Mohammad Eslami et al., “Impact of Medicaid Expansion of the Affordable Care on the Outcomes of Lower Extremity Bypass for Patients With Peripheral Artery Disease in the Vascular Quality Initiative Database,” Annals of Surgery 270, no. 4 (October 2019): 647-655, https://doi.org/10.1097/sla.0000000000003521 ↩︎
- John Scott et al., “Lifting the Burden: State Medicaid Expansion Reduces Financial Risk for the Injured,” Journal of Trauma and Acute Care Surgery Epub ahead of print (September 2019), https://doi.org/10.1097/ta.0000000000002493 ↩︎
- Gary Pickens et al., “Changes in Hospital Inpatient Utilization Following Health Care Reform,” Health Services Research epub ahead of print (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28664983 ↩︎
- Jeremy Holzmacher et al., “Association of Expanded Medicaid Coverage with Hospital Length of Stay After Injury,” JAMA Surgery published online (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28658482 ↩︎
- Andrew Admon, Thomas Valley, John Ayanian, Theodore Iwashyna, Colin Cooke, and Renuka Tipirneni, “Trends in Hospital Utilization After Medicaid Expansion,” Medical Care 57, no. 4 (April 2019): 312-317, https://journals.lww.com/lww-medicalcare/Abstract/publishahead/Brief_Report__Trends_in_Hospital_Utilization_After.98489.aspx ↩︎
- Cheryl Zogg et al., “Association of Medicaid Expansion With Access to Rehabilitative Care in Adult Trauma Patients,” JAMA Surgery epub ahead of print (January 2019), https://jamanetwork.com/journals/jamasurgery/article-abstract/2719270?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamasurg.2018.5177 ↩︎
- Andrew Admon, Michael Sjoding, Sarah Lyon, John Ayanian, Theodore Iwashyna, and Colin Cooke, “Medicaid Expansion and Mechanical Ventilation in Asthma, Chronic Obstructive Pulmonary Disease, and Heart Failure,” Annals of the American Thoracic Society epub ahead of print (February 2019), https://www.atsjournals.org/doi/pdf/10.1513/AnnalsATS.201811-777OC ↩︎
- Neal Bhutiani, Brian Harbrecht, Charles Scoggins, and Matthew Bozeman, “Evaluating The Early Impact Of Medicaid Expansion On Trends In Diagnosis And Treatment Of Benign Gallbladder Disease In Kentucky,” The American Journal of Surgery (January 2019), https://www.americanjournalofsurgery.com/article/S0002-9610(18)30894-8/fulltext ↩︎
- Manzilat Akande Peter Minneci, Katherine Deans, Henry Xiang, and Jennifer Cooper, “Association of Medicaid Expansion Under the Affordable Care Act With Outcomes and Access to Rehabilitation in Young Adult Trauma Patients,” JAMA Surgery 153, no. 8 (August 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2682872?widget=personalizedcontent&previousarticle=2719270 ↩︎
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562 ↩︎
- Ramiro Manzano-Nunez et al., “Association of Medicaid Expansion Policy with Outcomes in Homeless Patients Requiring Emergency General Surgery,” World Journal of Surgery 43, no. 6 (June 2019): 1483-1489, https://link.springer.com/article/10.1007/s00268-019-04932-0 ↩︎
- De-Chih Lee, Leiyu Shi, and Hailun Liang, “Primary Care Utilization And Clinical Quality Performance: A Comparison Between Health Centres In Medicaid Expansion States And Non-Expansion States,” Journal of Health Services Research & Policy 24, no. 1 (January 2019): 19-24, https://journals.sagepub.com/doi/abs/10.1177/1355819618788592 ↩︎
- Jusung Lee et al., “The Impact of Medicaid Expansion on Diabetes Management,” Diabetes Care Epub ahead of print (October 2019), https://doi.org/10.2337/dc19-1173 ↩︎
- John A. Graves et al., “Medicaid Expansion Slowed Rates of Health Decline for Low-Income Adults in Southern States,” Health Affairs 39, no. 1 (January 2020): 67-76, https://doi.org/10.1377/hlthaff.2019.00929 ↩︎
- Renuka Tipirneni et al., “Association of Expanded Medicaid Coverage With Health and Job-Related Outcomes Among Enrollees With Behavioral Health Disorders,” Psychiatric Services Epub ahead of print (September 2019), https://doi.org/10.1176/appi.ps.201900179 ↩︎
- Susan Dorr Goold et al., “Primary Care, Health Promotion, and Disease Prevention with Michigan Medicaid Expansion,” Journal of General Internal Medicine Epub ahead of print (December 2019), https://doi.org/10.1007/s11606-019-05370-3 ↩︎
- Ann-Marie Rosland et al., “Diagnosis and Care of Chronic Health Conditions Among Medicaid Expansion Enrollees: a Mixed-Methods Observational Study,” Journal of General Internal Medicine 34, no. 11 (November 2019): 2549-2558, https://doi.org/10.1007/s11606-019-05323-w ↩︎
- Claire E. Margerison et al., “Impacts of Medicaid Expansion on Health Among Women of Reproductive Age,” American Journal of Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.amepre.2019.08.019 ↩︎
- Renuka Tipirneni et al., “Changes in Health and Ability to Work Among Medicaid Expansion Enrollees: a Mixed Methods Study,” Journal of General Internal Medicine 34, no. 2 (February 2019): 272-280, https://link.springer.com/article/10.1007/s11606-018-4736-8 ↩︎
- Hyunjung Lee and Frank Porell, “The Effect of the Affordable Care Act Medicaid Expansion on Disparities in Access to Care and Health Status,” Medical Care Research and Review epub ahead of print (October 2018), https://journals.sagepub.com/doi/abs/10.1177/1077558718808709?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=mcrd ↩︎
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293 ↩︎
- Benjamin Sommers, Robert Blendon, E. John Orav, and Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420 ↩︎
- Stacey McMorrow, Jason Gates, Sharon Long, and Genevieve Kenney, “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents,” Health Affairs 36 no. 5 (May 2017): 808-818, https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650 ↩︎
- John Cawley, Aparna Soni, and Kosali Simon, “Third Year of Survey Data Shows Continuing Benefits of Medicaid Expansions for Low-Income Childless Adults in the U.S.,” Journal of General Internal Medicine 33, no. 9 (September 2018): 1495-1497, https://link.springer.com/article/10.1007%2Fs11606-018-4537-0 ↩︎
- Barbara DiPietro, Samantha Artiga, and Alexandra Gates, Early Impacts of the Medicaid Expansion for the Homeless Population (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, November 2014), http://kff.org/uninsured/issue-brief/early-impacts-of-the-medicaid-expansion-for-the-homeless-population/ ↩︎
- Kosali Simon, Aparna Soni, and John Cawley, “The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions” Journal of Policy Analysis and Management 36, no. 2 (March 2017), https://onlinelibrary.wiley.com/doi/abs/10.1002/pam.21972 ↩︎
- Tyler Winkelman and Virginia Chang, “Medicaid Expansion, Mental Health, and Access to Care Among Childless Adults With and Without Chronic Conditions,” Journal of General Internal Medicine epub ahead of print (November 2017), https://www.ncbi.nlm.nih.gov/pubmed/29181792 ↩︎
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf ↩︎
- Susan Dorr Goold et al., “Primary Care Clinicians’ Views About the Impact of Medicaid Expansion in Michigan: A Mixed Methods Study,” Journal of General Internal Medicine 33, no. 8 (June 2018): 1307-1316, https://link.springer.com/article/10.1007/s11606-018-4487-6 ↩︎
- Tong Gan et al., “Impact of the Affordable Care Act on Colorectal Cancer Screening, Incidence, and Survival in Kentucky,” Journal of the American College of Surgeons 228, no. 4 (April 2019): 342-353.e1, https://www.journalacs.org/article/S1072-7515(19)30046-8/fulltext ↩︎
- Eric Charles et al., “Impact of Medicaid Expansion on Cardiac Surgery Volume and Outcomes,” The Annals of Thoracic Surgery (June 2017), http://www.annalsthoracicsurgery.org/article/S0003-4975(17)30552-0/pdf ↩︎
- Cheryl Zogg et al., “Impact of Affordable Care Act Insurance Expansion on Pre-Hospital Access to Care: Changes in Adult Perforated Appendix Admission Rates after Medicaid Expansion and the Dependent Coverage Provision,” Journal of the American College of Surgeons 228, no. 1 (January 2019): 29-43, https://www.journalacs.org/article/S1072-7515(18)32078-7/fulltext ↩︎
- Clare Brown et al., “Association of State Medicaid Expansion Status With Low Birth Weight and Preterm Birth” Journal of the American Medical Association 321, no. 16 (April 2019), https://jamanetwork.com/journals/jama/fullarticle/2731179 ↩︎
- Steffani Bailey et al., “Tobacco Cessation in Affordable Care Act Medicaid Expansion States Versus Non-expansion States,” Nicotine & Tobacco Research epub ahead of print (May 2019), https://academic.oup.com/ntr/advance-article-abstract/doi/10.1093/ntr/ntz087/5498071 ↩︎
- Jonathan Koma, Julie Donohue, Colleen Barry, Haiden Huskamp, and Marian Jarlenski, “Medicaid Coverage Expansions and Cigarette Smoking Cessation Among Low-Income Adults,” Medical Care 55, no. 12 (December 2017): 1023-1029, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5688008/ ↩︎
- Sarah Miller, Sean Altekruse, Norman Johnson, and Laura R. Wherry, Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data (National Bureau of Economic Research, Working Paper No. 26081, July 2019), http://www.nber.org/papers/w26081 ↩︎
- Nicole Kravitz-Wirtz et al., “Association of Medicaid Expansion With Opioid Overdose Mortality in the United States,” JAMA Network Open 3, no. 1 (January 2020), https://doi.org/10.1001/jamanetworkopen.2019.19066 ↩︎
- Chintan Bhatt and Consuelo Beck-Sague, “Medicaid Expansion and Infant Mortality in the United States,” American Journal of Public Health 108, no. 4 (April 2018): 565-567, https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2017.304218 ↩︎
- Sameed Ahmed Khatana et al., “Association of Medicaid Expansion With Cardiovascular Mortality,” JAMA Cardiology 4, no. 7 (July 2019): 671-679, https://doi.org/10.1001/jamacardio.2019.1651 ↩︎
- Shailender Swaminathan, Benjamin Sommers, Rebecca Thorsness, Rajnish Mehrotra, Yoojin Lee, and Amal Trivedi, “Association of Medicaid Expansion With 1-Year Mortality Among Patients With End-Stage Renal Disease,” Journal of the American Medical Association (JAMA) 320, no. 21 (December 2018): 2242-2250, https://jamanetwork.com/journals/jama/fullarticle/2710505?guestAccessKey=ea3a8641-320b-4afd-b96e-dc59fbd90b20&utm_source=TrendMD&utm_medium=cpc&utm_campaign=J_Am_Med_TrendMD_1&utm_content=olf&utm_term=102518 ↩︎
- Emanuel Eguia et al., “The Impact of the Affordable Care Act (ACA) Medicaid Expansion on Access to Minimally Invasive Surgical Care,” The American Journal of Surgery Epub ahead of print (July 2019), https://doi.org/10.1016/j.amjsurg.2019.07.003 ↩︎
- Taressa K. Fraze et al., “Prevalence of Screening for Food Insecurity, Housing Instability, Utility Needs, Transportation Needs, and Interpersonal Violence by US Physician Practices and Hospitals,” JAMA Network Open 2, no. 9 (September 2019), https://doi.org/10.1001/jamanetworkopen.2019.11514 ↩︎
- Kelsey L. Corrigan et al., “The Impact of the Patient Protection and Affordable Care Act on Insurance Coverage and Cancer-Directed Treatment in HIV-Infected Patients With Cancer in the United States,” Cancer (November 2019), https://doi.org/10.1002/cncr.32563 ↩︎
- Mohammad Eslami et al., “Impact of Medicaid Expansion of the Affordable Care on the Outcomes of Lower Extremity Bypass for Patients With Peripheral Artery Disease in the Vascular Quality Initiative Database,” Annals of Surgery 270, no. 4 (October 2019): 647-655, https://doi.org/10.1097/sla.0000000000003521 ↩︎
- Megan Cole, Brad Wright, Ira Wilson, Omar Gallarraga, and Amal Trivedi, “Medicaid Expansion And Community Health Centers: Care Quality And Service Use Increased For Rural Patients” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1542 ↩︎
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293 ↩︎
- Rishi Wadhera et al., “Association of the Affordable Care Act’s Medicaid Expansion With Care Quality and Outcomes for Low-Income Patients Hospitalized With Heart Failure,” Circulation: Cardiovascular Quality and Outcomes 11, no. 7 (June 2018), https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.118.004729 ↩︎
- Rishi Wadhera et al., “Association of State Medicaid Expansion With Quality of Care and Outcomes for Low-Income Patients Hospitalized With Acute Myocardial Infarction,” JAMA Cardiology 4, no. 2 (January 2019): 120-127, https://jamanetwork.com/journals/jamacardiology/article-abstract/2720425?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamacardio.2018.4577 ↩︎
- Chima Ndumele, William Schpero, and Amal Trivedi, “Medicaid Expansion and Health Plan Quality in Medicaid Managed Care,” Health Services Research 53, no. 4, Part II (August 2018), https://onlinelibrary.wiley.com/doi/abs/10.1111/1475-6773.12814 ↩︎
- Megan Cole, Omar Galarraga, Ira Wilson, Brad Wright, and Amal Trivedi, “At Federally Funded Health Centers, Medicaid Expansion was Associated with Improved Quality of Care,” Health Affairs 36 no. 1 (January 2017): 40-48, http://content.healthaffairs.org/content/36/1/40.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19 ↩︎
- De-Chih Lee, Leiyu Shi, and Hailun Liang, “Primary Care Utilization And Clinical Quality Performance: A Comparison Between Health Centres In Medicaid Expansion States And Non-Expansion States,” Journal of Health Services Research & Policy 24, no. 1 (January 2019): 19-24, https://journals.sagepub.com/doi/abs/10.1177/1355819618788592 ↩︎
- John Scott et al., “Lifting the Burden: State Medicaid Expansion Reduces Financial Risk for the Injured,” Journal of Trauma and Acute Care Surgery Epub ahead of print (September 2019), https://doi.org/10.1097/ta.0000000000002493 ↩︎
- Gary Pickens et al., “Changes in Hospital Inpatient Utilization Following Health Care Reform,” Health Services Research epub ahead of print (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28664983 ↩︎
- Jeremy Holzmacher et al., “Association of Expanded Medicaid Coverage with Hospital Length of Stay After Injury,” JAMA Surgery published online (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28658482 ↩︎
- Mary Anderson, Jeffrey Glasheen, and Debra Anoff, “Impact of State Medicaid Expansion Status on Length of Stay and In-Hospital Mortality for General Medicine Patients at US Academic Medical Centers,” Journal of Hospital Medicine Epub ahead of print (August 2016), http://onlinelibrary.wiley.com/wol1/doi/10.1002/jhm.2649/citedby ↩︎
- Andrew Admon, Thomas Valley, John Ayanian, Theodore Iwashyna, Colin Cooke, and Renuka Tipirneni, “Trends in Hospital Utilization After Medicaid Expansion,” Medical Care 57, no. 4 (April 2019): 312-317, https://journals.lww.com/lww-medicalcare/Abstract/publishahead/Brief_Report__Trends_in_Hospital_Utilization_After.98489.aspx ↩︎
- Andrew Admon, Michael Sjoding, Sarah Lyon, John Ayanian, Theodore Iwashyna, and Colin Cooke, “Medicaid Expansion and Mechanical Ventilation in Asthma, Chronic Obstructive Pulmonary Disease, and Heart Failure,” Annals of the American Thoracic Society epub ahead of print (February 2019), https://www.atsjournals.org/doi/pdf/10.1513/AnnalsATS.201811-777OC ↩︎
- Ehimare Akhabue, Lindsay Pool, Clyde Yancy, Philip Greenland, and Donald Lloyd-Jones, “Association of State Medicaid Expansion With Rate of Uninsured Hospitalizations for Major Cardiovascular Events, 2009-2014,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2698077 ↩︎
- Donald Likosky, Devraj Sukul, Milan Seth, Chang He, Hitlander Gurm, and Richard Prager, “The Association Between Medicaid Expansion and Cardiovascular Interventions: The Michigan Experience,” Journal of the American College of Cardiology 71, no. 9 (March 2018): 1050-1051, https://www.sciencedirect.com/science/article/pii/S0735109718300056?via%3Dihub ↩︎
- Neal Bhutiani, Brian Harbrecht, Charles Scoggins, and Matthew Bozeman, “Evaluating The Early Impact Of Medicaid Expansion On Trends In Diagnosis And Treatment Of Benign Gallbladder Disease In Kentucky,” The American Journal of Surgery (January 2019), https://www.americanjournalofsurgery.com/article/S0002-9610(18)30894-8/fulltext ↩︎
- Rishi Wadhera et al., “Association of the Affordable Care Act’s Medicaid Expansion With Care Quality and Outcomes for Low-Income Patients Hospitalized With Heart Failure,” Circulation: Cardiovascular Quality and Outcomes 11, no. 7 (June 2018), https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.118.004729 ↩︎
- Rishi Wadhera et al., “Association of State Medicaid Expansion With Quality of Care and Outcomes for Low-Income Patients Hospitalized With Acute Myocardial Infarction,” JAMA Cardiology 4, no. 2 (January 2019): 120-127, https://jamanetwork.com/journals/jamacardiology/article-abstract/2720425?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamacardio.2018.4577 ↩︎
- Manzilat Akande Peter Minneci, Katherine Deans, Henry Xiang, and Jennifer Cooper, “Association of Medicaid Expansion Under the Affordable Care Act With Outcomes and Access to Rehabilitation in Young Adult Trauma Patients,” JAMA Surgery 153, no. 8 (August 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2682872?widget=personalizedcontent&previousarticle=2719270 ↩︎
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562 ↩︎
- Cheryl Zogg et al., “Association of Medicaid Expansion With Access to Rehabilitative Care in Adult Trauma Patients,” JAMA Surgery epub ahead of print (January 2019), https://jamanetwork.com/journals/jamasurgery/article-abstract/2719270?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamasurg.2018.5177 ↩︎
- Ramiro Manzano-Nunez et al., “Association of Medicaid Expansion Policy with Outcomes in Homeless Patients Requiring Emergency General Surgery,” World Journal of Surgery 43, no. 6 (June 2019): 1483-1489, https://link.springer.com/article/10.1007/s00268-019-04932-0 ↩︎
- Mark Clapp et al., “Association of Medicaid Expansion With Coverage and Access to Care for Pregnant Women,” Obstetrics & Gynecology 134, no. 5 (November 2019): 1066-1074, https://doi.org/10.1097/aog.0000000000003501 ↩︎
- John A. Graves et al., “Medicaid Expansion Slowed Rates of Health Decline for Low-Income Adults in Southern States,” Health Affairs 39, no. 1 (January 2020): 67-76, https://doi.org/10.1377/hlthaff.2019.00929 ↩︎
- Nicole Kravitz-Wirtz et al., “Association of Medicaid Expansion With Opioid Overdose Mortality in the United States,” JAMA Network Open 3, no. 1 (January 2020), https://doi.org/10.1001/jamanetworkopen.2019.19066 ↩︎
- James A. Swartz and Susanny J. Beltran, “Prescription Opioid Availability and Opioid Overdose-Related Mortality Rates in Medicaid Expansion and Non-Expansion States,” Addiction 114, no. 11 (November 2019): 2016-2025, https://doi.org/10.1111/add.14741 ↩︎
- Jusung Lee et al., “The Impact of Medicaid Expansion on Diabetes Management,” Diabetes Care Epub ahead of print (October 2019), https://doi.org/10.2337/dc19-1173 ↩︎
- Yunwei Gai and John Marthinsen, “Medicaid Expansion, HIV Testing, and HIV-Related Risk Behaviors in the United States, 2010-2017,” American Journal of Public Health 109, no. 10 (October 2019): 1404-1412, https://doi.org/10.2105/ajph.2019.305220 ↩︎
- Lindsay C. Kobayashi, Onur Altindag, Yulya Truskinovsky, and Lisa F. Berkman, “Effects of the Affordable Care Act Medicaid Expansion on Subjective Well-Being in the US Adult Population, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1236-1242, https://doi.org/10.2105/ajph.2019.305164 ↩︎
- Ann-Marie Rosland et al., “Diagnosis and Care of Chronic Health Conditions Among Medicaid Expansion Enrollees: a Mixed-Methods Observational Study,” Journal of General Internal Medicine 34, no. 11 (November 2019): 2549-2558, https://doi.org/10.1007/s11606-019-05323-w ↩︎
- Claire E. Margerison et al., “Impacts of Medicaid Expansion on Health Among Women of Reproductive Age,” American Journal of Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.amepre.2019.08.019 ↩︎
- Sri Lekha Tummalapalli, Samuel Leonard, Michelle M. Estrella, and Salomeh Keyhani, “The Effect of Medicaid Expansion on Self-Reported Kidney Disease,” Clinical Journal of American Society of Nephrology 14, no. 8 (August 2019): 1238-1240, https://doi.org/10.2215/cjn.02310219 ↩︎
- Stacey McMorrow, Jason Gates, Sharon Long, and Genevieve Kenney, “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents,” Health Affairs 36 no. 5 (May 2017): 808-818, https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650 ↩︎
- Sarah Miller and Laura Wherry, “Four Years Later: Insurance Coverage and Access to Care Continue to Diverge between ACA Medicaid Expansion and Non-Expansion States,” American Economic Association Papers and Proceedings 109 (May 2019): 327-333, https://www.aeaweb.org/articles?id=10.1257/pandp.20191046 ↩︎
- Tyler Winkelman and Virginia Chang, “Medicaid Expansion, Mental Health, and Access to Care Among Childless Adults With and Without Chronic Conditions,” Journal of General Internal Medicine epub ahead of print (November 2017), https://www.ncbi.nlm.nih.gov/pubmed/29181792 ↩︎
- Laura Wherry and Sarah Miller, “Early Coverage, Access, Utilization, and Health Effects Associated with the Affordable Care Act Medicaid Expansions: A Quasi-experimental Study,” Annals of Internal Medicine, Epub ahead of print (April 2016), http://annals.org/article.aspx?articleid=2513980 ↩︎
- Benjamin Sommers, Munira Gunja, Kenneth Finegold, and Thomas Musco, “Changes in Self-Reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act,” The Journal of the American Medical Association 314 no. 4 (July 2015): 366-374, http://jama.jamanetwork.com/article.aspx?articleid=2411283&resultClick=3 ↩︎
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890 ↩︎
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, Early Effects of the Affordable Care Act on Health Care Access, Risky Health Behaviors, and Self-Assessed Health (National Bureau of Economic Research, Working Paper no. 23269, March 2017), http://www.nber.org/papers/w23269 ↩︎
- Manzilat Akande, Peter Minneci, Katherine Deans, Henry Xiang, Deena Chisolm, and Jennifer Cooper, “Effects Of Medicaid Expansion On Disparities In Trauma Care And Outcomes In Young Adults,” Journal of Surgical Research 228 (August 2018): 42-53, https://www.sciencedirect.com/science/article/pii/S0022480418301562 ↩︎
- Hyunjung Lee and Frank Porell, “The Effect of the Affordable Care Act Medicaid Expansion on Disparities in Access to Care and Health Status,” Medical Care Research and Review epub ahead of print (October 2018), https://journals.sagepub.com/doi/abs/10.1177/1077558718808709?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=mcrd ↩︎
- John Cawley, Aparna Soni, and Kosali Simon, “Third Year of Survey Data Shows Continuing Benefits of Medicaid Expansions for Low-Income Childless Adults in the U.S.,” Journal of General Internal Medicine 33, no. 9 (September 2018): 1495-1497, https://link.springer.com/article/10.1007%2Fs11606-018-4537-0 ↩︎
- Kosali Simon, Aparna Soni, and John Cawley, “The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions” Journal of Policy Analysis and Management 36, no. 2 (March 2017), https://onlinelibrary.wiley.com/doi/abs/10.1002/pam.21972 ↩︎
- Nimish Valvi, Neomi Vin-Raviv, and Tomi Akinyemiju, “Current Smoking and Quit-Attempts Among US Adults Following Medicaid Expansion,” Preventive Medicine Reports epub ahead of print (June 2019), https://www.sciencedirect.com/science/article/pii/S2211335519300981 ↩︎
- Bernard Black, Alex Hollingsworth, Leticia Nunes, and Kosali Simon, The Effect of Health Insurance on Mortality: Power Analysis and What We Can Learn from the Affordable Care Act Coverage Expansions, (National Bureau of Economic Research, Working Paper Series No. 25568, February 2019), https://www.nber.org/papers/w25568 ↩︎
- Susan L. Averett, Julie K. Smith, and Yang Wang, “Medicaid Expansion and Opioid Deaths,” Health Economics 28, no. 12 (December 2019): 1491-1496, https://doi.org/10.1002/hec.3945 ↩︎
- Johanna Maclean and Brendan Saloner, The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act (National Bureau of Economic Research Working Paper No. 23342, April 2017), http://www.nber.org/papers/w23342.pdf ↩︎
- Mark L. Diana et al., Louisiana Medicaid Expansion and Access to Care (Louisiana Department of Health, Prepared by Tulane University, July 2019), http://ldh.la.gov/assets/media/AccesstoCareReport20132018final.pdf ↩︎
- Fredric Blavin, Impact of the Affordable Care Act’s Medicaid Expansion on Medicare Enrollees’ Access to Physician Services (Washington, DC: The Urban Institute, August 2019), https://www.urban.org/research/publication/effect-affordable-care-act-medicare-enrollees-access-physician-services ↩︎
- Jesse M. Hinde et al., “Increasing Access to Opioid Use Disorder Treatment: Assessing State Policies and the Evidence Behind Them,” Journal of Studies on Alcohol and Drugs 80, no. 6 (November 2019): 693-697, https://doi.org/10.15288/jsad.2019.80.693 ↩︎
- Angelica Meinhofer and Allison Witman, “The Role Of Health Insurance On Treatment For Opioid Use Disorders: Evidence From The Affordable Care Act Medicaid Expansion,” Journal of Health Economics 60 (June 2018): 177-197, https://www.sciencedirect.com/science/article/abs/pii/S0167629617311530 ↩︎
- Samantha Artiga, Robin Rudowitz, Jennifer Tolbert, Julia Paradise, and Melissa Majerol, Findings from the Field: Medicaid Delivery Systems and Access to Care in Four States in Year Three of the ACA (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, September 2016), http://kff.org/medicaid/issue-brief/findings-from-the-field-medicaid-delivery-systems-and-access-to-care-in-four-states-in-year-three-of-the-aca/ ↩︎
- Simon Basseyn, Brendan Saloner, Genevieve Kenney, Douglas Wissoker, Daniel Polsky, and Karin Rhodes, Primary Care Appointment Availability for Medicaid Patients: Comparing Traditional and Premium Assistance Plans, (Penn Leonard Davis Institute of Health Economics, July 2016), http://ldi.upenn.edu/brief/primary-care-appointment-availability-medicaid-patients-comparing-traditional-and-premium ↩︎
- Rachel Garfield, Elizabeth Hinton, Elizabeth Cornachione, and Cornelia Hall, Medicaid Managed Care Plans and Access to Care: Results from the Kaiser Family Foundation 2017 Survey of Medicaid Managed Care Plans (Washington, DC: Kaiser Family Foundation, March 2018), https://modern.kff.org/medicaid/report/medicaid-managed-care-plans-and-access-to-care-results-from-the-kaiser-family-foundation-2017-survey-of-medicaid-managed-care-plans ↩︎
- Hannah Neprash, Anna Zink, Joshua Gray, and Katherine Hempstead, “Physicians’ Participation In Medicaid Increased Only Slightly Following Expansion” Health Affairs 37, no. 7 (July 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1085 ↩︎
- Susan Dorr Goold et al., “Primary Care Clinicians’ Views About the Impact of Medicaid Expansion in Michigan: A Mixed Methods Study,” Journal of General Internal Medicine 33, no. 8 (June 2018): 1307-1316, https://link.springer.com/article/10.1007/s11606-018-4487-6 ↩︎
- Sara Rosenbaum, Jennifer Tolbert, Jessica Sharac, Peter Shin, Rachel Gunsalus, and Julia Zur, Community Health Centers: Growing Importance in a Changing Health Care System (Washington, DC: Kaiser Family Foundation, March 2018), https://modern.kff.org/medicaid/issue-brief/community-health-centers-growing-importance-in-a-changing-health-care-system/ ↩︎
- Hefei Wen, Adam S. Wilk, and Benjamin G. Druss, “Medicaid Acceptance by Psychiatrists Before and After Medicaid Expansion,” JAMA Psychiatry epub ahead of print (June 2019), https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2735109?resultClick=1 ↩︎
- Molly Candon et al., Primary Care Appointment Availability and the ACA Insurance Expansions (Philadelphia, PA: University of Pennsylvania Leonard Davis Institute of Health Economics, March 2017), https://ldi.upenn.edu/brief/primary-care-appointment-availability-and-aca-insurance-expansions ↩︎
- Benjamin Sommers, Robert Blendon, E. John Orav, and Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420 ↩︎
- Xinxin Han, Quian Luo, and Leighton Ku, “Medicaid Expansion and Grant Funding Increases Helped Improve Community Health Center Capacity,” Health Affairs 36 no. 1 (January 2017): 49-56, http://content.healthaffairs.org/content/36/1/49.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19 ↩︎
- Nathalie Huguet et al., “Medicaid Expansion Produces Long-Term Impact on Insurance Coverage Rates in Community Health Centers,” Journal of Primary Care & Community Health epub ahead of print (May 2017), http://journals.sagepub.com/doi/full/10.1177/2150131917709403 ↩︎
- Josh Gray, Anna Zink, and Tony Dreyfus, Effects of the Affordable Care Act Through 2015, (athenaResearch and Robert Wood Johnson Foundation ACA View Report, March 2016), http://www.athenahealth.com/~/media/athenaweb/files/pdf/acaview_tracking_the_impact_of_health_care_reform ↩︎
- Josh Gray, Iyue Sung, and Stewart Richardson, Observations on the Affordable Care Act: 2014 (athenaResearch and Robert Wood Johnson Foundation ACA View Report, February 2015), http://www.athenahealth.com/~/media/athenaweb/files/pdf/acaview_year_end_2014.pdf ↩︎
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf ↩︎
- MaryBeth Musumeci, Robin Rudowitz, Petry Ubri, and Elizabeth Hinton, An Early Look at Medicaid Expansion Waiver Implementation in Michigan and Indiana (Washington, DC: The Kaiser Family Foundation, January 2017), http://kff.org/medicaid/issue-brief/an-early-look-at-medicaid-expansion-waiver-implementation-in-michigan-and-indiana/ ↩︎
- Samantha Artiga, Jennifer Tolbert, and Robin Rudowitz, Year Two of the ACA Coverage Expansions: On-the-Ground Experiences from Five States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/health-reform/issue-brief/year-two-of-the-aca-coverage-expansions-on-the-ground-experiences-from-five-states/ ↩︎
- Government Accountability Office, Behavioral Health: Options for Low-Income Adults to Receive Treatment in Selected States (Washington, DC: Government Accountability Office, June 2015), http://www.gao.gov/assets/680/670894.pdf ↩︎
- Samantha Artiga and Robin Rudowitz, How Have State Medicaid Expansion Decisions Affected the Experiences of Low-Income Adults? Perspectives from Ohio, Arkansas, and Missouri (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/medicaid/issue-brief/how-have-state-medicaid-expansion-decisions-affected-the-experiences-of-low-income-adults-perspectives-from-ohio-arkansas-and-missouri/ ↩︎
- Peter Shin, Jessica Sharac, Julia Zur, Sara Rosenbaum, and Julia Paradise, Health Center Patient Trends, Enrollment Activities, and Service Capacity: Recent Experience in Medicaid Expansion and Non-Expansion States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, December 2015), http://kff.org/medicaid/issue-brief/health-center-patient-trends-enrollment-activities-and-service-capacity-recent-experience-in-medicaid-expansion-and-non-expansion-states/ ↩︎
- Renuka Tipirneni et al., “Primary Care Appointment Availability and Nonphysician Providers One Year After Medicaid Expansion,” The American Journal of Managed Care 22 no. 6 (June 2016): 427-431, http://www.ajmc.com/journals/issue/2016/2016-vol22-n6/primary-care-appointment-availability-and-nonphysician-providers-one-year-after-medicaid-expansion ↩︎
- Sara Collins, Munira Gunja, Michelle Doty, and Sophie Beutel, Americans’ Experiences with ACA Marketplace and Medicaid Coverage: Access to Care and Satisfaction (The Commonwealth Fund, May 2016), http://www.commonwealthfund.org/publications/issue-briefs/2016/may/aca-tracking-survey-access-to-care-and-satisfaction ↩︎
- Renuka Tipirneni et al., “Primary Care Appointment Availability For New Medicaid Patients Increased After Medicaid Expansion In Michigan,” Health Affairs (July 2015), http://content.healthaffairs.org/content/early/2015/07/15/hlthaff.2014.1425.full ↩︎
- De-Chih Lee, Leiyu Shi, and Hailun Liang, “Primary Care Utilization And Clinical Quality Performance: A Comparison Between Health Centres In Medicaid Expansion States And Non-Expansion States,” Journal of Health Services Research & Policy 24, no. 1 (January 2019): 19-24, https://journals.sagepub.com/doi/abs/10.1177/1355819618788592 ↩︎
- Adam M. Almaguer et al., “Do Geographic Region, Medicaid Status, and Academic Affiliation Affect Access to Care Among Medicaid and Privately Insured Total Hip Arthroplasty Patients?,” Journal of Arthroplasty 34, no. 12 (December 2019): 2866-2871, https://doi.org/10.1016/j.arth.2019.07.030 ↩︎
- Colleen M. Carey, Sarah Miller, and Laura R. Wherry, The Impact of Insurance Expansions on the Already Insured: The Affordable Care Act and Medicare, (National Bureau of Economic Research, Working Paper Series No. 25153, October 2018), https://www.nber.org/papers/w25153 ↩︎
- Carrie Fry and Benjamin Sommers, “Effect of Medicaid Expansion on Health Insurance Coverage and Access to Care Among Adults With Depression,” Psychiatric Services 69, no. 11 (November 2018), https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201800181 ↩︎
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830 ↩︎
- Joseph Labrum et al., “Does Medicaid Insurance Confer Adequate Access to Adult Orthopaedic Care in the Era of the Patient Protection and Affordable Care Act?” Clinical Orthopaedics and Related Research 475 no. 6 (June 2017): 1527-1536, https://link.springer.com/article/10.1007%2Fs11999-017-5263-3 ↩︎
- Fredric Blavin, Impact of the Affordable Care Act’s Medicaid Expansion on Medicare Enrollees’ Access to Physician Services (Washington, DC: The Urban Institute, August 2019), https://www.urban.org/research/publication/effect-affordable-care-act-medicare-enrollees-access-physician-services ↩︎
- Renuka Tipirneni et al., “Primary Care Appointment Availability For New Medicaid Patients Increased After Medicaid Expansion In Michigan,” Health Affairs (July 2015), http://content.healthaffairs.org/content/early/2015/07/15/hlthaff.2014.1425.full ↩︎
- Jevay Grooms and Alberto Ortega, “Examining Medicaid Expansion and the Treatment of Substance Use Disorders,” American Economic Association Papers and Proceedings 109 (May 2019): 187-192, https://www.aeaweb.org/articles?id=10.1257/pandp.20191090 ↩︎
- Hefei Wen, Adam S. Wilk, and Benjamin G. Druss, “Medicaid Acceptance by Psychiatrists Before and After Medicaid Expansion,” JAMA Psychiatry epub ahead of print (June 2019), https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2735109?resultClick=1 ↩︎
- Nathalie Huguet et al., “Medicaid Expansion Produces Long-Term Impact on Insurance Coverage Rates in Community Health Centers,” Journal of Primary Care & Community Health epub ahead of print (May 2017), http://journals.sagepub.com/doi/full/10.1177/2150131917709403 ↩︎
- Megan Cole, Omar Galarraga, Ira Wilson, Brad Wright, and Amal Trivedi, “At Federally Funded Health Centers, Medicaid Expansion was Associated with Improved Quality of Care,” Health Affairs 36 no. 1 (January 2017): 40-48, http://content.healthaffairs.org/content/36/1/40.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19 ↩︎
- Renuka Tipirneni et al., “Primary Care Appointment Availability and Nonphysician Providers One Year After Medicaid Expansion,” The American Journal of Managed Care 22 no. 6 (June 2016): 427-431, http://www.ajmc.com/journals/issue/2016/2016-vol22-n6/primary-care-appointment-availability-and-nonphysician-providers-one-year-after-medicaid-expansion ↩︎
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293 ↩︎
- Hilary Barnes, Michael Richards, Matthew McHugh, and Grant Martsolf, “Rural And Nonrural Primary Care Physician Practices Increasingly Rely On Nurse Practitioners,” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1158 ↩︎
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890 ↩︎
- Jenny Nguyen, Nidharshan Anandasivam, Daniel Cooperman, Richard Pelker, and Daniel Wiznia, “Does Medicaid Insurance Provide Sufficient Access to Pediatric Orthopedic Care Under the Affordable Care Act?,” Global Pediatric Health epub ahead of print (February 2019), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6381430/ ↩︎
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293 ↩︎
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830 ↩︎
- Samantha Artiga, Robin Rudowitz, Jennifer Tolbert, Julia Paradise, and Melissa Majerol, Findings from the Field: Medicaid Delivery Systems and Access to Care in Four States in Year Three of the ACA (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, September 2016), http://kff.org/medicaid/issue-brief/findings-from-the-field-medicaid-delivery-systems-and-access-to-care-in-four-states-in-year-three-of-the-aca/ ↩︎
- MaryBeth Musumeci, Robin Rudowitz, Petry Ubri, and Elizabeth Hinton, An Early Look at Medicaid Expansion Waiver Implementation in Michigan and Indiana (Washington, DC: The Kaiser Family Foundation, January 2017), http://kff.org/medicaid/issue-brief/an-early-look-at-medicaid-expansion-waiver-implementation-in-michigan-and-indiana/ ↩︎
- Samantha Artiga, Jennifer Tolbert, and Robin Rudowitz, Year Two of the ACA Coverage Expansions: On-the-Ground Experiences from Five States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/health-reform/issue-brief/year-two-of-the-aca-coverage-expansions-on-the-ground-experiences-from-five-states/ ↩︎
- Government Accountability Office, Behavioral Health: Options for Low-Income Adults to Receive Treatment in Selected States (Washington, DC: Government Accountability Office, June 2015), http://www.gao.gov/assets/680/670894.pdf ↩︎
- Samantha Artiga and Robin Rudowitz, How Have State Medicaid Expansion Decisions Affected the Experiences of Low-Income Adults? Perspectives from Ohio, Arkansas, and Missouri (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/medicaid/issue-brief/how-have-state-medicaid-expansion-decisions-affected-the-experiences-of-low-income-adults-perspectives-from-ohio-arkansas-and-missouri/ ↩︎
- Peter Shin, Jessica Sharac, Julia Zur, Sara Rosenbaum, and Julia Paradise, Health Center Patient Trends, Enrollment Activities, and Service Capacity: Recent Experience in Medicaid Expansion and Non-Expansion States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, December 2015), http://kff.org/medicaid/issue-brief/health-center-patient-trends-enrollment-activities-and-service-capacity-recent-experience-in-medicaid-expansion-and-non-expansion-states/ ↩︎
- Renuka Tipirneni et al., “Primary Care Appointment Availability and Nonphysician Providers One Year After Medicaid Expansion,” The American Journal of Managed Care 22 no. 6 (June 2016): 427-431, http://www.ajmc.com/journals/issue/2016/2016-vol22-n6/primary-care-appointment-availability-and-nonphysician-providers-one-year-after-medicaid-expansion ↩︎
- Renuka Tipirneni et al., “Primary Care Appointment Availability For New Medicaid Patients Increased After Medicaid Expansion In Michigan,” Health Affairs (July 2015), http://content.healthaffairs.org/content/early/2015/07/15/hlthaff.2014.1425.full ↩︎
- John Scott et al., “Lifting the Burden: State Medicaid Expansion Reduces Financial Risk for the Injured,” Journal of Trauma and Acute Care Surgery Epub ahead of print (September 2019), https://doi.org/10.1097/ta.0000000000002493 ↩︎
- Jesse C. Baumgartner, Sara R. Collins, David C. Radley, and Susan L. Hayes, How the Affordable Care Act Has Narrowed Racial and Ethnic Disparities in Access to Health Care (The Commonwealth Fund, January 2020), https://www.commonwealthfund.org/publications/2020/jan/how-ACA-narrowed-racial-ethnic-disparities-access ↩︎
- Xuesong Han et al., “Changes in Noninsurance and Care Unaffordability Among Cancer Survivors Following the Affordable Care Act,” Journal of the National Cancer Institute Epub ahead of print (November 2019), https://doi.org/10.1093/jnci/djz218 ↩︎
- Lindsay C. Kobayashi, Onur Altindag, Yulya Truskinovsky, and Lisa F. Berkman, “Effects of the Affordable Care Act Medicaid Expansion on Subjective Well-Being in the US Adult Population, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1236-1242, https://doi.org/10.2105/ajph.2019.305164 ↩︎
- Kevin N. Griffith, “Changes in Insurance Coverage and Access to Care for Young Adults in 2017,” Journal of Adolescent Health Epub ahead of print (July 2019), https://doi.org/10.1016/j.jadohealth.2019.05.020 ↩︎
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553 ↩︎
- Jin Huang and Shirley L. Porterfield, “Changes in Health Insurance Coverage and Health Care Access as Teens with Disabilities Transition to Adulthood,” Disability and Health Journal 12, no. 4 (October 2019): 551-556, https://doi.org/10.1016/j.dhjo.2019.06.009 ↩︎
- Claire E. Margerison et al., “Impacts of Medicaid Expansion on Health Among Women of Reproductive Age,” American Journal of Preventive Medicine Epub ahead of print (November 2019), https://doi.org/10.1016/j.amepre.2019.08.019 ↩︎
- Kyle Caswell and Timothy Waidmann, The Affordable Care Act Medicaid Expansions and Personal Finance (Washington, DC: The Urban Institute, September 2017), https://www.urban.org/research/publication/affordable-care-act-medicaid-expansions-and-personal-finance ↩︎
- Stacey McMorrow, Genevieve Kenney, Sharon Long, and Jason Gates, “Marketplaces Helped Drive Coverage Gains in 2015; Affordability Problems Remained,” Health Affairs 35 no. 10 (October 2016): 1810-1815, http://content.healthaffairs.org/content/35/10/1810.full ↩︎
- Kenneth Brevoort, Daniel Grodzicki, and Martin Hackmann, Medicaid and Financial Health (National Bureau of Economic Research, Working Paper No. 24002, November 2017), http://www.nber.org/papers/w24002 ↩︎
- Charles Courtemanche, James Marton, Benjamin Ukert, Aaron Yelowitz, Daniela Zapata, Early Effects of the Affordable Care Act on Health Care Access, Risky Health Behaviors, and Self-Assessed Health (National Bureau of Economic Research, Working Paper no. 23269, March 2017), http://www.nber.org/papers/w23269 ↩︎
- Tyler Winkelman and Virginia Chang, “Medicaid Expansion, Mental Health, and Access to Care Among Childless Adults With and Without Chronic Conditions,” Journal of General Internal Medicine epub ahead of print (November 2017), https://www.ncbi.nlm.nih.gov/pubmed/29181792 ↩︎
- Dahai Yue, Petra Rasmussen, and Ninez Ponce, “Racial/Ethnic Differential Effects of Medicaid Expansion on Health Care Access,” Health Services Research (February 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12834/abstract ↩︎
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf ↩︎
- Stacey McMorrow, Jason Gates, Sharon Long, and Genevieve Kenney, “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents,” Health Affairs 36 no. 5 (May 2017): 808-818, https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650 ↩︎
- Sarah Miller, Luojia Hu, Robert Kaestner, Bhashkar Mazumder, and Ashley Wong, The ACA Medicaid Expansion in Michigan and Financial Health, (National Bureau of Economic Research, working paper no. 25053, September 2018), https://www.nber.org/papers/w25053.pdf ↩︎
- Shiho Kino and Ichiro Kawachi, “Can Health Literacy Boost Health Services Utilization in the Context of Expanded Access to Health Insurance?,” Health Education & Behavior Epub ahead of print (October 2019), https://doi.org/10.1177/1090198119875998 ↩︎
- Mark L. Diana et al., Louisiana Medicaid Expansion and Access to Care (Louisiana Department of Health, Prepared by Tulane University, July 2019), http://ldh.la.gov/assets/media/AccesstoCareReport20132018final.pdf ↩︎
- Ann-Marie Rosland et al., “Diagnosis and Care of Chronic Health Conditions Among Medicaid Expansion Enrollees: a Mixed-Methods Observational Study,” Journal of General Internal Medicine 34, no. 11 (November 2019): 2549-2558, https://doi.org/10.1007/s11606-019-05323-w ↩︎
- Carrie Fry and Benjamin Sommers, “Effect of Medicaid Expansion on Health Insurance Coverage and Access to Care Among Adults With Depression,” Psychiatric Services 69, no. 11 (November 2018), https://ps.psychiatryonline.org/doi/10.1176/appi.ps.201800181 ↩︎
- Hyunjung Lee and Frank Porell, “The Effect of the Affordable Care Act Medicaid Expansion on Disparities in Access to Care and Health Status,” Medical Care Research and Review epub ahead of print (October 2018), https://journals.sagepub.com/doi/abs/10.1177/1077558718808709?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=mcrd ↩︎
- Sarah Miller and Laura Wherry, “Four Years Later: Insurance Coverage and Access to Care Continue to Diverge between ACA Medicaid Expansion and Non-Expansion States,” American Economic Association Papers and Proceedings 109 (May 2019): 327-333, https://www.aeaweb.org/articles?id=10.1257/pandp.20191046 ↩︎
- Sunha Choi, Sungkyu Lee, and Jason Matejkowski, “The Effects of State Medicaid Expansion on Low-Income Individuals’ Access to Health Care: Multilevel Modeling,” Population Health Management epub ahead of print (September 2017), http://online.liebertpub.com/doi/abs/10.1089/pop.2017.0104 ↩︎
- Susan Hayes, Pamela Riley, David Radley, and Douglas McCarthy, Reducing Racial and Ethnic Disparities in Access to Care: Has the Affordable Care Act Made a Difference? (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/racial-ethnic-disparities-care ↩︎
- Susan Hayes, Sara Collins, David Radley, and Douglas McCarthy, What’s at Stake: States’ Progress on Health Coverage and Access to Care, 2013-2016 (The Commonwealth Fund, December 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/dec/states-progress-health-coverage-and-access ↩︎
- Emily Johnston, Andrea Strahan, Peter Joski, Anne Dunlop, and E. Kathleen Adams, “Impacts of the Affordable Care Act’s Medicaid Expansion on Women of Reproductive Age,” Women’s Health Issues, 28, no. 2 (February 2018), http://www.whijournal.com/article/S1049-3867(17)30242-6/pdf ↩︎
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830 ↩︎
- Kevin Griffith, Leigh Evans, and Jacob Bor, “The Affordable Care Act Reduced Socioeconomic Disparities in Health Care Access,” Health Affairs 36 no. 8 (August 2017), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0083 ↩︎
- Sharon Long, Lea Bart, Michael Karpman, Adele Shartzer, and Stephen Zuckerman, “Sustained Gains in Coverage, Access, and Affordability Under the ACA: A 2017 Update,” Health Affairs 36 no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0798 ↩︎
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293 ↩︎
- Bryce Ward and Brandon Bridge, The Economic Impact of Medicaid Expansion in Montana: Updated Findings (Bureau of Business and Economic Research, January 2019), https://mthcf.org/wp-content/uploads/2019/01/Economic-Impact-of-MedEx-in-MT_1.28.19-FINAL.pdf ↩︎
- Ameen Barghi, Hugo Torres, Nancy Kressin, and Danny McCormick, “Coverage and Access for Americans with Cardiovascular Disease or Risk Factors After the ACA: a Quasi-experimental Study,” Journal of General Internal Medicine epub ahead of print (June 2019), https://link.springer.com/article/10.1007%2Fs11606-019-05108-1 ↩︎
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890 ↩︎
- Sara Collins, Munira Gunja, Michelle Doty, and Sophie Beutel, Americans’ Experiences with ACA Marketplace and Medicaid Coverage: Access to Care and Satisfaction (The Commonwealth Fund, May 2016), http://www.commonwealthfund.org/publications/issue-briefs/2016/may/aca-tracking-survey-access-to-care-and-satisfaction ↩︎
- Joseph Benitez, Liza Creel, and J’Aime Jennings, “Kentucky’s Medicaid Expansion Showing Early Promise on Coverage and Access to Care,” Health Affairs (February 2016), http://content.healthaffairs.org/content/early/2016/02/16/hlthaff.2015.1294 ↩︎
- Benjamin Sommers, Robert Blendon, and E. John Orav, “Both the ‘Private Option’ And Traditional Medicaid Expansions Improved Access To Care For Low-Income Adults,” Health Affairs 35, no. 1 (January 2016): 96-105, http://content.healthaffairs.org/content/35/1/96.abstract ↩︎
- Samantha Artiga and Robin Rudowitz, How Have State Medicaid Expansion Decisions Affected the Experiences of Low-Income Adults? Perspectives from Ohio, Arkansas, and Missouri (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2015), http://kff.org/medicaid/issue-brief/how-have-state-medicaid-expansion-decisions-affected-the-experiences-of-low-income-adults-perspectives-from-ohio-arkansas-and-missouri/ ↩︎
- John Cawley, Aparna Soni, and Kosali Simon, “Third Year of Survey Data Shows Continuing Benefits of Medicaid Expansions for Low-Income Childless Adults in the U.S.,” Journal of General Internal Medicine 33, no. 9 (September 2018): 1495-1497, https://link.springer.com/article/10.1007%2Fs11606-018-4537-0 ↩︎
- Aaron Sojourner and Ezra Golberstein, “Medicaid Expansion Reduced Unpaid Medical Debt and Increased Financial Satisfaction,” Health Affairs (July 2017), https://www.healthaffairs.org/do/10.1377/hblog20170724.061160/full/ ↩︎
- Frederic Blavin, Michael Karpman, Genevieve Kenney, and Benjamin Sommers, “Medicaid Versus Marketplace Coverage for Near-Poor Adults: Effects on Out-Of-Pocket Spending and Coverage,” Health Affairs 37 no. 2 (January 2018), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.1166 ↩︎
- Sherry Glied, Ougni Chakraborty, and Therese Russo, How Medicaid Expansion Affected Out-of-Pocket Health Care Spending for Low-Income Families (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/medicaid-expansion-out-of-pocket-spending-low-income ↩︎
- Benjamin Sommers, Robert Blendon, E. John Orav, and Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420 ↩︎
- Andrew Mulcahy, Christine Eibner, and Kenneth Finegold, “Gaining Coverage Through Medicaid Or Private Insurance Increased Prescription Use and Lowered Out-Of-Pocket Spending,” Health Affairs 35, no. 9 (September 2016), http://content.healthaffairs.org/content/early/2016/08/16/hlthaff.2016.0091.full ↩︎
- Anna Goldman, Steffie Woolhandler, and David Himmelstein, “Out-of-pocket Spending and Premium Contributions After Implementation of the Affordable Care Act,” Journal of the American Medical Association epub ahead of print (January 2018), https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2669908 ↩︎
- Helen Levy, Thomas Buchmueller, and Sayeh Nikpay, “The Impact of Medicaid Expansion on Household Consumption,” Eastern Economic Journal 45, no. 1 (January 2019): 34-57, https://link.springer.com/article/10.1057/s41302-018-0124-7 ↩︎
- Sarah Miller and Laura Wherry, “Four Years Later: Insurance Coverage and Access to Care Continue to Diverge between ACA Medicaid Expansion and Non-Expansion States,” American Economic Association Papers and Proceedings 109 (May 2019): 327-333, https://www.aeaweb.org/articles?id=10.1257/pandp.20191046 ↩︎
- Kenneth Brevoort, Daniel Grodzicki, and Martin Hackmann, Medicaid and Financial Health (National Bureau of Economic Research, Working Paper No. 24002, November 2017), http://www.nber.org/papers/w24002 ↩︎
- Kyle Caswell and Timothy Waidmann, The Affordable Care Act Medicaid Expansions and Personal Finance (Washington, DC: The Urban Institute, September 2017), https://www.urban.org/research/publication/affordable-care-act-medicaid-expansions-and-personal-finance ↩︎
- Sharon Long, Lea Bart, Michael Karpman, Adele Shartzer, and Stephen Zuckerman, “Sustained Gains in Coverage, Access, and Affordability Under the ACA: A 2017 Update,” Health Affairs 36 no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0798 ↩︎
- Aaron Sojourner and Ezra Golberstein, “Medicaid Expansion Reduced Unpaid Medical Debt and Increased Financial Satisfaction,” Health Affairs (July 2017), https://www.healthaffairs.org/do/10.1377/hblog20170724.061160/full/ ↩︎
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830 ↩︎
- Benjamin Sommers, Bethany Maylone, Robert Blendon, E. John Orav, and Arnold Epstein, “Three-Year Impacts of the Affordable Care Act: Improved Medical Care and Health Among Low-Income Adults,” Health Affairs epub ahead of print (May 2017), http://content.healthaffairs.org/content/early/2017/05/15/hlthaff.2017.0293 ↩︎
- Stacey McMorrow, Jason Gates, Sharon Long, and Genevieve Kenney, “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents,” Health Affairs 36 no. 5 (May 2017): 808-818, https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650 ↩︎
- Benjamin Sommers, Robert Blendon, E. John Orav, and Arnold Epstein, “Changes in Utilization and Health Among Low-Income Adults After Medicaid Expansion or Expanded Private Insurance,” The Journal of the American Medical Association 176 no. 10 (October 2016): 1501-1509, http://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2542420 ↩︎
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890 ↩︎
- Sarah Miller, Luojia Hu, Robert Kaestner, Bhashkar Mazumder, and Ashley Wong, The ACA Medicaid Expansion in Michigan and Financial Health, (National Bureau of Economic Research, working paper no. 25053, September 2018), https://www.nber.org/papers/w25053.pdf ↩︎
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf ↩︎
- Sarah Miller, Luojia Hu, Robert Kaestner, Bhashkar Mazumder, and Ashley Wong, The ACA Medicaid Expansion in Michigan and Financial Health, (National Bureau of Economic Research, working paper no. 25053, September 2018), https://www.nber.org/papers/w25053.pdf ↩︎
- Gracie Himmelstein, “Effect of the Affordable Care Act’s Medicaid Expansions on Food Security, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1243-1248, https://doi.org/10.2105/ajph.2019.305168 ↩︎
- Sanders Korenman, Dahlia K. Remler, and Rosemary T. Hyson, “Medicaid Expansions and Poverty: Comparing Supplemental and Health-Inclusive Poverty Measures,” Social Service Review 93, no. 3 (September 2019): 429-483, https://doi.org/10.1086/705319 ↩︎
- Naomi Zewde and Christopher Wimer, “Antipoverty Impact Of Medicaid Growing With State Expansions Over Time,” Health Affairs 38, no. 1 (January 2019), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05155 ↩︎
- Kenneth Brevoort, Daniel Grodzicki, and Martin Hackmann, Medicaid and Financial Health (National Bureau of Economic Research, Working Paper No. 24002, November 2017), http://www.nber.org/papers/w24002 ↩︎
- Kyle Caswell and Timothy Waidmann, The Affordable Care Act Medicaid Expansions and Personal Finance (Washington, DC: The Urban Institute, September 2017), https://www.urban.org/research/publication/affordable-care-act-medicaid-expansions-and-personal-finance ↩︎
- Aaron Sojourner and Ezra Golberstein, “Medicaid Expansion Reduced Unpaid Medical Debt and Increased Financial Satisfaction,” Health Affairs (July 2017), https://www.healthaffairs.org/do/10.1377/hblog20170724.061160/full/ ↩︎
- Luojia Hu, Robert Kaestenr, Bhashkar Mazumder, Sarah Miller, and Ashley Wong, “The Effect of the Affordable Care Act Medicaid Expansions on Financial Wellbeing,” Journal of Public Economics 163 (July 2018): 99-112, https://www.sciencedirect.com/science/article/abs/pii/S0047272718300707 ↩︎
- Sarah Miller, Luojia Hu, Robert Kaestner, Bhashkar Mazumder, and Ashley Wong, The ACA Medicaid Expansion in Michigan and Financial Health, (National Bureau of Economic Research, working paper no. 25053, September 2018), https://www.nber.org/papers/w25053.pdf ↩︎
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf ↩︎
- Gracie Himmelstein, “Effect of the Affordable Care Act’s Medicaid Expansions on Food Security, 2010-2016,” American Journal of Public Health 109, no. 9 (September 2019): 1243-1248, https://doi.org/10.2105/ajph.2019.305168 ↩︎
- Naomi Zewde and Christopher Wimer, “Antipoverty Impact Of Medicaid Growing With State Expansions Over Time,” Health Affairs 38, no. 1 (January 2019), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2018.05155 ↩︎
- Sanders Korenman, Dahlia K. Remler, and Rosemary T. Hyson, “Medicaid Expansions and Poverty: Comparing Supplemental and Health-Inclusive Poverty Measures,” Social Service Review 93, no. 3 (September 2019): 429-483, https://doi.org/10.1086/705319 ↩︎
- Naomi Zewde, Erica Eliason, Heidi Allen, and Tal Gross, “The Effects of the ACA Medicaid Expansion on Nationwide Home Evictions and Eviction-Court Initiations: United States, 2000-2016,” American Journal of Public Health 109, no. 10 (October 2019): 1379-1383, https://doi.org/10.2105/ajph.2019.305230 ↩︎
- Sarah Miller, Luojia Hu, Robert Kaestner, Bhashkar Mazumder, and Ashley Wong, The ACA Medicaid Expansion in Michigan and Financial Health, (National Bureau of Economic Research, working paper no. 25053, September 2018), https://www.nber.org/papers/w25053.pdf ↩︎
- Luojia Hu, Robert Kaestenr, Bhashkar Mazumder, Sarah Miller, and Ashley Wong, “The Effect of the Affordable Care Act Medicaid Expansions on Financial Wellbeing,” Journal of Public Economics 163 (July 2018): 99-112, https://www.sciencedirect.com/science/article/abs/pii/S0047272718300707 ↩︎
- Kenneth Brevoort, Daniel Grodzicki, and Martin Hackmann, Medicaid and Financial Health (National Bureau of Economic Research, Working Paper No. 24002, November 2017), http://www.nber.org/papers/w24002 ↩︎
- Aaron Sojourner and Ezra Golberstein, “Medicaid Expansion Reduced Unpaid Medical Debt and Increased Financial Satisfaction,” Health Affairs (July 2017), https://www.healthaffairs.org/do/10.1377/hblog20170724.061160/full/ ↩︎
- Kyle Caswell and Timothy Waidmann, The Affordable Care Act Medicaid Expansions and Personal Finance (Washington, DC: The Urban Institute, September 2017), https://www.urban.org/research/publication/affordable-care-act-medicaid-expansions-and-personal-finance ↩︎
- Sarah Miller, Luojia Hu, Robert Kaestner, Bhashkar Mazumder, and Ashley Wong, The ACA Medicaid Expansion in Michigan and Financial Health, (National Bureau of Economic Research, working paper no. 25053, September 2018), https://www.nber.org/papers/w25053.pdf ↩︎
- Xuesong Han et al., “Changes in Noninsurance and Care Unaffordability Among Cancer Survivors Following the Affordable Care Act,” Journal of the National Cancer Institute Epub ahead of print (November 2019), https://doi.org/10.1093/jnci/djz218 ↩︎
- Kevin Griffith, Leigh Evans, and Jacob Bor, “The Affordable Care Act Reduced Socioeconomic Disparities in Health Care Access,” Health Affairs 36 no. 8 (August 2017), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0083 ↩︎
- Shiho Kino and Ichiro Kawachi, “The Impact Of ACA Medicaid Expansion On Socioeconomic Inequality In Health Care Services Utilization,” PLoS ONE 13, no. 2 (December 2018), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0209935 ↩︎
- Susan Hayes, Sara Collins, David Radley, and Douglas McCarthy, What’s at Stake: States’ Progress on Health Coverage and Access to Care, 2013-2016 (The Commonwealth Fund, December 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/dec/states-progress-health-coverage-and-access ↩︎
- Susan Hayes, Pamela Riley, David Radley, and Douglas McCarthy, Reducing Racial and Ethnic Disparities in Access to Care: Has the Affordable Care Act Made a Difference? (The Commonwealth Fund, August 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/aug/racial-ethnic-disparities-care ↩︎
- Aaron Sojourner and Ezra Golberstein, “Medicaid Expansion Reduced Unpaid Medical Debt and Increased Financial Satisfaction,” Health Affairs (July 2017), https://www.healthaffairs.org/do/10.1377/hblog20170724.061160/full/ ↩︎
- Naomi Zewde, Erica Eliason, Heidi Allen, and Tal Gross, “The Effects of the ACA Medicaid Expansion on Nationwide Home Evictions and Eviction-Court Initiations: United States, 2000-2016,” American Journal of Public Health 109, no. 10 (October 2019): 1379-1383, https://doi.org/10.2105/ajph.2019.305230 ↩︎
- Jesse C. Baumgartner, Sara R. Collins, David C. Radley, and Susan L. Hayes, How the Affordable Care Act Has Narrowed Racial and Ethnic Disparities in Access to Health Care (The Commonwealth Fund, January 2020), https://www.commonwealthfund.org/publications/2020/jan/how-ACA-narrowed-racial-ethnic-disparities-access ↩︎
- A. Taylor Kelley, Renuka Tipirneni, and Helen Levy, “Changes in Veterans’ Coverage and Access to Care Following the Affordable Care Act, 2011-2017,” American Journal of Public Health 109, no. 9 (September 2019): 1233-1235, https://doi.org/10.2105/ajph.2019.305160 ↩︎
- Xuesong Han et al., “Changes in Noninsurance and Care Unaffordability Among Cancer Survivors Following the Affordable Care Act,” Journal of the National Cancer Institute Epub ahead of print (November 2019), https://doi.org/10.1093/jnci/djz218 ↩︎
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553 ↩︎
- Kevin N. Griffith, “Changes in Insurance Coverage and Access to Care for Young Adults in 2017,” Journal of Adolescent Health Epub ahead of print (July 2019), https://doi.org/10.1016/j.jadohealth.2019.05.020 ↩︎
- Jin Huang and Shirley L. Porterfield, “Changes in Health Insurance Coverage and Health Care Access as Teens with Disabilities Transition to Adulthood,” Disability and Health Journal 12, no. 4 (October 2019): 551-556, https://doi.org/10.1016/j.dhjo.2019.06.009 ↩︎
- Sanders Korenman, Dahlia K. Remler, and Rosemary T. Hyson, “Medicaid Expansions and Poverty: Comparing Supplemental and Health-Inclusive Poverty Measures,” Social Service Review 93, no. 3 (September 2019): 429-483, https://doi.org/10.1086/705319 ↩︎
- Jean M. Abraham, Anne B. Royalty, and Coleman Drake, “The Impact of Medicaid Expansion on Employer Provision of Health Insurance,” International Journal of Health Economics and Management 19, no. 3-4 (December 2019): 317-340, https://doi.org/10.1007/s10754-018-9256-x ↩︎
- Thomas Selden, Brandy Lipton, and Sandra Decker, “Medicaid Expansion and Marketplace Eligibility Both Increased Coverage, With Trade-Offs in Access, Affordability,” Health Affairs 36 no. 12 (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0830 ↩︎
- Sarah Miller and Laura Wherry, “Health and Access to Care During the First 2 Years of the ACA Medicaid Expansions,” The New England Journal of Medicine 376 no. 10 (March 2017), http://www.nejm.org/doi/full/10.1056/NEJMsa1612890 ↩︎
- Joseph Benitez, Liza Creel, and J’Aime Jennings, “Kentucky’s Medicaid Expansion Showing Early Promise on Coverage and Access to Care,” Health Affairs (February 2016), http://content.healthaffairs.org/content/early/2016/02/16/hlthaff.2015.1294 ↩︎
- Laura Wherry and Sarah Miller, “Early Coverage, Access, Utilization, and Health Effects Associated with the Affordable Care Act Medicaid Expansions: A Quasi-experimental Study,” Annals of Internal Medicine, Epub ahead of print (April 2016), http://annals.org/article.aspx?articleid=2513980 ↩︎
- Adele Shartzer, Sharon Long, and Nathaniel Anderson, “Access To Care and Affordability have Improved Following Affordable Care Act Implementation; Problems Remain,” Health Affairs (December 2015), http://content.healthaffairs.org/content/early/2015/12/14/hlthaff.2015.0755.full ↩︎
- Benjamin Sommers, Munira Gunja, Kenneth Finegold, and Thomas Musco, “Changes in Self-Reported Insurance Coverage, Access to Care, and Health Under the Affordable Care Act,” The Journal of the American Medical Association 314 no. 4 (July 2015): 366-374, http://jama.jamanetwork.com/article.aspx?articleid=2411283&resultClick=3 ↩︎
- Kenneth Brevoort, Daniel Grodzicki, and Martin Hackmann, Medicaid and Financial Health (National Bureau of Economic Research, Working Paper No. 24002, November 2017), http://www.nber.org/papers/w24002 ↩︎
- Aaron Sojourner and Ezra Golberstein, “Medicaid Expansion Reduced Unpaid Medical Debt and Increased Financial Satisfaction,” Health Affairs (July 2017), https://www.healthaffairs.org/do/10.1377/hblog20170724.061160/full/ ↩︎
- Stacey McMorrow, Jason Gates, Sharon Long, and Genevieve Kenney, “Medicaid Expansion Increased Coverage, Improved Affordability, and Reduced Psychological Distress for Low-Income Parents,” Health Affairs 36 no. 5 (May 2017): 808-818, https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1650 ↩︎
- Luojia Hu, Robert Kaestenr, Bhashkar Mazumder, Sarah Miller, and Ashley Wong, “The Effect of the Affordable Care Act Medicaid Expansions on Financial Wellbeing,” Journal of Public Economics 163 (July 2018): 99-112, https://www.sciencedirect.com/science/article/abs/pii/S0047272718300707 ↩︎
- Hyunjung Lee and Frank Porell, “The Effect of the Affordable Care Act Medicaid Expansion on Disparities in Access to Care and Health Status,” Medical Care Research and Review epub ahead of print (October 2018), https://journals.sagepub.com/doi/abs/10.1177/1077558718808709?rfr_dat=cr_pub%3Dpubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&journalCode=mcrd ↩︎
- Helen Levy, Thomas Buchmueller, and Sayeh Nikpay, “The Impact of Medicaid Expansion on Household Consumption,” Eastern Economic Journal 45, no. 1 (January 2019): 34-57, https://link.springer.com/article/10.1057/s41302-018-0124-7 ↩︎
- Helen Levy et al., “Macroeconomic Feedback Effects of Medicaid Expansion: Evidence from Michigan,” Journal of Health Politics, Policy and Law Epub ahead of print (October 2019), https://doi.org/10.1215/03616878-7893555 ↩︎
- James A. Richardson, Jared J. Llorens, and Roy L. Heidelberg. Medicaid Expansion and the Louisiana Economy, 2018 and 2019 (Louisiana Department of Health, Prepared by Louisiana State University, August 2019), http://ldh.la.gov/assets/media/3and4.2019FinalReportMedicaidExpansionstudy.pdf ↩︎
- James Richardson, Jared Llorens, and Roy Heidelberg, Medicaid Expansion and the Louisiana Economy (Louisiana Department of Health, March 2018), http://gov.louisiana.gov/assets/MedicaidExpansion/MedicaidExpansionStudy.pdf ↩︎
- Bryce Ward and Brandon Bridge, The Economic Impact of Medicaid Expansion in Montana: Updated Findings (Bureau of Business and Economic Research, January 2019), https://mthcf.org/wp-content/uploads/2019/01/Economic-Impact-of-MedEx-in-MT_1.28.19-FINAL.pdf ↩︎
- Manatt Health, Medicaid Expansion: How It Affects Montana’s State Budget, Economy, and Residents (Montana Healthcare Foundation, prepared by Manatt Health, June 2018), https://mthcf.org/wp-content/uploads/2018/06/Manatt-MedEx_FINAL_6.1.18.pdf ↩︎
- Mark Duggan, Atul Gupta, and Emilie Jackson, The Impact of the Affordable Care Act: Evidence from California’s Hospital Sector (National Bureau of Economic Research, working paper no. 25488, January 2019), https://www.nber.org/papers/w25488.pdf ↩︎
- Louisiana Department of Health, Medicaid Expansion 2016/17 (Baton Rouge, Louisiana Department of Health, June 2017), http://dhh.louisiana.gov/assets/HealthyLa/Resources/MdcdExpnAnnlRprt_2017_WEB.pdf ↩︎
- April Grady, Deborah Bachrach, and Patti Boozang, Medicaid’s Role in the Delivery and Payment of Substance Use Disorder Services in Montana, (Manatt Health, March 2017), http://mthcf.org/wp-content/uploads/2017/03/Medicaid-Role-in-Substance-Use-Disorder-Services-in-Montana_Final.pdf ↩︎
- The Colorado Health Foundation, Assessing the Economic and Budgetary Impact of Medicaid Expansion in Colorado, (The Colorado Health Foundation, March 2016), https://www.coloradohealth.org/sites/default/files/documents/2017-01/Medicaid_ExecutiveSummary_ONLINE.pdf ↩︎
- Lee A. Reynis, Economic and Fiscal Impacts of the Medicaid Expansion in New Mexico, (The University of New Mexico Bureau of Business and Economic Research, February 2016), http://bber.unm.edu/media/publications/Medicaid_Expansion_Final2116R.pdf ↩︎
- Benjamin Sommers and Jonathan Gruber, “Federal Funding Insulated State Budgets From Increased Spending Related To Medicaid Expansion,” Health Affairs epub ahead of print (April 2017), https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2016.1666 ↩︎
- Abby Evans, John Folkemer, Joel Menges, Amira Mouna, Nick Pantaleo, Emily Ricci, and Poornima Sigh, Assessment of Medicaid Expansion and Reform, Initial Analysis (The Menges Group, January 2016), https://alaskamentalhealthtrust.org/wp-content/uploads/2018/08/HandOut-MedicaidExpansionAndReformInitialAnalysis-011516-TheMengesGroup.pdf ↩︎
- Chris Brown and John Bennett, Economic Impacts of the Arkansas Private Option (Regional Economic Models, Inc., August 2015), http://www.arkhospitals.org/Misc.%20Files/August2015APOEconomicImpacts.pdf ↩︎
- Deborah Bachrach, Patricia Boozang, Avi Herring, and Dori Glanz Reyneri, States Expanding Medicaid See Significant Budget Savings and Revenue Gains, (Manatt Health Solutions, prepared by the Robert Wood Johnson Foundation’s State Health Reform Assistance Network, March 2016), http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2016/rwjf419097 ↩︎
- Stan Dorn, Norton Francis, Laura Snyder, and Robin Rudowitz, The Effects of the Medicaid Expansion on State Budgets: An Early Look in Select States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, March 2015), http://kff.org/medicaid/issue-brief/the-effects-of-the-medicaid-expansion-on-state-budgets-an-early-look-in-select-states/ ↩︎
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf ↩︎
- Robin Rudowitz, Laura Snyder, and Vernon K. Smith, Medicaid Enrollment and Spending Growth: FY 2015 & 2016 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, October 2015), https://modern.kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2015-2016/ ↩︎
- Robin Rudowitz, Elizabeth Hinton, and Larisa Antonisse, Medicaid Enrollment and Spending Growth: FY 2018 & 2019 (Washington, DC: Kaiser Family Foundation, October 2018), https://modern.kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2018-2019/ ↩︎
- Robin Rudowitz, Elizabeth Hinton, Maria Diaz, Madeline Guth, and Marina Tian, Medicaid Enrollment and Spending Growth: FY 2019 & 2020 (Washington, DC: Kaiser Family Foundation, October 2019), https://modern.kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2019-2020/ ↩︎
- Micah Hartman et al., “National Health Care Spending in 2016: Spending and Enrollment Growth Slow After Initial Coverage Expansions,” Health Affairs epub ahead of print (December 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1299 ↩︎
- Jacqueline Fiore, The Impact of the Affordable Care Act’s Medicaid Expansion on Medicaid Spending by Health Care Service Category (Tulane University, July 2017), http://econ.tulane.edu/RePEc/pdf/tul1706.pdf ↩︎
- Vikki Wachino and Samantha Artiga, How Connecting Justice-Involved Individuals to Medicaid Can Help Address the Opioid Epidemic (Washington, DC: Kaiser Family Foundation, June 2019), https://modern.kff.org/medicaid/issue-brief/how-connecting-justice-involved-individuals-to-medicaid-can-help-address-the-opioid-epidemic/ ↩︎
- Aaron McNay, Amy Watson, Barbara Wagner, and Chris Bradley, Montana Medicaid and Montana Employers (Montana Department of Revenue and Montana Department of Labor & Industry, January 2019), http://lmi.mt.gov/Portals/193/Publications/LMI-Pubs/Special%20Reports%20and%20Studies/MT-Medicaid_Report.pdf ↩︎
- Benjamin Sommers and Jonathan Gruber, “Federal Funding Insulated State Budgets From Increased Spending Related To Medicaid Expansion,” Health Affairs epub ahead of print (April 2017), http://content.healthaffairs.org/content/early/2017/04/10/hlthaff.2016.1666.full ↩︎
- Louisiana Department of Health, Medicaid Expansion 2016/17 (Baton Rouge, Louisiana Department of Health, June 2017), http://dhh.louisiana.gov/assets/HealthyLa/Resources/MdcdExpnAnnlRprt_2017_WEB.pdf ↩︎
- James Richardson, Jared Llorens, and Roy Heidelberg, Medicaid Expansion and the Louisiana Economy (Louisiana Department of Health, March 2018), http://gov.louisiana.gov/assets/MedicaidExpansion/MedicaidExpansionStudy.pdf ↩︎
- James A. Richardson, Jared J. Llorens, and Roy L. Heidelberg. Medicaid Expansion and the Louisiana Economy, 2018 and 2019 (Louisiana Department of Health, Prepared by Louisiana State University, August 2019), http://ldh.la.gov/assets/media/3and4.2019FinalReportMedicaidExpansionstudy.pdf ↩︎
- Manatt Health, Medicaid Expansion: How It Affects Montana’s State Budget, Economy, and Residents (Montana Healthcare Foundation, prepared by Manatt Health, June 2018), https://mthcf.org/wp-content/uploads/2018/06/Manatt-MedEx_FINAL_6.1.18.pdf ↩︎
- Aaron McNay, Amy Watson, Barbara Wagner, and Chris Bradley, Montana Medicaid and Montana Employers (Montana Department of Revenue and Montana Department of Labor & Industry, January 2019), http://lmi.mt.gov/Portals/193/Publications/LMI-Pubs/Special%20Reports%20and%20Studies/MT-Medicaid_Report.pdf ↩︎
- Helen Levy et al., “Macroeconomic Feedback Effects of Medicaid Expansion: Evidence from Michigan,” Journal of Health Politics, Policy and Law Epub ahead of print (October 2019), https://doi.org/10.1215/03616878-7893555 ↩︎
- Qiwei He and Scott Barkowski, “The Effect of Health Insurance on Crime: Evidence from the Affordable Care Act Medicaid Expansion,” Health Economics Epub ahead of print (January 2020): 261-277, https://doi.org/10.1002/hec.3977 ↩︎
- Jesse M. Hinde et al., “Increasing Access to Opioid Use Disorder Treatment: Assessing State Policies and the Evidence Behind Them,” Journal of Studies on Alcohol and Drugs 80, no. 6 (November 2019): 693-697, https://doi.org/10.15288/jsad.2019.80.693 ↩︎
- April Grady, Deborah Bachrach, and Patti Boozang, Medicaid’s Role in the Delivery and Payment of Substance Use Disorder Services in Montana, (Manatt Health, March 2017), http://mthcf.org/wp-content/uploads/2017/03/Medicaid-Role-in-Substance-Use-Disorder-Services-in-Montana_Final.pdf ↩︎
- Jacob Vogler, Access to Health Care and Criminal Behavior: Short-Run Evidence from the ACA Medicaid Expansions (University of Illinois at Urbana-Champaign, November 2017), https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3042267 ↩︎
- Vikki Wachino and Samantha Artiga, How Connecting Justice-Involved Individuals to Medicaid Can Help Address the Opioid Epidemic (Washington, DC: Kaiser Family Foundation, June 2019), https://modern.kff.org/medicaid/issue-brief/how-connecting-justice-involved-individuals-to-medicaid-can-help-address-the-opioid-epidemic/ ↩︎
- Deborah Bachrach, Patricia Boozang, Avi Herring, and Dori Glanz Reyneri, States Expanding Medicaid See Significant Budget Savings and Revenue Gains, (Manatt Health Solutions, prepared by the Robert Wood Johnson Foundation’s State Health Reform Assistance Network, March 2016), http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2016/rwjf419097 ↩︎
- Stan Dorn, Norton Francis, Laura Snyder, and Robin Rudowitz, The Effects of the Medicaid Expansion on State Budgets: An Early Look in Select States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, March 2015), http://kff.org/medicaid/issue-brief/the-effects-of-the-medicaid-expansion-on-state-budgets-an-early-look-in-select-states/ ↩︎
- Lee A. Reynis, Economic and Fiscal Impacts of the Medicaid Expansion in New Mexico, (The University of New Mexico Bureau of Business and Economic Research, February 2016), http://bber.unm.edu/media/publications/Medicaid_Expansion_Final2116R.pdf ↩︎
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf ↩︎
- Abby Evans, John Folkemer, Joel Menges, Amira Mouna, Nick Pantaleo, Emily Ricci, and Poornima Sigh, Assessment of Medicaid Expansion and Reform, Initial Analysis (The Menges Group, January 2016), https://alaskamentalhealthtrust.org/wp-content/uploads/2018/08/HandOut-MedicaidExpansionAndReformInitialAnalysis-011516-TheMengesGroup.pdf ↩︎
- Johanna Maclean and Brendan Saloner, “The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act,” Journal of Policy Analysis and Management 38, no. 2 (2019): 366-393, https://www.ncbi.nlm.nih.gov/pubmed/30882195 ↩︎
- Mark Duggan, Atul Gupta, and Emilie Jackson, The Impact of the Affordable Care Act: Evidence from California’s Hospital Sector (National Bureau of Economic Research, working paper no. 25488, January 2019), https://www.nber.org/papers/w25488.pdf ↩︎
- Amanda Abraham et al., “Changes in State Technical Assistance Priorities and Block Grant Funds for Addiction After ACA Implementation,” American Journal of Public Health epub ahead of print (May 2019), https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2019.305052 ↩︎
- Aparna Soni, Marguerite Burns, Laura Dague, and Kosali Simon, “Medicaid Expansion and State Trends in Supplemental Security Income Program Participation,” Health Affairs 36 no. 8, (August 2017): 1485-1488, http://content.healthaffairs.org/content/36/8/1485.full?sid=982b20c0-0a17-4dc4-a35a-b0302d4ec289 ↩︎
- Paul Jacobs, Genevieve Kenney, and Thomas Selden, “Newly Eligible Enrollees In Medicaid Spend Less And Use Less Care Than Those Previously Eligible,” Health Affairs 36, no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0252 ↩︎
- David Lassman et al., “Health Spending by State 1991-2014: Measuring Per Capita Spending by Payers and Programs,” Health Affairs epub ahead of print (June 2017), http://content.healthaffairs.org/content/early/2017/06/13/hlthaff.2017.0416 ↩︎
- Stephan R. Lindner et al., “Health Care Expenditures Among Adults With Diabetes After Oregon’s Medicaid Expansion,” Diabetes Care Epub ahead of print (December 2019), https://doi.org/10.2337/dc19-1343 ↩︎
- Laura Snyder, Katherine Young, Robin Rudowitz, and Rachel Garfield, Medicaid Expansion Spending and Enrollment in Context: An Early Look at CMS Claims Data for 2014 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, January 2016), http://kff.org/medicaid/issue-brief/medicaid-expansion-spending-and-enrollment-in-context-an-early-look-at-cms-claims-data-for-2014/ ↩︎
- Heather Holderness et al., “Where Do Oregon Medicaid Enrollees Seek Outpatient Care Post-Affordable Care Act Medicaid Expansion?,” Medical Care 57, no. 10 (October 2019): 788-794, https://doi.org/10.1097/mlr.0000000000001189 ↩︎
- Christian Wolfe, Kathryn Rennie, and Christopher Truffer, 2017 Actuarial Report on the Financial Outlook for Medicaid (Office of the Actuary, Centers for Medicare and Medicaid Services, September 2018), https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/ActuarialStudies/Downloads/MedicaidReport2017.pdf ↩︎
- The Colorado Health Institute, Medicaid Expansion in Colorado: An Analysis of Enrollment, Costs and Benefits—and How They Exceeded Expectations (The Colorado Health Institute, May 2016), http://www.coloradohealthinstitute.org/uploads/postfiles/MK_Expansion_Report.pdf ↩︎
- Pennsylvania Department of Human Services, Medicaid Expansion Report, (Pennsylvania Department of Human Services, January 2017), http://www.dhs.pa.gov/cs/groups/webcontent/documents/document/c_257436.pdf ↩︎
- Laura Snyder, Katherine Young, Robin Rudowitz, and Rachel Garfield, Medicaid Expansion Spending and Enrollment in Context: An Early Look at CMS Claims Data for 2014 (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, January 2016), http://kff.org/medicaid/issue-brief/medicaid-expansion-spending-and-enrollment-in-context-an-early-look-at-cms-claims-data-for-2014/ ↩︎
- Paul Jacobs, Genevieve Kenney, and Thomas Selden, “Newly Eligible Enrollees In Medicaid Spend Less And Use Less Care Than Those Previously Eligible,” Health Affairs 36, no. 9 (September 2017), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0252 ↩︎
- David Lassman et al., “Health Spending by State 1991-2014: Measuring Per Capita Spending by Payers and Programs,” Health Affairs epub ahead of print (June 2017), http://content.healthaffairs.org/content/early/2017/06/13/hlthaff.2017.0416 ↩︎
- Aditi Sen and Thomas DeLeire, The Effect of Medicaid Expansion on Marketplace Premiums (Office of the Assistant Secretary for Planning and Evaluation, August 2016), https://aspe.hhs.gov/sites/default/files/pdf/206761/McaidExpMktplcPrem.pdf ↩︎
- Aditi Sen and Thomas DeLeire, “How Does Expansion Of Public Health Insurance Affect Risk Pools And Premiums In The Market For Private Health Insurance? Evidence From Medicaid And The Affordable Care Act Marketplaces,” Health Economics 27 (July 2018): 1877–1903, https://onlinelibrary.wiley.com/doi/abs/10.1002/hec.3809 ↩︎
- Ashley Semanskee, Cynthia Cox, and Larry Levitt, Data Note: Effect of State Decisions on State Risk Scores (Kaiser Family Foundation, October 2016), https://modern.kff.org/health-reform/issue-brief/data-note-effect-of-state-decisions-on-state-risk-scores/ ↩︎
- Jocelyn Guyer, Naomi Shine, MaryBeth Musumeci, and Robin Rudowitz, A Look at the Private Option in Arkansas (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, August 2015), http://kff.org/medicaid/issue-brief/a-look-at-the-private-option-in-arkansas/ ↩︎
- Bela Gorman and Jenn Smagula, 2016 Actuarial Analysis of NH Premium Assistance Program, (Gorman Actuarial, Inc., August 2017), https://www.nh.gov/insurance/reports/documents/08-28-17-ga-nh-pap-analysis-final.pdf ↩︎
- Hefei Wen, Kenton J. Johnston, Lindsay Allen, and Teresa M. Waters, “Medicaid Expansion Associated With Reductions In Preventable Hospitalizations,” Health Affairs 38, no. 11 (November 2019): 1845-1849, https://doi.org/10.1377/hlthaff.2019.00483 ↩︎
- Alexander T. Janke, Shooshan Danagoulian, Arjun K. Venkatesh, and Phillip D. Levy, “Medicaid Expansion and Resource Utilization in the Emergency Department,” The American Journal of Emergency Medicine Epub ahead of print (January 2020), https://doi.org/10.1016/j.ajem.2019.12.050 ↩︎
- Hawazin W. Elani, Ichiro Kawachi, and Benjamin D. Sommers, “Changes in Emergency Department Dental Visits after Medicaid Expansion,” Health Services Research Epub ahead of print (January 2020), https://doi.org/10.1111/1475-6773.13261 ↩︎
- Emanuel Eguia et al., “The Impact of the Affordable Care Act Medicaid Expansion on Vascular Surgery,” Annals of Vascular Surgery Epub ahead of print (January 2020), https://doi.org/10.1016/j.avsg.2020.01.006 ↩︎
- Mark Clapp et al., “Association of Medicaid Expansion With Coverage and Access to Care for Pregnant Women,” Obstetrics & Gynecology 134, no. 5 (November 2019): 1066-1074, https://doi.org/10.1097/aog.0000000000003501 ↩︎
- Charles A. Daly et al., “The Effects of Medicaid Expansion on Triage and Regional Transfer After Upper-Extremity Trauma,” The Journal of Hand Surgery 44, no. 9 (September 2019): 720-727, https://doi.org/10.1016/j.jhsa.2019.05.020 ↩︎
- John Scott et al., “Lifting the Burden: State Medicaid Expansion Reduces Financial Risk for the Injured,” Journal of Trauma and Acute Care Surgery Epub ahead of print (September 2019), https://doi.org/10.1097/ta.0000000000002493 ↩︎
- Craig Garthwaite et al., All Medicaid Expansions Are Not Created Equal: The Geography and Targeting of the Affordable Care Act (National Bureau of Economic Research, Working Paper No. 26289, September 2019), http://www.nber.org/papers/w26289 ↩︎
- Shannon McConville, Maria Raven, Sarah Sabbagh, and Renee Hsia, “Frequent Emergency Department Users: A Statewide Comparison Before And After Affordable Care Act Implementation,” Health Affairs 37, no. 6, (June 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0784 ↩︎
- Rahul Ladhania, Amelia Haviland, Arvind Venkat, Rahul Telang, and Jesse Pines, “The Effect of Medicaid Expansion on the Nature of New Enrollees’ Emergency Department Use,” Medical Care Research and Review epub ahead of print (May 2019), https://journals.sagepub.com/doi/abs/10.1177/1077558719848270 ↩︎
- Beatrice D. Probst, Luther Walls, Michael Cirone, and Talar Markossian, “Examining the Effect of the Affordable Care Act on Two Illinois Emergency Departments,” Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health 20, no. 5 (September 2019): 710-716, https://doi.org/10.5811/westjem.2019.6.41943 ↩︎
- Kurt Gillis, Physicians’ Patient Mix – A Snapshot from the 2016 Benchmark Survey and Changes Associated with the ACA (American Medical Association, October 2017), https://www.ama-assn.org/sites/default/files/media-browser/public/health-policy/PRP-2017-physician-benchmark-survey-patient-mix.pdf ↩︎
- Seth Freedman, Sayeh Nikpay, Aaron Carroll, and Kosali Simon, “Changes in inpatient payer-mix and hospitalizations following Medicaid expansion: Evidence from all-capture hospital discharge data,” PLoS ONE 12 no. 9 (September 2017), http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0183616 ↩︎
- Allen Dobson, Joan DaVanzo, Randy Haught, and Phap Hoa Luu, Comparing the Affordable Care Act’s Financial Impact on Safety-Net Hospitals in States that Expanded Medicaid and Those That Did Not (The Commonwealth Fund, November 2017), http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2017/nov/dobson_impact_medicaid_expanion_safety_net_hosps_ib.pdf ↩︎
- Richard Lindrooth, Marcelo Perraillon, Rose Hardy, and Gregory Tung, “Understanding the Relationship Between Medicaid Expansions and Hospital Closures,” Health Affairs epub ahead of print (January 2018), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0976 ↩︎
- Heather Angier et al., “Uninsured Primary Care Visit Disparities under the Affordable Care Act,” Annals of Family Medicine, 15 no. 5 (September 2017): 434-442, http://www.annfammed.org/content/15/5/434.full.pdf+html ↩︎
- Andrew Loehrer et al., “Association of the Affordable Care Act Medicaid Expansion with Access to and Quality of Care for Surgical Conditions,” Journal of the American Medical Association Surgery, epub ahead of print (January 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2670459?redirect=true ↩︎
- Sayeh Nikpay, Seth Freedman, Helen Levy, and Tom Buchmueller, “Effect of the Affordable Care Act Medicaid Expansion on Emergency Department Visits: Evidence From State-Level Emergency Department Databases,” Annals of Emergency Medicine 70, no.2 (August 2017), http://www.annemergmed.com/article/S0196-0644(17)30319-0/pdf ↩︎
- Johanna Maclean and Brendan Saloner, “The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act,” Journal of Policy Analysis and Management 38, no. 2 (2019): 366-393, https://www.ncbi.nlm.nih.gov/pubmed/30882195 ↩︎
- Monique Barakat et al., “Affordable Care Act and Healthcare Delivery: A Comparison of California and Florida Hospitals and Emergency Departments,” PLoS ONE 12 no. 8 (August 2017), http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0182346 ↩︎
- Eili Klein et al., “The Effect of Medicaid Expansion on Utilization in Maryland Emergency Departments,” Annals of Emergency Medicine epub ahead of print (June 2017), http://www.annemergmed.com/article/S0196-0644(17)30784-9/pdf ↩︎
- Aabha Sharma, Scott Dresden, Emilie Powell, Raymond Kang, Joe Feinglass, “Emergency Department Visits and Hospitalizations for the Uninsured in Illinois Before and After Affordable Care Act Insurance Expansion,” Journal of Community Health 42 no. 3 (June 2017): 591-597, https://link.springer.com/article/10.1007/s10900-016-0293-4 ↩︎
- Vivian Wu et al., “Early Impact of the Affordable Care Act Coverage Expansion on Safety-Net Hospital Inpatient Payer Mix and Market Shares,” Health Services Research (January 2018), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12812/full ↩︎
- David Dranove, Craig Garthwaite, and Christopher Ody, The Impact of the ACA’s Medicaid Expansion on Hospitals’ Uncompensated Care Burden and the Potential Effects of Repeal, (The Commonwealth Fund, May 2017), http://www.commonwealthfund.org/publications/issue-briefs/2017/may/aca-medicaid-expansion-hospital-uncompensated-care ↩︎
- Fredric Blavin, How Has the ACA Changed Finances for Different Types of Hospitals? Updated Insights from 2015 Cost Report Data (The Urban Institute, April 2017), http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2017/rwjf436310 ↩︎
- Craig Garthwaite, Tal Gross, Matthew Notowidigdo, and John Graves, “Insurance Expansion and Hospital Emergency Department Access: Evidence from the Affordable Care Act,” Annals of Internal Medicine 166 no. 3 (February 2017): 172-179, http://annals.org/aim/article/2593599/insurance-expansion-hospital-emergency-department-access-evidence-from-affordable-care ↩︎
- Nathalie Huguet et al., “Medicaid Expansion Produces Long-Term Impact on Insurance Coverage Rates in Community Health Centers,” Journal of Primary Care & Community Health epub ahead of print (May 2017), http://journals.sagepub.com/doi/full/10.1177/2150131917709403 ↩︎
- Susan Camilleri, “The ACA Medicaid Expansion, Disproportionate Share Hospitals, and Uncompensated Care” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12702/abstract ↩︎
- Natalia Chalmers, Jane Grover, and Rob Compton, “After Medicaid Expansion in Kentucky, Use of Hospital Emergency Departments for Dental Conditions Increased,” Health Affairs 35, no. 12 (December 2016), http://content.healthaffairs.org/content/35/12/2268.full#xref-ref-32-1 ↩︎
- Arkansas Health Reform Legislative Task Force, Health Care Task Force Preliminary Report, (Arkansas Health Reform Legislative Task Force, December 2015), http://www.arkleg.state.ar.us/assembly/2015/Meeting%20Attachments/836/I14218/Task%20Force%20report%2012-17-15%20sent%20to%20Jill.pdf ↩︎
- Arkansas Hospital Association, “Survey Reveals Private Option Impact on Hospitals,” The Notebook 21, no. 33 (November 2014), http://www.arkhospitals.org/archive/notebookpdf/Notebook_11-03-14.pdf ↩︎
- Mary Anderson, Jeffrey Glasheen, and Debra Anoff, “Impact of State Medicaid Expansion Status on Length of Stay and In-Hospital Mortality for General Medicine Patients at US Academic Medical Centers,” Journal of Hospital Medicine Epub ahead of print (August 2016), http://onlinelibrary.wiley.com/wol1/doi/10.1002/jhm.2649/citedby ↩︎
- The University of Michigan Institute for Healthcare Policy & Innovation, The Healthy Michigan Plan: 2015 Report on Uncompensated Care and Insurance Rates (The University of Michigan Institute for Healthcare Policy & Innovation, prepared for the Michigan Department of Health and Human Services and the Michigan Department of Insurance and Financial Services, December 2016), http://www.michigan.gov/documents/mdhhs/2015_Report_on_Uncompensated_Care_and_Insurance_Rates-HMP_547720_7.pdf ↩︎
- Laurie Felland, Peter Cunningham, Annie Doubleday, and Cannon Warren, Effects of the Affordable Care Act on Safety Net Hospitals (Washington, DC: Mathematica Policy Research, prepared for the Assistant Secretary for Planning and Evaluation, November 2016), https://aspe.hhs.gov/sites/default/files/pdf/255491/SafetyNetHospital.pdf ↩︎
- Sayeh Nikpay, Thomas Buchmueller, and Helen Levy. “Affordable Care Act Medicaid Expansion Reduced Uninsured Hospital Stays in 2014,” Health Affairs 35, no.1 (January 2016): 106-110, http://content.healthaffairs.org/content/35/1/106.full ↩︎
- Fred Hellinger, “In Four ACA Expansion States, The Percentage of Uninsured Hospitalizations for People With HIV Declined, 2012-14,” Health Affairs 34, no. 12 (December 2015): 2061-2068, http://search.proquest.com/docview/1749932806/627DA95CDEA44BE7PQ/77?accountid=39486# ↩︎
- Deborah Bachrach, Patricia Boozang, and Mindy Lipson, The Impact of Medicaid Expansion on Uncompensated Care Costs: Early Results and Policy Implications for States, (Manatt Health Solutions, prepared by the Robert Wood Johnson Foundation’s State Health Reform Assistance Network, June 2015), https://www.manatt.com/uploadedFiles/Content/5_Insights/White_Papers/State-Network-Manatt-Impact-of-Medicaid-Expansion-on-Uncompensated-Care-Costs-June-2015.pdf ↩︎
- Peter Cunningham, Rachel Garfield, and Robin Rudowitz, How Are Hospitals Faring Under the Affordable Care Act? Early Experiences from Ascension Health (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, April 2015), http://kff.org/health-reform/issue-brief/how-are-hospitals-faring-under-the-affordable-care-act-early-experiences-from-ascension-health/ ↩︎
- Thomas DeLeire, Karen Joynt, and Ruth McDonald, Impact of Insurance Expansion on Hospital Uncompensated Care Costs in 2014 (Office of the Assistant Secretary for Planning and Evaluation, September 2014), https://aspe.hhs.gov/sites/default/files/pdf/77061/ib_UncompensatedCare.pdf ↩︎
- PricewaterhouseCoopers LLP Health Research Institute, Medicaid 2.0: Health System Haves and Have Nots (PwC Health Research Institute, September 2014), http://www.pwc.com/us/en/health-industries/health-research-institute/assets/pwc-hri-medicaid-report-final.pdf ↩︎
- Colorado Hospital Association, Impact of Medicaid Expansion on Hospital Volumes (Colorado Hospital Association Center for Health Information and Data Analytics, June 2014), http://www.cha.com/documents/press-releases/cha-medicaid-expansion-study-june-2014.aspx ↩︎
- Fredric Blavin, “Association Between the 2014 Medicaid Expansion and US Hospital Finances,” The Journal of the American Medical Association 316 no. 14 (October 2016): 1475-1483, http://jamanetwork.com/journals/jama/article-abstract/2565750 ↩︎
- David Dranove, Craig Garthwaite, and Christopher Ody, “Uncompensated Care Decreased At Hospitals In Medicaid Expansion States But Not At Hospitals In Nonexpansion States,” Health Affairs 35 no. 8 (August 2016): 1471-1479, http://content.healthaffairs.org/content/35/8/1471.full ↩︎
- Peter Cunningham, Robin Rudowitz, Katherine Young, Rachel Garfield, and Julia Foutz, Understanding Medicaid Hospital Payments and the Impact of Recent Policy Changes (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, June 2016), http://kff.org/medicaid/issue-brief/understanding-medicaid-hospital-payments-and-the-impact-of-recent-policy-changes/ ↩︎
- Christine Jones, Serena Scott, Debra Anoff, Read Pierce, and Jeffrey Glasheen, “Changes in Payer Mix and Physician Reimbursement After the Affordable Care Act and Medicaid Expansion,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 52 (August 2015), http://inq.sagepub.com/content/52/0046958015602464.full ↩︎
- Nadia Laniado, Avery R. Brow, Eric Tranby, and Victor M. Badner, “Trends in Non-Traumatic Dental Emergency Department Use in New York and New Jersey: A Look at Medicaid Expansion from Both Sides of the Hudson River,” Journal of Public Health Dentistry Epub ahead of print (October 2019), https://doi.org/10.1111/jphd.12343 ↩︎
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf ↩︎
- Robin Rudowitz and Rachel Garfield, New Analysis Shows States with Medicaid Expansion Experienced Declines in Uninsured Hospital Discharges (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, September 2015), http://kff.org/health-reform/issue-brief/new-analysis-shows-states-with-medicaid-expansion-experienced-declines-in-uninsured-hospital-discharges/ ↩︎
- Jordan Rhodes, Thomas Buchmueller, Helen Levy, and Sayeh Nikpay, “Heterogeneous Effects Of The Aca Medicaid Expansion On Hospital Financial Outcomes,” Contemporary Economic Policy epub ahead of print (April 2019), https://onlinelibrary.wiley.com/doi/full/10.1111/coep.12428 ↩︎
- Gary Young, Stephen Flaherty, E. Zepeda, Simone Singh, and Sara Rosenbaum, “Impact of ACA Medicaid Expansion on Hospitals’ Financial Status” Journal of Healthcare Management 64, no. 2 (March 2019): 91–102, https://insights.ovid.com/crossref?an=00115514-201904000-00007 ↩︎
- Nathalie Huguet et al., “The Impact of the Affordable Care Act (ACA) Medicaid Expansion on Visit Rates for Diabetes in Safety Net Health Centers,” Journal of the American Board of Family Medicine 31, no. 6 (November 2018): 905-916, https://www.jabfm.org/content/31/6/905.full ↩︎
- Susan Dorr Goold et al., “Primary Care Clinicians’ Views About the Impact of Medicaid Expansion in Michigan: A Mixed Methods Study,” Journal of General Internal Medicine 33, no. 8 (June 2018): 1307-1316, https://link.springer.com/article/10.1007/s11606-018-4487-6 ↩︎
- Pennsylvania Department of Human Services, Medicaid Expansion Report, (Pennsylvania Department of Human Services, January 2017), http://www.dhs.pa.gov/cs/groups/webcontent/documents/document/c_257436.pdf ↩︎
- Megan Cole, Brad Wright, Ira Wilson, Omar Gallarraga, and Amal Trivedi, “Medicaid Expansion And Community Health Centers: Care Quality And Service Use Increased For Rural Patients” Health Affairs 37, no. 6 (June 2018), https://www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2017.1542 ↩︎
- Mark Duggan, Atul Gupta, and Emilie Jackson, The Impact of the Affordable Care Act: Evidence from California’s Hospital Sector (National Bureau of Economic Research, working paper no. 25488, January 2019), https://www.nber.org/papers/w25488.pdf ↩︎
- Sara Rosenbaum, Jennifer Tolbert, Jessica Sharac, Peter Shin, Rachel Gunsalus, and Julia Zur, Community Health Centers: Growing Importance in a Changing Health Care System (Washington, DC: Kaiser Family Foundation, March 2018), https://modern.kff.org/medicaid/issue-brief/community-health-centers-growing-importance-in-a-changing-health-care-system/ ↩︎
- Michel Boudreaux, Yoon Choi, Liyang Xie, and Daniel Marthey, “Medicaid Expansion at Title X Clinics: Client Volume, Payer Mix, and Contraceptive Method Type,” Medical Care epub ahead of print (April 2019), https://www.ncbi.nlm.nih.gov/pubmed/30973473 ↩︎
- Christina Andrews et al., “Medicaid Coverage In Substance Use Disorder Treatment After The Affordable Care Act,” Journal of Substance Abuse Treatment epub ahead of print (April 2019), https://www.sciencedirect.com/science/article/pii/S0740547218305750 ↩︎
- Jesse Pines, Rahul Ladhania BTech, Bernard Black , Christopher Corbit, Jestin Carlson, and Arvind Venkat, “Changes in Reimbursement to Emergency Physicians After Medicaid Expansion Under the Patient Protection and Affordable Care Act,” Annals of Emergency Medicine 73, no. 3 (March 2019): 213-224, https://www.sciencedirect.com/science/article/pii/S019606441831374X ↩︎
- Heather Angier et al., “Racial/Ethnic Disparities in Health Insurance and Differences in Visit Type for a Population of Patients with Diabetes after Medicaid Expansion” Journal of Health Care for the Poor and Underserved 30, no.1, (March 2019) 116–130: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6429963/ ↩︎
- Gary Pickens et al., “Changes In Hospital Service Demand, Cost, And Patient Illness Severity Following Health Reform,” Health Services Research (May 2019), https://doi.org/10.1111/1475-6773.13165 ↩︎
- Neal Bhutiani, Brian Harbrecht, Charles Scoggins, and Matthew Bozeman, “Evaluating The Early Impact Of Medicaid Expansion On Trends In Diagnosis And Treatment Of Benign Gallbladder Disease In Kentucky,” The American Journal of Surgery (January 2019), https://www.americanjournalofsurgery.com/article/S0002-9610(18)30894-8/fulltext ↩︎
- Brendan Saloner, Sachini Bandara, Emma McGinty, and Colleen Barry, “Justice-Involved Adults With Substance Use Disorders: Coverage Increased but Rates of Treatment Did Not in 2014,” Health Affairs 35 no. 6 (June 2016), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2016.0005 ↩︎
- Brendan Saloner, Sachini Bandara, Emma McGinty, and Colleen Barry, “Justice-Involved Adults With Substance Use Disorders: Coverage Increased but Rates of Treatment Did Not in 2014,” Health Affairs 35 no. 6 (June 2016), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2016.0005 ↩︎
- Ehimare Akhabue, Lindsay Pool, Clyde Yancy, Philip Greenland, and Donald Lloyd-Jones, “Association of State Medicaid Expansion With Rate of Uninsured Hospitalizations for Major Cardiovascular Events, 2009-2014,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2698077 ↩︎
- Manzilat Akande Peter Minneci, Katherine Deans, Henry Xiang, and Jennifer Cooper, “Association of Medicaid Expansion Under the Affordable Care Act With Outcomes and Access to Rehabilitation in Young Adult Trauma Patients,” JAMA Surgery 153, no. 8 (August 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2682872?widget=personalizedcontent&previousarticle=2719270 ↩︎
- Cheryl Zogg et al., “Impact of Affordable Care Act Insurance Expansion on Pre-Hospital Access to Care: Changes in Adult Perforated Appendix Admission Rates after Medicaid Expansion and the Dependent Coverage Provision,” Journal of the American College of Surgeons 228, no. 1 (January 2019): 29-43, https://www.journalacs.org/article/S1072-7515(18)32078-7/fulltext ↩︎
- Cheryl Zogg et al., “Association of Medicaid Expansion With Access to Rehabilitative Care in Adult Trauma Patients,” JAMA Surgery epub ahead of print (January 2019), https://jamanetwork.com/journals/jamasurgery/article-abstract/2719270?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamasurg.2018.5177 ↩︎
- Rishi Wadhera et al., “Association of State Medicaid Expansion With Quality of Care and Outcomes for Low-Income Patients Hospitalized With Acute Myocardial Infarction,” JAMA Cardiology 4, no. 2 (January 2019): 120-127, https://jamanetwork.com/journals/jamacardiology/article-abstract/2720425?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamacardio.2018.4577 ↩︎
- Angelica Meinhofer and Allison Witman, “The Role Of Health Insurance On Treatment For Opioid Use Disorders: Evidence From The Affordable Care Act Medicaid Expansion,” Journal of Health Economics 60 (June 2018): 177-197, https://www.sciencedirect.com/science/article/abs/pii/S0167629617311530 ↩︎
- Favel Mondesir et al., “Medicaid Expansion and Hospitalization for Ambulatory Care–Sensitive Conditions Among Nonelderly Adults With Diabetes,” Journal of Ambulatory Care Management epub ahead of print (May 2019), https://insights.ovid.com/pubmed?pmid=31107800 ↩︎
- Xinxin Han, Quian Luo, and Leighton Ku, “Medicaid Expansion and Grant Funding Increases Helped Improve Community Health Center Capacity,” Health Affairs 36 no. 1 (January 2017): 49-56, http://content.healthaffairs.org/content/36/1/49.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19 ↩︎
- Josh Gray, Iyue Sung, and Stewart Richardson, Observations on the Affordable Care Act: 2014 (athenaResearch and Robert Wood Johnson Foundation ACA View Report, February 2015), http://www.athenahealth.com/~/media/athenaweb/files/pdf/acaview_year_end_2014.pdf ↩︎
- Gary Pickens et al., “Changes in Hospital Inpatient Utilization Following Health Care Reform,” Health Services Research epub ahead of print (June 2017), https://www.ncbi.nlm.nih.gov/pubmed/28664983 ↩︎
- Megan Hoopes, Heather Angier, Rachel Gold, Steffani Bailey, Nathalie Huguet, Miguel Marino, and Jennifer DeVoe, “Utilization of Community Health Centers in Medicaid Expansion and Nonexpansion States, 2013-2014,” Journal of Ambulatory Care Management 39 no. 4 (October 2016): 290-298, https://www.ncbi.nlm.nih.gov/pubmed/26765808 ↩︎
- Peter Shin, Jessica Sharac, Julia Zur, Sara Rosenbaum, and Julia Paradise, Health Center Patient Trends, Enrollment Activities, and Service Capacity: Recent Experience in Medicaid Expansion and Non-Expansion States (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, December 2015), http://kff.org/medicaid/issue-brief/health-center-patient-trends-enrollment-activities-and-service-capacity-recent-experience-in-medicaid-expansion-and-non-expansion-states/ ↩︎
- Steven Wallace, Maria-Elena Young, Michael Rodriguez, Amy Bonilla, and Nadereh Pourat, Community Health Centers Play a Critical Role in Caring for the Remaining Uninsured in the Affordable Care Act Era (UCLA Center for Health Policy Research, October 2016), http://healthpolicy.ucla.edu/publications/Documents/PDF/2016/FQHC_PB-oct2016.pdf ↩︎
- Jesse M. Pines, Mark Zocchi, Ali Moghtaderi, Bernard Black, Steven A. Farmer, Greg Hufstetler, Kevin Klauer and Randy Pilgrim, “Medicaid Expansion In 2014 Did Not Increase Emergency Department Use But Did Change Insurance Payer Mix,” Health Affairs 35, no. 8 (August 2016), http://content.healthaffairs.org/content/35/8/1480.full ↩︎
- Mathew Davis, Achamyeleh Gebremariam, John Ayanian, “Changes in Insurance Coverage Among Hospitalized Nonelderly Adults After Medicaid Expansion in Michigan,” The Journal of the American Medical Association 315 no. 23 (June 2016): 2617-2618, http://jamanetwork.com/journals/jama/fullarticle/2529615 ↩︎
- Brystana Kaufman, Kristin Reiter, George Pink, and George Holmes, “Medicaid Expansion Affects Rural and Urban Hospitals Differently,” Health Affairs 35 no. 9 (September 2016): 1665-1672, http://content.healthaffairs.org/content/35/9/1665.full?sid=4aea494e-8e02-4c66-8298-3c828bfc313b ↩︎
- Eric Charles et al., “Impact of Medicaid Expansion on Cardiac Surgery Volume and Outcomes,” The Annals of Thoracic Surgery (June 2017), http://www.annalsthoracicsurgery.org/article/S0003-4975(17)30552-0/pdf ↩︎
- Megan Cole, Omar Galarraga, Ira Wilson, Brad Wright, and Amal Trivedi, “At Federally Funded Health Centers, Medicaid Expansion was Associated with Improved Quality of Care,” Health Affairs 36 no. 1 (January 2017): 40-48, http://content.healthaffairs.org/content/36/1/40.full?sid=a3089120-6f4b-428b-bba8-5f005b444e19 ↩︎
- Stephen Berry et al., “Healthcare Coverage for HIV Provider Visits before and after Implementation of the Affordable Care Act,” Clinical Infectious Diseases, (May 2016), http://www.ncbi.nlm.nih.gov/pubmed/27143660 ↩︎
- Ramiro Manzano-Nunez et al., “Association of Medicaid Expansion Policy with Outcomes in Homeless Patients Requiring Emergency General Surgery,” World Journal of Surgery 43, no. 6 (June 2019): 1483-1489, https://link.springer.com/article/10.1007/s00268-019-04932-0 ↩︎
- Craig Garthwaite et al., All Medicaid Expansions Are Not Created Equal: The Geography and Targeting of the Affordable Care Act (National Bureau of Economic Research, Working Paper No. 26289, September 2019), http://www.nber.org/papers/w26289 ↩︎
- Alexander T. Janke, Shooshan Danagoulian, Arjun K. Venkatesh, and Phillip D. Levy, “Medicaid Expansion and Resource Utilization in the Emergency Department,” The American Journal of Emergency Medicine Epub ahead of print (January 2020), https://doi.org/10.1016/j.ajem.2019.12.050 ↩︎
- Hawazin W. Elani, Ichiro Kawachi, and Benjamin D. Sommers, “Changes in Emergency Department Dental Visits after Medicaid Expansion,” Health Services Research Epub ahead of print (January 2020), https://doi.org/10.1111/1475-6773.13261 ↩︎
- Beatrice D. Probst, Luther Walls, Michael Cirone, and Talar Markossian, “Examining the Effect of the Affordable Care Act on Two Illinois Emergency Departments,” Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health 20, no. 5 (September 2019): 710-716, https://doi.org/10.5811/westjem.2019.6.41943 ↩︎
- Shannon McConville, Maria Raven, Sarah Sabbagh, and Renee Hsia, “Frequent Emergency Department Users: A Statewide Comparison Before And After Affordable Care Act Implementation,” Health Affairs 37, no. 6, (June 2018), https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0784 ↩︎
- Sayeh Nikpay, Seth Freedman, Helen Levy, and Tom Buchmueller, “Effect of the Affordable Care Act Medicaid Expansion on Emergency Department Visits: Evidence From State-Level Emergency Department Databases,” Annals of Emergency Medicine 70, no.2 (August 2017), http://www.annemergmed.com/article/S0196-0644(17)30319-0/pdf ↩︎
- Monique Barakat et al., “Affordable Care Act and Healthcare Delivery: A Comparison of California and Florida Hospitals and Emergency Departments,” PLoS ONE 12 no. 8 (August 2017), http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0182346 ↩︎
- Rahul Ladhania, Amelia Haviland, Arvind Venkat, Rahul Telang, and Jesse Pines, “The Effect of Medicaid Expansion on the Nature of New Enrollees’ Emergency Department Use,” Medical Care Research and Review epub ahead of print (May 2019), https://journals.sagepub.com/doi/abs/10.1177/1077558719848270 ↩︎
- Jesse M. Pines, Mark Zocchi, Ali Moghtaderi, Bernard Black, Steven A. Farmer, Greg Hufstetler, Kevin Klauer and Randy Pilgrim, “Medicaid Expansion In 2014 Did Not Increase Emergency Department Use But Did Change Insurance Payer Mix,” Health Affairs 35, no. 8 (August 2016), http://content.healthaffairs.org/content/35/8/1480.full ↩︎
- Craig Garthwaite, Tal Gross, Matthew Notowidigdo, and John Graves, “Insurance Expansion and Hospital Emergency Department Access: Evidence from the Affordable Care Act,” Annals of Internal Medicine 166 no. 3 (February 2017): 172-179, http://annals.org/aim/article/2593599/insurance-expansion-hospital-emergency-department-access-evidence-from-affordable-care ↩︎
- Eili Klein et al., “The Effect of Medicaid Expansion on Utilization in Maryland Emergency Departments,” Annals of Emergency Medicine epub ahead of print (June 2017), http://www.annemergmed.com/article/S0196-0644(17)30784-9/pdf ↩︎
- Aabha Sharma, Scott Dresden, Emilie Powell, Raymond Kang, Joe Feinglass, “Emergency Department Visits and Hospitalizations for the Uninsured in Illinois Before and After Affordable Care Act Insurance Expansion,” Journal of Community Health 42 no. 3 (June 2017): 591-597, https://link.springer.com/article/10.1007/s10900-016-0293-4 ↩︎
- Gary Pickens et al., “Changes In Hospital Service Demand, Cost, And Patient Illness Severity Following Health Reform,” Health Services Research (May 2019), https://doi.org/10.1111/1475-6773.13165 ↩︎
- Jesse Pines, Rahul Ladhania BTech, Bernard Black , Christopher Corbit, Jestin Carlson, and Arvind Venkat, “Changes in Reimbursement to Emergency Physicians After Medicaid Expansion Under the Patient Protection and Affordable Care Act,” Annals of Emergency Medicine 73, no. 3 (March 2019): 213-224, https://www.sciencedirect.com/science/article/pii/S019606441831374X ↩︎
- Johanna Maclean and Brendan Saloner, “The Effect of Public Insurance Expansions on Substance Use Disorder Treatment: Evidence from the Affordable Care Act,” Journal of Policy Analysis and Management 38, no. 2 (2019): 366-393, https://www.ncbi.nlm.nih.gov/pubmed/30882195 ↩︎
- Christina Andrews et al., “Medicaid Coverage In Substance Use Disorder Treatment After The Affordable Care Act,” Journal of Substance Abuse Treatment epub ahead of print (April 2019), https://www.sciencedirect.com/science/article/pii/S0740547218305750 ↩︎
- Ramin Mojtabai, Christine Mauro, Melanie Wall, Colleen Barry, and Mark Olfson, “The Affordable Care Act and Opioid Agonist Therapy for Opioid Use Disorder,” Psychiatry Online (April 2019), https://doi.org/10.1176/appi.ps.201900025 ↩︎
- Angelica Meinhofer and Allison Witman, “The Role Of Health Insurance On Treatment For Opioid Use Disorders: Evidence From The Affordable Care Act Medicaid Expansion,” Journal of Health Economics 60 (June 2018): 177-197, https://www.sciencedirect.com/science/article/abs/pii/S0167629617311530 ↩︎
- Brendan Saloner, Sachini Bandara, Emma McGinty, and Colleen Barry, “Justice-Involved Adults With Substance Use Disorders: Coverage Increased but Rates of Treatment Did Not in 2014,” Health Affairs 35 no. 6 (June 2016), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2016.0005 ↩︎
- Mark Clapp et al., “Association of Medicaid Expansion With Coverage and Access to Care for Pregnant Women,” Obstetrics & Gynecology 134, no. 5 (November 2019): 1066-1074, https://doi.org/10.1097/aog.0000000000003501 ↩︎
- Rishi Wadhera et al., “Association of the Affordable Care Act’s Medicaid Expansion With Care Quality and Outcomes for Low-Income Patients Hospitalized With Heart Failure,” Circulation: Cardiovascular Quality and Outcomes 11, no. 7 (June 2018), https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.118.004729 ↩︎
- Emanuel Eguia et al., “The Impact of the Affordable Care Act Medicaid Expansion on Vascular Surgery,” Annals of Vascular Surgery Epub ahead of print (January 2020), https://doi.org/10.1016/j.avsg.2020.01.006 ↩︎
- Donald Likosky, Devraj Sukul, Milan Seth, Chang He, Hitlander Gurm, and Richard Prager, “The Association Between Medicaid Expansion and Cardiovascular Interventions: The Michigan Experience,” Journal of the American College of Cardiology 71, no. 9 (March 2018): 1050-1051, https://www.sciencedirect.com/science/article/pii/S0735109718300056?via%3Dihub ↩︎
- Rishi Wadhera et al., “Association of State Medicaid Expansion With Quality of Care and Outcomes for Low-Income Patients Hospitalized With Acute Myocardial Infarction,” JAMA Cardiology 4, no. 2 (January 2019): 120-127, https://jamanetwork.com/journals/jamacardiology/article-abstract/2720425?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamacardio.2018.4577 ↩︎
- Andrew Crocker et al., “Expansion Coverage And Preferential Utilization Of Cancer Surgery Among Racial And Ethnic Minorities And Low-Income Groups,” Surgery epub ahead of print (June 2019), https://www.surgjournal.com/article/S0039-6060(19)30198-9/fulltext ↩︎
- Ehimare Akhabue, Lindsay Pool, Clyde Yancy, Philip Greenland, and Donald Lloyd-Jones, “Association of State Medicaid Expansion With Rate of Uninsured Hospitalizations for Major Cardiovascular Events, 2009-2014,” JAMA Network Open 1, no. 4 (August 2018), https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2698077 ↩︎
- Favel Mondesir et al., “Medicaid Expansion and Hospitalization for Ambulatory Care–Sensitive Conditions Among Nonelderly Adults With Diabetes,” Journal of Ambulatory Care Management epub ahead of print (May 2019), https://insights.ovid.com/pubmed?pmid=31107800 ↩︎
- Andrew Loehrer et al., “Association of the Affordable Care Act Medicaid Expansion with Access to and Quality of Care for Surgical Conditions,” Journal of the American Medical Association Surgery, epub ahead of print (January 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2670459?redirect=true ↩︎
- Cheryl Zogg et al., “Impact of Affordable Care Act Insurance Expansion on Pre-Hospital Access to Care: Changes in Adult Perforated Appendix Admission Rates after Medicaid Expansion and the Dependent Coverage Provision,” Journal of the American College of Surgeons 228, no. 1 (January 2019): 29-43, https://www.journalacs.org/article/S1072-7515(18)32078-7/fulltext ↩︎
- Andrew Admon, Michael Sjoding, Sarah Lyon, John Ayanian, Theodore Iwashyna, and Colin Cooke, “Medicaid Expansion and Mechanical Ventilation in Asthma, Chronic Obstructive Pulmonary Disease, and Heart Failure,” Annals of the American Thoracic Society epub ahead of print (February 2019), https://www.atsjournals.org/doi/pdf/10.1513/AnnalsATS.201811-777OC ↩︎
- John Scott et al., “Lifting the Burden: State Medicaid Expansion Reduces Financial Risk for the Injured,” Journal of Trauma and Acute Care Surgery Epub ahead of print (September 2019), https://doi.org/10.1097/ta.0000000000002493 ↩︎
- Charles A. Daly et al., “The Effects of Medicaid Expansion on Triage and Regional Transfer After Upper-Extremity Trauma,” The Journal of Hand Surgery 44, no. 9 (September 2019): 720-727, https://doi.org/10.1016/j.jhsa.2019.05.020 ↩︎
- Cheryl Zogg et al., “Association of Medicaid Expansion With Access to Rehabilitative Care in Adult Trauma Patients,” JAMA Surgery epub ahead of print (January 2019), https://jamanetwork.com/journals/jamasurgery/article-abstract/2719270?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamasurg.2018.5177 ↩︎
- Manzilat Akande Peter Minneci, Katherine Deans, Henry Xiang, and Jennifer Cooper, “Association of Medicaid Expansion Under the Affordable Care Act With Outcomes and Access to Rehabilitation in Young Adult Trauma Patients,” JAMA Surgery 153, no. 8 (August 2018), https://jamanetwork.com/journals/jamasurgery/article-abstract/2682872?widget=personalizedcontent&previousarticle=2719270 ↩︎
- Neal Bhutiani, Brian Harbrecht, Charles Scoggins, and Matthew Bozeman, “Evaluating The Early Impact Of Medicaid Expansion On Trends In Diagnosis And Treatment Of Benign Gallbladder Disease In Kentucky,” The American Journal of Surgery (January 2019), https://www.americanjournalofsurgery.com/article/S0002-9610(18)30894-8/fulltext ↩︎
- Emanuel Eguia et al., “Impact of the Affordable Care Act (ACA) Medicaid Expansion on Cancer Admissions and Surgeries,” Annals of Surgery 268, no. 4 (October 2018): 584-590, https://journals.lww.com/annalsofsurgery/Abstract/2018/10000/Impact_of_the_Affordable_Care_Act__ACA__Medicaid.6.aspx ↩︎
- J.W. Awori Hayanga et al., “Lung Transplantation and Affordable Care Act Medicaid Expansion in the Era of Lung Allocation Score” Transplant International epub ahead of print (February 2019), https://onlinelibrary.wiley.com/doi/pdf/10.1111/tri.13420 ↩︎
- Meera Harhay et al., “Association between Medicaid Expansion under the Affordable Care Act and Preemptive Listings for Kidney Transplantation,” Clinical Journal of the American Society of Nephrology 13 (July 2018), https://cjasn.asnjournals.org/content/13/7/1069 ↩︎
- Meera N. Harhay, Ryan M. McKenna, and Michael O. Harhay, “Association Between Medicaid Expansion Under the Affordable Care Act and Medicaid-Covered Pre-emptive Kidney Transplantation,” Journal of General Internal Medicine 34, no. 11 (November 2019): 2322-2325, https://doi.org/10.1007/s11606-019-05279-x ↩︎
- Dmitry Tumin et al., “Medicaid Participation among Liver Transplant Candidates after the Affordable Care Act Medicaid Expansion” Journal of the American College of Surgeons 225, no. 2 (August 2017): 173-180.e2, https://www.journalacs.org/article/S1072-7515(17)30454-4/fulltext ↩︎
- Dmitry Tumin, Don Hayes Jr., Kenneth Washburn, Joseph Tobias, and Sylvester Black, “Medicaid Enrollment after Liver Transplantation: Effects of Medicaid Expansion,” Liver Transplantation (May 2016), https://aasldpubs.onlinelibrary.wiley.com/doi/full/10.1002/lt.24480 ↩︎
- Ramiro Manzano-Nunez et al., “Association of Medicaid Expansion Policy with Outcomes in Homeless Patients Requiring Emergency General Surgery,” World Journal of Surgery 43, no. 6 (June 2019): 1483-1489, https://link.springer.com/article/10.1007/s00268-019-04932-0 ↩︎
- Susan Camilleri, “The ACA Medicaid Expansion, Disproportionate Share Hospitals, and Uncompensated Care” Health Services Research epub ahead of print (May 2017), http://onlinelibrary.wiley.com/doi/10.1111/1475-6773.12702/abstract ↩︎
- Jordan Rhodes, Thomas Buchmueller, Helen Levy, and Sayeh Nikpay, “Heterogeneous Effects Of The Aca Medicaid Expansion On Hospital Financial Outcomes,” Contemporary Economic Policy epub ahead of print (April 2019), https://onlinelibrary.wiley.com/doi/full/10.1111/coep.12428 ↩︎
- Tyler McClintock, Ye Wang, Mahek Shah, Benjamin Chung, and Steven Chang, “How Have Hospital Pricing Practices for Surgical Episodes of Care Responded to Affordable Care Act-Related Medicaid Expansion?” Urology 125 (March 2019): 79-85, https://doi.org/10.1016/j.urology.2018.10.034 ↩︎
- Brystana Kaufman, Kristin Reiter, George Pink, and George Holmes, “Medicaid Expansion Affects Rural and Urban Hospitals Differently,” Health Affairs 35 no. 9 (September 2016): 1665-1672, http://content.healthaffairs.org/content/35/9/1665.full?sid=4aea494e-8e02-4c66-8298-3c828bfc313b ↩︎
- Charles A. Daly et al., “The Effects of Medicaid Expansion on Triage and Regional Transfer After Upper-Extremity Trauma,” The Journal of Hand Surgery 44, no. 9 (September 2019): 720-727, https://doi.org/10.1016/j.jhsa.2019.05.020 ↩︎
- Michael McCue, “The Impact of Medicaid Expansion on Medicaid Focused Insurers in California,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 52 (July 2015), http://inq.sagepub.com/content/52/0046958015595960.full.pdf+html ↩︎
- Steven Wallace, Maria-Elena Young, Michael Rodriguez, Amy Bonilla, and Nadereh Pourat, Community Health Centers Play a Critical Role in Caring for the Remaining Uninsured in the Affordable Care Act Era (UCLA Center for Health Policy Research, October 2016), http://healthpolicy.ucla.edu/publications/Documents/PDF/2016/FQHC_PB-oct2016.pdf ↩︎
- Matt Warfield, Barbara DiPietro, and Samantha Artiga, How has the ACA Medicaid Expansion Affected Providers Serving the Homeless Population: Analysis of Coverage, Revenues, and Costs (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, March 2016), http://files.kff.org/attachment/issue-brief-how-has-the-aca-medicaid-expansion-affected-providers-serving-the-homeless-population ↩︎
- Jane Wishner, Patricia Solleveld, Robin Rudowitz, Julia Paradise, and Larisa Antonisse, A Look at Rural Hospital Closures and Implications for Access to Care: Three Case Studies (Washington, DC: Kaiser Commission on Medicaid and the Uninsured and The Urban Institute, July 2016), http://kff.org/medicaid/issue-brief/a-look-at-rural-hospital-closures-and-implications-for-access-to-care/ ↩︎
- Laurie Felland, Peter Cunningham, Annie Doubleday, and Cannon Warren, Effects of the Affordable Care Act on Safety Net Hospitals (Washington, DC: Mathematica Policy Research, prepared for the Assistant Secretary for Planning and Evaluation, November 2016), https://aspe.hhs.gov/sites/default/files/pdf/255491/SafetyNetHospital.pdf ↩︎
- Rachel Garfield, Elizabeth Hinton, Elizabeth Cornachione, and Cornelia Hall, Medicaid Managed Care Plans and Access to Care: Results from the Kaiser Family Foundation 2017 Survey of Medicaid Managed Care Plans (Washington, DC: Kaiser Family Foundation, March 2018), https://modern.kff.org/medicaid/report/medicaid-managed-care-plans-and-access-to-care-results-from-the-kaiser-family-foundation-2017-survey-of-medicaid-managed-care-plans ↩︎
- Richard Lindrooth, Marcelo Perraillon, Rose Hardy, and Gregory Tung, “Understanding the Relationship Between Medicaid Expansions and Hospital Closures,” Health Affairs epub ahead of print (January 2018), https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2017.0976 ↩︎
- Allen Dobson, Joan DaVanzo, Randy Haught, and Phap Hoa Luu, Comparing the Affordable Care Act’s Financial Impact on Safety-Net Hospitals in States that Expanded Medicaid and Those That Did Not (The Commonwealth Fund, November 2017), http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2017/nov/dobson_impact_medicaid_expanion_safety_net_hosps_ib.pdf ↩︎
- Jordan Rhodes, Thomas Buchmueller, Helen Levy, and Sayeh Nikpay, “Heterogeneous Effects Of The Aca Medicaid Expansion On Hospital Financial Outcomes,” Contemporary Economic Policy epub ahead of print (April 2019), https://onlinelibrary.wiley.com/doi/full/10.1111/coep.12428 ↩︎
- Fredric Blavin, How Has the ACA Changed Finances for Different Types of Hospitals? Updated Insights from 2015 Cost Report Data (The Urban Institute, April 2017), http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2017/rwjf436310 ↩︎
- Mark Duggan, Atul Gupta, and Emilie Jackson, The Impact of the Affordable Care Act: Evidence from California’s Hospital Sector (National Bureau of Economic Research, working paper no. 25488, January 2019), https://www.nber.org/papers/w25488.pdf ↩︎
- Peter Cunningham, Rachel Garfield, and Robin Rudowitz, How Are Hospitals Faring Under the Affordable Care Act? Early Experiences from Ascension Health (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, April 2015), http://kff.org/health-reform/issue-brief/how-are-hospitals-faring-under-the-affordable-care-act-early-experiences-from-ascension-health/ ↩︎
- Peter Cunningham, Rachel Garfield, and Robin Rudowitz, How Are Hospitals Faring Under the Affordable Care Act? Early Experiences from Ascension Health (Washington, DC: Kaiser Commission on Medicaid and the Uninsured, April 2015), http://kff.org/health-reform/issue-brief/how-are-hospitals-faring-under-the-affordable-care-act-early-experiences-from-ascension-health/ ↩︎
- Rachel Garfield, Elizabeth Hinton, Elizabeth Cornachione, and Cornelia Hall, Medicaid Managed Care Plans and Access to Care: Results from the Kaiser Family Foundation 2017 Survey of Medicaid Managed Care Plans (Washington, DC: Kaiser Family Foundation, March 2018), https://modern.kff.org/medicaid/report/medicaid-managed-care-plans-and-access-to-care-results-from-the-kaiser-family-foundation-2017-survey-of-medicaid-managed-care-plans ↩︎
- Hefei Wen, Kenton J. Johnston, Lindsay Allen, and Teresa M. Waters, “Medicaid Expansion Associated With Reductions In Preventable Hospitalizations,” Health Affairs 38, no. 11 (November 2019): 1845-1849, https://doi.org/10.1377/hlthaff.2019.00483 ↩︎
- Ramiro Manzano-Nunez et al., “Association of Medicaid Expansion Policy with Outcomes in Homeless Patients Requiring Emergency General Surgery,” World Journal of Surgery 43, no. 6 (June 2019): 1483-1489, https://link.springer.com/article/10.1007/s00268-019-04932-0 ↩︎
- Elizabeth A. Brown et al., “The Impact of the ACA Medicaid Expansion on Access to Care and Hospitalization Charges for Lupus Patients,” Arthritis Care & Research Epub ahead of print (September 2019), https://doi.org/10.1002/acr.24080 ↩︎
- Emanuel Eguia et al., “The Impact of the Affordable Care Act (ACA) Medicaid Expansion on Access to Minimally Invasive Surgical Care,” The American Journal of Surgery Epub ahead of print (July 2019), https://doi.org/10.1016/j.amjsurg.2019.07.003 ↩︎
- Gary Young, Stephen Flaherty, E. Zepeda, Simone Singh, and Sara Rosenbaum, “Impact of ACA Medicaid Expansion on Hospitals’ Financial Status” Journal of Healthcare Management 64, no. 2 (March 2019): 91–102, https://insights.ovid.com/crossref?an=00115514-201904000-00007 ↩︎
- James Richardson, Jared Llorens, and Roy Heidelberg, Medicaid Expansion and the Louisiana Economy (Louisiana Department of Health, March 2018), http://gov.louisiana.gov/assets/MedicaidExpansion/MedicaidExpansionStudy.pdf ↩︎
- James A. Richardson, Jared J. Llorens, and Roy L. Heidelberg. Medicaid Expansion and the Louisiana Economy, 2018 and 2019 (Louisiana Department of Health, Prepared by Louisiana State University, August 2019), http://ldh.la.gov/assets/media/3and4.2019FinalReportMedicaidExpansionstudy.pdf ↩︎
- Deloitte Development LLC, Commonwealth of Kentucky Medicaid Expansion Report, (Deloitte Development LLC, February 2015), http://jointhehealthjourney.com/images/uploads/channel-files/Kentucky_Medicaid_Expansion_One-Year_Study_FINAL.pdf ↩︎
- The Colorado Health Foundation, Assessing the Economic and Budgetary Impact of Medicaid Expansion in Colorado, (The Colorado Health Foundation, March 2016), https://www.coloradohealth.org/sites/default/files/documents/2017-01/Medicaid_ExecutiveSummary_ONLINE.pdf ↩︎
- John Ayanian, Gabriel Ehrlich, Donald Grimes, and Helen Levy, “Economic Effects of Medicaid Expansion in Michigan,” The New England Journal of Medicine epub ahead of print (January 2017), http://www.nejm.org/doi/full/10.1056/NEJMp1613981 ↩︎
- Aparna Soni, Marguerite Burns, Laura Dague, and Kosali Simon, “Medicaid Expansion and State Trends in Supplemental Security Income Program Participation,” Health Affairs 36 no. 8, (August 2017): 1485-1488, http://content.healthaffairs.org/content/36/8/1485.full?sid=982b20c0-0a17-4dc4-a35a-b0302d4ec289 ↩︎
- Renuka Tipirneni et al., “Association of Medicaid Expansion With Enrollee Employment and Student Status in Michigan,” JAMA Network Open 3, no. 1 (January 2020), https://doi.org/10.1001/jamanetworkopen.2019.20316 ↩︎
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553 ↩︎
- Jean Hall, Adele Shartzer, Noelle Kurth, and Kathleen Thomas, “Medicaid Expansion as an Employment Incentive Program for People With Disabilities,” American Journal of Public Health epub ahead of print (July 2018), https://ajph.aphapublications.org/doi/pdf/10.2105/AJPH.2018.304536 ↩︎
- Kevin Callison and Paul Sicilian, “Economic Freedom and the Affordable Care Act: Medicaid Expansions and Labor Mobility by Race and Ethnicity,” Public Finance Review 46, no. 2 (March 2018), https://journals.sagepub.com/doi/abs/10.1177/1091142116668254 ↩︎
- Bryce Ward and Brandon Bridge, The Economic Impact of Medicaid Expansion in Montana: Updated Findings (Bureau of Business and Economic Research, January 2019), https://mthcf.org/wp-content/uploads/2019/01/Economic-Impact-of-MedEx-in-MT_1.28.19-FINAL.pdf ↩︎
- The Ohio Department of Medicaid, 2018 Ohio Medicaid Group VIII Assessment: A Follow‐Up to the 2016 Ohio Medicaid Group VIII Assessment, (The Ohio Department of Medicaid, August 2018), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Final-Report.pdf An older version of this Ohio report (see citation below) found that as of 2016, 74.8% of expansion enrollees who were unemployed but looking for work reported that Medicaid enrollment made it easier to seek employment and 52.1% of expansion enrollees who were employed reported that Medicaid enrollment made it easier to continue working. The Ohio Department of Medicaid, Ohio Medicaid Group VIII Assessment: A Report to the Ohio General Assembly (The Ohio Department of Medicaid, January 2017), https://medicaid.ohio.gov/Portals/0/Resources/Reports/Annual/Group-VIII-Assessment.pdf ↩︎
- Renuka Tipirneni et al., “Changes in Health and Ability to Work Among Medicaid Expansion Enrollees: a Mixed Methods Study” Journal of General Internal Medicine 34, no. 2 (February 2019): 272-280, https://link.springer.com/article/10.1007/s11606-018-4736-8 ↩︎
- Susan Dorr Goold et al., “Primary Care Clinicians’ Views About the Impact of Medicaid Expansion in Michigan: A Mixed Methods Study,” Journal of General Internal Medicine 33, no. 8 (June 2018): 1307-1316, https://link.springer.com/article/10.1007/s11606-018-4487-6 ↩︎
- Renuka Tipirneni et al., “Association of Expanded Medicaid Coverage With Health and Job-Related Outcomes Among Enrollees With Behavioral Health Disorders,” Psychiatric Services Epub ahead of print (September 2019), https://doi.org/10.1176/appi.ps.201900179 ↩︎
- Heeju Sohn and Stefan Timmermans, “Social Effects of Health Care Reform: Medicaid Expansion under the Affordable Care Act and Changes in Volunteering,” Socius: Socialogical Research for a Dynamic World 3 (March 2017): 1-12, http://journals.sagepub.com/doi/full/10.1177/2378023117700903 ↩︎
- Lizhong Peng, Xiaohui Guo, and Chad D. Meyerhoefer, “The Effects of Medicaid Expansion on Labor Market Outcomes: Evidence from Border Counties,” Health Economics Epub ahead of print (December 2019), https://doi.org/10.1002/hec.3976 ↩︎
- Olga Scrivner et al., “Job Postings in the Substance Use Disorder Treatment Related Sector During the First Five Years of Medicaid Expansion,” PLoS One 15, no. 1 (January 2020), https://doi.org/10.1371/journal.pone.0228394 ↩︎
- Lucie Schmidt, Lara Shore-Sheppard, and Tara Watson, The Impact of the ACA Medicaid Expansion on Disability Program Applications (National Bureau of Economic Research, Working Paper No. 26192, August 2019), http://www.nber.org/papers/w26192 ↩︎
- Thomas C. Buchmueller, Helen G. Levy, and Robert G. Valletta, Medicaid Expansion and the Unemployed (National Bureau of Economic Research, Working Paper No. 26553, December 2019), http://www.nber.org/papers/w26553 ↩︎
- Kevin Callison and Paul Sicilian, “Economic Freedom and the Affordable Care Act: Medicaid Expansions and Labor Mobility by Race and Ethnicity,” Public Finance Review 46, no. 2 (March 2018), https://journals.sagepub.com/doi/abs/10.1177/1091142116668254 ↩︎
- Pauline Leung and Alexandre Mas, Employment Effects of the ACA Medicaid Expansions (Working Paper No. 22540, National Bureau of Economic Research, August 2016), http://www.nber.org/papers/w22540 ↩︎
- Angshuman Gooptu, Asako Moriya, Kosali Simon, and Benjamin Sommers, “Medicaid Expansion Did Not Result in Significant Employment Changes or Job Reductions in 2014,” Health Affairs 35, no. 1 (January 2016): 111-118, 1-12, http://content.healthaffairs.org/content/35/1/111.short ↩︎
- Bowen Garrett and Robert Kaestner, Recent Evidence on the ACA and Employment: Has the ACA Been a Job Killer? (Washington, DC: The Urban Institute and the Robert Wood Johnson Foundation, August 2015), http://www.urban.org/research/publication/recent-evidence-aca-and-employment-has-aca-been-job-killer/view/full_report ↩︎
- Robert Kaestner, Bowen Garrett, Anuj Gangopadhyaya, and Caitlyn Fleming, Effects of ACA Medicaid Expansions on Health Insurance Coverage and Labor Supply (Working Paper No. 21836, National Bureau of Economic Research, December 2015), http://www.nber.org/papers/w21836 ↩︎
- Priyanka Anand, Jody Schimmel Hyde, Maggie Colby, and Paul O’Leary, “The Impact of Affordable Care Act Medicaid Expansions on Applications to Federal Disability Programs,” Forum for Health Economics and Policy (February 2019), https://www.ncbi.nlm.nih.gov/pubmed/30796844 ↩︎
- Emily Brown, Michelle Garrison, Hao Bao, Pingping Qu, Carole Jenny, and Ali Rowhani-Rahbar, “Assessment of Rates of Child Maltreatment in States With Medicaid Expansion vs States Without Medicaid Expansion,” JAMA Network Open 2, no. 6 (June 2019), https://jamanetwork.com/journals/jamanetworkopen/article-abstract/2735758 ↩︎
- Michel Boudreaux, James M. Noon, Brett Fried, and Joanne Pascale, “Medicaid Expansion and the Medicaid Undercount in the American Community Survey,” Health Services Research 54, no. 6 (December 2019): 1263-1272, https://doi.org/10.1111/1475-6773.13213 ↩︎
- David Slusky and Donna Ginther, Did Medicaid Expansion Reduce Medical Divorce? (Working Paper No. 23139, National Bureau of Economic Research, February 2017), http://www.nber.org/papers/w23139?utm_campaign=ntw&utm_medium=email&utm_source=ntw ↩︎
- Lucas Goodman, “The Effect of the Affordable Care Act Medicaid Expansion on Migration,” Journal of Policy Analysis 36, no. 1 (November 2016): 211-238, http://onlinelibrary.wiley.com/doi/10.1002/pam.21952/abstract ↩︎
- Joshua Clinton and Michael Sances, “The Politics of Policy: The Initial Mass Political Effects of Medicaid Expansion in the States,” American Political Science Review 112, no. 1 (February 2018): 167-185, https://www.cambridge.org/core/journals/american-political-science-review/article/politics-of-policy-the-initial-mass-political-effects-of-medicaid-expansion-in-the-states/246AA0F10B44EFD62A7B27C661730823 ↩︎
- Jake Haselswerdt, “Expanding Medicaid, Expanding the Electorate: The Affordable Care Act’s Short-Term Impact on Political Participation,” Journal of Health Politics, Policy, and Law 42, no. 4 (August 2017), https://read.dukeupress.edu/jhppl/article-abstract/42/4/667/130386/Expanding-Medicaid-Expanding-the-Electorate-The?redirectedFrom=fulltext ↩︎
- Daniel Hopkins and Kalind Parish, “The Medicaid Expansion and Attitudes toward the Affordable Care Act: Testing for a Policy Feedback on Mass Opinion,” Public Opinion Quarterly 83, no. 1 (April 2019): 123-134, https://academic.oup.com/poq/article-abstract/83/1/123/5430239 ↩︎
- Michael Sances and Joshua Clinton, New Policy, New Politics? The Effect of Medicaid Expansion on Public Support for the Affordable Care Act, (University of Memphis and Vanderbilt University, February 2017), https://csap.yale.edu/sites/default/files/files/apppw_jc2_3-8-17.pdf ↩︎
- Richard Fording and Dana Patton, “Medicaid Expansion and the Political Fate of the Governors Who Support It,” Policy Studies Journal 47, no. 2 (January 2019), https://onlinelibrary.wiley.com/doi/full/10.1111/psj.12311 ↩︎