Note: Figures 12 and 13 were updated on April 26, 2024.
Introduction
The June 2022 Supreme Court ruling in the case Dobbs v. Jackson Women’s Health Organization has significant implications for racial disparities in health and health care. The decision overturned the longstanding Constitutional right to abortion and eliminated federal standards on abortion access that had been in place for nearly 50 years in all states across the country. As a result of Dobbs, large swaths of the country lack abortion access, with a disproportionate impact on those residing in the South and Midwest.
As of April 2024, 14 states have implemented abortion bans, 11 states have placed gestational limits on abortion between 6 and 22 weeks, and 25 states and the District of Columbia provide broader access to abortions after 22 weeks gestation. (This reflects Arizona being counted in the gestational limits category, as implementation of a recently upheld Civil War-era law banning nearly all abortions in the state is still pending amid ongoing court actions.)
Pregnant women seeking abortion that reside in states that prohibit or restrict abortions either have to travel out of state or try to obtain medication abortion pills via a telehealth appointment with an out-of-state clinician, but these options are not accessible to everyone. Some women may turn to self-managed abortions, but some will not be able to obtain an abortion and have to continue a pregnancy they do not want. Additionally, there have been reports of clinicians in states with bans and early gestational limits leaving their states due to the restrictions and criminalization for care that they provide, potentially exacerbating provider shortages in some areas.
With these state-level restrictions in place, people of color residing in those states may face disproportionately greater challenges accessing abortions due to longstanding underlying social and economic inequities, which could exacerbate existing disparities in maternal and infant health. This analysis examines the implications of state restrictions on abortion coverage for racial disparities in access to care and health outcomes. It is based on KFF analysis of data from the Centers for Disease Control and Prevention (CDC), American Community Survey (ACS), Behavioral Risk Factor Surveillance Survey (BRFSS), and Survey of Household Economics and Decisionmaking (SHED) (see Methods). Throughout this brief we refer to “women” but recognize that some individuals who have abortions do not identify as women, including transgender. Key takeaways include the following:
- Black and American Indian and Alaska Native (AIAN) women ages 18-49 are more likely than other groups to live in states with abortion bans and restrictions. About six in ten Black (60%) and AIAN (59%) women ages 18-49 living in states with abortion bans or restrictions compared with just over half (53%) of White, less than half of Hispanic (45%), and about three in ten Asian (28%) and Native Hawaiian or Pacific Islander (NHPI) (29%) women ages 18-49.
- Many groups of women of color have higher uninsured rates compared to their White counterparts, and, across racial and ethnic groups, uninsured rates are higher in states with abortion bans or restrictions than in those that provide broader abortion access. Among women ages 18-49, roughly a fifth of AIAN (22%) and Hispanic (21%) women are uninsured as are 14% of NHPI women and 11% of Black women compared with less than one in ten (7%) of White women. Moreover, uninsured rates for women ages 18-49 are at least twice as high in states that banned abortion compared to those in states with broader access for White (10% vs. 5%), Hispanic (33% vs. 15%), Black (14% vs. 7%), and Asian (10% vs. 5%) women, and nearly three times higher for NHPI women (29% vs. 10%).
- Women of color have more limited financial resources and transportation options than White women, making it more difficult for them to travel out-of-state for an abortion. Some may also face linguistic barriers and have immigration-related fears that create additional challenges to accessing abortions.
- The bans and restrictions on abortions may widen the already stark racial disparities in maternal health, especially since some states do not explicitly have exceptions that allow abortion services when pregnancy is jeopardizing a woman’s health. The restrictions may also contribute to growing provider shortages in some areas, as clinicians are responding to concerns about criminalization and prohibited from offering the full spectrum of pregnancy care. Moreover, abortion restrictions may have negative economic consequences on families and put pregnant people at increased risk for criminalization.
While there have been large inequities in abortion access for many years, the Dobbs ruling opened the door to widening those differences further. Black and AIAN women are more likely to live in states with abortion bans or restrictions. While data on the impact of Dobbs to date on health outcomes is limited to date, many indicators suggest that the ruling may exacerbate longstanding large disparities in maternal and infant health. The issue also has moved to the forefront of policy debates in the U.S. Sixteen percent of women voters, rising to 28% of Black women voters, say abortion is the “most important issue” to their vote in the 2024 presidential election.
How do Abortion Rates Vary by Race and Ethnicity?
Data on abortions by race and ethnicity are limited. The federal Abortion Surveillance System from the CDC has been providing annual national and state-level statistics on abortion for decades, based on data that is voluntarily reported by states, DC, and New York City. While most states participate, one notable exception is California, which has many protections for abortion access and is one of the most racially diverse states in the nation. Furthermore, availability of data by race and ethnicity varies among states. The most recent data in the Abortion Surveillance System, from 2021, only includes racial and ethnic data from 31 states and DC and is generally only available for White, Black, and Hispanic women. While we present the data from the Abortion Surveillance System in this brief, we recognize these limitations.
Prior to Dobbs, the abortion rate was higher among Black and Hispanic women compared to their White peers. As of 2021, the abortion rate was 28.6 per 1,000 women among Black women, compared to 12.3 per 1,000 among Hispanic women, and 6.4 per 1,000 among White women (Figure 1). Data for other racial and ethnic groups were not available. The vast majority of abortions across racial and ethnic groups are in the first trimester. Approximately eight in ten abortions among White (82%), Hispanic (82%), and Black women (80%) occur by nine weeks of pregnancy. While data on the number of abortions post-Dobbs has been released by both the #WeCount project from the Society for Family Planning and the Guttmacher Institute’s Monthly Abortion Provision Study, neither sets of data have reported demographic characteristics of abortion patients.

There are many reasons why abortion rates are higher among some women of color. As discussed below, Black, Hispanic, American Indian and Alaska Native (AIAN), and Native Hawaiian or Pacific Islander (NHPI) women have more limited access to health care, which affects their access to contraception and other sexual health services that are important for pregnancy planning. Data show that contraception use is higher among White women (69%) compared to Black (61%) and Hispanic (61%) women. Some women of color live in areas with more limited access to comprehensive contraceptive options. In addition, the health care system has a long history of racist practices targeting the sexual and reproductive health of people of color, including forced sterilization, medical experimentation, the systematic reduction of midwifery, just to name a few. Many women of color also report discrimination by providers, with reports of dismissive treatment, assumption of stereotypes, and inattention to conditions that take a disproportionate toll on women of color and certain conditions, such as uterine fibroids. These factors have contributed to medical mistrust, which some women cite as a reason that they may not access contraception. In addition, inequities across broader social and economic factors — such as income, housing, safety and education—that drive health, often referred to as social determinants of health, affect decisions related to family planning and reproductive health.
How Do State Abortion Policies Vary Across Racial and Ethnic Groups?
Overall, 16.3 million or 25% of women ages 18-49 in the US live in one of the 14 states where abortion is banned, and another 16.9 million, or 26%, live in one of the 11 states with gestational limits between 6 and 22 weeks LMP. The remaining 32.8 million, or roughly 50%, live in states that provide broader access to abortions.
White, Black, and American Indian and Alaska Native women account for larger shares of women ages 18-49 in states that have banned or limited abortion access compared to states that provide broader access to abortion. Most of the states that have banned or restricted abortion are in the South, where more than half of the Black population and roughly a third of the White (36%) and AIAN (31%) population reside. In contrast, Hispanic and Asian women make up larger shares of women ages 18-49 in states that provide broader access to abortion compared to states with abortion bans or limits. (See Appendix Table B for the racial and ethnic distribution of women ages 18-49 by state).

Six in ten of Black (60%) and AIAN (59%) women ages 18-49 live in states with abortion bans or restrictions (Figure 3). Just over half (53%) of White women ages 18-49 live in states with bans or restrictions, while less than half of Hispanic (45%) and about three in ten Asian (28%) and NHPI (29%) women ages 18-49 live in these states. Of note, in April 2024, the Arizona State Supreme Court upheld a Civil War era law banning nearly all abortions in the state. While that law is not currently in effect, if it were to go into effect in the future, the share of AIAN women living in a state with an abortion ban would rise from about three in ten (31%) to about four in ten (41%), and the share of Hispanic women living in a state with an abortion ban would increase from 24% to 28%.
How do potential barriers to accessing abortions vary by race and ethnicity?
Variation in abortion policies by state due to the Dobbs decision will likely result in women of color facing disproportionate access barriers since they face underlying disparities in health coverage and have more limited financial resources that may make it challenging to obtain an abortion out-of-state or via telehealth.
Health Coverage
Lack of health insurance limits women’s access to a broad range of health services, including contraception and pregnancy care, and leaves them at risk for significant out of pocket expenses for care. However, having coverage does not guarantee that it includes abortion benefits. In general coverage of abortion is more limited than for many other common health services. Some states prohibit coverage of abortion in state-regulated private insurance plans, and federal law bars the use of federal dollars for abortion, including in Medicaid, the national health coverage program for low-income individuals.
AIAN, Hispanic, NHPI, and Black women between ages 18-49 have higher uninsured rates compared to their White counterparts. Among women in this age group, roughly a fifth of AIAN (22%) and Hispanic (21%) women are uninsured as are 14% of NHPI women and 11% of Black women. In contrast, less than one in ten (7%) of White women lack insurance (Figure 4). These differences in uninsured rates are driven by lower rates of private coverage among these groups. Medicaid coverage helps to narrow these differences but does not fully offset them.

Across racial and ethnic groups, uninsured rates for women ages 18-49 in states that have banned or limited abortion are higher than rates in states where abortion is available beyond 22 weeks. Overall, 16% of women ages 18-49 in states that have banned abortion are uninsured compared to 12% in states that have gestational limits on abortions less than 22 weeks and 8% in states that have broader access to abortions. Uninsured rates for women ages 18-49 are at least twice as high in states that banned abortion compared to those in states with broader access for White (10% vs. 5%), Hispanic (33% vs. 15%), Black (14% vs. 7%), and Asian (10% vs. 5%) women, and nearly three times higher for NHPI women (29% vs. 10%) (Figure 5). However, even in states where abortion is not banned, many women do not have coverage, and uninsured rates remain higher for AIAN, Hispanic, and NHPI women compared to White women.

AIAN, Black, NHPI, and Hispanic women are more likely than their White counterparts to be covered by Medicaid, which provides limited coverage for abortions. For decades, the Hyde Amendment has prohibited the use of federal funds for coverage of abortion under Medicaid, except in cases of rape, incest, or life endangerment for the pregnant person. States can choose to use state funds to pay for abortions under Medicaid in other instances. However, among the 36 states that do not ban abortion, 17 use state funds to pay for abortions beyond the Hyde limitations for Medicaid enrollees. The other 19 states and DC continue to follow the Hyde limits, meaning women in these states covered by Medicaid likely must pay out of pocket for an abortion unless they meet the narrow circumstances of the Hyde Amendment.
Social and Economic Access Barriers
Women of color have more limited financial resources and transportation options than White women, making it more difficult for them to travel out-of-state for an abortion. The median self-pay cost of obtaining an abortion exceeded $500 in 2021, but costs can vary depending on the type of abortion, location, and if an individual has coverage. Traveling out of state raises the cost of abortion due to added costs for transportation, accommodation, and childcare. Moreover, it may result in more missed work, meaning greater loss of pay. Data suggest that women of color would have more difficulty than White women affording these increased costs and may face other barriers that could prevent them from traveling to obtain an abortion and instead turning to self-managed abortions or continuing the pregnancies.
Overall, AIAN (48%), Black (43%), NHPI (41%) and Hispanic (40%) women ages 18-49 are nearly twice as likely as their White counterparts (24%) to have low incomes (below 200% of the federal poverty level or $46,060 for a family of three as of 2022) (Figure 6). Moreover, across most racial and ethnic groups, women in states that have banned abortion are more likely to have low incomes than women in states that allow abortions beyond 22 weeks. For example, 48% of NHPI women in states that have banned abortion have low incomes compared to 38% of NHPI women in states where abortion is available after 22 weeks gestation. (See Appendix Table C for state-level data on the share of women who are low-income by race and ethnicity.)

Over half of Hispanic (57%) and Black women (58%) ages 18-49 could not cover an emergency expense of at least $500 using their current savings compared to 36% of White women in this age group (Figure 7). (Data for this measure were not available for other racial groups.) Women who have fewer resources for an emergency expense may be more likely to seek assistance from an abortion fund, which help cover the costs of abortions for people who cannot afford them. However, abortion funds are not able to keep up with the demand and support all those seeking assistance.

Black women ages 18-49 are more likely than their White counterparts to live in a household without access to a vehicle (12% vs. 4%), and Asian and AIAN women in this age group are more likely than White women to lack vehicle access (9% and 8%, respectively, vs. 4%) (Figure 8). Hispanic and NHPI women are also more likely than White women to lack vehicle access, although the difference is smaller (6% and 6%, respectively, vs 4%). Research shows that out-of-state travel for abortion care has risen significantly since Dobbs, but women without vehicle access may face greater challenges to traveling out of state.

Immigration-related fears make some women reluctant to travel out of state for an abortion. Among women ages 18-49, about one-third of Asian women (33%) and roughly a quarter of Hispanic (24%) and NHPI (22%) women are noncitizens, who include lawfully present and undocumented immigrants (Figure 9). Many citizen women may also live in mixed immigration status families, which may include noncitizen family members. Noncitizen women and those living in mixed immigration status families may fear that traveling out of state could put them or a family member at risk for negative impacts on their immigration status or detention or deportation, especially in states that have moved to criminalize abortions. For example, some states have enacted laws that make it illegal to “aid or abet” someone in obtaining an abortion while some are trying to make it illegal to take a minor across state lines to obtain an abortion.

Differences in language barriers and access to technology may also contribute to racial disparities in abortion access. Roughly a quarter of Hispanic (26%) and Asian (25%) women ages 18-49 speak English “less than very well,” as do one in ten NHPI women (10%) compared to just 1% of White women (Figure 10). This can affect their ability to find information about abortions and locate a clinic that offers abortion services. In a national KFF survey of women conducted just before the Dobbs ruling, nearly three in ten Hispanic women (29%) said if they needed an abortion, they did not know where to go or find the information, higher than other groups. Internet access is another important factor for finding information about abortion care and also for telehealth appointments, which comprise a growing share of abortion care. Among women ages 18-49, 8% of AIAN and 6% of NHPI (6%) women live in a household without internet access, compared to 2% of White women (Figure 10).

What are the Potential Implications of Abortion Restrictions on Racial Disparities in Health, Finances, and Criminal Penalties?
Stark racial disparities in maternal and infant health predate the Dobbs decision but may widen due to the new restrictions on abortions since abortion services can be a key factor in managing pregnancy complications and emergencies that can lead to poor outcomes. Data suggest that the abortion restrictions may also contribute to growing provider shortages in some areas, which may increase access challenges and have negative impacts on health. Moreover, abortion restrictions may have negative economic consequences on families and put people at increased risk for criminalization.
Maternal Health
Prior to the Dobbs ruling there were already significant racial disparities in pregnancy-related and infant mortality, which may widen due to abortion restrictions. NHPI, Black and AIAN people are more likely to die while pregnant or within a year of the end of pregnancy compared to White people (62.8, 39.9 and 32.0 per 100,000 births vs. 14.1 per 100,000 births) (Figure 11). Restrictions on access to abortions limit options to terminate pregnancies for medical reasons. While all state bans have some limited exceptions to preserve the life of pregnant women, the language of these exceptions is vague and narrow, and far fewer have health exceptions. This means that some people have been forced to remain pregnant even when the pregnancy is threatening their health, which could further widen disparities. One study estimated that a total abortion ban in the U.S. would increase the number of pregnancy-related deaths by 21% for all women and 33% among Black women.

There also are racial disparities in certain birth risks and adverse birth outcomes which may be exacerbated by the abortion restrictions. Specifically, as of 2022, higher shares of births to Hispanic, Black, AIAN and NHPI people were among those who received late or no prenatal care, or were preterm, or low birthweight, compared to White people (Figure 12). Timely prenatal care is particularly important for people with higher-risk pregnancies, yet research suggests that restrictive abortion policies may be causing people to start prenatal care later in pregnancy, which is already a concern for women of color who are more likely to experience delays in prenatal care initiation. Births among Asian people were also more likely to be low birthweight than those of White people. Moreover, while the birth rate among teens has been declining over time for all groups, the rate for Black, Hispanic, AIAN, and NHPI teens was over two times higher than the rate among White and Asian teens in 2021 (Figure 13). Research has also found that state-level abortion restrictions that were in place prior to Dobbs were associated with disproportionately higher rates of adverse birth outcomes, including preterm birth, for Black individuals, and that inequities widened as states became more restrictive.


Abortion bans and restrictions limit care for people experiencing a pregnancy loss, which some groups of women of color are at higher risk of experiencing compared to their White counterparts. Pregnancy loss, which includes miscarriage and stillbirth, is common, occurring in up to an estimated 20% of all pregnancies. Data on racial and ethnic disparities in miscarriage is limited, but research shows that the rates of fetal mortality (fetal demise following 20 weeks of gestation) are higher among Black, AIAN, and NHPI women compared to White women (Figure 14). While some miscarriages, particularly earlier in pregnancy, pass without any medical intervention, some people seek medical care to complete a miscarriage and/or because their health may worsen with the continuation of an unviable pregnancy. Almost all medications and procedures used to manage miscarriages and stillbirths are identical to those used in abortions. As a result, clinicians may hesitate to provide care even when medically indicated because of concerns they could be conflated with providing an abortion and therefore risk criminalization or penalties as a result. Since the Dobbs ruling, there have been several high-profile cases of people experiencing pregnancy losses who could not obtain timely miscarriage care due to state abortion bans, jeopardizing their health as a result. In KFF’s national survey of OBGYNs after the Dobbs decision, more than half (55%) of OBGYNs practicing in states where abortion is banned said their ability to practice within the standard of care has worsened since Dobbs.

In states where abortion is banned or severely restricted, the number of women forced to continue a pregnancy is likely to rise, with data suggesting disproportionate increases among women of color. While it is relatively early to see the impact of the Dobbs ruling on births, initial research suggests that birth rates could increase as a result. One study to date has estimated that there have been approximately 32,000 “additional” births as a result of the ruling, primarily concentrated in states that have banned abortions and with a disproportionate effect among people of color. A study in Texas, which had implemented a ban on abortions after six weeks gestation starting September 2021 (prior to Dobbs), found a 2% rise in the state’s fertility rate after the law’s implementation, with the sharpest increase among Hispanic women (8%).
Provider Access and Shortages
The Dobbs decision may exacerbate health care workforce shortages, particularly among clinicians providing obstetric and gynecologic care. State-level abortion bans criminalize clinicians who provide abortion care, and this has cascading effects on other aspects of maternity care. Even prior to Dobbs, there were concerns about workforce shortages in maternity care. The estimates that more than 5 million women of reproductive age in the U.S. live in counties that have few or no obstetric providers, with the largest gaps in rural communities as well as areas with higher rates of poverty, and larger shares of Black women. Many of these areas are in states with abortion bans and gestational restrictions, and there are reports of clinicians leaving these states because they are prohibited from and criminalized for offering the full scope of services they trained for and that comport with medical standards. Abortion restrictions may also affect the pipeline of new clinicians. A few studies to date, have found declines in US medical school graduates applying to OBGYN residency positions in states with abortion bans. While all positions were filled and the changes to date have been relatively small, they could suggest that future clinicians may prefer not to practice in states that ban abortion, potentially widening existing gaps in workforce capacity.
Many OBGYNs say that the Dobbs decision has had a negative impact on racial and ethnic inequities and the broader field of maternity care. In a national KFF survey, seven in ten OBGYNs say that since the Dobbs decision, racial and ethnic inequities in maternal health (70%) as well as management of pregnancy-related medical emergencies (68%) have gotten worse. Over half think that the ability to attract new OBGYNs to the profession has worsened (55%) and 64% think the same about pregnancy-related mortality (Figure 15).
Economic Circumstances
Denying women access to abortion services has negative economic consequences. Many women who are not able to obtain abortions will have children that they hadn’t planned for and face the associated costs of raising a child. In addition to the direct costs, lack of abortion access can affect women’s longer-term educational and career opportunities. Research from the Turnaway Study, which examined the impact of an unwanted pregnancy on women’s lives, found a range of negative economic effects of abortion denials, including higher poverty rates, financial debt, and poorer credit scores among women who were not able to obtain abortions compared to women who received abortions. The study also found negative socioeconomic impacts for the children born to women who were denied abortions, which may exacerbate existing racial disparities in income. Poverty rates are already much higher among children of color than White children, and research shows children in families with lower incomes experience negative long-term outcomes, including lower earnings and income, increased use of public assistance, greater likelihood of committing crimes, and more health problems.
Criminalization
People of color may be at increased risk for criminalization in the post-Roe environment. A long history of racism in judicial policy in this country has led to disproportionately higher rates of criminalization among people of color and is likely to grow as abortion care is criminalized. Prior to the Dobbs ruling, there were already cases of women criminalized for their own miscarriages, stillbirths, or infant death, due in part to the establishment of laws that protect and prioritize “fetal personhood.” The women charged were disproportionately women with lower incomes, Black women, and women living in southern states that have subsequently banned or greatly restricted abortion access. None of the state-level abortion bans specifically criminalize women for getting an abortion, but fetal personhood laws can conflate miscarriage and abortion. For example, in one high-profile case, Brittany Watts is an Ohio woman who faced criminal charges after she had a miscarriage at home in Fall 2023. While Ms. Watts sought medical care, other pregnant people experiencing a miscarriage or other complications may be deterred from seeking care, since treatment could be conflated with an abortion, putting their own health at risk as a result. Furthermore, many accusations of fetal harm are initiated by health care providers. State laws that penalize people who aid and abet abortion access and those that grant fetal personhood can perpetuate the culture of criminalizing pregnancy, particularly among communities of color.
Methods
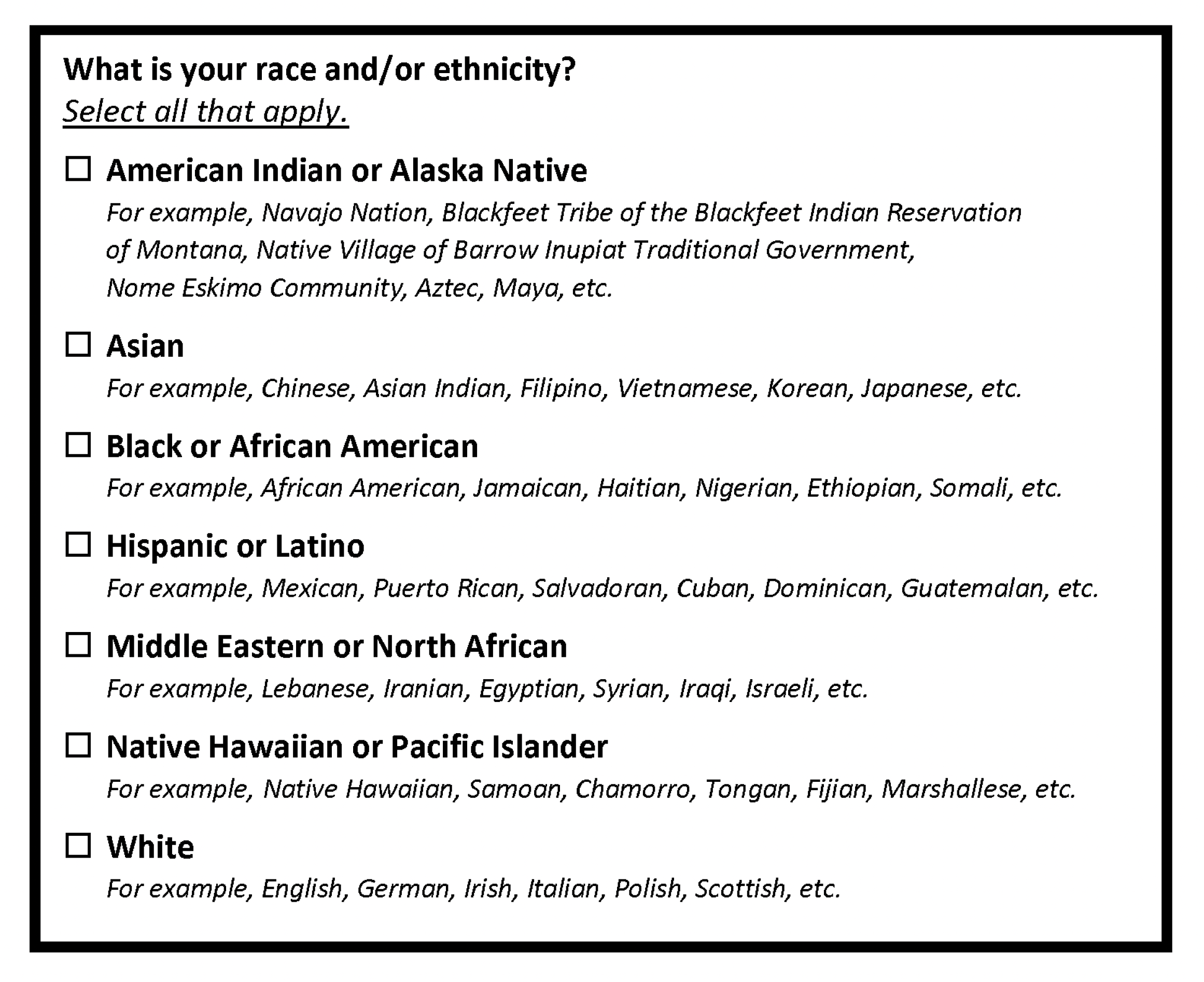
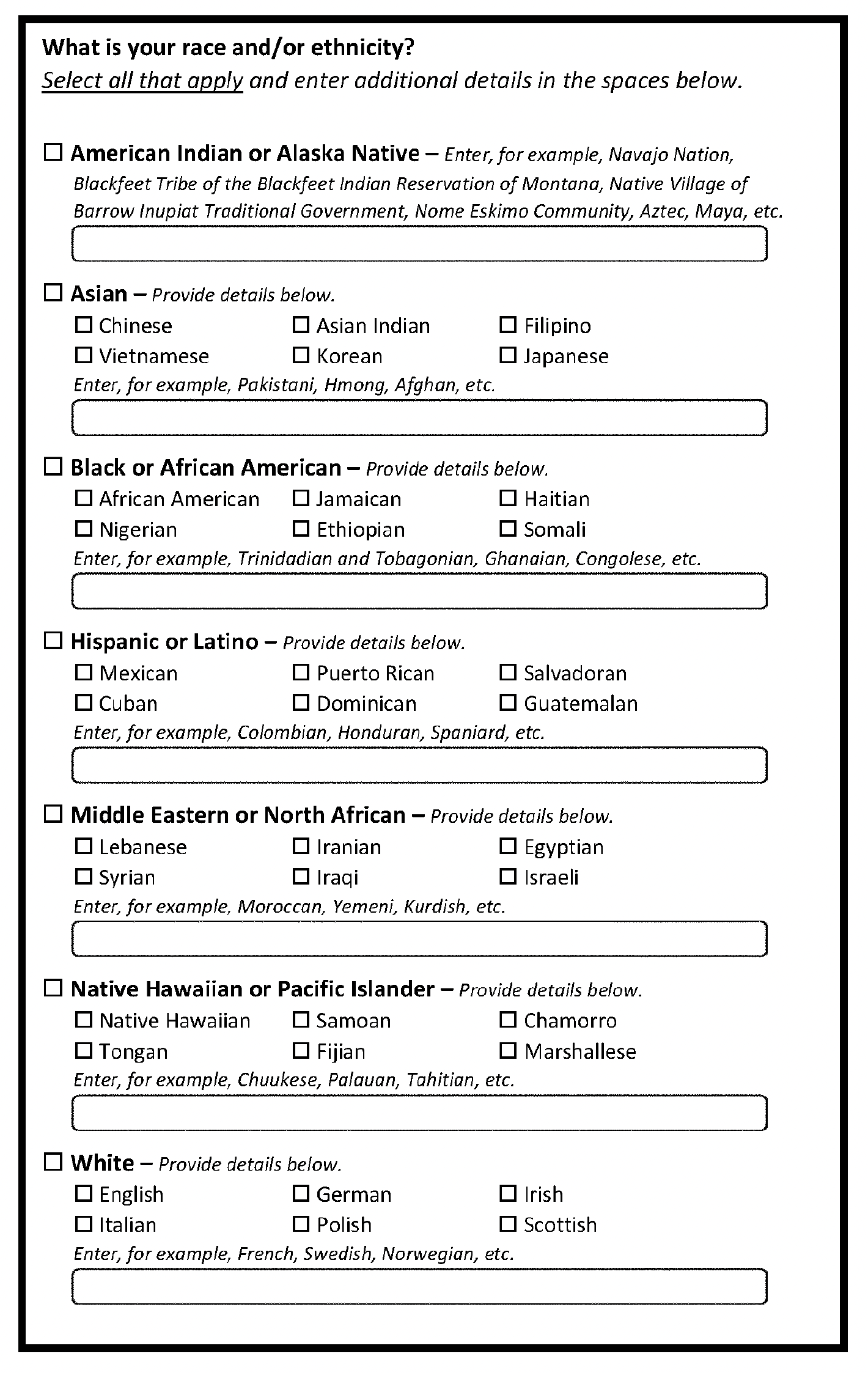
This analysis uses data from multiple sources including the 2022 American Community Survey, the 2022 Behavioral Risk Factor Surveillance System, the 2022 Survey of Household Economics and Decisionmaking, as well as from several online reports and databases including the Centers for Disease Control and Prevention (CDC) Morbidity and Mortality Weekly Report (MMWR) on abortion surveillance, National Vital Statistics Reports, the 2017 CDC Natality Public Use File, and the CDC WONDER online database. Unless otherwise noted, race/ethnicity was categorized by non-Hispanic White (White), non-Hispanic Black (Black), Hispanic, non-Hispanic American Indian and Alaska Native (AIAN), non-Hispanic Asian (Asian), and non-Hispanic Native Hawaiian or Pacific Islander (NHPI).
In this analysis, states are grouped into three categories of abortion policies based on policies implemented as of April 2024 as follows:
- Abortion Banned: Alabama, Arkansas, Idaho, Indiana, Louisiana, Kentucky, Missouri, Mississippi, North Dakota, Oklahoma, South Dakota, Texas, Tennessee, West Virginia
- Abortion Limits Between 6 and 22 weeks gestation: Arizona, Florida, Georgia, Iowa, Kansas, Nebraska, North Carolina, Ohio, South Carolina, Utah, Wisconsin
- Broader Access to Abortion: Alaska, California, Colorado, Connecticut, Delaware, District of Columbia, Hawaii, Illinois, Maine, Maryland, Massachusetts, Michigan, Montana, New Hampshire, New Jersey, New Mexico, New York, Minnesota, Oregon, Pennsylvania, Rhode Island, Vermont, Virginia, Washington, Wyoming
This analysis uses 2022 population data but categories for state abortion status are based on 2024 policy. In 2022, Wisconsin’s pre-Roe abortion ban was in effect and Indiana’s 22-week LMP ban was in effect.
Data on the share of women ages 18-49 who could not cover a $500 emergency expense using current savings is from the 2022 Survey of Household Economics and Decisionmaking and is defined as largest emergency expense individuals could handle right now using only savings.