On July 16, 2022, the federally mandated crisis number, 988, became available to all landline and cell phone users at no charge. This three-digit number connects users–via phone, text, or chat–to a network of over 200 local and state-funded crisis call centers, providing access to the 988 Suicide & Crisis Lifeline for crisis counseling, resources, and referrals. Federal investments supported the launch and implementation of 988, but ongoing funding of local call centers, as well as the development of other core components of the behavioral health crisis continuum, largely falls to state and local governments.
Over half a million lives (500,399) were lost to suicide between 2012 to 2022, with suicide rates rising nationally and in most states over this period (Appendix Table 1). Reflecting rising suicide rates, 9 in 10 adults believe the United States is amid a mental health crisis. Firearms are the predominant suicide method, involved in over half of all suicides, and increases in firearm suicides drove the total suicides to a record high in 2022.
This brief examines 988 two years after implementation using the most recent data available through May 2024 from Lifeline, including: 988 performance metrics nationally and by state, state efforts to fund local 988 call centers, emerging policies and initiatives that may indicate future trends, and a look at data that may be helpful in ongoing monitoring and development of 988.
Key takeaways from this KFF analysis of Lifeline data include the following:
- Since launch in July 2022, 988 has received 10.8 million calls, texts, and chats. In May 2024, monthly contacts exceeded half a million, up about one-third from a year ago and 80% since May 2022. Despite increased demand for 988 services, national answer rates improved and wait times decreased, though some gains slipped in the second year.
- State-level call volume and in-state answer rates vary widely across states. Monthly call volume increased in all states—ranging from 25% to 185% since launch — and the most recent in-state answer rates range from 64% to 97% in May 2024.
- Ten states have added telecom fees to provide more sustainable funding for local 988 crisis call centers, which may help centers keep up with the rising call volumes.
- Developments in 988 policy and crisis service policy include potential changes in 988 routing (georouting), continued expansion of mobile crisis and short-term crisis stabilization facilities, enhanced technology and infrastructure to connect 988 with other crisis and emergency services, and growth of specialized services for certain populations.
- 988 metrics are available online through Lifeline, though these data tend to be somewhat limited. Some states are using dashboards to provide additional data that may help to inform efforts to address suicide rates in their state.
What do we know about 988 utilization and awareness?
Since launch in July 2022, 988 received nearly 10.8 million contacts, including 1.4 million to the Veteran’s Crisis Line (VCL), with the remaining contacts consisting of 6.4 million calls, 1.4 million chats, and 1.6 million texts. SAMHSA reports that over 10 million calls, texts and chats have been answered by crisis counselors since launch, including those to the VCL. Detailed data for the VCL is not publicly available, so the remainder of the brief will not include that data. Calls are the most common mode of 988 contact, accounting for about two-thirds (68%) of total contacts to 988. Text messages and chats make up the remaining one-third of total contacts, accounting for 17% and 15%, respectively. Lifeline metrics provide only a partial picture of total crisis hotline contacts, as fewer than half of all crisis call centers (about 200 of 544) participate in the Lifeline network.
988 contacts (calls, texts, and chats) exceeded half a million in May 2024, up about one-third from a year ago and 80% since May 2022. Text message volume saw the highest relative increase, growing more than 11-fold since launch, compared to nearly 2-fold for calls. In contrast, chat volume decreased, possibly because text communication via cell phone is preferred over browser-based chat (Figure 1).

Since launch, national answer rates improved and wait times fell, even with substantial rises in contact volume—though some gains slipped in year 2. Overall answer rates rose from 70% in May 2022 (before launch) to 89% two years later, and wait times fell from 2 minutes and 20 seconds to 1 minute and 31 seconds. While these do represent improvements since launch, they are somewhat lower than they stood at one year after 988’s launch—where answer rates were higher, at 93% and wait times were lower, at 35 seconds. The decline in some performance metrics in year 2 may be due to continued rise in 988 contacts (Table 1).

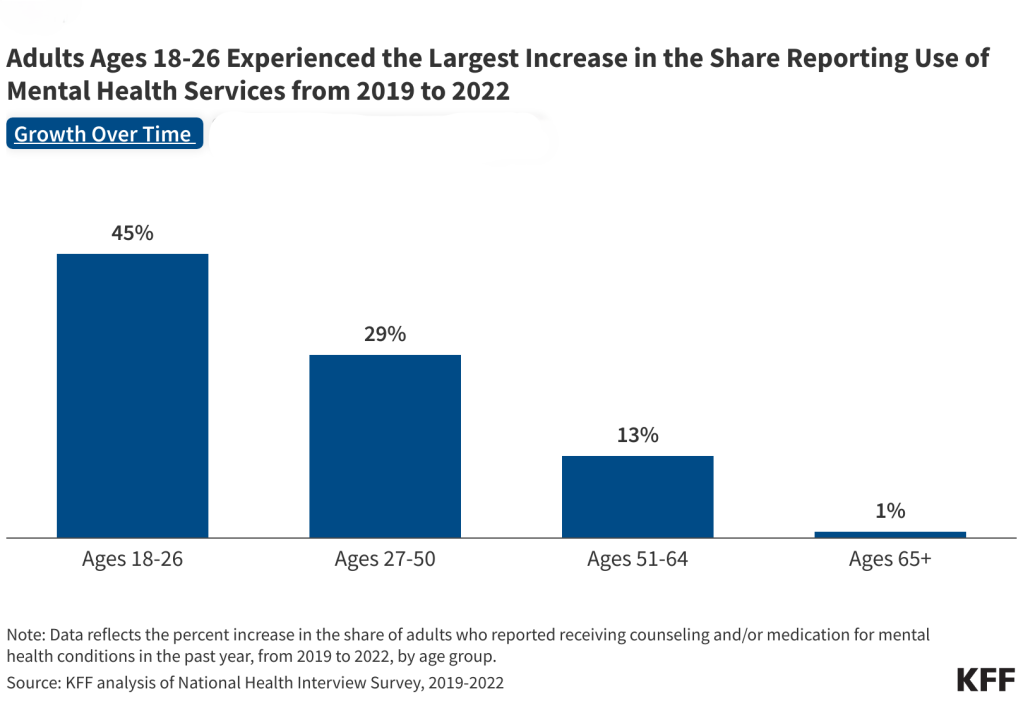
KFF polling indicates that public awareness of 988 is generally low, with 18% of adults reporting they have heard a lot or some about it. As of mid-2023, fewer than 2 in 10 adults reported familiarity with 988 and its services, though awareness may have increased since then. Despite generally low awareness, those with high psychological distress, adults who speak English very well, and White adults are more likely to report familiarity with 988. In contrast, awareness is lower among Black, Hispanic, and Asian adults and among those who do not speak English very well (Figure 2). Federal awareness campaigns set to launch in mid to late 2024, along with proposed legislation introduced to Congress late last year, aim to boost public awareness of 988 and its services. As knowledge of 988 rises, so could the demand for its services.
How does implementation vary by state?
Call volume increased in all states, with increases up to 185%. State-level data is available through Lifeline for calls to 988, but not for text or chat. Nationally, call volume rose by 95% from pre-launch to two years later, but this varied widely across states, from a low of 24% in Idaho to a high of 185% in Oklahoma. The variation in growth rates across states may be influenced by the development of 988 infrastructure and public awareness campaigns

Although nearly all states have maintained or improved their in-state answer rate since 988’s launch, answer rates continue to vary across states and range from 64 to 97% as of May 2024. 988 routes calls based on the caller’s area code to the nearest crisis center. An “in-state answer rate” measures the percentage of calls answered in the state that aligns with the caller’s area code. In May 2024, in-state answer rates ranged from a low of 64% in Nevada up to 97% in Mississippi, Montana, and Rhode Island. Calls not answered in-state are either transferred to one of Lifeline’s national backup centers or abandoned by their caller. Long wait times or local crisis center unavailability can lead to a call being redirected to national backup centers, where counselors will answer the crisis call, but may be less familiar with local resources. These calls count toward the national answer rate but not toward the answer rate of the state where the Lifeline backup center is located. Nationally, about 6% of state calls are transferred to a federal overflow facility and 10% are abandoned in-state, though these rates also vary by state. Per SAMHSA, calls may be abandoned by their user due to a technical reason (e.g. internet or mobile connection strength or service interruptions, etc.) or because the person seeking assistance ends the contact before a counselor answers, which could also happen for a range of reasons, such as they had to wait too long or decided they were not comfortable discussing their experience.

Ten states have added telecom fees to provide more sustainable funding for local 988 crisis call centers, which may help local crisis centers keep up with rising demand for the service. Although federal investments support 988 nationally and help to support state implementation, states are largely responsible for long-term funding of the local 988 crisis call centers, which have historically received minimal funding from the federal government. Under the National Suicide Hotline Designation Act of 2020, states can collect cell phone fees to help sustainably fund their local 988 call centers (similar to how 911 is funded). So far, ten states have enacted legislation to fund crisis services through telecom fees, including Virginia, Colorado, Washington, Nevada, Minnesota, California, Oregon, Delaware, Maryland, and most recently Vermont. Additionally, four other states have pending telecommunications fee legislation. Early adopters of telecom fees, such as Virginia and Washington, collected between $10.9 to $30.4 million in 988 telecom fees during FY 2022, according to an FCC report. Other sources of 988 funding include trust funds and general fund appropriations, and 5% crisis services set aside from mental health block grant funds. Insurer payments can help financially sustain 988 and other crisis services, with some states billing Medicaid or other payers and several states also passing laws requiring insurers to cover crisis care services.
Proposals to improve 988 routing aim to mirror certain 911 standards, including georouting and requirements for cell phone carriers to route 988 calls during service interruptions. Currently, 988 routes calls based on the caller’s area code, which can be problematic for people with area codes not reflective of their current location, resulting in connections to distant crisis centers with counselors unfamiliar with the local resources near the caller. Unlike 911, which uses precise geolocation data, the proposed 988 georouting would direct calls to the nearest crisis center without disclosing the caller’s exact location, helping to address technical, privacy, and legal concerns. In April of this year, the Federal Communications Commission (FCC) issued a notice proposing rulemaking for wireless carriers to adopt 988 georouting and requested comments on extending this to text messages and specialized services like LGBTQ+ and Spanish services, which are not available at all local crisis center locations. Separate legislation proposed late last year aims to improve 988 access by requiring carriers to allow 988 calls during service disruptions and ensuring multi-line systems, such as those in hotels, recognize 988 calls directly without additional steps like dialing 9 first.
Similar to 988, mobile crisis units and short-term crisis stabilization facilities are core components of the behavioral health crisis continuum, though their development and availability varies across states. Mental health professionals staff these services and provide alternatives to emergency departments and law enforcement during mental health emergencies. States are at different stages of establishing mobile crisis and short-term crisis stabilization services, and some states have leveraged Medicaid and Medicaid-focused provisions in the American Rescue Plan Act to support mobile crisis development. Most states have some form of mobile crisis, but short-term crisis stabilization facilities are less common. Even among states that have mobile crisis units, these units are often not available 24/7 or statewide. Compared to 988, other components of the crisis response system have little federal coordination, which may result in more variation in their development and structure across states.
States are investing in technology to improve infrastructure and coordination across crisis services and other emergency and health services. For example, some states are developing infrastructure to enable coordination and call diversion for mental health calls from 911 to 988. However, technical and logistics challenges, such as the presence of multiple local 911 call centers per area code and the need to develop operational rules and agreements for each, have slowed progress. Other technological developments include service registries to track bed availability, facility capacity, and appointment scheduling. GPS-enabled mobile crisis dispatch systems and tools for crisis staff to view and schedule mental health appointments are also being developed. Recent CMS guidance clarifies how Medicaid may help support some of these efforts. Additionally, the federal government’s action plan, part of the HHS’s 2024 National Strategy for Suicide Prevention, proposes funding a mobile crisis locator for use by 988 crisis centers.
Specialized services to meet the unique needs of various populations, including LGBTQ people, Spanish speakers, American Indian and Alaska Native (AIAN) people, older adults, and others, are being developed at both federal and state levels. In March 2023, Lifeline expanded its LGBTQ+ services, providing 24/7 text and phone access to affirming counseling for those under age 25. This line accounted for nearly 10% of all 988 contacts over a four-month period, but had higher abandonment rates and longer wait times than the general 988 line. Additionally, 988 offers options to route Veterans, people who speak Spanish, and people who have difficulty hearing to specialized services. Certain states are building targeted services for older adults (staffed with older adult peer supports) and launching youth-specific initiatives, including mobile crisis services for youth. Efforts are being made to provide culturally competent services for AIAN populations and other racial and ethnic groups, to address the unique needs of rural and remote areas, and to support individuals with co-occurring mental health and substance use needs.
Additional state and national crisis center metrics may help inform the 988 implementation and future program improvements. Call volume, wait times, and other metrics from Lifeline provide some insights into accessibility and demand for 988, but they don’t tell the whole story. For example, without additional data, it’s not possible to answer questions about the conditions or circumstances that prompted the 988 calls, the resolution of these calls and whether they connected to additional crisis or outpatient services, and user experience across different demographics and geographies. Comprehensive metrics can help policymakers and researchers evaluate 988’s effectiveness, identify gaps, and develop targeted interventions. Table 2 lists metrics that could be helpful for understanding 988’s implementation.

Some states or crisis call centers already track and display detailed crisis metrics through regularly updated dashboards. These online dashboards display key metrics of crisis call data, refreshed at regular intervals. In Arizona, the Solari Crisis Response Network displays aggregate data for crisis call centers in two regions. Similarly, the University of Utah summarizes Utah’s crisis data in a dashboard and in crisis services annual reports (2021 and 2020). South Dakota’s only crisis line displays detailed aggregate data on a publicly accessible dashboard, including historical data and breakouts by age, race, and gender. Data presented on these dashboards are more detailed than Lifeline data, containing metrics on accessibility, referral source, reason for the call, and some outcomes, but many do not contain historical summaries. Wisconsin’s dashboard is an exception, as it provides monthly snapshots and downloadable historical summary data.
If you or someone you know is considering suicide, call or text the 988 Suicide & Crisis Lifeline at 988