Racial and Ethnic Disparities in Access to Medical Advancements and Technologies
Introduction
Racial and ethnic disparities in health outcomes remain persistent in the United States, driven by inequities in access to and utilization of health care services and broader social and economic factors that reflect historic and ongoing racism. Given higher rates of certain illnesses among people of color, they could disproportionately benefit from medical advancements such as new drugs and therapies. However, they face increased barriers to accessing new drug therapies and treatments due to lack of diversity in clinical trials and structural barriers, including financial barriers. These disparities in access to medical advancements may further exacerbate racial disparities in health outcomes and life expectancy. This brief provides an overview of diversity in clinical trials, disparities in access to novel drug therapies and other treatments, and the implications for health and health care.
Diversity in Clinical Trials
Diverse racial and ethnic representation in clinical trials is important because drugs, vaccines, and other therapies can differentially affect groups due to variations in underlying experiences and environmental exposures. Clinical trials are research studies that determine whether medical products like medicines, vaccines, or devices are safe and effective. It is important that participants in clinical trials represent the future users of these medical products as responses to them may vary across patient groups by factors such as gender, race, ethnicity, and age because of variations in underlying experiences and environmental exposures. Having the demographics of clinical trial participants mirror the population intended to use the product can help to ensure its effectiveness and safety across patients, which may help improve health outcomes of the overall population. Racial and ethnic diversity in clinical trials also is important for building confidence in the effectiveness of new treatments. For example, research shows that Black people are more likely to have confidence in a new treatment when the trial had a greater representation of Black people.
Access barriers, lack of information, and historic and ongoing structural racism and discrimination contribute to the underrepresentation of people of color in clinical trials. People of color face an array of structural access-related barriers to participating in clinical trials. For example, fewer clinical trials are available through under-resourced hospital systems where people of color are more likely to receive care, and people of color may be less likely to be eligible to participate in trials if being uninsured or having comorbidities excludes individuals from participation. Other access challenges like limited transportation options, inflexible work schedules, and lack of access to technology may also impede participation. Beyond access barriers, knowledge gaps contribute to underrepresentation. Research indicates that physicians are less likely to discuss trials with patients of color. In addition, some patients are denied coverage for services rendered under clinical trials by their health coverage plans. Research shows that increases in education and understanding of clinical trials are associated with increased interest in participating in clinical trials. Further, ensuring enrollment efforts are culturally sensitive and addressing language and health literacy differences is important. Historical medical abuses of people of color as well as ongoing racism and discrimination may also foster reluctance among people of color to engage in clinical trials. However, research suggests that many people of color are willing to participate in clinical trials when provided the opportunity to do so.
There have been growing efforts to increase diversity in clinical trials. The National Institutes of Health (NIH) has longstanding guidelines on the inclusion of women and other underrepresented groups in clinical research and identified representative participation of underrepresented groups in NIH-funded research as a goal of its Minority Health and Health Disparities (NIHMD) 2021-2025 strategic plan. The NIMHD sponsors funding opportunities to increase the enrollment of people of color into clinical trials. The Food and Drug Administration (FDA) has a public education campaign, collaborates with stakeholders, provides clinical trial information in a variety of languages, and has identified actionable steps to improve diversity in clinical trials. It also has provided guidelines on the collection of race and ethnicity data in clinical trials and, in 2022, issued draft guidance to the industry for developing plans to increase diversity in clinical trials. During the development of the COVID-19 vaccines, the FDA offered nonbinding industry recommendations that strongly encouraged “enrollment of populations most affected by COVID-19, specifically racial and ethnic minorities.” Pfizer and Moderna made efforts to include people of color in their COVID-19 vaccine trials, and historically Black colleges and universities encouraged participation in their communities. At the industry level, the Pharmaceutical Research and Manufacturers of America implemented an Equity Initiative in 2022. It has engaged in with academic centers, community organizations, and other health partners to launch Equitable Breakthroughs in Medicine Development, a collaboration that seeks to pilot a network of sustainable, connected, and community-based trial sites.
Research suggests that collaborating with community clinicians may help increase diversity in clinical trials. It is suggested that engaging community clinics in clinical research could enhance diversity since they have established, trusted relationships with patients and can reduce accessibility and enrollment barriers for patients. A recent survey of leadership at community health centers, which serve disproportionate shares of low-income people and people of color, found that most responding health centers are interested in conducting research but face time and workforce constraints to participating in research. However, some collaborate with other organizations, such as academic institutions, to conduct this research, allowing for varied stakeholder strengths and perspectives to inform it.
Despite efforts to increase diversity, people of color remain underrepresented in clinical trials and other medical development research. Analysis finds that more than half of U.S. trials listed on ClinicalTrials.gov between 2000 and 2020 did not report enrollment data by race and ethnicity, although the share reporting any racial and ethnic enrollment data increased over time. The analysis further shows that, although there were modest improvements in diversity of trial participants over time, among trials that reported racial and ethnic data, people of color continued to be underrepresented relative to their share of the population. Between 2000 to 2020, the median enrollment of Hispanic (6%), Asian (1%), and American Indian and Alaska Native (AIAN) (0%) people was lower compared to their makeup of the total U.S. population based on the 2010 Census (Figure 1). The median enrollment of Black people was not statistically significantly lower than their share of the population as of 2010, but 21% of trials reported zero Black enrollees. Conversely, White people were overrepresented in clinical trials, with a median enrollment of 80%, and 10% of trials reported 100% White enrollees. Given that the U.S. population became more racially and ethnically diverse between 2010 to 2020, this overrepresentation has persisted. The analysis further found that industry-funded trials were associated with less racial and ethnic reporting and lower rates of enrollment of people of color compared with U.S. government-funded trials even after controlling for differences in features of the trials.
Other analysis of FDA drug approvals from 2014 to 2021 found that the median representation of Black participants was one-third of the disease burden in the population and no increases in their representation relative to White participants over the period. Even in clinical trials for COVID-19 vaccinations, which demonstrated relatively better diversity, publicly accessible data still indicated an overall underrepresentation of people of color compared to their proportion of the total U.S. population, with Black individuals having the largest disparity in representation.
Disparities in Access to New Drugs and Therapies
Lack of diversity in clinical trials may exacerbate existing disparities in treatment access for people of color. The lack of diversity in clinical trials may limit access to new drugs and therapies as their approval and indications may be limited to the populations included in the studies and clinical guidelines and insurance reimbursement may be limited by the lack of data for certain populations. For example, in 2021, the U.S. Preventive Services Task Force indicated it was unable to make specific colorectal cancer screening guidelines for Black people despite them having the highest incidence and mortality rates from colorectal cancer, due to the lack of representative cancer screening studies.
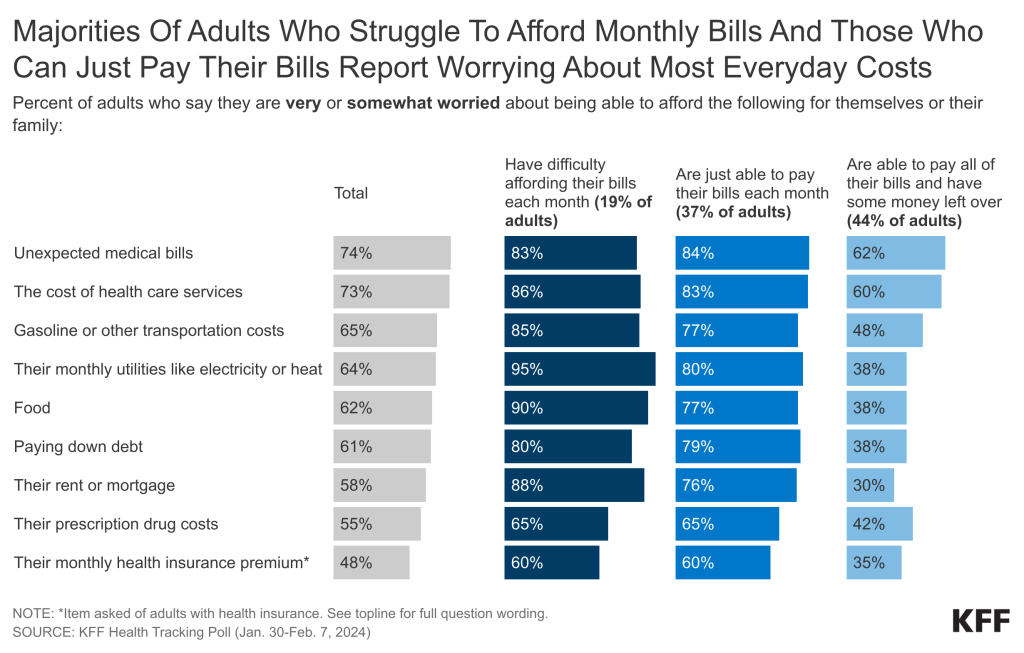
New drugs and therapeutics often have high out-of-pocket costs which may lead to disproportionate access barriers among people of color. Newly developed drugs and treatments often come with high costs that reflect development costs. In some cases, these treatments are not covered by insurance, and even when they are, they may still have high out-of-pocket costs. Patient discounts for drugs may be available but access to them may be varied and could become more limited. Due to underlying social and economic inequities, people of color are more likely than their White counterparts to be uninsured and have lower incomes meaning they likely face disproportionate cost barriers to these drugs and treatments. At the same time, people of color have worse health outcomes and higher rates of certain conditions, suggesting they potentially could disproportionately benefit from new drugs and treatments. For example:
- The recently FDA-approved Alzheimer’s drug Leqembi has a current list price of $26,500. Even though it is covered by Medicare, Medicare patients administered the drug face more than $5,000 in out-of-pocket costs per year, based on a 20% coinsurance requirement in traditional Medicare, although those with supplemental insurance may have lower costs. With higher rates of dementia and lower incomes among older Hispanic and Black adults than their White counterparts, the high cost of treatment could raise equity concerns if Black, Hispanic, and other underserved beneficiaries are less likely to gain access to this treatment because they can’t afford it.
- Similarly, the emergence of new medications for obesity treatment has raised questions about who can access them and the potential impacts on racial health disparities. Access to these medications varies and they remain unaffordable for many individuals given that they currently are excluded from Medicarecoverage, coverage through Medicaid and private plans remains limited, and out-of-pocket costs without coverage can be in excess of $1,300 per month. Although most people with obesity are White, many people of color are at increased risk for obesity, meaning they could benefit from new treatment options. However, they also are more likely than their White counterparts to face barriers to affording and accessing the new medications.
- Concerns have also been raised surrounding access to new gene therapies for sickle cell disease, an illness that disproportionately impacts Black and Hispanic people. While gene therapies provide the opportunity for a highly effective one-time treatment, they come with a hefty price point—gene therapy prices for a one-time use can cost more than $2 million.
Biases in clinical decision-making processes and technologies and limitations in access to providers may also create disproportionate access barriers for people of color. Clinical algorithms and other decision-making tools are used by physicians to guide clinical diagnoses and inform treatment plans. People of color may be less likely to receive prescriptions for effective therapies due to decision making processes that incorporate race in clinical algorithms and treatment guidelines. Research has shown that these algorithms and tools may have racial bias because the underlying data on which they are trained may be biased and/or may not reflect a diverse population. For example, recent research shows that pulse oximeters have lower accuracy for patients with darker skin. Heightened attention to this issue during the COVID-19 pandemic prompted the FDA to consider how to improve studies used to assess their performance. Differences in access to providers, including specialists who may have greater knowledge about new therapies, may also create access barriers as well as concerns about utilizing newly developed drugs or therapies given the legacy of medical system abuses. For example, analysis from 2022 shows that Black and Hispanic patients were 36% and 30%, respectively, less likely to receive nirmatrelvir-ritonavir (Paxlovid) treatment than White patients for COVID-19. Researchers suggested these disparities likely reflected more limited access to COVID-19 treatment facilities; potential prior negative experiences with the health care system, racism, or implicit bias among providers; as well as social and economic factors such as limited knowledge of treatment options, limited technology access, limited transportation, and/or language barriers.
Implications and Key Issues Looking Ahead
While some efforts are being made to mitigate disparities in access to new drugs and therapies, continued actions will be important going forward for preventing widening disparities.
As noted above, there are ongoing efforts to increase diversity in clinical trials. Under the Food and Drug Omnibus Reform Act, which was enacted as part of the Consolidated Appropriations Act of 2023, the FDA will require diversity action plans for certain clinical trials that specify enrollment goals to address historical underrepresentation of certain groups. The FDA has existing draft guidance that provides recommendations on diversity action plans. Under the legislation, the FDA can update or issue new guidance to implement the action plan requirements.
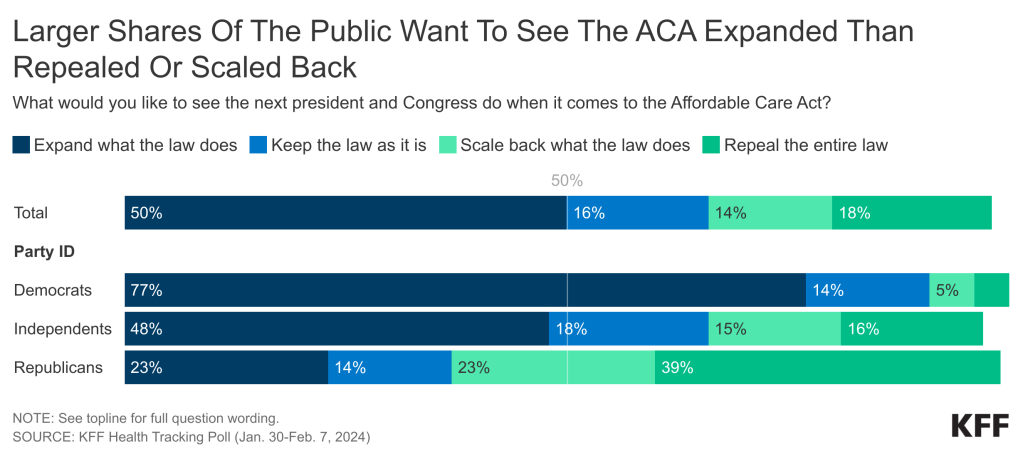
Expanding coverage for new drugs, treatments, and therapies could mitigate some financial access barriers, but disparities in financial barriers may still persist. A bipartisan group of lawmakers introduced the Treat and Reduce Obesity Act, which would authorize Medicare Part D coverage of medications when used for the treatment of obesity or weight loss management in overweight individuals with related comorbidities. As of July 2023, sixteen states reported Medicaid Fee-For-Service coverage of at least one weight-loss medication for the treatment of obesity for adults. The newly developed Alzheimer’s drug, Leqembi, already is covered by Medicare for all indicated populations. Having coverage available for these new drugs may help address some disparities in financial access barriers. However, even with coverage, uninsured individuals would continue to face financial barriers and some covered individuals may continue to face substantial out-of-pocket costs, leaving treatments unaffordable.
Prioritizing equity in access to new treatments is of increasing importance amid the growing use of clinical algorithms and artificial intelligence (AI) to guide health care. As use of AI grows in health care, it will be important to ensure that algorithms do not perpetuate disparities and biases through the use of race or due to biases in the underlying data upon which they rely. Research further suggests that if carefully designed, algorithms could mitigate bias and help to reduce disparities in care. There have been recent federal and state level efforts to reduce and protect against bias in the use of AI and clinical algorithms. The FDA proposed a framework to monitor and evaluate the use, safety, and effectiveness of AI, which includes a focus on improving methods to identify, evaluate, and address algorithmic bias. In 2022, the Department of Health and Human Services (HHS) issued a proposed rule that prohibits discrimination through the use of decision-making clinical algorithms, although researchers have noted that the proposed rule does not offer specific guidelines on how to prevent discrimination and that there are a wide range of potential strategies available for reducing bias in clinical algorithms. In December 2023, HHS finalized a rule that implements new transparency requirements for clinical decision support tools and algorithms to ensure users have access to a baseline set of information that supports their ability to assess their “fairness, appropriateness, validity, effectiveness, and safety.” At the state level, at least eleven states have begun regulating the use of AI and algorithms in health care in an effort to mitigate instances of discrimination. In early 2023, the Coalition for Health AI released guidance for the implementation of AI to increase trustworthiness and transparency in AI tools that centers equity, fairness, and ethics. The guidance includes recommendations on developing a common set of principles to guide the development and use of AI tools and a coalition or advisory board to help ensure equity and facilitate trustworthiness in health-related AI.